Physical Comorbidities and Depression in Recent and Long-Term Adult Cancer Survivors: NHANES 2007–2018
Abstract
:Simple Summary
Abstract
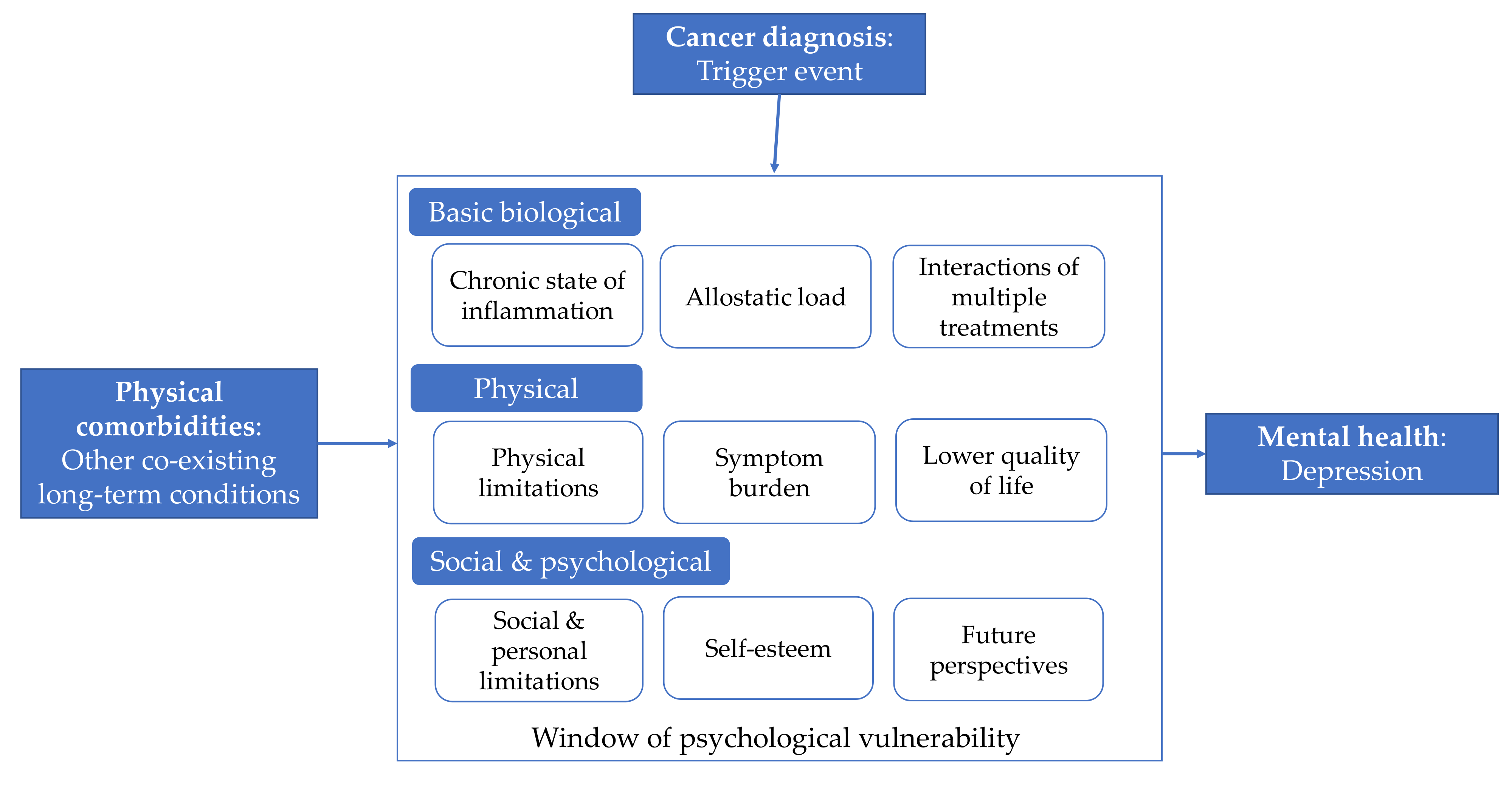
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Variables
2.2.1. Sociodemographic Characteristics
2.2.2. Physical Function Limitations
2.2.3. Cancer Site
2.2.4. Time Since Diagnosis
2.2.5. Physical Comorbidities
2.2.6. Physical Comorbidities Pre- and Post-Diagnosis
2.2.7. Depression
2.3. Statistical Analysis
3. Results
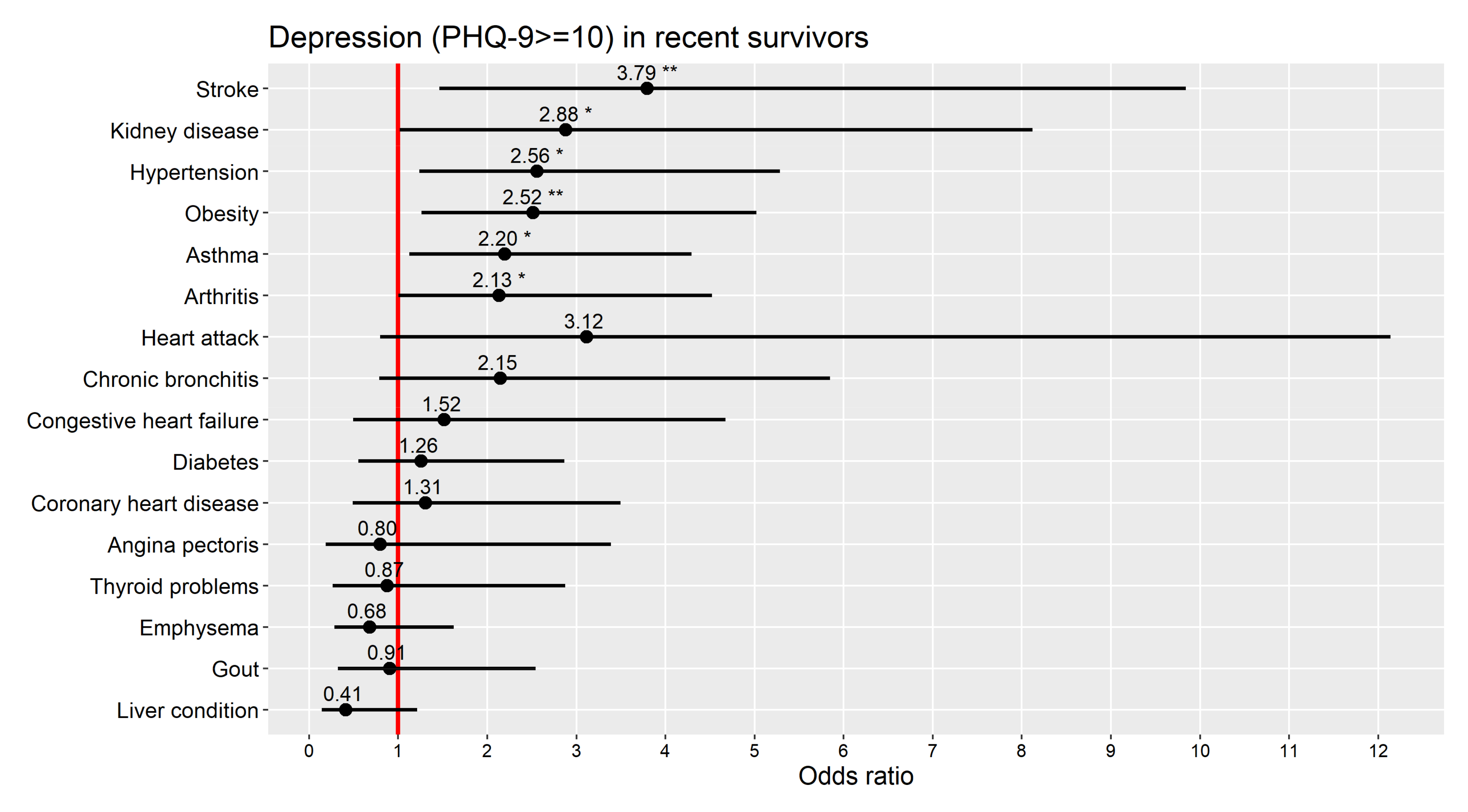
3.1. Recent Survivors
3.2. Long-Term Survivors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| NHANES Code | Cancer | N Recent Survivors | N Long-Term Survivors | Group According to Body Location/System |
|---|---|---|---|---|
| 10 | Bladder | 18 | 17 | Genitorunary |
| 11 | Blood | 1 | 1 | Other |
| 12 | Bone | 4 | 2 | Other |
| 13 | Brain | 3 | 7 | Other |
| 14 | Breast | 128 | 202 | Breast |
| 15 | Cervix (cervical) | 32 | 124 | Gynecological |
| 16 | Colon | 52 | 59 | Digestive/gastrointestinal |
| 17 | Esophagus (esophageal) | 5 | 6 | Digestive/gastrointestinal |
| 18 | Gallbladder | 0 | 1 | Digestive/gastrointestinal |
| 19 | Kidney | 15 | 22 | Genitorunary |
| 20 | Larynx/windpipe | 2 | 5 | Other |
| 21 | Leukemia | 8 | 9 | Other |
| 22 | Liver | 6 | 2 | Digestive/gastrointestinal |
| 23 | Lung | 31 | 12 | Other |
| 24 | Lymphoma/Hodgkin’s disease | 24 | 28 | Other |
| 25 | Melanoma | 44 | 70 | Melanoma |
| 26 | Mouth/tongue/lip | 3 | 9 | Other |
| 27 | Nervous system | 0 | 1 | Other |
| 28 | Ovary (ovarian) | 14 | 37 | Gynecological |
| 29 | Pancreas (pancreatic) | 6 | 2 | Digestive/gastrointestinal |
| 30 | Prostate | 154 | 165 | Genitorunary |
| 31 | Rectum (rectal) | 3 | 5 | Digestive/gastrointestinal |
| 32 | Skin non-melanoma | 145 | 161 | Skin non-melanoma |
| 33 | Skin (don’t know what kind) | 60 | 88 | Skin unknown kind |
| 34 | Soft tissue (muscle or fat) | 0 | 3 | Other |
| 35 | Stomach | 7 | 8 | Digestive/gastrointestinal |
| 36 | Testis (testicular) | 2 | 12 | Genitorunary |
| 37 | Thyroid | 17 | 34 | Other |
| 38 | Uterus (uterine) | 28 | 68 | Gynecological |
