Broad-Spectrum Antibiotic Use and Disease Progression in Early-Stage Melanoma Patients: A Retrospective Cohort Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Data
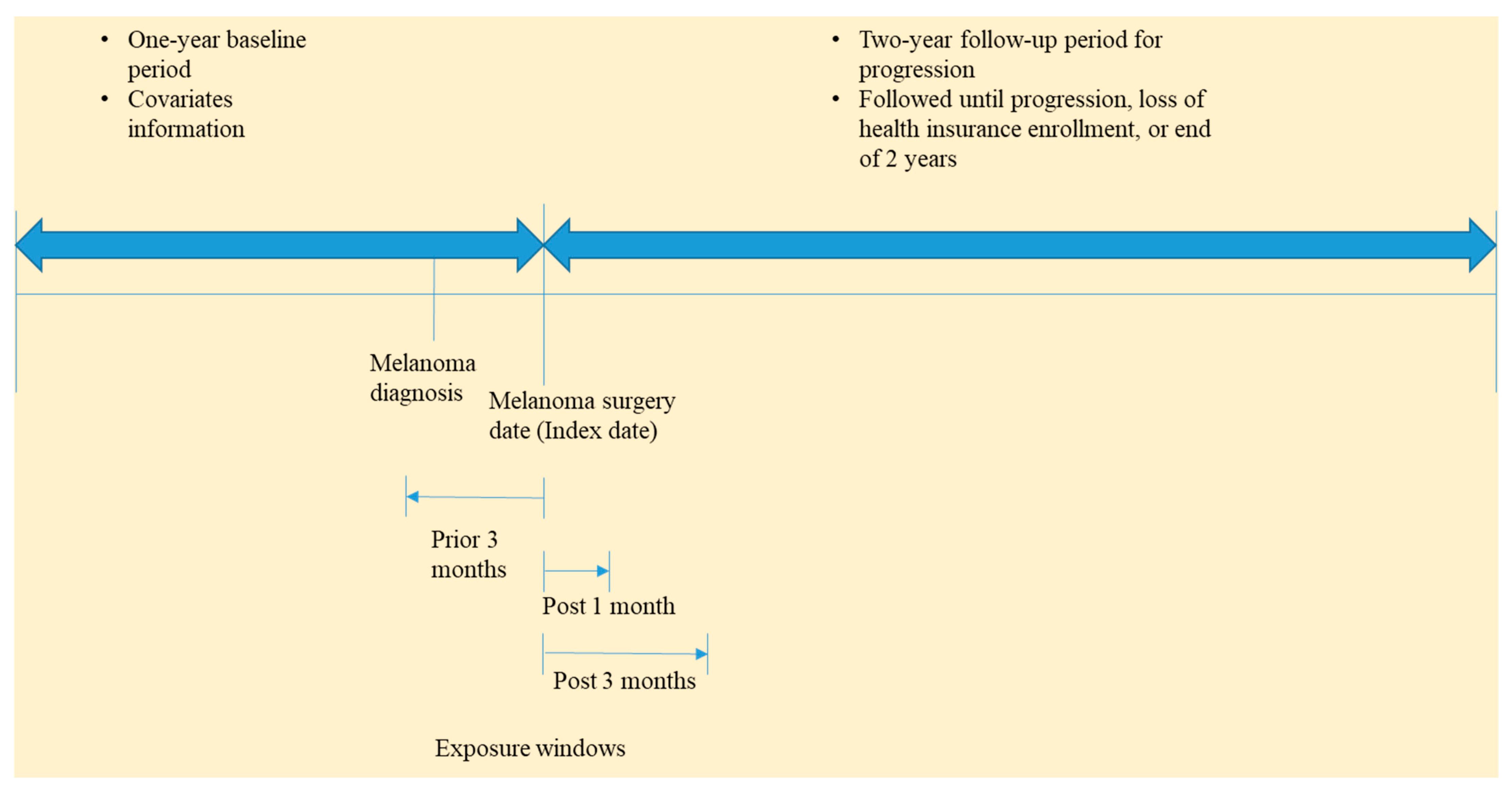
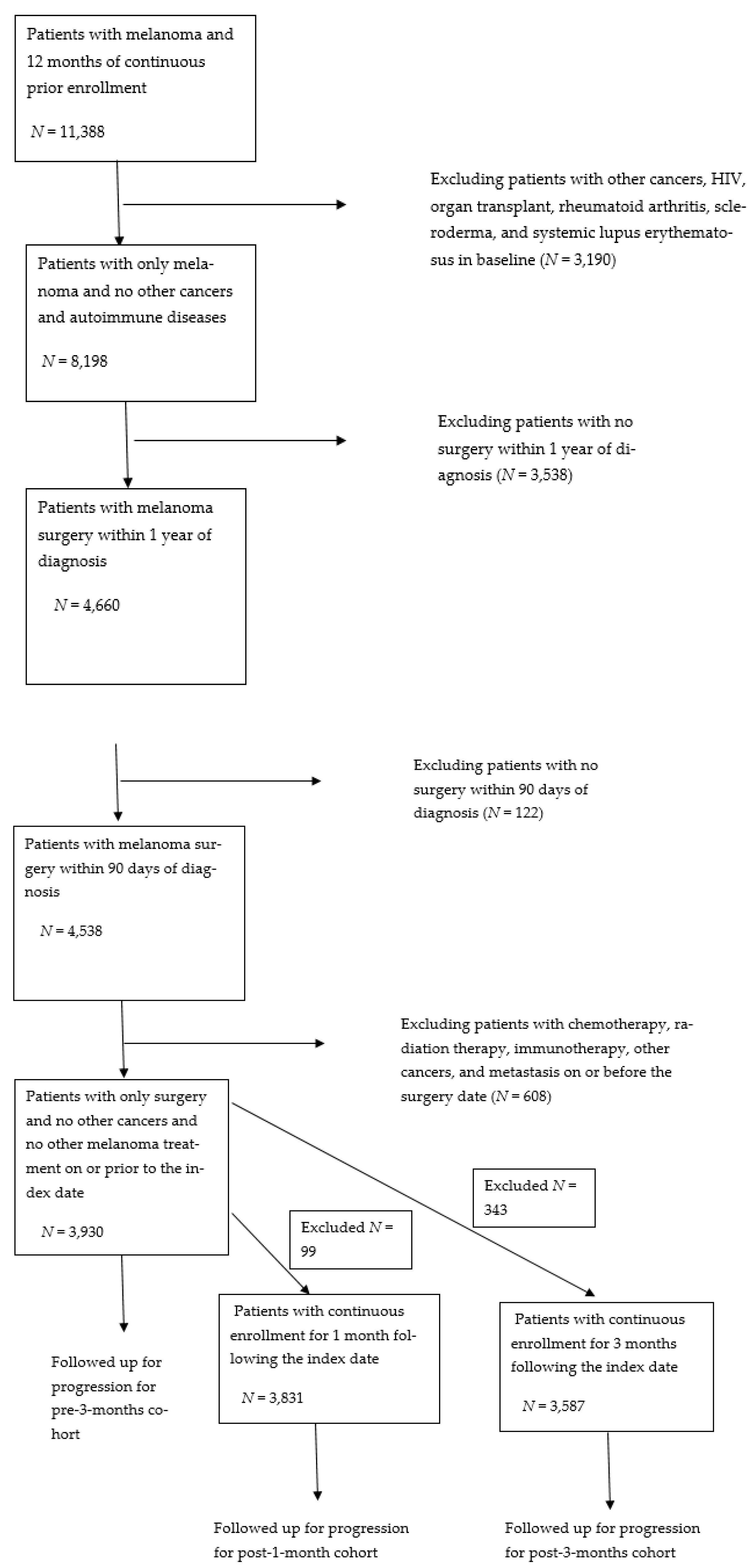
2.2. Study Design and Patient Population
2.3. Antibiotic Exposure
2.4. Outcome
2.5. Covariates
2.6. Statistical Analysis
2.7. Sensitivity Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.; Miller, K.; Jemal, A. Cancer Statistics, 2017. CA Cancer J. Clin. 2017, 67, 7–30. [Google Scholar] [CrossRef]
- Glazer, A.M.; Winkelmann, R.R.; Farberg, A.S.; Rigel, D.S. Analysis of Trends in US Melanoma Incidence and Mortality. JAMA Dermatol. 2017, 153, 225–226. [Google Scholar] [CrossRef] [PubMed]
- Paulson, K.G.; Gupta, D.; Kim, T.S.; Veatch, J.R.; Byrd, D.R.; Bhatia, S.; Wojcik, K.; Chapuis, A.G.; Thompson, J.A.; Madeleine, M.M.; et al. Age-Specific Incidence of Melanoma in the United States. JAMA Dermatol. 2020, 156, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Gershenwald, J.E.; Scolyer, R.A.; Hess, K.R.; Sondak, V.K.; Long, G.V.; Ross, M.I.; Lazar, A.J.; Faries, M.B.; Kirkwood, J.M.; McArthur, G.A.; et al. Melanoma staging: Evidence-based changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J. Clin. 2017, 67, 472–492. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.; Walker, S.; Shui, I.; Brandtmüller, A.; Brandtmüller, B.; Cadwell, K.; Scherrer, E. Epidemiology and survival outcomes in stages II and III cutaneous melanoma: A systematic review. Futur. Med. 2020, 7, 39–53. [Google Scholar] [CrossRef]
- Tas, F. Metastatic behavior in melanoma: Timing, pattern, survival, and influencing factors. J. Oncol. 2012, 2012, 1–9. [Google Scholar] [CrossRef]
- Metastatic Melanoma|Melanoma Research Foundation. Available online: https://www.melanoma.org/understand-melanoma/what-is-melanoma/metastatic-melanoma (accessed on 2 January 2019).
- Song, X.; Zhao, Z.; Barber, B.; Farr, A.M.; Ivanov, B.; Novich, M. Overall survival in patients with metastatic melanoma. Curr. Med. Res. Opin. 2015, 31, 987–991. [Google Scholar] [CrossRef]
- Coit, D.G.; Thompson, J.A.; Albertini, M.R.; Barker, C.; Carson, W.E.; Contreras, C.; Daniels, G.A.; DiMaio, D.; Fields, R.C.; Fleming, M.D.; et al. Cutaneous melanoma, version 2.2019. JNCCN J. Natl. Compr. Cancer Netw. 2019, 17, 367–402. [Google Scholar] [CrossRef]
- Lee, M.P.; Sobanko, J.F.; Shin, T.M.; Howe, N.M.; Barbieri, J.S.; Miller, C.J.; Etzkorn, J.R. Evolution of Excisional Surgery Practices for Melanoma in the United States. JAMA Dermatol. 2019, 155, 1244–1251. [Google Scholar] [CrossRef]
