Current Status and Future Perspectives about Molecular Biomarkers of Nasopharyngeal Carcinoma
Abstract
Simple Summary
Abstract
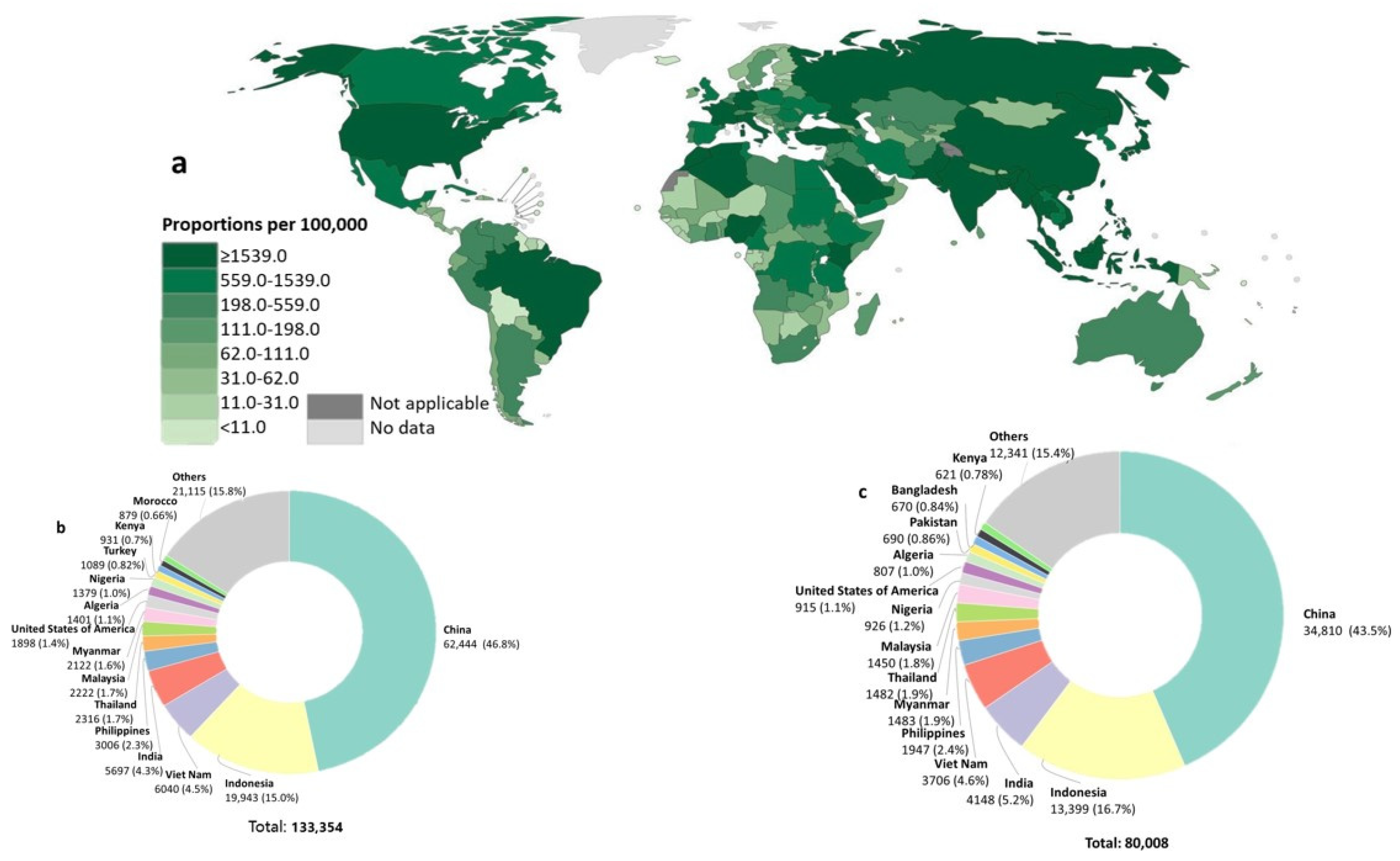
1. Introduction
2. Diagnostic and Prognostic Biomarker Discovery for NPC
3. NPC Diagnostic Biomarkers
3.1. NPC Associated Genomic Biomarkers
- (a)
- NPC associated polymorphism and HLA
- (b)
- Chromosome aberration
- (c)
- Copy number alterations
- (d)
- Signalling pathways
- (e)
- Viral (EBV and HPV)
3.2. NPC Associated mRNA Biomarkers
3.3. NPC Associated Protein Biomarkers
3.4. NPC Associated Metabolite Biomarkers
3.5. Cigarette Smoking Associated Biomarkers
4. NPC Prognosis Biomarkers
5. Future Perspective and Challenges
Author Contributions
Funding
Conflicts of Interest
References
- Dai, W.; Zheng, H.; Cheung, A.K.; Lung, M.L. Genetic and epigenetic landscape of nasopharyngeal carcinoma. Chin. Clin. Oncol. 2016, 5, 16. [Google Scholar] [CrossRef] [PubMed]
- Alotaibi, A.D.; Ahmed, H.G.; Elasbali, A.M. Nasopharyngeal cancer in Saudi Arabia: Epidemiology and possible risk factors. J. Oncol. Sci. 2019, 5, 23–30. [Google Scholar] [CrossRef]
- Le, Q.T.; Colevas, A.D.; O’Sullivan, B.; Lee, A.W.M.; Lee, N.; Ma, B.; Siu, L.L.; Waldron, J.; Lim, C.M.; Riaz, N.; et al. Current Treatment Landscape of Nasopharyngeal Carcinoma and Potential Trials Evaluating the Value of Immunotherapy. J. Natl. Cancer Inst. 2019, 111, 655–663. [Google Scholar] [CrossRef] [PubMed]
- GLOBOCAN. Estimated Number of Incident Cases Nasopharynx, Both Sexes, All Ages. Available online: https://gco.iarc.fr/ (accessed on 1 February 2021).
- Tsang, C.M.; Lui, V.W.Y.; Bruce, J.P.; Pugh, T.J.; Lo, K.W. Translational genomics of nasopharyngeal cancer. Semin. Cancer Biol. 2020, 61, 84–100. [Google Scholar] [CrossRef]
- Lee, K.T.; Tan, J.K.; Lam, A.K.; Gan, S.Y. MicroRNAs serving as potential biomarkers and therapeutic targets in nasopharyngeal carcinoma: A critical review. Crit. Rev. Oncol. Hematol. 2016, 103, 1–9. [Google Scholar] [CrossRef]
- GLOBOCAN. Nasopharynx Fact Sheets. Available online: https://gco.iarc.fr/today/data/factsheets/cancers/4-Nasopharynx-fact-sheet.pdf (accessed on 1 February 2021).
- Lu, T.; Guo, Q.; Lin, K.; Chen, H.; Chen, Y.; Xu, Y.; Lin, C.; Su, Y.; Chen, Y.; Chen, M.; et al. Circulating Epstein-Barr virus microRNAs BART7-3p and BART13-3p as novel biomarkers in nasopharyngeal carcinoma. Cancer Sci. 2020, 111, 1711–1723. [Google Scholar] [CrossRef]
- Mi, J.L.; Xu, M.; Liu, C.; Wang, R.S. Identification of novel biomarkers and small-molecule compounds for nasopharyngeal carcinoma with metastasis. Medicine 2020, 99, e21505. [Google Scholar] [CrossRef]
- Mahdavifar, N.; Ghoncheh, M.; Mohammadian-Hafshejani, A.; Khosravi, B.; Salehiniya, H. Epidemiology and Inequality in the Incidence and Mortality of Nasopharynx Cancer in Asia. Osong Public Health Res. Perspect. 2016, 7, 360–372. [Google Scholar] [CrossRef]
- Xia, W.X.; Zhang, H.B.; Shi, J.L.; Lu, X.; Wang, L.; Ye, Y.F.; Cao, K.J.; Qian, C.N.; Guo, X.; Xiang, Y.Q. A prognostic model predicts the risk of distant metastasis and death for patients with nasopharyngeal carcinoma based on pre-treatment serum C-reactive protein and N-classification. Eur. J. Cancer 2013, 49, 2152–2160. [Google Scholar] [CrossRef]
- Wong, T.S.; Gao, W.; Chan, J.Y.W. Biomarkers in Nasopharyngeal Carcinoma and Ionizing Radiation. In Biomarkers in Cancer, Biomarkers in Disease: Methods, Discoveries and Applications; Preedy, V., Patel, V., Eds.; Springer: Dordrecht, The Netherlands, 2015; pp. 875–890. [Google Scholar]
- Sireci, F.; Speciale, R.; Sorrentino, R.; Turri-Zanoni, M.; Nicolotti, M.; Canevari, F.R. Nasal packing in sphenopalatine artery bleeding: Therapeutic or harmful? Eur. Arch. Otorhinolaryngol. 2017, 274, 1501–1505. [Google Scholar] [CrossRef]
- Wei, W.I.; Sham, J.S. Nasopharyngeal carcinoma. Lancet 2005, 365, 2041–2054. [Google Scholar] [CrossRef]
- Sun, X.S.; Xiao, B.B.; Lu, Z.J.; Liu, S.L.; Chen, Q.Y.; Yuan, L.; Tang, L.Q.; Mai, H.Q. Stratification of Candidates for Induction Chemotherapy in Stage III-IV Nasopharyngeal Carcinoma: A Large Cohort Study Based on a Comprehensive Prognostic Model. Front. Oncol. 2020, 10, 255. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.W.; Ho, S.Y.; Lee, S.W.; Chen, C.C.; Litsu, S.; Huang, W.T.; Yang, C.C.; Lin, C.H.; Chen, H.Y.; Lin, L.C. Induction Chemotherapy Improved Long Term Outcomes in Stage IV Locoregional Advanced Nasopharyngeal Carcinoma. Int. J. Med. Sci. 2020, 17, 568–576. [Google Scholar] [CrossRef] [PubMed]
- Zhan, J.; Zhang, S.; Wei, X.; Fu, Y.; Zheng, J. Etiology and management of nasopharyngeal hemorrhage after radiotherapy for nasopharyngeal carcinoma. Cancer Manag. Res. 2019, 11, 2171–2178. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.P.; Chan, A.T.C.; Le, Q.T.; Blanchard, P.; Sun, Y.; Ma, J. Nasopharyngeal carcinoma. Lancet 2019, 394, 64–80. [Google Scholar] [CrossRef]
- Chen, Y.; Liu, M.Z.; Liang, S.B.; Zong, J.F.; Mao, Y.P.; Tang, L.L.; Guo, Y.; Lin, A.H.; Zeng, X.F.; Ma, J. Preliminary results of a prospective randomized trial comparing concurrent chemoradiotherapy plus adjuvant chemotherapy with radiotherapy alone in patients with locoregionally advanced nasopharyngeal carcinoma in endemic regions of china. Int. J. Radiat. Oncol. Biol. Phys. 2008, 71, 1356–1364. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Liu, W.; Li, H.; Zhao, Z.; Yang, Y.; Xiao, H.; Song, Y.; Luo, B. Conservation and polymorphism of EBV RPMS1 gene in EBV-associated tumors and healthy individuals from endemic and non-endemic nasopharyngeal carcinoma areas in China. Virus Res. 2018, 250, 75–80. [Google Scholar] [CrossRef]
- Fu, J.; Li, Z.; Li, N. The association between COX-2 gene rs5275 polymorphism and Nasopharyngeal carcinoma risk. Pathol. Res. Pract. 2018, 214, 1579–1582. [Google Scholar] [CrossRef]
- Niu, Y.; Zhou, G.; Wang, Y.; Qin, J.; Ping, J.; Zhang, Q.; Han, B.W.; Liu, Y.X.; Yang, C.; Zhai, Y.; et al. Association of MCP-1 promoter polymorphism with susceptibility to nasopharyngeal carcinoma. J. Cell Biochem. 2019, 120, 6661–6670. [Google Scholar] [CrossRef]
- Wang, R.; Qin, H.M.; Qin, L.; Wei, J.X.; Wei, Y.X.; Wang, J.L. Genetic association of promoter in GRP78 gene with nasopharyngeal carcinoma in a Chinese population. Int. J. Clin. Oncol. 2019, 24, 359–365. [Google Scholar] [CrossRef]
- Ning, S.; Yao, M.; Wu, Y.; Zhou, X.; Zhong, C.; Yan, K.; Wei, Z.; Xie, Y. Correlation of variable repeat number in the neck regions of DC-SIGN and DC-SIGNR with susceptibility to nasopharyngeal carcinoma in a Chinese population. Cancer Manag. Res. 2018, 10, 3193–3198. [Google Scholar] [CrossRef]
- Li, S.; Lu, Z.; Yao, M.; Ning, S.; Wu, Y.; Zhou, X.; Zhong, C.; Yan, K.; Xie, Y.; Wei, Z. Association of Single-Nucleotide Polymorphisms in DC-SIGN with Nasopharyngeal Carcinoma Susceptibility. Dis. Markers 2017, 2017, 6309754. [Google Scholar] [CrossRef]
- Lu, S.J.; Day, N.E.; Degos, L.; Lepage, V.; Wang, P.C.; Chan, S.H.; Simons, M.; McKnight, B.; Easton, D.; Zeng, Y.; et al. Linkage of a nasopharyngeal carcinoma susceptibility locus to the HLA region. Nature 1990, 346, 470–471. [Google Scholar] [CrossRef] [PubMed]