| 39 | Other | 41 | 60 | Other |
| Recent Survivors n = 853 | Long-Term Survivors n = 1220 | |
|---|---|---|
| Percentage (95% CI) | Percentage (95% CI) | |
| Obesity (BMI ≥ 30 kg/m2) * | 51.9 (46.8, 57.1) | 53.1 (49.7, 56.5) |
| Hypertension | 51.2 (46.4, 56.0) | 48.5 (44.5, 52.4) |
| Arthritis | 43.7 (38.8, 48.4) | 50.6 (46.7, 54.4) |
| Asthma | 17.9 (14.1, 21.8) | 17.4 (14.4, 20.4) |
| Diabetes | 17.8 (14.3, 21.2) | 15.4 (12.7, 18.1) |
| Thyroid problems | 15.3 (12.4, 18.3) | 19.9 (16.7, 23.1) |
| Chronic bronchitis | 10.6 (8.1, 13.1) | 10.7 (7.9, 13.4) |
| Gout | 8.3 (5.7, 10.9) | 8.3 (6.4, 10.3) |
| Coronary heart disease | 6.6 (4.6, 8.7) | 6.2 (4.2, 8.2) |
| Myocardial infarction | 6.2 (4.1, 8.3) | 5.9 (4.1, 7.8) |
| Weak or failing kidneys | 6.1 (3.8, 8.3) | 5.6 (3.9, 7.1) |
| Congestive heart failure | 5.6 (3.8, 7.5) | 4.1 (2.8, 5.4) |
| Emphysema | 5.6 (3.7, 7.5) | 5.3 (3.2, 7.3) |
| Liver condition | 5.6 (3.6, 7.4) | 5.6 (4.0, 7.1) |
| Stroke | 5.1 (3.2, 7.2) | 5.2 (3.7, 6.7) |
| Angina pectoris | 3.3 (1.6, 5.0) | 4.8 (2.7, 6.8) |
References
- Caruso, R.; Breitbart, W. Mental health care in oncology. Contemporary perspective on the psychosocial burden of cancer and evidence-based interventions. Epidemiol. Psychiatr. Sci. 2020, 29, e86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakash, O.; Shemesh, A.; Nagar, M.; Levav, I. Cancer and common mental disorders in the community: Results of the Israel-World Mental Health Survey. Eur. J. Psychiatry 2012, 26, 174–184. [Google Scholar] [CrossRef] [Green Version]
- Ng, H.S.; Roder, D.; Koczwara, B.; Vitry, A. Comorbidity, physical and mental health among cancer patients and survivors: An Australian population-based study. Asia Pac. J. Clin. Oncol. 2018, 14, e181–e192. [Google Scholar] [CrossRef] [PubMed]
- Petrova, D.; Redondo-Sánchez, D.; Rodríguez-Barranco, M.; Ruiz, A.R.; Catena, A.; Garcia-Retamero, R.; Sánchez, M. Physical comorbidities as a marker for high risk of psychological distress in cancer patients. Psychooncology 2021. [Google Scholar] [CrossRef]
- Mitchell, A.J.; Chan, M.; Bhatti, H.; Halton, M.; Grassi, L.; Johansen, C.; Meader, N. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: A meta-analysis of 94 interview-based studies. Lancet Oncol. 2011, 12, 160–174. [Google Scholar] [CrossRef]