- Leeneman, B.; Franken, M.G.; Coupé, V.M.H.; Hendriks, M.P.; Kruit, W.; Plaisier, P.W.; van Ruth, S.; Verstijnen, J.A.M.C.; Wouters, M.W.J.M.; Blommestein, H.M.; et al. Stage-specific disease recurrence and survival in localized and regionally advanced cutaneous melanoma. Eur. J. Surg. Oncol. 2019, 45, 825–831. [Google Scholar] [CrossRef]
- Robert, C.; Schachter, J.; Long, G.V.; Arance, A.; Grob, J.J.; Mortier, L.; Daud, A.; Carlino, M.S.; McNeil, C.; Lotem, M.; et al. Pembrolizumab versus Ipilimumab in Advanced Melanoma. N. Engl. J. Med. 2015, 372, 2521–2532. [Google Scholar] [CrossRef] [PubMed]
- Ribas, A.; Hamid, O.; Daud, A.; Hodi, F.S.; Wolchok, J.D.; Kefford, R.; Joshua, A.M.; Patnaik, A.; Hwu, W.-J.; Weber, J.S.; et al. Association of Pembrolizumab With Tumor Response and Survival Among Patients With Advanced Melanoma. JAMA 2016, 315, 1600. [Google Scholar] [CrossRef]
- Wolchok, J.D.; Kluger, H.; Callahan, M.K.; Postow, M.A.; Rizvi, N.A.; Lesokhin, A.M.; Segal, N.H.; Ariyan, C.E.; Gordon, R.-A.; Reed, K.; et al. Nivolumab plus Ipilimumab in Advanced Melanoma. N. Engl. J. Med. 2013, 369, 122–133. [Google Scholar] [CrossRef] [PubMed]
- King, L.M.; Bartoces, M.; Fleming-Dutra, K.E.; Roberts, R.M.; Hicks, L.A. Changes in US outpatient antibiotic prescriptions from 2011-2016. Clin. Infect. Dis. 2020, 70, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Barnett, M.L.; Linder, J.A. Antibiotic prescribing to adults with sore throat in the United States, 1997–2010. JAMA Intern. Med. 2014, 174, 138–140. [Google Scholar] [CrossRef]
- Fairlie, T.; Shapiro, D.J.; Hersh, A.L.; Hicks, L.A. National trends in visit rates and antibiotic prescribing for adults with acute sinusitis. Arch. Intern. Med. 2012, 172, 1513–1514. [Google Scholar] [CrossRef][Green Version]
- Ventola, C.L. The antibiotic resistance crisis: Part 1: Causes and threats. Pharm. Ther. 2015, 40, 277–283. [Google Scholar]
- Guarner, F.; Malagelada, J. Gut flora in health and disease. Lancet 2003, 360, 512–519. [Google Scholar] [CrossRef]
- Zattra, E.; Fortina, A.B.; Bordignon, M.; Piaserico, S.; Alaibac, M. Immunosuppression and melanocyte proliferation. Melanoma Res. 2009, 19, 63–68. [Google Scholar] [CrossRef]
- Eslami-S, Z.; Majidzadeh-A, K.; Halvaei, S.; Babapirali, F.; Esmaeili, R. Microbiome and Breast Cancer: New Role for an Ancient Population. Front. Oncol. 2020, 10, 120. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Li, S.; Wang, N.; Tan, H.-Y.; Zhang, Z.; Feng, Y. The Cross-Talk Between Gut Microbiota and Lungs in Common Lung Diseases. Front. Microbiol. 2020, 11, 301. [Google Scholar] [CrossRef]
- Pflug, N.; Kluth, S.; Vehreschild, J.J.; Bahlo, J.; Tacke, D.; Biehl, L.; Eichhorst, B.; Fischer, K.; Cramer, P.; Fink, A.M.; et al. Efficacy of antineoplastic treatment is associated with the use of antibiotics that modulate intestinal microbiota. Oncoimmunology 2016, 5, e1150399. [Google Scholar] [CrossRef]