- Rietveld, C.A.; Medland, S.E.; Derringer, J.; Yang, J.; Esko, T.; Martin, N.W.; Westra, H.J.; Shakhbazov, K.; Abdellaoui, A.; Agrawal, A.; et al. GWAS of 126,559 individuals identifies genetic variants associated with educational attainment. Science 2013, 340, 1467–1471. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Wei, X.; Wu, B.; Su, J.; Tan, W.; Yang, K. Tumor-educated platelet miR-34c-3p and miR-18a-5p as potential liquid biopsy biomarkers for nasopharyngeal carcinoma diagnosis. Cancer Manag. Res. 2019, 11, 3351–3360. [Google Scholar] [CrossRef]
- Lo, K.W.; Chung, G.T.; To, K.F. Deciphering the molecular genetic basis of NPC through molecular, cytogenetic, and epigenetic approaches. Semin. Cancer Biol. 2012, 22, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.S.H. Construction of evolutionary tree models for nasopharyngeal carcinoma using comparative genomic hybridization data. Cancer Genet. Cytogenet. 2006, 168, 105–108. [Google Scholar]
- Huang, D.P.; Lo, K.W.; van Hasselt, C.A.; Woo, J.K.; Choi, P.H.; Leung, S.F.; Cheung, S.T.; Cairns, P.; Sidransky, D.; Lee, J.C. A region of homozygous deletion on chromosome 9p21-22 in primary nasopharyngeal carcinoma. Cancer Res. 1994, 54, 4003–4006. [Google Scholar]
- Rahman, S.; Subroto, H.; Budiman, B.; Asri, A.; Bachtiar, H. Expression of epidermal growth factor receptor in advance stage nonkeratinizing nasopharyngeal carcinoma in West Sumatra, Indonesia. Arch. Oncol. 2018, 24, 20–23. [Google Scholar] [CrossRef][Green Version]
- Chen, S.; Youhong, T.; Tan, Y.; He, Y.; Ban, Y.; Cai, J.; Li, X.; Xiong, W.; Zeng, Z.; Li, G.; et al. EGFR-PKM2 signaling promotes the metastatic potential of nasopharyngeal carcinoma through induction of FOSL1 and ANTXR2. Carcinogenesis 2020, 41, 723–733. [Google Scholar] [CrossRef]
- Yip, T.T.; Ngan, R.K.; Fong, A.H.; Law, S.C. Application of circulating plasma/serum EBV DNA in the clinical management of nasopharyngeal carcinoma. Oral Oncol. 2014, 50, 527–538. [Google Scholar] [CrossRef]
- Chan, K.C.A.; Woo, J.K.S.; King, A.; Zee, B.C.Y.; Lam, W.K.J.; Chan, S.L.; Chu, S.W.I.; Mak, C.; Tse, I.O.L.; Leung, S.Y.M.; et al. Analysis of Plasma Epstein-Barr Virus DNA to Screen for Nasopharyngeal Cancer. New Engl. J. Med. 2017, 377, 513–522. [Google Scholar] [CrossRef]
- Shen, J.J.; Niu, W.N.; Zhou, M.; Zhou, F.; Zhang, H.Y.; Wang, L. Association of Epstein Barr virus A73 gene polymorphism with nasopharyngeal carcinoma. Genet. Test. Mol. Biomark. 2015, 19, 187–190. [Google Scholar] [CrossRef]
- Xu, M.; Yao, Y.; Chen, H.; Zhang, S.; Cao, S.M.; Zhang, Z.; Luo, B.; Liu, Z.; Li, Z.; Xiang, T.; et al. Genome sequencing analysis identifies Epstein-Barr virus subtypes associated with high risk of nasopharyngeal carcinoma. Nat. Genet. 2019, 51, 1131–1136. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.C.; Chen, G.H.; Chen, Y.H.; Liao, W.L.; Liu, C.Y.; Chang, K.P.; Chang, Y.S.; Chen, S.J. MicroRNA deregulation and pathway alterations in nasopharyngeal carcinoma. Br. J. Cancer 2009, 100, 1002–1011. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Luo, H.N.; Tian, W.D.; Lu, J.; Li, G.; Wang, L.; Zhang, B.; Liang, B.J.; Peng, X.H.; Lin, S.X.; et al. Diagnostic and prognostic value of plasma microRNA deregulation in nasopharyngeal carcinoma. Cancer Biol. Ther. 2013, 14, 1133–1142. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.; Guo, X.; Zhou, H.; Zhang, W.; Zeng, Z.; Liao, Q.; Li, X.; Xiang, B.; Yang, J.; Ma, J.; et al. SPLUNC1 regulates cell progression and apoptosis through the miR-141-PTEN/p27 pathway, but is hindered by LMP1. PLoS ONE 2013, 8, e56929. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Deng, T.; Li, X.; Liu, H.; Zhou, H.; Ma, J.; Wu, M.; Zhou, M.; Shen, S.; Li, X.; et al. microRNA-141 is involved in a nasopharyngeal carcinoma-related genes network. Carcinogenesis 2010, 31, 559–566. [Google Scholar] [CrossRef]
- Zhang, H.; Zou, X.; Wu, L.; Zhang, S.; Wang, T.; Liu, P.; Zhu, W.; Zhu, J. Identification of a 7-microRNA signature in plasma as promising biomarker for nasopharyngeal carcinoma detection. Cancer Med. 2020, 9, 1230–1241. [Google Scholar] [CrossRef]
- He, B.; Zeng, J.; Chao, W.; Chen, X.; Huang, Y.; Deng, K.; Huang, Z.; Li, J.; Dai, M.; Chen, S.; et al. Serum long non-coding RNAs MALAT1, AFAP1-AS1 and AL359062 as diagnostic and prognostic biomarkers for nasopharyngeal carcinoma. Oncotarget 2017, 8, 41166–41177. [Google Scholar] [CrossRef]
- Hui, K.F.; Chan, T.F.; Yang, W.; Shen, J.J.; Lam, K.P.; Kwok, H.; Sham, P.C.; Tsao, S.W.; Kwong, D.L.; Lung, M.L.; et al. High risk Epstein-Barr virus variants characterized by distinct polymorphisms in the EBER locus are strongly associated with nasopharyngeal carcinoma. Int. J. Cancer 2019, 144, 3031–3042. [Google Scholar] [CrossRef]
- Xu, Y.J.; Zhou, R.; Zong, J.F.; Lin, W.S.; Tong, S.; Guo, Q.J.; Lin, C.; Lin, S.J.; Chen, Y.X.; Chen, M.R.; et al. Epstein-Barr virus-coded miR-BART13 promotes nasopharyngeal carcinoma cell growth and metastasis via targeting of the NKIRAS2/NF-κB pathway. Cancer Lett. 2019, 447, 33–40. [Google Scholar] [CrossRef]
- Lyu, X.; Wang, J.; Guo, X.; Wu, G.; Jiao, Y.; Faleti, O.D.; Liu, P.; Liu, T.; Long, Y.; Chong, T.; et al. EBV-miR-BART1-5P activates AMPK/mTOR/HIF1 pathway via a PTEN independent manner to promote glycolysis and angiogenesis in nasopharyngeal carcinoma. PLoS Pathog. 2018, 14, e1007484. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.C.; Chien, K.Y.; Tsang, N.M.; Chang, K.P.; Hao, S.P.; Tsao, C.H.; Chang, Y.S.; Yu, J.S. Cancer cell-secreted proteomes as a basis for searching potential tumor markers: Nasopharyngeal carcinoma as a model. Proteomics 2005, 5, 3173–3182. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Z.; Li, G.; Chen, Y.; Li, M.; Peng, F.; Li, C.; Li, F.; Yu, Y.; Ouyang, Y.; Xiao, Z.; et al. Quantitative proteomic analysis of formalin-fixed and paraffin-embedded nasopharyngeal carcinoma using iTRAQ labeling, two-dimensional liquid chromatography, and tandem mass spectrometry. J. Histochem. Cytochem. 2010, 58, 517–527. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Li, C.; Li, D.; Xie, Y.; Shi, J.; Li, G.; Guan, Y.; Li, M.; Zhang, P.; Peng, F.; et al. Periostin, a stroma-associated protein, correlates with tumor invasiveness and progression in nasopharyngeal carcinoma. Clin. Exp. Metastasis 2012, 29, 865–877. [Google Scholar] [CrossRef]
- Li, X.; Fasano, R.; Wang, E.; Yao, K.T.; Marincola, F.M. HLA associations with nasopharyngeal carcinoma. Curr. Mol. Med. 2009, 9, 751–765. [Google Scholar] [CrossRef]
- Li, M.X.; Xiao, Z.Q.; Liu, Y.F.; Chen, Y.H.; Li, C.; Zhang, P.F.; Li, M.Y.; Li, F.; Peng, F.; Duan, C.J.; et al. Quantitative proteomic analysis of differential proteins in the stroma of nasopharyngeal carcinoma and normal nasopharyngeal epithelial tissue. J. Cell Biochem. 2009, 106, 570–579. [Google Scholar] [CrossRef]