- Caruso, R.; Nanni, M.G.; Riba, M.; Sabato, S.; Mitchell, A.J.; Croce, E.; Grassi, L. Depressive spectrum disorders in cancer: Prevalence, risk factors and screening for depression: A critical review. Acta Oncol. 2017, 56, 146–155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Linden, W.; Vodermaier, A.; MacKenzie, R.; Greig, D. Anxiety and depression after cancer diagnosis: Prevalence rates by cancer type, gender, and age. J. Affect. Disord. 2012, 141, 343–351. [Google Scholar] [CrossRef]
- Mitchell, A.J.; Ferguson, D.W.; Gill, J.; Paul, J.; Symonds, P. Depression and anxiety in long-term cancer survivors compared with spouses and healthy controls: A systematic review and meta-analysis. Lancet Oncol. 2013, 14, 721–732. [Google Scholar] [CrossRef]
- Brandenbarg, D.; Maass, S.W.; Geerse, O.P.; Stegmann, M.E.; Handberg, C.; Schroevers, M.J.; Duijts, S.F. A systematic review on the prevalence of symptoms of depression, anxiety and distress in long-term cancer survivors: Implications for primary care. Eur. J. Cancer Care 2019, 28, e13086. [Google Scholar] [CrossRef]
- Krebber AM, H.; Buffart, L.M.; Kleijn, G.; Riepma, I.C.; De Bree, R.; Leemans, C.R.; Verdonck-de Leeuw, I.M. Prevalence of depression in cancer patients: A meta-analysis of diagnostic interviews and self-report instruments. Psycho Oncol. 2014, 23, 121–130. [Google Scholar] [CrossRef]
- Nezu, A.M.; Nezu, C.M.; Greenberg, L.M.; Salber, K.E. 19 Cancer and Depression. In The Oxford Handbook of Depression and Comorbidity; Oxford University Press: New York, NY, USA, 2014; p. 302. [Google Scholar]
- AIHW (Australian Institute of Health and Welfare). Comorbidity of Mental Disorders and Physical Conditions 2007; AIHW: Canberra, Australia, 2017.
- Sarfati, D.; Koczwara, B.; Jackson, C. The impact of comorbidity on cancer and its treatment. CA Cancer J. Clin. 2016, 66, 337–350. [Google Scholar] [CrossRef]
- Sogaard, M.; Thomsen, R.; Bossen, K.S.; Sørensen, H.H.T.; Nørgaard, M. The impact of comorbidity on cancer survival: A review. Clin. Epidemiol. 2013, 5 (Suppl. 1), 3–29. [Google Scholar] [CrossRef] [Green Version]