- Derosa, L.; Hellmann, M.D.; Spaziano, M.; Halpenny, D.; Fidelle, M.; Rizvi, H.; Long, N.; Plodkowski, A.J.; Arbour, K.C.; Chaft, J.E.; et al. Negative association of antibiotics on clinical activity of immune checkpoint inhibitors in patients with advanced renal cell and non-small-cell lung cancer. Ann. Oncol. 2018, 29, 1437–1444. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, A.M.; Kichenadasse, G.; Karapetis, C.S.; Rowland, A.; Sorich, M.J. Concomitant Antibiotic Use and Survival in Urothelial Carcinoma Treated with Atezolizumab. Eur. Urol. 2020, 78, 540–543. [Google Scholar] [CrossRef]
- Elkrief, A.; El Raichani, L.; Richard, C.; Messaoudene, M.; Belkaid, W.; Malo, J.; Belanger, K.; Miller, W.; Jamal, R.; Letarte, N.; et al. Antibiotics are associated with decreased progression-free survival of advanced melanoma patients treated with immune checkpoint inhibitors. Oncoimmunology 2019, 8, e1568812. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.-Z.; Gao, P.; Song, Y.-X.; Xu, Y.; Sun, J.-X.; Chen, X.-W.; Zhao, J.-H.; Wang, Z.-N. Antibiotic use and the efficacy of immune checkpoint inhibitors in cancer patients: A pooled analysis of 2740 cancer patients. OncoImmunology 2019, 8, e1665973. [Google Scholar] [CrossRef] [PubMed]
- Karpiński, T.M.; Adamczak, A. Anticancer activity of bacterial proteins and peptides. Pharmaceutics 2018, 10, 54. [Google Scholar] [CrossRef]
- Lamb, R.; Ozsvari, B.; Lisanti, C.L.; Tanowitz, H.B.; Howell, A.; Martinez-Outschoorn, U.E.; Sotgia, F.; Lisanti, M.P. Antibiotics that target mitochondria effectively eradicate cancer stem cells, across multiple tumor types: Treating cancer like an infectious disease. Oncotarget 2015, 6, 4569–4584. [Google Scholar] [CrossRef] [PubMed]
- Long, M.D.; Martin, C.F.; Pipkin, C.A.; Herfarth, H.H.; Sandler, R.S.; Kappelman, M.D. Risk of Melanoma and Nonmelanoma Skin Cancer Among Patients With Inflammatory Bowel Disease. Gastroenterology 2012, 143, 390–399. [Google Scholar] [CrossRef] [PubMed]
- Conic, R.Z.; Cabrera, C.I.; Khorana, A.A.; Gastman, B.R. Determination of the impact of melanoma surgical timing on survival using the National Cancer Database. J. Am. Acad. Dermatol. 2018, 78, 40. [Google Scholar] [CrossRef]
- Hernán, M.A.; Sauer, B.C.; Hernández-Díaz, S.; Platt, R.; Shrier, I. Specifying a target trial prevents immortal time bias and other self-inflicted injuries in observational analyses. J. Clin. Epidemiol. 2016, 79, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Antibiotics: List of Common Antibiotics & Types—Drugs.com. Available online: https://www.drugs.com/article/antibiotics.html (accessed on 6 May 2021).