- Ge, S.; Mao, Y.; Yi, Y.; Xie, D.; Chen, Z.; Xiao, Z. Comparative proteomic analysis of secreted proteins from nasopharyngeal carcinoma-associated stromal fibroblasts and normal fibroblasts. Exp. Ther. Med. 2012, 3, 857–860. [Google Scholar] [CrossRef][Green Version]
- Lin, S.J.; Chang, K.P.; Hsu, C.W.; Chi, L.M.; Chien, K.Y.; Liang, Y.; Tsai, M.H.; Lin, Y.T.; Yu, J.S. Low-molecular-mass secretome profiling identifies C-C motif chemokine 5 as a potential plasma biomarker and therapeutic target for nasopharyngeal carcinoma. J. Proteom. 2013, 94, 186–201. [Google Scholar] [CrossRef]
- Chang, Y.H.; Wu, C.C.; Chang, K.P.; Yu, J.S.; Chang, Y.C.; Liao, P.C. Cell secretome analysis using hollow fiber culture system leads to the discovery of CLIC1 protein as a novel plasma marker for nasopharyngeal carcinoma. J. Proteome Res. 2009, 8, 5465–5474. [Google Scholar] [CrossRef] [PubMed]
- Hao, S.P.; Tsang, N.M.; Chang, K.P.; Ueng, S.H. Molecular diagnosis of nasopharyngeal carcinoma: Detecting LMP-1 and EBNA by nasopharyngeal swab. Otolaryngol. Head Neck Surg. 2004, 131, 651–654. [Google Scholar] [CrossRef] [PubMed]
- Banko, A.V.; Lazarevic, I.B.; Folic, M.M.; Djukic, V.B.; Cirkovic, A.M.; Karalic, D.Z.; Cupic, M.D.; Jovanovic, T.P. Characterization of the Variability of Epstein-Barr Virus Genes in Nasopharyngeal Biopsies: Potential Predictors for Carcinoma Progression. PLoS ONE 2016, 11, e0153498. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Ji, M.; Cheng, W.; Wu, B.; Du, Y.; Cao, S. Assessment of the Long-term Diagnostic Performance of a New Serological Screening Scheme in Large-scale Nasopharyngeal Carcinoma Screening. J. Cancer 2018, 9, 2093–2097. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Ji, M.F.; Huang, Q.H.; Fang, F.; Liu, Q.; Jia, W.H.; Guo, X.; Xie, S.H.; Chen, F.; Liu, Y.; et al. Two Epstein-Barr virus-related serologic antibody tests in nasopharyngeal carcinoma screening: Results from the initial phase of a cluster randomized controlled trial in Southern China. Am. J. Epidemiol. 2013, 177, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Tang, F.; Xie, C.; Huang, D.; Wu, Y.; Zeng, M.; Yi, L.; Wang, Y.; Mei, W.; Cao, Y.; Sun, L. Novel potential markers of nasopharyngeal carcinoma for diagnosis and therapy. Clin. Biochem. 2011, 44, 711–718. [Google Scholar] [CrossRef]
- Yi, L.; Dong, N.; Shi, S.; Deng, B.; Yun, Y.; Yi, Z.; Zhang, Y. Metabolomic identification of novel biomarkers of nasopharyngeal carcinoma. RSC Adv. 2014, 4, 59094–59101. [Google Scholar] [CrossRef]
- Yi, L.; Song, C.; Hu, Z.; Yang, L.; Xiao, L.; Yi, B.; Jiang, W.; Cao, Y.; Sun, L. A metabolic discrimination model for nasopharyngeal carcinoma and its potential role in the therapeutic evaluation of radiotherapy. Metabolomics 2014, 10, 697–708. [Google Scholar] [CrossRef]
- Wang, J.L.; Wang, X.; Yang, D.; Shi, W.J. Association between 8473T>C polymorphism in the cyclooxygenase-2 gene and the risk of nasopharyngeal carcinoma. Int. J. Clin. Exp. Pathol. 2015, 8, 7441–7445. [Google Scholar]
- Simons, M.J.; Wee, G.B.; Day, N.E.; Morris, P.J.; Shanmugaratnam, K.; De-Thé, G.B. Immunogenetic aspects of nasopharyngeal carcinoma: I. Differences in HL-A antigen profiles between patients and control groups. Int. J. Cancer 1974, 13, 122–134. [Google Scholar] [CrossRef]
- Hu, S.P.; Day, N.E.; Li, D.R.; Luben, R.N.; Cai, K.L.; Ou-Yang, T.; Li, B.; Lu, X.Z.; Ponder, B.A. Further evidence for an HLA-related recessive mutation in nasopharyngeal carcinoma among the Chinese. Br. J. Cancer 2005, 92, 967–970. [Google Scholar] [CrossRef] [PubMed]
- Ooft, M.L.; van Ipenburg, J.; van de Loo, R.J.M.; de Jong, R.; Moelans, C.B.; de Bree, R.; de Herdt, M.J.I.; Koljenović, S.; Baatenburg de Jong, R.; Hardillo, J.; et al. Differences in cancer gene copy number alterations between Epstein-Barr virus-positive and Epstein-Barr virus-negative nasopharyngeal carcinoma. Head Neck 2018, 40, 1986–1998. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.T.; Chen, M.K.; Huang, C.C.; Huang, C.Y. Prognostic Value of Molecular Markers and Implication for Molecular Targeted Therapies in Nasopharyngeal Carcinoma: An Update in an Era of New Targeted Molecules Development. World J. Oncol. 2015, 6, 243–261. [Google Scholar] [CrossRef]
- Jo, M.; Stolz, D.B.; Esplen, J.E.; Dorko, K.; Michalopoulos, G.K.; Strom, S.C. Cross-talk between epidermal growth factor receptor and c-Met signal pathways in transformed cells. J. Biol. Chem. 2000, 275, 8806–8811. [Google Scholar] [CrossRef] [PubMed]
- Paul, P.; Deka, H.; Malakar, A.K.; Halder, B.; Chakraborty, S. Nasopharyngeal carcinoma: Understanding its molecular biology at a fine scale. Eur. J. Cancer Prev. 2018, 27, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Tao, Q.; Chan, A.T. Nasopharyngeal carcinoma: Molecular pathogenesis and therapeutic developments. Expert Rev. Mol. Med. 2007, 9, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Pathmanathan, R.; Prasad, U.; Chandrika, G.; Sadler, R.; Flynn, K.; Raab-Traub, N. Undifferentiated, nonkeratinizing, and squamous cell carcinoma of the nasopharynx. Variants of Epstein-Barr virus-infected neoplasia. Am. J. Pathol. 1995, 146, 1355–1367. [Google Scholar] [PubMed]
- Tsao, S.W.; Tsang, C.M.; Lo, K.W. Epstein-Barr virus infection and nasopharyngeal carcinoma. Philos. Trans. R Soc. Lond. B Biol. Sci. 2017, 372, 20160270. [Google Scholar] [CrossRef]
- Chan, K.C.; Hung, E.C.; Woo, J.K.; Chan, P.K.; Leung, S.F.; Lai, F.P.; Cheng, A.S.; Yeung, S.W.; Chan, Y.W.; Tsui, T.K.; et al. Early detection of nasopharyngeal carcinoma by plasma Epstein-Barr virus DNA analysis in a surveillance program. Cancer 2013, 119, 1838–1844. [Google Scholar] [CrossRef]
- Donnelly, D., 3rd; Aung, P.P.; Jour, G. The “-OMICS” facet of melanoma: Heterogeneity of genomic, proteomic and metabolomic biomarkers. Semin. Cancer Biol. 2019, 59, 165–174. [Google Scholar] [CrossRef]
- Tam, V.; Patel, N.; Turcotte, M.; Bossé, Y.; Paré, G.; Meyre, D. Benefits and limitations of genome-wide association studies. Nat. Rev. Genet. 2019, 20, 467–484. [Google Scholar] [CrossRef]
- Janvilisri, T. Omics-based identification of biomarkers for nasopharyngeal carcinoma. Dis. Markers 2015, 2015, 762128. [Google Scholar] [CrossRef]
- Ruuskanen, M.; Irjala, H.; Minn, H.; Vahlberg, T.; Randen-Brady, R.; Hagström, J.; Syrjänen, S.; Leivo, I. Epstein-Barr virus and human papillomaviruses as favorable prognostic factors in nasopharyngeal carcinoma: A nationwide study in Finland. Head Neck 2019, 41, 349–357. [Google Scholar] [CrossRef]
- Luo, F.F.; Li, Z.Y.; Huang, S.N.; Chen, G.; Xie, T.T.; Li, Y.Q.; Xing, W.W.; Li, W.Y.; Lu, Y.K.; Ding, H. Prevalence of human papillomavirus in patients with nasopharyngeal carcinoma: A meta-analysis. Int. J. Clin. Exp. Med. 2017, 10, 9837–9847. [Google Scholar]
- Huang, W.B.; Chan, J.Y.W.; Liu, D.L. Human papillomavirus and World Health Organization type III nasopharyngeal carcinoma: Multicenter study from an endemic area in Southern China. Cancer 2018, 124, 530–536. [Google Scholar] [CrossRef] [PubMed]