- Luque-Fernandez, M.A.; Redondo-Sanchez, D.; Lee, S.F.; Rodríguez-Barranco, M.; Carmona-García, M.C.; Marcos-Gragera, R.; Sánchez, M.-J. Multimorbidity by patient and tumor factors and time-to-surgery among colorectal cancer patients in Spain: A population-based study. Clin. Epidemiol. 2020, 12, 31–40. [Google Scholar] [CrossRef] [Green Version]
- Luque-Fernandez, M.A.; Goncalves, K.; Salamanca-Fernández, E.; Redondo-Sanchez, D.; Lee, S.F.; Rodríguez-Barranco, M.; Carmona-García, M.C.; Marcos-Gragera, R.; Sánchez, M.-J. Multimorbidity and short-term overall mortality among colorectal cancer patients in Spain: A population-based cohort study. Eur. J. Cancer 2020, 129, 4–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pilling, S.; Anderson, I.; Goldberg, D.; Meader, N.; Taylor, C. Depression in adults, including those with a chronic physical health problem: summary of NICE guidance. BMJ 2009, 339, b4108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mausbach, B.T.; Irwin, S.A. Depression and healthcare service utilization in patients with cancer. Psychooncology 2017, 26, 1133–1139. [Google Scholar] [CrossRef] [PubMed]
- Donovan, K.A.; Grassi, L.; Deshields, T.L.; Corbett, C.; Riba, M.B. Advancing the science of distress screening and management in cancer care. Epidemiol. Psychiatr. Sci. 2020, 29, e85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riba, M.B.; Donovan, K.A.; Andersen, B.; Braun, I.; Breitbart, W.S.; Brewer, B.W.; Buchmann, L.O.; Clark, M.M.; Collins, M.; Corbett, C.; et al. Distress management, version 3.2019, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 2019, 17, 1229–1249. [Google Scholar] [CrossRef]
- Götz, A.; Kröner, A.; Jenewein, J.; Spirig, R. Evaluation of the adherence of distress screening with the distress thermometer in cancer patients 4 years after implementation. Support. Care Cancer 2018, 27, 2799–2807. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC); National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. 2007–2018. Available online: https://www.cdc.gov/nchs/nhanes/index.htm (accessed on 5 July 2021).