- Von Schuckmann, L.A.; Hughes, M.C.B.; Ghiasvand, R.; Malt, M.; van der Pols, J.C.; Beesley, V.L.; Khosrotehrani, K.; Smithers, B.M.; Green, A.C. Risk of Melanoma Recurrence After Diagnosis of a High-Risk Primary Tumor. JAMA Dermatol. 2019, 155, 688–693. [Google Scholar] [CrossRef]
- Nordstrom, B.L.; Simeone, J.C.; Malley, K.G.; Fraeman, K.H.; Klippel, Z.; Durst, M.; Page, J.H.; Xu, H. Validation of claims algorithms for progression to metastatic cancer in patients with breast, non-small cell lung, and colorectal cancer. Front. Oncol. 2016, 6, 18. [Google Scholar] [CrossRef] [PubMed]
- Lideikaitė, A.; Mozūraitienė, J.; Letautienė, S. Analysis of prognostic factors for melanoma patients. Acta Med. Litu. 2017, 24, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Schneeweiss, S.; Rassen, J.A.; Glynn, R.J.; Avorn, J.; Mogun, H.; Brookhart, M.A. High-dimensional propensity score adjustment in studies of treatment effects using health care claims data. Epidemiology 2009, 20, 512–522. [Google Scholar] [CrossRef]
- ICD-9-CM to and from ICD-10-CM and ICD-10-PCS Crosswalk or General Equivalence Mappings|NBER. Available online: https://data.nber.org/data/icd9-icd-10-cm-and-pcs-crosswalk-general-equivalence-mapping.html (accessed on 17 April 2020).
- Desai, R.J.; Franklin, J.M. Alternative approaches for confounding adjustment in observational studies using weighting based on the propensity score: A primer for practitioners. BMJ 2019, 367, l5657. [Google Scholar] [CrossRef]
- Cole, S.R.; Hernan, M.A. Constructing Inverse Probability Weights for Marginal Structural Models. Am. J. Epidemiol. 2008, 168, 656–664. [Google Scholar] [CrossRef]
- Prasad, V.; Jena, A.B. Prespecified Falsification End Points: Can They Validate True Observational Associations? JAMA 2013, 309, 241–242. [Google Scholar] [CrossRef]
- Bråten, L.C.H.; Rolfsen, M.P.; Espeland, A.; Wigemyr, M.; Aßmus, J.; Froholdt, A.; Haugen, A.J.; Marchand, G.H.; Kristoffersen, P.M.; Lutro, O.; et al. Efficacy of antibiotic treatment in patients with chronic low back pain and Modic changes (the AIM study): Double blind, randomised, placebo controlled, multicentre trial. BMJ 2019, 367, l5654. [Google Scholar] [CrossRef]
- Türkan, F.; Huyut, Z.; Taslimi, P.; Huyut, M.T.; Gülçin, İ. Investigation of the effects of cephalosporin antibiotics on glutathione S-transferase activity in different tissues of rats in vivo conditions in order to drug development research. Drug Chem. Toxicol. 2020, 43, 423–428. [Google Scholar] [CrossRef]
- Townsend, D.M.; Tew, K.D. The role of glutathione-S-transferase in anti-cancer drug resistance. Oncogene 2003, 22, 7369–7375. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, A.; Gupta, S. The multifaceted role of glutathione S-transferases in cancer. Cancer Lett. 2018, 433, 33–42. [Google Scholar] [CrossRef]
- Branda, R.F.; McCormack, J.J.; Perlmutter, C.A. Cellular pharmacology of chloroquinoxaline sulfonamide and a related compound in murine B16 melanoma cells. Biochem. Pharmacol. 1988, 37, 4557–4564. [Google Scholar] [CrossRef]
- Casini, A.; Scozzafava, A.; Mastrolorenzo, A.; Supuran, C. Sulfonamides and Sulfonylated Derivatives as Anticancer Agents. Curr. Cancer Drug Targets 2005, 2, 55–75. [Google Scholar] [CrossRef]
- Singh, S.; Lomelino, C.L.; Mboge, M.Y.; Frost, S.C.; McKenna, R. Cancer drug development of carbonic anhydrase inhibitors beyond the active site. Molecules 2018, 23, 1045. [Google Scholar] [CrossRef] [PubMed]
- Saikali, Z.; Singh, G. Doxycycline and other tetracyclines in the treatment of bone metastasis. Anticancer. Drugs 2003, 14, 773–778. [Google Scholar] [CrossRef]
- Quintero-Fabián, S.; Arreola, R.; Becerril-Villanueva, E.; Torres-Romero, J.C.; Arana-Argáez, V.; Lara-Riegos, J.; Ramírez-Camacho, M.A.; Alvarez-Sánchez, M.E. Role of Matrix Metalloproteinases in Angiogenesis and Cancer. Front. Oncol. 2019, 9, 1370. [Google Scholar] [CrossRef] [PubMed]
- Duivenvoorden, W.C.M.; Vukmirović-Popović, S.; Kalina, M.; Seidlitz, E.; Singh, G. Effect of zoledronic acid on the doxycycline-induced decrease in tumour burden in a bone metastasis model of human breast cancer. Br. J. Cancer 2007, 96, 1526–1531. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rok, J.; Karkoszka, M.; Rzepka, Z.; Respondek, M.; Banach, K.; Beberok, A.; Wrześniok, D. Cytotoxic and proapoptotic effect of doxycycline—An in vitro study on the human skin melanoma cells. Toxicol. In Vitro 2020, 65, 104790. [Google Scholar] [CrossRef]