- Stenmark, M.H.; McHugh, J.B.; Schipper, M.; Walline, H.M.; Komarck, C.; Feng, F.Y.; Worden, F.P.; Wolf, G.T.; Chepeha, D.B.; Prince, M.E.; et al. Nonendemic HPV-positive nasopharyngeal carcinoma: Association with poor prognosis. Int. J. Radiat. Oncol. Biol. Phys. 2014, 88, 580–588. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, W.R.; Srivastava, A.; Chundury, A.; Cosper, P.; Contreras, J.; Gay, H.A.; Parikh, P.J.; Wang, X.; Gondim, D.; Chernock, R.; et al. HPV-Positive EBV-Negative Nasopharyngeal Cancer: Prevalence and Impact on Outcomes in a Non-Endemic Population. Int. J. Radiat. Oncol. Biol. Phys. 2020, 106, 1170. [Google Scholar] [CrossRef]
- Lin, Z.; Khong, B.; Kwok, S.; Cao, H.; West, R.B.; Le, Q.T.; Kong, C.S. Human papillomavirus 16 detected in nasopharyngeal carcinomas in white Americans but not in endemic Southern Chinese patients. Head Neck 2014, 36, 709–714. [Google Scholar] [CrossRef]
- Dogan, S.; Hedberg, M.L.; Ferris, R.L.; Rath, T.J.; Assaad, A.M.; Chiosea, S.I. Human papillomavirus and Epstein-Barr virus in nasopharyngeal carcinoma in a low-incidence population. Head Neck 2014, 36, 511–516. [Google Scholar] [CrossRef]
- Robinson, M.; Suh, Y.E.; Paleri, V.; Devlin, D.; Ayaz, B.; Pertl, L.; Thavaraj, S. Oncogenic human papillomavirus-associated nasopharyngeal carcinoma: An observational study of correlation with ethnicity, histological subtype and outcome in a UK population. Infect. Agents Cancer 2013, 8, 30. [Google Scholar] [CrossRef]
- Laantri, N.; Attaleb, M.; Kandil, M.; Naji, F.; Mouttaki, T.; Dardari, R.; Belghmi, K.; Benchakroun, N.; El Mzibri, M.; Khyatti, M. Human papillomavirus detection in moroccan patients with nasopharyngeal carcinoma. Infect. Agents Cancer 2011, 6, 3. [Google Scholar] [CrossRef]
- Mirzamani, N.; Salehian, P.; Farhadi, M.; Tehran, E.A. Detection of EBV and HPV in nasopharyngeal carcinoma by in situ hybridization. Exp. Mol. Pathol. 2006, 81, 231–234. [Google Scholar] [CrossRef]
- Kano, M.; Kondo, S.; Wakisaka, N.; Moriyama-Kita, M.; Nakanishi, Y.; Endo, K.; Murono, S.; Nakamura, H.; Yoshizaki, T. The influence of human papillomavirus on nasopharyngeal carcinoma in Japan. Auris Nasus Larynx 2017, 44, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Altekin, I.; Taş, A.; Yalcin, O.; Guven, S.G.; Aslan, Z.; Adali, M.K.; Karasalihoğlu, A.R. Frequency of Epstein-Barr virus and human papilloma virus in patients with nasopharyngeal carcinoma. Eur. Arch. Otorhinolaryngol. 2020, 277, 2041–2047. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.; Xiang, J.; Wu, M.; Xiong, W.; Tang, H.; Deng, M.; Li, X.; Liao, Q.; Su, B.; Luo, Z.; et al. Circulating miR-17, miR-20a, miR-29c, and miR-223 combined as non-invasive biomarkers in nasopharyngeal carcinoma. PLoS ONE 2012, 7, e46367. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.L.; Peng, X.H.; Zhao, F.P.; Liu, X.; Lu, J.; Wang, L.; Li, G.; Chen, H.H.; Li, X.P. MicroRNA-378 functions as an onco-miR in nasopharyngeal carcinoma by repressing TOB2 expression. Int. J. Oncol. 2014, 44, 1215–1222. [Google Scholar] [CrossRef]
- Wen, W.; Mai, S.J.; Lin, H.X.; Zhang, M.Y.; Huang, J.L.; Hua, X.; Lin, C.; Long, Z.Q.; Lu, Z.J.; Sun, X.Q.; et al. Identification of two microRNA signatures in whole blood as novel biomarkers for diagnosis of nasopharyngeal carcinoma. J. Transl. Med. 2019, 17, 186. [Google Scholar] [CrossRef]
- Best, M.G.; Sol, N.; Kooi, I.; Tannous, J.; Westerman, B.A.; Rustenburg, F.; Schellen, P.; Verschueren, H.; Post, E.; Koster, J.; et al. RNA-Seq of Tumor-Educated Platelets Enables Blood-Based Pan-Cancer, Multiclass, and Molecular Pathway Cancer Diagnostics. Cancer Cell 2015, 28, 666–676. [Google Scholar] [CrossRef]
- Zhao, C.X.; Zhu, W.; Ba, Z.Q.; Xu, H.J.; Liu, W.D.; Zhu, B.; Wang, L.; Song, Y.J.; Yuan, S.; Ren, C.P. The regulatory network of nasopharyngeal carcinoma metastasis with a focus on EBV, lncRNAs and miRNAs. Am. J. Cancer Res. 2018, 8, 2185–2209. [Google Scholar]
- Hayes, J.; Peruzzi, P.P.; Lawler, S. MicroRNAs in cancer: Biomarkers, functions and therapy. Trends Mol. Med. 2014, 20, 460–469. [Google Scholar] [CrossRef]
- Wang, H.; Peng, R.; Wang, J.; Qin, Z.; Xue, L. Circulating microRNAs as potential cancer biomarkers: The advantage and disadvantage. Clin. Epigenetics 2018, 10, 59. [Google Scholar] [CrossRef] [PubMed]
- Chan, Y.K.; Zhang, H.; Liu, P.; Tsao, S.W.; Lung, M.L.; Mak, N.K.; Wong, R.N.S.; Yue, P.Y.K. Proteomic analysis of exosomes from nasopharyngeal carcinoma cell identifies intercellular transfer of angiogenic proteins. Int. J. Cancer 2015, 137, 1830–1841. [Google Scholar] [CrossRef] [PubMed]
- Li, X.M.; Huang, W.G.; Yi, H.; Cheng, A.L.; Xiao, Z.Q. Proteomic analysis to identify cytokeratin 18 as a novel biomarker of nasopharyngeal carcinoma. J. Cancer Res. Clin. Oncol. 2009, 135, 1763–1775. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.Y.; Chang, Y.H.; Chang, Y.C.; Liao, P.C. Proteomics analysis of nasopharyngeal carcinoma cell secretome using a hollow fiber culture system and mass spectrometry. J. Proteome Res. 2009, 8, 380–389. [Google Scholar] [CrossRef]
- Coghill, A.E.; Hsu, W.L.; Pfeiffer, R.M.; Juwana, H.; Yu, K.J.; Lou, P.J.; Wang, C.P.; Chen, J.Y.; Chen, C.J.; Middeldorp, J.M.; et al. Epstein-Barr virus serology as a potential screening marker for nasopharyngeal carcinoma among high-risk individuals from multiplex families in Taiwan. Cancer Epidemiol. Biomarkers Prev. 2014, 23, 1213–1219. [Google Scholar] [CrossRef] [PubMed]
- Tay, J.K.; Chan, S.H.; Lim, C.M.; Siow, C.H.; Goh, H.L.; Loh, K.S. The Role of Epstein-Barr Virus DNA Load and Serology as Screening Tools for Nasopharyngeal Carcinoma. Otolaryngol. Head Neck Surg. 2016, 155, 274–280. [Google Scholar] [CrossRef]
- Tan, L.P.; Tan, G.W.; Sivanesan, V.M.; Goh, S.L.; Ng, X.J.; Lim, C.S.; Kim, W.R.; Mohidin, T.; Mohd Dali, N.S.; Ong, S.H.; et al. Malaysian Nasopharyngeal Carcinoma Study Group. Systematic comparison of plasma EBV DNA, anti-EBV antibodies and miRNA levels for early detection and prognosis of nasopharyngeal carcinoma. Int. J. Cancer 2020, 146, 2336–2347. [Google Scholar] [CrossRef]
- Chang, C.; Middeldorp, J.; Yu, K.J.; Juwana, H.; Hsu, W.L.; Lou, P.J.; Wang, C.P.; Chen, J.Y.; Liu, M.Y.; Pfeiffer, R.M.; et al. Characterization of ELISA detection of broad-spectrum anti-Epstein-Barr virus antibodies associated with nasopharyngeal carcinoma. J. Med. Virol. 2013, 85, 524–529. [Google Scholar] [CrossRef]
- Manes, N.P.; Nita-Lazar, A. Application of targeted mass spectrometry in bottom-up proteomics for systems biology research. J. Proteom. 2018, 189, 75–90. [Google Scholar] [CrossRef] [PubMed]
- Aslam, B.; Basit, M.; Nisar, M.A.; Khurshid, M.; Rasool, M.H. Proteomics: Technologies and Their Applications. J. Chromatogr. Sci. 2017, 55, 182–196. [Google Scholar] [CrossRef] [PubMed]
- Gosho, M.; Nagashima, K.; Sato, Y. Study designs and statistical analyses for biomarker research. Sensors 2012, 12, 8966–8986. [Google Scholar] [CrossRef] [PubMed]
- Rinschen, M.M.; Ivanisevic, J.; Giera, M.; Siuzdak, G. Identification of bioactive metabolites using activity metabolomics. Nat. Rev. Mol. Cell Biol. 2019, 20, 353–367. [Google Scholar] [CrossRef]