- Steeves, J.A.; Shiroma, E.J.; Conger, S.A.; Van Domelen, D.; Harris, T.B. Physical activity patterns and multimorbidity burden of older adults with different levels of functional status: NHANES 2003–2006. Disabil. Health J. 2019, 12, 495–502. [Google Scholar] [CrossRef] [PubMed]
- National cancer Institute (NCI). Cancers by Body Location/System. 2021. Available online: https://www.cancer.gov/types/by-body-location (accessed on 5 July 2021).
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Hinz, A.; Mehnert, A.; Kocalevent, R.-D.; Brähler, E.; Forkmann, T.; Singer, S.; Schulte, T. Assessment of depression severity with the PHQ-9 in cancer patients and in the general population. BMC Psychiatry 2016, 16, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moriarty, A.S.; Gilbody, S.; McMillan, D.; Manea, L. Screening and case finding for major depressive disorder using the Patient Health Questionnaire (PHQ-9): A meta-analysis. Gen. Hosp. Psychiatry 2015, 37, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Manea, L.; Gilbody, S.; McMillan, D. A diagnostic meta-analysis of the Patient Health Questionnaire-9 (PHQ-9) algorithm scoring method as a screen for depression. Gen. Hosp. Psychiatry 2015, 37, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Löwe, B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. Gen. Hosp. Psychiatry 2010, 32, 345–359. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. 2021. Available online: https://www.R-project.org/ (accessed on 5 July 2021).
- Lumley, T. Package ‘Survey’. Available online: http://cran.r2020 (accessed on 5 July 2021).
- Therneau, T.M.; Lumley, T. Package ‘Survival’. CRAN 2014, 2, 3. [Google Scholar]
- Pinquart, M.; Duberstein, P.R. Depression and cancer mortality: A meta-analysis. Psychol. Med. 2010, 40, 1797–1810. [Google Scholar] [CrossRef]
- Syrowatka, A.; Motulsky, A.; Kurteva, S.; Hanley, J.A.; Dixon, W.G.; Meguerditchian, A.N.; Tamblyn, R. Predictors of distress in female breast cancer survivors: A systematic review. Breast Cancer Res. Treat. 2017, 165, 229–245. [Google Scholar] [CrossRef]
- Robinson, R.G.; Jorge, R.E. Post-stroke depression: A review. Am. J. Psychiatry 2016, 173, 221–231. [Google Scholar] [CrossRef] [Green Version]
- Bautovich, A.; Katz, I.; Smith, M.; Loo, C.; Harvey, S. Depression and chronic kidney disease: A review for clinicians. Aust. N. Z. J. Psychiatry 2014, 48, 530–541. [Google Scholar] [CrossRef]
- Pan, A.; Keum, N.; Okereke, O.I.; Sun, Q.; Kivimaki, M.; Rubin, R.R.; Hu, F.B. Bidirectional association between depression and metabolic syndrome: A systematic review and meta-analysis of epidemiological studies. Diabetes Care 2012, 35, 1171–1180. [Google Scholar] [CrossRef] [Green Version]
- Opolski, M.; Wilson, I. Asthma and depression: A pragmatic review of the literature and recommendations for future research. Clin. Pract. Epidemiol. Ment. Health 2005, 1, 18. [Google Scholar] [CrossRef] [Green Version]
- Matcham, F.; Rayner, L.; Steer, S.; Hotopf, M. The prevalence of depression in rheumatoid arthritis: A systematic review and meta-analysis. Rheumatology 2013, 52, 2136–2148. [Google Scholar] [CrossRef] [Green Version]