- Yadav, V.; Talwar, P. Repositioning of fluoroquinolones from antibiotic to anti-cancer agents: An underestimated truth. Biomed. Pharmacother. 2019, 111, 934–946. [Google Scholar] [CrossRef]
- Beberok, A.; Wrześniok, D.; Szlachta, M.; Rok, J.; Rzepka, Z.; Respondek, M.; Buszman, E. Lomefloxacin Induces Oxidative Stress and Apoptosis in COLO829 Melanoma Cells. Int. J. Mol. Sci. 2017, 18, 2194. [Google Scholar] [CrossRef] [PubMed]
- Dinos, G.P.; Athanassopoulos, C.M.; Missiri, D.A.; Giannopoulou, P.C.; Vlachogiannis, I.A.; Papadopoulos, G.E.; Papaioannou, D.; Kalpaxis, D.L. Chloramphenicol derivatives as antibacterial and anticancer agents: Historic problems and current solutions. Antibiotics 2016, 5, 20. [Google Scholar] [CrossRef]
- Giannopoulou, P.; Missiri, D.; Kournoutou, G.; Sazakli, E.; Papadopoulos, G.; Papaioannou, D.; Dinos, G.; Athanassopoulos, C.; Kalpaxis, D. New Chloramphenicol Derivatives from the Viewpoint of Anticancer and Antimicrobial Activity. Antibiotics 2019, 8, 9. [Google Scholar] [CrossRef]
- Uribe-Herranz, M.; Rafail, S.; Beghi, S.; Gil-de-Gómez, L.; Verginadis, I.; Bittinger, K.; Pustylnikov, S.; Pierini, S.; Perales-Linares, R.; Blair, I.A.; et al. Gut microbiota modulate dendritic cell antigen presentation and radiotherapy-induced antitumor immune response. J. Clin. Investig. 2020, 130, 466–479. [Google Scholar] [CrossRef] [PubMed]
- Zheng, D.; Liwinski, T.; Elinav, E. Interaction between microbiota and immunity in health and disease. Cell Res. 2020, 30, 492–506. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Tang, H.; Chen, P.; Xie, H.; Tao, Y. Demystifying the manipulation of host immunity, metabolism, and extraintestinal tumors by the gut microbiome. Signal Transduct. Target. Ther. 2019, 4, 1–34. [Google Scholar] [CrossRef] [PubMed]
- Ruff, W.E.; Greiling, T.M.; Kriegel, M.A. Host–microbiota interactions in immune-mediated diseases. Nat. Rev. Microbiol. 2020, 18, 521–538. [Google Scholar] [CrossRef] [PubMed]
- Rivas, M.N.; Crother, T.R.; Arditi, M. The microbiome in asthma. Curr. Opin. Pediatr. 2016, 28, 764–771. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Li, J.; Gui, X.; Shi, X.; Bao, Z.; Han, H.; Li, M.D. Updated review of research on the gut microbiota and their relation to depression in animals and human beings. Mol. Psychiatry 2020, 25, 2759–2772. [Google Scholar] [CrossRef]
- Saji, N.; Niida, S.; Murotani, K.; Hisada, T.; Tsuduki, T.; Sugimoto, T.; Kimura, A.; Toba, K.; Sakurai, T. Analysis of the relationship between the gut microbiome and dementia: A cross-sectional study conducted in Japan. Sci. Rep. 2019, 9, 1–9. [Google Scholar] [CrossRef]
- Thomas, R.M.; Gharaibeh, R.Z.; Gauthier, J.; Beveridge, M.; Pope, J.L.; Guijarro, M.V.; Yu, Q.; He, Z.; Ohland, C.; Newsome, R.; et al. Intestinal microbiota enhances pancreatic carcinogenesis in preclinical models. Carcinogenesis 2018, 39, 1068–1078. [Google Scholar] [CrossRef] [PubMed]
- Dapito, D.H.; Mencin, A.; Gwak, G.Y.; Pradere, J.P.; Jang, M.K.; Mederacke, I.; Caviglia, J.M.; Khiabanian, H.; Adeyemi, A.; Bataller, R.; et al. Promotion of Hepatocellular Carcinoma by the Intestinal Microbiota and TLR4. Cancer Cell 2012, 21, 504–516. [Google Scholar] [CrossRef]
- Yachida, S.; Mizutani, S.; Shiroma, H.; Shiba, S.; Nakajima, T.; Sakamoto, T.; Watanabe, H.; Masuda, K.; Nishimoto, Y.; Kubo, M.; et al. Metagenomic and metabolomic analyses reveal distinct stage-specific phenotypes of the gut microbiota in colorectal cancer. Nat. Med. 2019, 25, 968–976. [Google Scholar] [CrossRef]
- Kirkup, B.; McKee, A.; Makin, K.; Paveley, J.; Caim, S.; Alcon-Giner, C.; Leclaire, C.; Dalby, M.; Le Gall, G.; Andrusaite, A.; et al. Perturbation of the gut microbiota by antibiotics results in accelerated breast tumour growth and metabolic dysregulation. bioRxiv 2019, 553602. [Google Scholar] [CrossRef]