- Guijas, C.; Montenegro-Burke, J.R.; Warth, B.; Spilker, M.E.; Siuzdak, G. Metabolomics activity screening for identifying metabolites that modulate phenotype. Nat. Biotechnol. 2018, 36, 316–320. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.T.; Adami, H.O. The enigmatic epidemiology of nasopharyngeal carcinoma. Cancer Epidemiol. Biomark. Prev. 2006, 15, 1765–1777. [Google Scholar] [CrossRef]
- Lin, J.C.; Chen, K.Y.; Wang, W.Y.; Jan, J.S.; Liang, W.M.; Tsai, C.S.; Wei, Y.H. Detection of Epstein-Barr virus DNA in the peripheral-blood cells of patients with nasopharyngeal carcinoma: Relationship to distant metastasis and survival. J. Clin. Oncol. 2001, 19, 2607–2615. [Google Scholar] [CrossRef]
- Yuan, J.M.; Wang, X.L.; Xiang, Y.B.; Gao, Y.T.; Ross, R.K.; Yu, M.C. Non-dietary risk factors for nasopharyngeal carcinoma in Shanghai, China. Int. J. Cancer 2000, 85, 364–369. [Google Scholar] [CrossRef]
- Cheng, Y.J.; Hildesheim, A.; Hsu, M.M.; Chen, I.H.; Brinton, L.A.; Levine, P.H.; Chen, C.J.; Yang, C.S. Cigarette smoking, alcohol consumption and risk of nasopharyngeal carcinoma in Taiwan. Cancer Causes Control 1999, 10, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Mutirangura, A.; Pornthanakasem, W.; Theamboonlers, A.; Sriuranpong, V.; Lertsanguansinchi, P.; Yenrudi, S.; Voravud, N.; Supiyaphun, P.; Poovorawan, Y. Epstein-Barr viral DNA in serum of patients with nasopharyngeal carcinoma. Clin. Cancer Res. 1998, 4, 665–669. [Google Scholar] [PubMed]
- Kurniawan, A.; Risanti, E.D.; Suhda, S.; Rinonce, H.T.; Dwianingsih, E.K.; Fachiroh, J. WIF1 Qualitative-Methylation from Peripheral Blood Could Not Be Used as Biomarker for The Risk of Nasopharyngeal Carcinoma or Smoking Behavior in Yogyakarta Panel. Indones. Biomed. J. 2019, 11, 273–278. [Google Scholar] [CrossRef]
- Risanti, E.D.; Kurniawan, A.; Wahyuningsih, L.; Dwianingsih, E.K.; Rinonce, H.T.; Fachiroh, J. Association of Peripheral Blood RASSF1A and CDKN2A Methylation Status with Smoking Behaviour in Nasopharyngeal Carcinoma. Indones. Biomed. J. 2018, 10, 123–127. [Google Scholar] [CrossRef]
- Pfeifer, G.P.; Denissenko, M.F.; Olivier, M.; Tretyakova, N.; Hecht, S.S.; Hainaut, P. Tobacco smoke carcinogens, DNA damage and p53 mutations in smoking-associated cancers. Oncogene 2002, 21, 7435–7451. [Google Scholar] [CrossRef] [PubMed]
- Dai, W.; Cheung, A.K.; Ko, J.M.; Cheng, Y.; Zheng, H.; Ngan, R.K.; Ng, W.T.; Lee, A.W.; Yau, C.C.; Lee, V.H.; et al. Comparative methylome analysis in solid tumors reveals aberrant methylation at chromosome 6p in nasopharyngeal carcinoma. Cancer Med. 2015, 4, 1079–1090. [Google Scholar] [CrossRef]
- Deep, J.S.; Sidhu, S.; Chandel, A.; Thapliyal, S.; Garg, C. Aberrant Methylation in Promoters of GSTP1, p16, p14, and RASSF1A Genes in Smokers of North India. ISRN Pulmonol. 2012, 2012, 247631. [Google Scholar] [CrossRef]
- Zou, J.; Sun, Q.; Akiba, S.; Yuan, Y.; Zha, Y.; Tao, Z.; Wei, L.; Sugahara, T. A case-control study of nasopharyngeal carcinoma in the high background radiation areas of Yangjiang, China. J. Radiat. Res. 2000, 41, 53–62. [Google Scholar] [CrossRef]
- Ng, T.P. A case-referent study of cancer of the nasal cavity and sinuses in Hong Kong. Int. J. Epidemiol. 1986, 15, 171–175. [Google Scholar] [CrossRef]
- Xu, F.H.; Xiong, D.; Xu, Y.F.; Cao, S.M.; Xue, W.Q.; Qin, H.D.; Liu, W.S.; Cao, J.Y.; Zhang, Y.; Feng, Q.S.; et al. An epidemiological and molecular study of the relationship between smoking, risk of nasopharyngeal carcinoma, and Epstein-Barr virus activation. J. Natl. Cancer Inst. 2012, 104, 1396–1410. [Google Scholar] [CrossRef]
- Sopori, M. Effects of cigarette smoke on the immune system. Nat. Rev. Immunol. 2002, 2, 372–377. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Hu, G.H. Biomarkers for enhancing the radiosensitivity of nasopharyngeal carcinoma. Cancer Biol. Med. 2015, 12, 23–32. [Google Scholar]
- Yu, J.; Huang, Y.; Liu, L.; Wang, J.; Yin, J.; Huang, L.; Chen, S.; Li, J.; Yuan, H.; Yang, G.; et al. Genetic polymorphisms of Wnt/β-catenin pathway genes are associated with the efficacy and toxicities of radiotherapy in patients with nasopharyngeal carcinoma. Oncotarget 2016, 7, 82528–82537. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Wu, M.; Li, G.; Hua, L.; Chen, S.; Huang, H. Association between XRCC1 single-nucleotide polymorphism and acute radiation reaction in patients with nasopharyngeal carcinoma: A cohort study. Medicine 2017, 96, e8202. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.B.; Ma, W.L.; Liu, L.J.; Huang, Y.L.; Wang, J.; Huang, L.H.; Peng, X.D.; Yin, J.Y.; Li, J.G.; Chen, S.J.; et al. Effects of gene polymorphisms in the endoplasmic reticulum stress pathway on clinical outcomes of chemoradiotherapy in Chinese patients with nasopharyngeal carcinoma. Acta Pharmacol. Sin. 2017, 38, 571–580. [Google Scholar] [CrossRef]
- Wang, J.; Guo, C.; Gong, X.; Ao, F.; Huang, Y.; Huang, L.; Tang, Y.; Jiang, C.; Xie, X.; Dong, Q.; et al. The impacts of genetic polymorphisms in genes of base excision repair pathway on the efficacy and acute toxicities of (chemo)radiotherapy in patients with nasopharyngeal carcinoma. Oncotarget 2017, 8, 78633–78641. [Google Scholar] [CrossRef][Green Version]
- Zhai, X.M.; Hu, Q.C.; Gu, K.; Wang, J.P.; Zhang, J.N.; Wu, Y.W. Significance of XRCC1 Codon399 polymorphisms in Chinese patients with locally advanced nasopharyngeal carcinoma treated with radiation therapy. Asia Pac. J. Clin. Oncol. 2016, 12, e125–e132. [Google Scholar] [CrossRef]
- Hui, E.P.; Ma, B.B.; Chan, K.C.; Chan, C.M.; Wong, C.S.; To, K.F.; Chan, A.W.; Tung, S.Y.; Ng, W.T.; Cheng, A.C.; et al. Clinical utility of plasma Epstein-Barr virus DNA and ERCC1 single nucleotide polymorphism in nasopharyngeal carcinoma. Cancer 2015, 121, 2720–2729. [Google Scholar] [CrossRef]
- Tang, X.R.; Li, Y.Q.; Liang, S.B.; Jiang, W.; Liu, F.; Ge, W.X.; Tang, L.L.; Mao, Y.P.; He, Q.M.; Yang, X.J.; et al. Development and validation of a gene expression-based signature to predict distant metastasis in locoregionally advanced nasopharyngeal carcinoma: A retrospective, multicentre, cohort study. Lancet Oncol. 2018, 19, 382–393. [Google Scholar] [CrossRef]
- Qu, J.Q.; Yi, H.M.; Ye, X.; Zhu, J.F.; Yi, H.; Li, L.N.; Xiao, T.; Yuan, L.; Li, J.Y.; Wang, Y.Y.; et al. MiRNA-203 Reduces Nasopharyngeal Carcinoma Radioresistance by Targeting IL8/AKT Signaling. Mol. Cancer Ther. 2015, 14, 2653–2664. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Qiu, Y.; Su, Z.; Ren, S.; Liu, C.; Tian, Y.; Liu, Y. Genome-wide analyses of radioresistance-associated miRNA expression profile in nasopharyngeal carcinoma using next generation deep sequencing. PLoS ONE 2013, 8, e84486. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Huang, S.; Zhu, X.; Zhou, Z.; Liu, Y.; Qu, S.; Guo, Y. Identification of radioresistance-associated proteins in human nasopharyngeal carcinoma cell lines by proteomic analysis. Cancer Biother. Radiopharm. 2013, 28, 380–384. [Google Scholar] [CrossRef]