- Smith, H.R. Depression in cancer patients: Pathogenesis, implications and treatment. Oncol. Lett. 2015, 9, 1509–1514. [Google Scholar] [CrossRef] [Green Version]
- Goldsmith, D.R.; Rapaport, M.H.; Miller, B.J. A meta-analysis of blood cytokine network alterations in psychiatric patients: Comparisons between schizophrenia, bipolar disorder and depression. Mol. Psychiatry 2016, 21, 1696–1709. [Google Scholar] [CrossRef]
- Osimo, E.F.; Baxter, L.J.; Lewis, G.; Jones, P.B.; Khandaker, G.M. Prevalence of low-grade inflammation in depression: A systematic review and meta-analysis of CRP levels. Psychol. Med. 2019, 49, 1958–1970. [Google Scholar] [CrossRef]
- Michels, N.; van Aart, C.; Morisse, J.; Mullee, A.; Huybrechts, I. Chronic inflammation towards cancer incidence: A systematic review and meta-analysis of epidemiological studies. Crit. Rev. Oncol. 2021, 157, 103177. [Google Scholar] [CrossRef] [PubMed]
- Prasad, S.; Sung, B.; Aggarwal, B.B. Age-associated chronic diseases require age-old medicine: Role of chronic inflammation. Prev. Med. 2012, 54, S29–S37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- EEdwards, B.K.; Ms, A.N.; Mariotto, A.B.; Simard, E.P.; Boscoe, F.P.; Henley, S.J.; Jemal, A.; Cho, H.; Anderson, R.N.; Kohler, B.A.; et al. Annual Report to the Nation on the status of cancer, 1975–2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer 2014, 120, 1290–1314. [Google Scholar] [CrossRef] [PubMed]
- Furman, D.; Campisi, J.; Verdin, E.; Carrera-Bastos, P.; Targ, S.; Franceschi, C.; Ferrucci, L.; Gilroy, D.W.; Fasano, A.; Miller, G.W.; et al. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 2019, 25, 1822–1832. [Google Scholar] [CrossRef] [PubMed]
- Mathew, A.; Doorenbos, A.Z.; Li, H.; Jang, M.K.; Park, C.G.; Bronas, U.G. Allostatic Load in Cancer: A Systematic Review and Mini Meta-Analysis. Biol. Res. Nurs. 2021, 23, 341–361. [Google Scholar] [CrossRef]
- McEwen, B.S. Allostasis and allostatic load: Implications for neuropsychopharmacology. Neuropsychopharmacology 2000, 22, 108–124. [Google Scholar] [CrossRef]
- Mao, J.J.; Armstrong, K.; Bowman, M.; Xie, S.X.; Kadakia, R.; Farrar, J.T. Symptom burden among cancer survivors: Impact of age and comorbidity. J. Am. Board Fam. Med. 2007, 20, 434–443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, A.W.; Reeve, B.B.; Bellizzi, K.M.; Harlan, L.C.; Klabunde, C.N.; Amsellem, M.; Bierman, A.S.; Hays, R.D. Cancer, comorbidities, and health-related quality of life of older adults. Health Care Financ. Rev. 2008, 29, 41–56. [Google Scholar] [PubMed]
- Sowislo, J.F.; Orth, U. Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychol. Bull. 2013, 139, 213–240. [Google Scholar] [CrossRef]
- Deimling, G.T.; Bowman, K.F.; Wagner, L.J. Cancer survivorship and identity among long-term survivors. Cancer Investig. 2007, 25, 758–765. [Google Scholar] [CrossRef]
- Harrington, C.B.; Hansen, J.A.; Moskowitz, M.; Todd, B.L.; Feuerstein, M. It’s not over when it’s over: Long-term symptoms in cancer survivors—a systematic review. Int. J. Psychiatry Med. 2010, 40, 163–181. [Google Scholar] [CrossRef]