- Golombos, D.M.; Ayangbesan, A.; O’Malley, P.; Lewicki, P.; Barlow, L.M.; Barbieri, C.E.; Chan, C.; DuLong, C.; Abu-Ali, G.; Huttenhower, C.; et al. The Role of Gut Microbiome in the Pathogenesis of Prostate Cancer: A Prospective, Pilot Study. Urology 2018, 111, 122–128. [Google Scholar] [CrossRef]
- Zhuang, H.; Cheng, L.; Wang, Y.; Zhang, Y.-K.; Zhao, M.-F.; Liang, G.-D.; Zhang, M.-C.; Li, Y.-G.; Zhao, J.-B.; Gao, Y.-N.; et al. Dysbiosis of the Gut Microbiome in Lung Cancer. Front. Cell. Infect. Microbiol. 2019, 9, 112. [Google Scholar] [CrossRef]
- Li, Y.; Tinoco, R.; Elmén, L.; Segota, I.; Xian, Y.; Fujita, Y.; Sahu, A.; Zarecki, R.; Marie, K.; Feng, Y.; et al. Gut microbiota dependent anti-tumor immunity restricts melanoma growth in Rnf5 −/− mice. Nat. Commun. 2019, 10, 468. [Google Scholar] [CrossRef] [PubMed]
- Petrelli, F.; Ghidini, M.; Ghidini, A.; Perego, G.; Cabiddu, M.; Khakoo, S.; Oggionni, E.; Abeni, C.; Hahne, J.C.; Tomasello, G.; et al. Use of antibiotics and risk of cancer: A systematic review and meta-analysis of observational studies. Cancers 2019, 11, 1174. [Google Scholar] [CrossRef]
- Friedman, G.D.; Oestreicher, N.; Chan, J.; Quesenberry, C.P.; Udaltsova, N.; Habel, L.A. Antibiotics and risk of breast cancer: Up to 9 years of follow-up of 2.1 million women. Cancer Epidemiol. Biomarkers Prev. 2006, 15, 2102–2106. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; García Rodríguez, L.A.; Hernández-Díaz, S. Antibiotic use and the risk of lung cancer. Cancer Epidemiol. Biomarkers Prev. 2008, 17, 1308–1315. [Google Scholar] [CrossRef] [PubMed]
- Mohiuddin, J.J.; Chu, B.; Facciabene, A.; Poirier, K.; Wang, X.; Doucette, A.; Zheng, C.; Xu, W.; Anstadt, E.J.; Amaravadi, R.K.; et al. Association of Antibiotic Exposure with Survival and Toxicity in Patients with Melanoma Receiving Immunotherapy. J. Natl. Cancer Inst. 2021, 113, 162–170. [Google Scholar] [CrossRef]
- Pinato, D.J.; Howlett, S.; Ottaviani, D.; Urus, H.; Patel, A.; Mineo, T.; Brock, C.; Power, D.; Hatcher, O.; Falconer, A.; et al. Association of prior antibiotic treatment with survival and response to immune checkpoint inhibitor therapy in patients with cancer. JAMA Oncol. 2019, 5, 1774–1778. [Google Scholar] [CrossRef] [PubMed]
- Tinsley, N.; Zhou, C.; Tan, G.; Rack, S.; Lorigan, P.; Blackhall, F.; Krebs, M.; Carter, L.; Thistlethwaite, F.; Graham, D.; et al. Cumulative Antibiotic Use Significantly Decreases Efficacy of Checkpoint Inhibitors in Patients with Advanced Cancer. Oncologist 2020, 25, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Elkrief, A.; Derosa, L.; Kroemer, G.; Zitvogel, L.; Routy, B. The negative impact of antibiotics on outcomes in cancer patients treated with immunotherapy: A new independent prognostic factor? Ann. Oncol. 2019, 30, 1572–1579. [Google Scholar] [CrossRef]
- Lurienne, L.; Cervesi, J.; Duhalde, L.; de Gunzburg, J.; Andremont, A.; Zalcman, G.; Buffet, R.; Bandinelli, P.A. NSCLC Immunotherapy Efficacy and Antibiotic Use: A Systematic Review and Meta-Analysis. J. Thorac. Oncol. 2020, 15, 1147–1159. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Kong, S.; Cheung, W.Y.; Bouchard-Fortier, A.; Dort, J.C.; Quan, H.; Buie, E.M.; McKinnon, G.; Quan, M.L. Development and validation of case-finding algorithms for recurrence of breast cancer using routinely collected administrative data. BMC Cancer 2019, 19, 1–10. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Antibiotics in Pre-3-Months; n (%) | Antibiotics in Post-1-Month; n (%) | Antibiotics in Post-3-Months; n (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total (n = 3930) | No Use (n = 3284) | Use (n = 646) | p-Value | Total (n = 3831) | No Use (n = 3006) | Use (n = 825) | p-Value | Total (n = 3593) | No Use (n = 2819) | Use (n = 774) | p-Value | |
| Age (years) mean (sd) | 56.43 (13.78) | 56.48 (13.72) | 56.18 (14.09) | 0.622 | 56.46 (13.77) | 56.50 (13.67) | 56.30 (14.15) | 0.718 | 56.43 (13.83) | 56.46 (13.69) | 56.31 (14.34) | 0.787 |
| Gender | <0.001 | 0.883 | 0.831 | |||||||||
| Female | 1926 (49.01) | 1561 (47.53) | 365 (56.50) | 1872 (48.86) | 1467 (48.80) | 405 (49.09) | 1753 (48.79) | 1378 (48.88) | 375 (48.45) | |||
| Male | 2004 (50.99) | 1723 (52.47) | 281 (43.50) | 1959 (51.14) | 1539 (51.20) | 420 (50.91) | 1840 (51.21) | 1441 (51.12) | 399 (51.55) | |||