- Gao, F.; Zhao, Z.L.; Zhao, W.T.; Fan, Q.R.; Wang, S.C.; Li, J.; Zhang, Y.Q.; Shi, J.W.; Lin, X.L.; Yang, S.; et al. miR-9 modulates the expression of interferon-regulated genes and MHC class I molecules in human nasopharyngeal carcinoma cells. Biochem. Biophys. Res. Commun. 2013, 431, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Cao, H.; Xu, D.; Zhu, K. MicroRNA-92a promotes metastasis of nasopharyngeal carcinoma by targeting the PTEN/AKT pathway. OncoTargets Ther. 2016, 9, 3579–3588. [Google Scholar]
- Deng, X.; Liu, Z.; Liu, X.; Fu, Q.; Deng, T.; Lu, J.; Liu, Y.; Liang, Z.; Jiang, Q.; Cheng, C.; et al. miR-296-3p Negatively Regulated by Nicotine Stimulates Cytoplasmic Translocation of c-Myc via MK2 to Suppress Chemotherapy Resistance. Mol. Ther. 2018, 26, 1066–1081. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, P.Y.; Su, Z.; Mao, Y.P.; Liang, X.X.; Liu, Q.; Deng, W.; Xie, F.Y. Prognostic impact of cigarette smoking on the survival of patients with established nasopharyngeal carcinoma. Cancer Epidemiol. Biomark. Prev. 2013, 22, 2285–2294. [Google Scholar] [CrossRef]
- Shuai, M.; Hong, J.; Huang, D.; Zhang, X.; Tian, Y. Upregulation of circRNA_0000285 serves as a prognostic biomarker for nasopharyngeal carcinoma and is involved in radiosensitivity. Oncol. Lett. 2018, 16, 6495–6501. [Google Scholar] [CrossRef]
- Yuan, Y.; Zhou, X.; Song, J.; Qiu, X.; Li, J.; Ye, L.; Meng, X.; Xia, D. Expression and clinical significance of epidermal growth factor receptor and type 1 insulin-like growth factor receptor in nasopharyngeal carcinoma. Ann. Otol. Rhinol. Laryngol. 2008, 117, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Ruan, L.; Li, X.H.; Wan, X.X.; Yi, H.; Li, C.; Li, M.Y.; Zhang, P.F.; Zeng, G.Q.; Qu, J.Q.; He, Q.Y.; et al. Analysis of EGFR signaling pathway in nasopharyngeal carcinoma cells by quantitative phosphoproteomics. Proteome Sci. 2011, 9, 35. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Pan, Y.; Zhang, R.; Xu, T.; Wu, W.; Zhang, R.; Wang, C.; Huang, H.; Calin, C.A.; Yang, H.; et al. Hsa-miR-24-3p increases nasopharyngeal carcinoma radiosensitivity by targeting both the 3’UTR and 5’UTR of Jab1/CSN5. Oncogene 2016, 35, 6096–6108. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Shen, Z.; Wang, K.; Ha, Y.; Lei, H.; Jia, Y.; Ding, R.; Wu, D.; Gan, S.; Li, R.; et al. High FMNL3 expression promotes nasopharyngeal carcinoma cell metastasis: Role in TGF-β1-induced epithelia-to-mesenchymal transition. Sci. Rep. 2017, 7, 42507. [Google Scholar] [CrossRef]
- Fan, X.; Xie, Y.; Chen, H.; Guo, X.; Ma, Y.; Pang, X.; Huang, Y.; He, F.; Liu, S.; Yu, Y.; et al. Distant Metastasis Risk Definition by Tumor Biomarkers Integrated Nomogram Approach for Locally Advanced Nasopharyngeal Carcinoma. Distant Metastasis Risk Definition by Tumor Biomarkers Integrated Nomogram Approach for Locally Advanced Nasopharyngeal Carcinoma. Cancer Control 2019, 26, 1073274819883895. [Google Scholar]
- Wu, J.B.; Shen, L.; Qiu, L.; Duan, Q.W.; Luo, Z.G.; Dong, X.X. Reversal effect of GnT-V on the radioresistance of human nasopharyngeal carcinoma cells by alteration β1, 6-GlcNAc branched N-glycans. Int. J. Clin. Exp. Pathol. 2015, 8, 9901–9911. [Google Scholar]
- Lu, Y.; Huang, H.; Yang, H.; Chen, D.; Wu, S.; Jiang, Z.; Wang, R. Small molecule inhibitor TW-37 is tolerable and synergistic with chemotherapy in nasopharyngeal carcinoma. Cell Cycle 2017, 16, 1376–1383. [Google Scholar] [CrossRef]
- Su, W.; Lin, Y.; Wu, F.; Guo, H.; Li, L.; Zhu, S.; Lai, Z.; Liang, R.; Yang, Z. Bcl-2 regulation by miR-429 in human nasopharyngeal carcinoma in vivo. Int. J. Clin. Exp. Pathol. 2016, 9, 5998–6006. [Google Scholar]
- Zhang, G.; Zhang, K.; Li, C.; Li, Y.; Li, Z.; Li, N.; Zhou, Q.; Shen, L. Serum proteomics identify potential biomarkers for nasopharyngeal carcinoma sensitivity to radiotherapy. Biosci. Rep. 2019, 39, BSR20190027. [Google Scholar] [CrossRef]
- Yi, H.M.; Yi, H.; Zhu, J.F.; Xiao, T.; Lu, S.S.; Guan, Y.J.; Xiao, Z.Q. A five-variable signature predicts radioresistance and prognosis in nasopharyngeal carcinoma patients receiving radical radiotherapy. Tumor Biol. 2016, 37, 2941–2949. [Google Scholar] [CrossRef]
- Feng, X.P.; Yi, H.; Li, M.Y.; Li, X.H.; Yi, B.; Zhang, P.F.; Li, C.; Peng, F.; Tang, C.E.; Li, J.L.; et al. Identification of biomarkers for predicting nasopharyngeal carcinoma response to radiotherapy by proteomics. Cancer Res. 2010, 70, 3450–3462. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Liu, Y.; Su, Z.; Ren, S.; Zhu, G.; Tian, Y.; Qiu, Y. MicroRNA-324-3p regulates nasopharyngeal carcinoma radioresistance by directly targeting WNT2B. Eur. J. Cancer 2013, 49, 2596–2607. [Google Scholar] [CrossRef] [PubMed]
- Liao, L.; Yan, W.J.; Tian, C.M.; Li, M.Y.; Tian, Y.Q.; Zeng, G.Q. Knockdown of Annexin A1 Enhances Radioresistance and Inhibits Apoptosis in Nasopharyngeal Carcinoma. Technol. Cancer Res. Treat. 2018, 17, 1533034617750309. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Liao, L.; Wan, Y.; Cheng, A.; Li, M.; Chen, S.; Li, M.; Tan, X.; Zeng, G. Downregulation of Annexin A1 is correlated with radioresistance in nasopharyngeal carcinoma. Oncol. Lett. 2016, 12, 5229–5234. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Huang, W.; Zhong, M.; Yin, L.; Jiang, H.; Hou, S.; Gan, P.; Yuan, Y. Identification Keratin 1 as a cDDP-resistant protein in nasopharyngeal carcinoma cell lines. J. Proteom. 2012, 75, 2352–2360. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Qi, Z.; Chen, M.; Xiao, T.; Guan, J.; Zhou, M.; Wang, Q.; Lin, Z.; Wang, Z. Serum amyloid A1 as a biomarker for radiation dose estimation and lethality prediction in irradiated mouse. Ann. Transl. Med. 2019, 7, 715. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Qu, J.Q.; Xiao, L.; Yi, H.; Zhang, P.F.; Li, M.Y.; Hu, R.; Wan, X.X.; He, Q.Y.; Li, J.H.; et al. Identification of heat shock protein 27 as a radioresistance-related protein in nasopharyngeal carcinoma cells. J. Cancer Res. Clin. Oncol. 2012, 138, 2117–2125. [Google Scholar] [CrossRef]
- Wang, R.; Qin, H.M.; Liao, B.Y.; Yang, F.L.; Wang, J.L. Genetic polymorphisms in interleukin 13 gene with the susceptibility to nasopharyngeal carcinoma in a Chinese population. Cytokine 2019, 115, 121–126. [Google Scholar] [CrossRef]
- Ferrari, D.; Codecà, C.; Bertuzzi, C.; Broggio, F.; Crepaldi, F.; Luciani, A.; Floriani, I.; Ansarin, M.; Chiesa, F.; Alterio, D.; et al. Role of plasma EBV DNA levels in predicting recurrence of nasopharyngeal carcinoma in a Western population. BMC Cancer 2012, 12, 208. [Google Scholar] [CrossRef] [PubMed]
- Shao, J.Y.; Li, Y.H.; Gao, H.Y.; Wu, Q.L.; Cui, N.J.; Zhang, L.; Cheng, G.; Hu, L.F.; Ernberg, I.; Zeng, Y.X. Comparison of plasma Epstein-Barr virus (EBV) DNA levels and serum EBV immunoglobulin A/virus capsid antigen antibody titers in patients with nasopharyngeal carcinoma. Cancer 2004, 100, 1162–1170. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology. Head and Neck Cancer. Version 2. Available online: https://www.nccn.org/professionals/physician (accessed on 28 June 2019).