- Gonçalves, V. Long-term quality of life in gynecological cancer survivors. Curr. Opin. Obstet. Gynecol. 2010, 22, 30–35. [Google Scholar] [CrossRef]
- Lopresti, A.L.; Hood, S.D.; Drummond, P.D. A review of lifestyle factors that contribute to important pathways associated with major depression: Diet, sleep and exercise. J. Affect. Disord. 2013, 148, 12–27. [Google Scholar] [CrossRef] [Green Version]
- Bergmann, M.M.; Calle, E.E.; Mervis, C.A.; Miracle-McMahill, H.L.; Thun, M.J.; Health, C.W. Validity of self-reported cancers in a propsective cohort study in comparison with data from state cancer registries. Am. J. Epidemiol. 1998, 147, 556–562. [Google Scholar] [CrossRef]
- Bergmann, M.M.; Byers, T.; Freedman, D.S.; Mokdad, A. Validity of self-reported diagnoses leading to hospitalization: A comparison of self-reports with hospital records in a prospective study of American adults. Am. J. Epidemiol. 1998, 147, 969–977. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Variable | Category | Recent Survivors n = 853 | Long-Term Survivors n = 1220 | p |
|---|---|---|---|---|
| Sex | Male | 49.4 | 40.9 | 0.007 |
| Female | 50.6 | 59.1 | ||
| Age | M ± SD | 58.6 (13.1) | 61.2 (11.9) | 0.001 |
| 18–39 | 10.4 | 6.9 | ||
| 40–59 | 37.2 | 31.4 | ||
| 60–79 | 52.4 | 61.7 | ||
| Race | Non-Hispanic White | 85.3 | 83.9 | 0.006 |
| Non-Hispanic Black | 6.7 | 5.3 | ||
| Other Hispanic | 2.8 | 2.8 | ||
| Mexican American | 2.7 | 2.9 | ||
| Other | 2.5 | 5.1 | ||
| Education | Less than 9th grade | 2.8 | 3.2 | 0.707 |
| 9–11th grade | 7.8 | 6.6 | ||
| High school graduate/GED | 20.8 | 19.5 | ||
| Some college or AA degree | 33.1 | 32.5 | ||
| College graduate or above | 35.5 | 38.2 | ||
| Civil status | Married or living with partner | 70.1 | 68.2 | 0.052 |
| Divorced or separated | 14.8 | 17.3 | ||
| Single, never married | 8.2 | 5.2 | ||
| Widowed | 6.9 | 9.3 | ||
| Insurance status | Insured | 95.4 | 92.8 | 0.095 |
| Uninsured | 4.6 | 7.2 | ||
| Cancer site | Skin non-melanoma | 27.7 | 19.7 | <0.001 |
| Melanoma | 6.8 | 7.7 | ||
| Skin unknown type | 8.6 | 8.5 | ||
| Breast | 13.8 | 15.2 | ||
| Gynecological | 7.9 | 18.6 | ||
| Genitourinary | 13.8 | 12.7 | ||
| Gastrointestinal | 6.2 | 4.4 | ||
| Other | 15.2 | 13.1 | ||
| Years since diagnosis | 1 year | 35.2 | - | - |
| 2 years | 18.4 | - | ||
| 3 years | 17.1 | - | ||
| 4 years | 14.3 | - | ||
| 5 years | 15.0 | - | ||
| 6–10 years | - | 40.6 | ||
| 11–20 years | - | 34.9 | ||
| 20+ years | - | 24.5 | ||
| Comorbidities total | M ± SD | 2.61 (2.06) | 2.67 (2.01) | 0.704 |
| None | 15.6 | 10.2 | ||
| One | 17.8 | 22.7 | ||
| Two | 19.9 | 20.1 | ||
| Three or more | 46.7 | 47.0 | ||
| Comorbidities pre-diagnosis | M ± SD | 2.45 (1.83) | 1.21(1.32) | <0.001 |
| None | 10.1 | 35.8 | ||
| One | 24.5 | 32.6 | ||
| Two | 23.9 | 16.5 | ||
| Three or more | 41.5 | 15.0 | ||
| Comorbidities post-diagnosis | M ± SD | 0.55 (0.78) | 1.84 (1.44) | <0.001 |
| None | 58.2 | 14.5 | ||
| One | 31.9 | 33.4 | ||
| Two or more | 9.9 | 52.1 | ||
| Physical function limitations | No limitations | 64.6 | 62.2 | 0.431 |