| Region | 0.019 | 0.054 | 0.086 | |||||||||
| East | 902 (22.95) | 748 (22.78) | 154 (23.84) | 885 (23.10) | 717 (23.85) | 168 (20.36) | 832 (23.16) | 672 (23.84) | 160 (20.67) | |||
| Midwest | 972 (24.73) | 839 (25.55) | 133 (20.59) | 943 (24.61) | 747 (24.85) | 196 (23.76) | 891 (24.80) | 708 (25.12) | 183 (23.64) | |||
| South | 1285 (32.70) | 1047 (31.88) | 238 (36.84) | 1259 (32.86) | 959 (31.90) | 300 (36.36) | 1179 (32.81) | 899 (31.89) | 280 (36.18) | |||
| West | 771 (19.62) | 650 (19.79) | 121 (18.73) | 744 (19.42) | 583 (19.39) | 161 (19.52) | 691 (19.23) | 540 (19.16) | 151 (19.51) | |||
| Year of diagnosis | 0.222 | 0.298 | 0.273 | |||||||||
| 2009 | 743 (18.91) | 628 (19.12) | 115 (17.80) | 732 (19.11) | 597 (19.86) | 135 (16.36) | 706 (19.65) | 577 (20.47) | 129 (16.67) | |||
| 2010 | 658 (16.74) | 543 (16.53) | 115 (17.80) | 646 (16.86) | 505 (16.80) | 141 (17.09) | 624 (17.37) | 488 (17.31) | 136 (17.57) | |||
| 2011 | 591 (15.04) | 493 (15.01) | 98 (15.17) | 582 (15.19) | 448 (14.90) | 134 (16.24) | 557 (15.50) | 427 (15.15) | 130 (16.80) | |||
| 2012 | 532 (13.54) | 429 (13.06) | 103 (15.94) | 509 (13.29) | 389 (12.94) | 120 (14.55) | 455 (12.66) | 352 (12.49) | 103 (13.31) | |||
| 2013 | 327 (8.32) | 276 (8.40) | 51 (7.89) | 321 (8.38) | 250 (8.32) | 71 (8.61) | 302 (8.41) | 235 (8.34) | 67 (8.66) | |||
| 2014 | 290 (7.38) | 243 (7.40) | 47 (7.28) | 280 (7.31) | 220 (7.32) | 60 (7.27) | 250 (6.96) | 195 (6.92) | 55 (7.11) | |||
| 2015 | 306 (7.79) | 250 (7.61) | 56 (8.67) | 297 (7.75) | 223 (7.42) | 74 (8.97) | 280 (7.79) | 208 (7.38) | 72 (9.30) | |||
| 2016 | 333 (8.47) | 289 (8.80) | 44 (6.81) | 323 (8.43) | 261 (8.68) | 62 (7.52) | 296 (8.24) | 239 (8.48) | 57 (7.36) | |||
| 2017 | 150 (3.82) | 133 (4.05) | 17 (2.63) | 141 (3.68) | 113 (3.76) | 28 (3.39) | 123 (3.42) | 98 (3.48) | 25 (3.23) | |||
| Chronic kidney disease | 170 (4.33) | 133 (4.05) | 37 (5.73) | 0.056 | 169 (4.41) | 135 (4.49) | 34 (4.12) | 0.647 | 155 (4.31) | 124 (4.40) | 31 (4.01) | 0.633 |
| Diabetes mellitus | 486 (12.37) | 400 (12.18) | 86 (13.31) | 0.424 | 469 (12.24) | 360 (11.98) | 109 (13.21) | 0.337 | 430 (11.97) | 329 (11.67) | 101 (13.05) | 0.295 |
| Cardiovascular Diseases | 349 (8.88) | 276 (8.40) | 73 (11.30) | 0.018 | 344 (8.98) | 264 (8.78) | 80 (9.70) | 0.416 | 326 (9.07) | 248 (8.80) | 78 (10.08) | 0.272 |
| COPD | 204 (5.19) | 153 (4.66) | 51 (7.89) | 0.001 | 201 (5.25) | 159 (5.29) | 42 (5.09) | 0.821 | 181 (5.04) | 143 (5.07) | 38 (4.91) | 0.854 |
| Liver disease | 81 (2.06) | 68 (2.07) | 13 (2.01) | 0.924 | 78 (2.04) | 57 (1.90) | 21 (2.55) | 0.242 | 73 (2.03) | 52 (1.84) | 21 (2.71) | 0.129 |
| Inflammatory Bowel disease | 33 (0.84) | 25 (0.76) | 8 (1.24) | 0.224 | 32 (0.84) | 22 (0.73) | 10 (1.21) | 0.179 | 30 (0.83) | 21 (0.74) | 9 (1.16) | 0.258 |
| Outcomes | n (%) | Total Person-Days | n/1000 Person-Days | n (%) | Total Person-Days | n/1000 Person-Days |
|---|---|---|---|---|---|---|
| Main analysis (surgery within 90 days) | ||||||
| Antibiotics in Pre-3-Months | ||||||
| No Use (n = 3284) | Use (n = 646) | |||||
| Progression | 282 (8.59) | 1,524,248 | 0.19 | 56 (8.67) | 292,890 | 0.19 |
| Antibiotics in Post-1-Month | ||||||
| No use (n = 3006) | Use (n = 825) | |||||
| Progression | 272 (9.05) | 2,106,838 | 0.13 | 68 (8.24) | 578,860 | 0.12 |
| Antibiotics in Post-3-Months | ||||||
| No use (n = 2819) | Use (n = 774) | |||||
| Progression | 271 (9.61) | 1,970,534 | 0.14 | 68 (8.79) | 541,630 | 0.13 |
| Progression | Unadjusted HR (95% CI) for Antibiotic Use (Ref = No Use) | Adjusted HR (95% CI) for Antibiotic Use (Ref = No Use) |
|---|---|---|
| Antibiotic use in Pre-3-Months | ||
| Main Analysis | ||
| propensity score (PS) weighting | 1.04 (0.78–1.38) | 0.81 (0.57–1.14) |
| Sensitivity Analysis 4: Stabilized PS weights | 0.67 (0.41–1.10) | |
| PS adjustment | 0.76 (0.55–1.04) | |
| Antibiotic use in Post-1-Month | ||
| Main Analysis | ||
| propensity score (PS) weighting | 0.91 (0.70–1.19) | 0.69 (0.51–0.92) |
| Sensitivity Analysis 4: Stabilized PS weights | 0.65 (0.48–0.88) | |
| PS adjustment | 0.69 (0.51–0.91) | |
| Antibiotic use in Post-3-Months | ||
| Main Analysis | ||