- Moor, A.E.; Itzkovitz, S. Spatial transcriptomics: Paving the way for tissue-level systems biology. Curr. Opin. Biotechnol. 2017, 46, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.J.; Chou, Y.F.; Chen, P.R.; Su, B.; Hsu, Y.C.; Chang, C.H.; Lee, J.W. Differential miRNA expression in repeated recurrence of nasopharyngeal carcinoma. Cancer Lett. 2014, 344, 188–194. [Google Scholar] [CrossRef]
- Liu, G.; Zeng, X.; Wu, B.; Zhao, J.; Pan, Y. RNA-Seq analysis of peripheral blood mononuclear cells reveals unique transcriptional signatures associated with radiotherapy response of nasopharyngeal carcinoma and prognosis of head and neck cancer. Cancer Biol. Ther. 2020, 21, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Zamanian Azodi, M.; Rezaei Tavirani, M.; Rezaei Tavirani, M.; Vafaee, R.; Rostami-Nejad, M. Nasopharyngeal Carcinoma Protein Interaction Mapping Analysis via Proteomic Approaches. Asian Pac. J. Cancer Prev. 2018, 19, 845–851. [Google Scholar]
- Meng, H.; Zhu, X.; Li, L.; Liang, Z.; Li, X.; Pan, X.; Zeng, F.; Qu, S. Identification of CALM as the potential serum biomarker for predicting the recurrence of nasopharyngeal carcinoma using a mass spectrometry-based comparative proteomic approach. Int. J. Mol. Med. 2017, 40, 1152–1164. [Google Scholar] [CrossRef][Green Version]
- Pan, Y.; Wang, M.; Bu, X.; Zuo, Y.; Wang, S.; Wang, D.; Liu, Q.; Su, B.; Xu, T.; Wang, C.; et al. Curcumin analogue T83 exhibits potent antitumor activity and induces radiosensitivity through inactivation of Jab1 in nasopharyngeal carcinoma. BMC Cancer 2013, 13, 323. [Google Scholar] [CrossRef]
- Zhang, W.; Zeng, Z.; Zhou, Y.; Xiong, W.; Fan, S.; Xiao, L.; Huang, D.; Li, Z.; Li, D.; Wu, M.; et al. Identification of aberrant cell cycle regulation in Epstein-Barr virus-associated nasopharyngeal carcinoma by cDNA microarray and gene set enrichment analysis. Acta Biochim. Biophys. Sin. 2009, 41, 414–428. [Google Scholar] [CrossRef][Green Version]
- Tulalamba, W.; Janvilisri, T. Nasopharyngeal carcinoma signaling pathway: An update on molecular biomarkers. Int. J. Cell Biol. 2012, 2012, 594681. [Google Scholar] [CrossRef]
- Li, Z.; Ren, Y.; Lin, S.X.; Liang, Y.J.; Liang, H.Z. Association of E-cadherin and beta-catenin with metastasis in nasopharyngeal carcinoma. Chin. Med. J. 2004, 117, 1232–1239. [Google Scholar]
- Cheng, A.L.; Huang, W.G.; Chen, Z.C.; Peng, F.; Zhang, P.F.; Li, M.Y.; Li, F.; Li, J.L.; Li, C.; Yi, H.; et al. Identification of novel nasopharyngeal carcinoma biomarkers by laser capture microdissection and proteomic analysis. Clin. Cancer Res. 2008, 14, 435–445. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.L.; Huang, W.G.; Chen, Z.C.; Zhang, P.F.; Li, M.Y.; Li, F.; Li, J.L.; Li, C.; Yi, H.; Peng, F.; et al. Identificating cathepsin D as a biomarker for differentiation and prognosis of nasopharyngeal carcinoma by laser capture microdissection and proteomic analysis. J. Proteome Res. 2008, 7, 2415–2426. [Google Scholar] [CrossRef] [PubMed]
- Xiao, L.; Xiao, T.; Wang, Z.M.; Cho, W.C.; Xiao, Z.Q. Biomarker discovery of nasopharyngeal carcinoma by proteomics. Expert Rev. Proteom. 2014, 11, 215–225. [Google Scholar] [CrossRef]
- Cho, W.C.; Yip, T.T.; Yip, C.; Yip, V.; Thulasiraman, V.; Ngan, R.K.; Yip, T.T.; Lau, W.H.; Au, J.S.; Law, S.C.; et al. Identification of serum amyloid a protein as a potentially useful biomarker to monitor relapse of nasopharyngeal cancer by serum proteomic profiling. Clin. Cancer Res. 2004, 10, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Melissaridou, S.; Wiechec, E.; Magan, M.; Jain, M.V.; Chung, M.K.; Farnebo, L.; Roberg, K. The effect of 2D and 3D cell cultures on treatment response, EMT profile and stem cell features in head and neck cancer. Cancer Cell Int. 2019, 19, 16. [Google Scholar] [CrossRef] [PubMed]
- Imamura, Y.; Mukohara, T.; Shimono, Y.; Funakoshi, Y.; Chayahara, N.; Toyoda, M.; Kiyota, N.; Takao, S.; Kono, S.; Nakatsura, T.; et al. Comparison of 2D- and 3D-culture models as drug-testing platforms in breast cancer. Oncol. Rep. 2015, 33, 1837–1843. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.Y.; Le, Q.T.; Yom, S.S.; Pinsky, B.A.; Bratman, S.V.; Ng, R.H.; El Mubarak, H.S.; Chan, K.C.; Sander, M.; Conley, B.A. Current State of PCR-Based Epstein-Barr Virus DNA Testing for Nasopharyngeal Cancer. J. Natl. Cancer Inst. 2017, 109, djx007. [Google Scholar] [CrossRef] [PubMed]
- Cancer Research UK. Cancer Research UK Policy Statement: Patient Access to Molecular Diagnostics and Targeted Medicines in England. Available online: https://www.cancerresearchuk.org/sites/default/files/access_to_molecular_diagnostic_tests_and_targeted_medicines_in_england_0.pdf (accessed on 15 March 2020).
| Biomolecules | Full Name | Role | Aberration | Sources |
|---|---|---|---|---|
| Genomic biomarkers | ||||
| COX-2 | Cyclooxygenase-2 | Cell proliferation, apoptosis | Polymorphism in rs5275 | [21] |
| MCP-1 | Monocyte chemoattractant protein-1 | Monocytes or macrophages migration and infiltration | Polymorphism in rs1024611 | [22] |
| GRP78 | Glucose-regulated protein | Apoptosis | Polymorphism in rs3216733 | [23] |
| DC-SIGN | Dendritic cells specific intercellular adhesion molecule 3-grabbing nonintegrin | Induced immune cells | Polymorphism in rs7252229, rs735240, rs4804803 or rs2287886 | [24,25] |
| HLA-A2-B46 (Chinese) | Human leukocyte antigen-A2-B46 | Immune response | Polymorphism in chromosome 6p21 | [26,27] |
| HLA-A2-B-17 (Chinese) | Human leukocyte antigen-A2-B-17 | Immune response | ||
| HLA-B5 (Caucasians) | Human leukocyte antigen-B5 | Immune response | ||
| IL-13 | Interleukin-13 | Polymorphism in rs20541 (TT genotype) | [28] | |
| Chromosome 3p and 9p | N/A | N/A | Chromosomal loss | [29] |
| Chromosome 12 | N/A | N/A | Gain number | [30] |
| RASSF1 | Ras association (RalGDS/AF-6) domain family member 1A | Tumour suppression, cell growth, proliferation | copy number variant in in 3p21 | [1] |
| CDKN2A, CDKN2B | Cyclin-dependent kinase inhibitor 2A, 2B | Tumour suppression, cell cycle | Allelic deletion in 9p21.3 | [31] |
| EGFR | Epidermal growth factor receptor | Cell proliferation, cell cycles, apoptosis | Upregulation | [32,33] |
| BamH1-W | Bacillus amyloliquefaciens 1 WZhet | Viral replicative cycle | Upregulation | [34,35] |
| A73 | N/A | Cell proliferation and angiogenesis | Polymorphism in A157154C | [20,36] |
| RPMS1 | N/A | Cell proliferation and angiogenesis | Polymorphism in G155391A | |
| BALF2 | N/A | Viral infection and replication | EBV variants with 162476_C or 163364_T | [37] |
| miRNA biomarkers | ||||
| miR17-92 | MicroRNA17-92 | Targeting PTEN and apoptosis protein | Upregulation | [38] |
| miR-155 | MicroRNA-155 | Leucosis | Upregulation | [39] |
| miR-378 | MicroRNA-378 | Affect tumour suppression, cell cycle | Upregulation | [40,41] |
| miR-141 | MicroRNA-141 | |||
| miR144-3p | MicroRNA-144-3p | Targeting PTEN/Akt, cell cycle, apoptosis | Upregulation | [42] |
| miR-17-5p | MicroRNA-17-5p | |||
| miR-20a-5p | MicroRNA-20a-5p | |||
| miR-20b-5p | MicroRNA-20b-5p | |||
| miR-205-5p | MicroRNA-205-5p | |||
| miR-16 | MicroRNA-16 | Cell proliferation, invasion | Upregulation | [39] |
| miR-21 | MicroRNA-21 | Targets PDCD4, PTEN, SPRY, ERCK, and Bcl-2 family proteins | ||
| miR-24 | MicroRNA-24 | Epithelial-to-mesenchymal transition | Upregulation | |
| miR-146a | Inflammation | Upregulation | [6] | |
| miR-34 | MicroRNA-34 | Tumour suppression | Downregulation | [38] |
| miR-143 | MicroRNA-143 | Tumour suppression | ||
| miR-145 | MicroRNA-145 | Tumour suppression | ||
| let-7b-5p | MicroRNA let-7b-5p | Cell proliferation | Downregulation | [42] |
| miR-140-3p | MicroRNA-140-3p | Cell proliferation | ||
| Platelet miR-34c-3p | MicroRNA-34c-3p | Tumour suppression | Upregulation | [28] |
| Platelet miR-18a-5p | MicroRNA-18a-5p | Tumour suppression | ||
| MALAT1 | metastasis associated with lung adenocarcinoma transcript 1 | Invasion | Upregulation | [43] |
| AFAP1-AS1 | actin filament-associated protein 1-antisense RNA1 | Invasion | ||
| AL359062 | N/A | N/A | ||
| EBER | Epstein–Barr encoding region | Cell proliferation, apoptosis, innate immunity | Four base deletion SNPs | [44] |
| miR-BART7-3p | BamH1 A rightward transcript 7-3p | Cell proliferation targeting NF-κB signalling, angiogenesis targeting AMPK/mTOR/HIF1 signalling | Upregulation | [8,45,46] |
| miR-BART13-3p | BamH1 A rightward transcript 13-3p | Cell proliferation targeting NF-κB signalling, angiogenesis targeting AMPK/mTOR/HIF1 signalling | ||
| Protein biomarkers | ||||
| PAI-1 | Plasminogen activator inhibitor 1 | Angiogenesis, signalling activities | Upregulation | [47] |
| Fibronectin | N/A | Cell adhesion | ||
| Mac-2 BP | Mac-2-binding protein | Cell adhesion | ||
| CTSD | Cathepsin D | Apoptosis | Upregulation | [48] |
| POSTN | Periostin | Cell adhesion | Upregulation | [49] |
| CK18 | Cytokeratin 18 | Transcription | Upregulation | [50] |
| KRT8 | Keratin-8 | Tumour necrosis factor-mediated signaling pathway, cell differentiation | Upregulation | [48] |
| STMN1 | Stathmin-1 | Signal transduction | ||
| LCP1 | L-plastin | Cell differentiation | Upregulation | [51] |
| LGALS1 | Galectin-1 | Apoptosis | Upregulation | [52] |
| S100A9 | S100 calcium-binding protein A9 | Cell proliferation, innate immunity, apoptosis | Upregulation | [51] |
| CCL5 | C-C motif chemokine 5 | Cell adhesion, migration, apoptosis | Upregulation | [53] |
| CLIC1 | Chloride intracellular channel 1 | Cell cycle, signal transduction | Upregulation | [54] |
| LMP1 | Latent membrane protein | Signalling activities | Upregulation | [55] |
| P-Thr-sv-5 | N/A | Gene expression (sub-variant of EBNA1) | subvariant of EBNA1 | [56] |
| EBNA1/IgA | EBV nuclear antigens immunoglobulin A | Antibody against EBV antigen | Increased level | [57,58] |
| VCA/IgA | Viral capsid antigen immunoglobulin A | Antibody against EBV antigen | ||
| BALF2/Ab | BALF2 antibodies | Antibody against EBV antigen | Increased level | [37] |
| Metabolite biomarkers | ||||
| kynurenine | N/A | Metabolism | Upregulation | [59] |
| N-acetylglucosaminylamine | N/A | Metabolism | ||
| N-acetylglucosamine hydroxyphenylpyruvate | N/A | Metabolism | ||
| Pyroglutamate | N/A | Metabolism | Upregulation | [60] |
| Glucose | N/A | Metabolism | ||
| Glutamate | N/A | Metabolism | ||
| Glycerol 1-hexadecanoate | N/A | Metabolism | Upregulation | [61] |
| b-hydroxybutyrate | N/A | Metabolism | ||
| Arachidonic acid | N/A | Metabolism | ||
| Stearic acid | N/A | Metabolism | ||
| Linoleic acid | N/A | Metabolism | ||
| Proline | N/A | Metabolism | ||
| Biomolecules | Name | Role | Aberration | Sources |
|---|---|---|---|---|
| β-catenin 1 | Beta-catenin1 | Activate multiple downstream growth signalling components such as cyclin D1 and c-Myc | Polymorphism in rs1880481 or rs3864004 | [122] |
| GSK-3β | glycogen synthase kinase-3β | Cell growth, metabolism, gene transcription, protein translation, cytoskeletal organisation | Polymorphism in rs3755557 | |
| APC | adenomatous polyposis coli | Cell adhesion | Polymorphism in rs454886 | |
| XRCC1 | X-ray repair cross-complementing 1 | DNA repair | Polymorphism in rs25489 or Codon399 | [123,124,125,126] |
| CT | Calcitonin receptor | Calcium homeostasis | Polymorphism in rs2528521 | |
| VCP | Valosin-containing protein | Proteolysis | Polymorphism in rs2074549 | |
| IL-13 | Interleukin-13 | Chinese population with IL-13 rs20541 | Polymorphisms in rs20541 | [28] |
| ERCC1 | Excision repair 1 endonuclease non-catalytic subunit | DNA repair | Polymorphism with C118T genotype | [127] |
| EBV-DNA | Epstein–Barr virus-DNA | EBV genome | Upregulation | [33] |
| YBX3 | Y-Box Binding Protein 3 | Apoptosis, Gene expression | Upregulation | [128] |
| CBR3 | Carbonyl reductase 3 | Xenobiotic metabolic process | ||
| LRIG1 | Leucine-rich repeats and immunoglobulin-like domains 1 | Negative regulator of tyrosine kinases signalling | ||
| CXCL10 | Chemokine C-X-C motif ligand 10 | Chemokine receptors recruit tumour infiltrating T-lymphocytes, tumour microenvironment | ||
| DCTN1 | Dynactin-1 | G2/M transition of mitotic cell cycle | Downregulation | |
| GRM4 | Glutamate metabotropic receptor 4 | Tumour suppression | ||
| HDLBP | High density lipoprotein binding protein | Cholesterol metabolic process | ||
| ANXA1 | Annexin | Cell cycle, apoptosis | ||
| POLR2M | RNA polymerase II subunit M | Negative regulator of transcriptional | ||
| CLASP1 | Cytoplasmic linker associated protein 1 | Dynamic microtubules stabilization | ||
| FNDC3B | Fibronectin type III domain-containing protein 3B | Positive regulator of adipogenesis | ||
| WSB2 | WD repeat and SOCS box-containing protein 2 | Protein ubiquitination, post-translation modification | ||
| WNK1 | lysine deficient protein kinase 1 | T-cell receptor signalling pathway | ||
| miR-203 | MicroRNA-203 | Targeting IL-8/Akt signalling | Downregulation | [129] |
| miR-324-3p | MicroRNA-324-3p | Tumour suppression | Downregulation | [130,131] |
| miR-93-3p | MicroRNA-93-3p | Targeting Wnt/β-catenin signalling | ||
| miR-4501 | MicroRNA-4501 | Cellular process | ||
| miR-371a-5p | MicroRNA-371a-5p | Cellular pathway, apoptosis | Upregulation | |
| miR-34c-5p | MicroRNA-34c-5p | Cell proliferation, apoptosis, targeting JAK2/STAT3 signalling pathway | ||
| miR-1323 | MicroRNA-1323 | DNA repair | ||
| miR-9 | MicroRNA-9 | MHC class I and interferon-regulated gene expression | Downregulation | [132] |
| miR-92a | MicroRNA-92a | Invasion, migration | Upregulation | [133] |
| miR-574-5p | MicroRNA-574-5p | Mesenchymal transition | Downregulation | [9] |
| miR-296-3p | Micro-296-3p | Cytoplasmic Translocation of c-Myc | Downregulation | [134,135] |
| RNA_0000285 | homeodomain interacting protein kinase 3 (HIPK3) | Upregulation | [136] | |
| EGFR | Epidermal growth factor receptor | Cell proliferation, cell cycles, apoptosis | Upregulation | [137] |
| GSTP1 | Glutathione S-transferase P1 | Cell adhesion, apoptosis, negative regulator of NF-kB signaling | Methylation | [138] |
| IGF-1R | Insulin-like growth factor-1 receptor | Cell proliferation, cell cycles and apoptosis | Upregulation | [137] |
| Jab1 | C-Jun activation domain-binding protein-1 | Cell proliferation, targeting negative regulator proteins and tumour suppressors (p27 and p53) | Upregulation | [139] |
| EMT | Epithelial-to-mesenchymal transition | Carcinogenesis and metastatic progression | Upregulation | [140] |
| β-catenin | N/A | Activate multiple downstream growth signalling components such as cyclin D1 and c-Myc | Upregulation | [141] |
| E-cadherin | N/A | Cell adhesion, tumour suppression | Downregulation | |
| GnT-V | N-acetylglucosaminyltransferase-V | Protein glycosylation, cell proliferation | Upregulation | [142] |
| Bcl2 | B-cell lymphoma 2 | Apoptosis | Upregulation | [143,144] |
| SPARC | Secreted protein acidic and Cysteine rich | Extracellular matrix synthesis, cell shape | Upregulation | [145] |
| ERPIND1 | Serpin family D member 1S | Invasion | ||
| C4B | Complement C4B | Component of the classical activation pathway | ||
| PPIB | Ppeptidylprolyl lsomerase B | Cyclosporine A-mediated immunosuppression | ||
| FAM173A | Family with sequence similarity 173 member A | Adenine nucleotide translocase | ||
| Maspin | Mammary serine protease inhibitor | Tumour suppression | Upregulation | [146,147] |
| GRP78 | Glucose-regulated protein | Apoptosis | ||
| Mn-SOD | Manganese superoxide dismutase | Apoptosis | ||
| 14-3-3σ | 14-3-3 protein sigma | Cell cycle arrest, DNA damage response, signal transduction | Downregulation | |
| ANXA1,3 | Annexin A1, A3 | Cell cycle, apoptosis | Downregulation | [148,149,150] |
| Nm23 H1 | Non-metastatic clone 23, isoform H1 | TGF-β signaling | Upregulation | |
| KRT1 | Keratin 1 | Angiogenesis | Upregulation | [151] |
| SAA | Serum amyloid A | MAPK activities, innate immune response | Downregulation | [152] |
| HSP27 | Heat shock protein 27 | Apoptosis, cell differentiation | Upregulation | [153] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siak, P.Y.; Khoo, A.S.-B.; Leong, C.O.; Hoh, B.-P.; Cheah, S.-C. Current Status and Future Perspectives about Molecular Biomarkers of Nasopharyngeal Carcinoma. Cancers 2021, 13, 3490. https://doi.org/10.3390/cancers13143490
Siak PY, Khoo AS-B, Leong CO, Hoh B-P, Cheah S-C. Current Status and Future Perspectives about Molecular Biomarkers of Nasopharyngeal Carcinoma. Cancers. 2021; 13(14):3490. https://doi.org/10.3390/cancers13143490
Chicago/Turabian StyleSiak, Pui Yan, Alan Soo-Beng Khoo, Chee Onn Leong, Boon-Peng Hoh, and Shiau-Chuen Cheah. 2021. "Current Status and Future Perspectives about Molecular Biomarkers of Nasopharyngeal Carcinoma" Cancers 13, no. 14: 3490. https://doi.org/10.3390/cancers13143490
APA StyleSiak, P. Y., Khoo, A. S.-B., Leong, C. O., Hoh, B.-P., & Cheah, S.-C. (2021). Current Status and Future Perspectives about Molecular Biomarkers of Nasopharyngeal Carcinoma. Cancers, 13(14), 3490. https://doi.org/10.3390/cancers13143490