| Propensity score (PS) weighting | 0.91 (0.70–1.19) | 0.68 (0.51–0.91) |
| Sensitivity Analysis 4: Stabilized PS weights | 0.68 (0.51–0.91) | |
| PS adjustment | 0.65 (0.48–0.88) | |
| Outcomes | n (%) | Total Person-Days | n/1000 Person-Days | n (%) | Total Person-Days | n/1000 Person-Days | Unadjusted Hazard Ratios (95% CI) | Adjusted (Propensity Weighting) Hazard Ratios (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Antibiotics in Pre-3-Months | ||||||||
| Sensitivity Analysis 1: Alternative strategies for ascertaining melanoma cases | ||||||||
| Same day surgery as diagnosis | No use (n = 1087) | Use (n = 204) | ||||||
| Progression | 92 (8.46) | 519,124 | 0.18 | 17 (8.33) | 97,032 | 0.18 | 0.99 (0.59–1.65) | 0.68 (0.36–1.30) |
| Surgery within 15 days after diagnosis | No use (n = 1986) | Use (n = 384) | ||||||
| Progression | 168 (8.46) | 938,653 | 0.18 | 32 (8.33) | 181,702 | 0.18 | 0.99 (0.68–1.43) | 0.72 (0.46–1.15) |
| Sensitivity Analysis 2: Any healthcare encounter | No use (n = 3284) | Use (n = 646) | ||||||
| Any healthcare use | 3217 (97.96) | 114,797 | 28.02 | 643 (99.54) | 10,785 | 59.62 | 1.37 (1.26–1.49) | 1.14 (1.04–1.25) |
| Sensitivity Analysis 3: Falsification test | No use (n = 3284) | Use (n = 646) | ||||||
| Chronic pain | 1672 (50.91) | 1,060,266 | 1.58 | 384 (59.44) | 178,934 | 2.15 | 1.31 (1.17–1.47) | 1.02 (0.90–1.16) |
| Antibiotics in Post-1-Month | ||||||||
| Sensitivity Analysis 1: Alternative strategies for ascertaining melanoma cases | ||||||||
| Same day surgery as diagnosis | No use (n = 1035) | Use (n = 229) | ||||||
| Progression | 94 (9.08) | 724,739 | 0.13 | 17 (7.42) | 160,539 | 0.11 | 0.82 (0.49–1.38) | 0.64 (0.37–1.12) |
| Surgery within 15 days after diagnosis | No use (n = 1821) | Use (n = 498) | ||||||
| Progression | 157 (8.62) | 1,277,395 | 0.12 | 41 (8.23) | 350,429 | 0.12 | 0.95 (0.68–1.34) | 0.76 (0.52–1.09) |
| Sensitivity Analysis 2: Any healthcare encounter | No use (n = 3006) | Use (n = 825) | ||||||
| Any healthcare use | 2902 (96.54) | 158,468 | 18.31 | 803 (97.33) | 34,471 | 23.29 | 1.19 (1.10–1.29) | 1.09 (1.01–1.19) |
| Sensitivity Analysis 3: Falsification test | No use (n = 3006) | Use (n = 825) | ||||||
| Chronic pain | 1538 (51.16) | 1,465,928 | 1.05 | 451 (54.67) | 368,602 | 1.22 | 1.17 (1.06–1.31) | 1.08 (0.97–1.21) |
| Antibiotics in Post-3-Months | ||||||||
| Sensitivity Analysis 1: Alternative strategies for ascertaining melanoma cases | ||||||||
| Same day surgery as diagnosis | No use (n = 977) | Use (n = 213) | ||||||
| Progression | 94 (9.62) | 682,399 | 0.14 | 17 (7.98) | 148,859 | 0.11 | 0.83 (0.49–1.40) | 0.61 (0.35–1.06) |
| Surgery within 15 days after diagnosis | No use (n = 1721) | Use (n = 462) | ||||||
| Progression | 157 (9.12) | 1,204,395 | 0.13 | 41 (8.87) | 324,149 | 0.13 | 0.97 (0.69–1.37) | 0.72 (0.49–1.05) |
| Sensitivity Analysis 2: Any healthcare encounter | No use (n = 2819) | Use (n = 774) | ||||||
| Any healthcare use | 2779 (98.58) | 110,108 | 25.24 | 766 (98.97) | 23,625 | 32.42 | 1.21 (1.11–1.31) | 1.08 (1.00–1.18) |
| Sensitivity Analysis 3: Falsification test | No use (n = 2819) | Use (n = 774) | ||||||
| Chronic pain | 1508 (53.49) | 1,349,985 | 1.12 | 444 (57.36) | 336,359 | 1.32 | 1.19 (1.07–1.32) | 1.07 (0.95–1.19) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Acharya, M.; Kim, T.; Li, C. Broad-Spectrum Antibiotic Use and Disease Progression in Early-Stage Melanoma Patients: A Retrospective Cohort Study. Cancers 2021, 13, 4367. https://doi.org/10.3390/cancers13174367
Acharya M, Kim T, Li C. Broad-Spectrum Antibiotic Use and Disease Progression in Early-Stage Melanoma Patients: A Retrospective Cohort Study. Cancers. 2021; 13(17):4367. https://doi.org/10.3390/cancers13174367
Chicago/Turabian StyleAcharya, Mahip, Thomas Kim, and Chenghui Li. 2021. "Broad-Spectrum Antibiotic Use and Disease Progression in Early-Stage Melanoma Patients: A Retrospective Cohort Study" Cancers 13, no. 17: 4367. https://doi.org/10.3390/cancers13174367
APA StyleAcharya, M., Kim, T., & Li, C. (2021). Broad-Spectrum Antibiotic Use and Disease Progression in Early-Stage Melanoma Patients: A Retrospective Cohort Study. Cancers, 13(17), 4367. https://doi.org/10.3390/cancers13174367