| Limited | 20.1 | 23.2 | ||
| Disabled | 15.3 | 14.6 | ||
| Depression (PHQ-9 ≥ 10) | Depressed | 8.4 | 8.8 | 0.754 |
| Not depressed | 91.6 | 91.2 |
| Recent Survivors | Long-Term Survivors | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | Matched Controls | Cases | Matched Controls | ||||||||
| Total N | Observed N with PHQ-9 ≥ 10 | Prevalence (weighted % and 95% CI) | Observed N with PHQ-9 ≥ 10 | Prevalence (weighted % and 95% CI) | N | Observed N with PHQ-9 ≥ 10 | Prevalence (weighted % and 95% CI) | Observed N with PHQ-9 ≥ 10 | Prevalence (weighted % and 95% CI) | ||
| Cancer site | All | 853 | 89 | 8.4 (6.1, 11.2) | 70 | 7.5 (5.5, 9.9) | 1220 | 139 | 8.8 (6.9, 11.0) *^ | 89 | 5.6 (3.9, 7.6) |
| All except skin non-mel. | 708 | 83 | 10.3 (7.4, 13.9) | 61 | 7.7 (5.5, 10.5) | 1059 | 131 | 9.7 (7.7, 11.9) *^ | 78 | 6.0 (4.2, 8.3) | |
| Skin non-melanoma | 145 | 6 | 3.2 (0.7, 9.1) | 9 | 6.7 (2.1, 15.3) | 161 | 8 | 5.5 (2.2, 11.0) | 11 | 3.3 (1.4, 6.5) | |
| Melanoma | 44 | 2 | 6.6 (0.1, 37.2) | 3 | 3.8 (0.1, 18.1) | 70 | 7 | 8.9 (2.2, 22.4) | 10 | 11.1 (2.1, 30.6) | |
| Skin unknown type | 60 | 6 | 5.9 (0.5, 21.3) | 4 | 6.9 (0.4, 27.6) | 88 | 12 | 12.6 (4.8, 25.4) ^ | 5 | 2.1 (0.6, 5.5) | |
| Breast | 128 | 22 | 16.6 (7.8, 29.3) | 16 | 11.7 (4.8, 22.7) | 202 | 23 | 8.6 (3.5, 17.0) | 12 | 3.6 (1.4, 7.5) | |
| Gynecological | 74 | 18 | 19.1 (7.6, 36.6) * | 6 | 7.6 (1.3, 23.3) | 229 | 44 | 14.0 (8.9, 20.7) *^ | 21 | 8.1 (4.3, 13.6) | |
| Genitourinary | 189 | 11 | 7.0 (2.6, 14.6) | 11 | 6.1 (2.6, 12.0) | 216 | 14 | 4.1 (1.8, 8.1) | 13 | 4.2 (1.9, 8.0) | |
| Digestive/gastrointest. | 79 | 13 | 11.9 (4.7, 23.6) | 6 | 7.9 (3.0, 16.2) | 83 | 14 | 12.7 (4.8, 25.7) | 8 | 10.1 (1.8, 28.6) | |
| Other | 134 | 11 | 6.7 (2.4, 14.6) | 15 | 7.5 (3.2, 14.5) | 171 | 17 | 7.5 (3.9, 12.9) | 9 | 5.0 (1.6, 11.5) | |
| Time since diagnosis (all except skin non-mel.) | 1 year | 238 | 29 | 12.4 (7.1, 19.6)^ | 17 | 4.4 (2.3, 7.6) | - | ||||
| 2 years | 139 | 17 | 9.1 (4.0, 17.2) | 12 | 10.3 (3.1, 23.4) | - | |||||
| 3 years | 117 | 15 | 10.9 (4.0, 22.8) | 12 | 10.0 (4.4, 18.8) | - | |||||
| 4 years | 94 | 13 | 8.8 (3.9, 16.6) | 7 | 6.9 (2.3, 15.3) | - | |||||
| 5 years | 120 | 9 | 8.1 (4.5, 13.2) | 13 | 9.5 (4.6, 16.9) | - | |||||
| 6–10 years | - | 430 | 40 | 7.9 (5.9, 10.2) | 31 | 6.0 (3.4, 9.6) | |||||
| 11–20 years | - | 383 | 59 | 11.4 (7.8, 15.9) *^ | 30 | 5.6 (3.0, 9.3) | |||||
| >20 years | - | 246 | 32 | 10.1 (5.7, 16.1) * | 17 | 6.6 (2.8, 12.9) | |||||
| Table | Comorbidities Total | Comorbidities Pre-Diagnosis | |
|---|---|---|---|
| N | OR (95% CI) | OR (95% CI) | |
| All * | 853 | 1.54 (1.29, 1.84) | 1.51 (1.22, 1.87) |
| All except skin non-melanoma * | 708 | 1.57 (1.30, 1.89) | 1.63 (1.30, 2.03) |
| Skin non-melanoma ** | 145 | 1.52 (1.00, 2.30) | 1.45 (1.10, 1.91) |
| Skin (melanoma and skin unknown type) ** | 104 | 1.39 (0.87, 2.20) | 1.39 (0.87, 2.21) |
| Breast ** | 128 | 2.49 (1.63, 3.81) | 2.32 (1.60, 3.36) |
| Gynecological ** | 74 | 1.53 (1.12, 2.09) | 1.40 (0.96, 2.05) |
| Genitourinary ** | 189 | 1.61 (1.20, 2.16) | 1.77 (1.16, 2.70) |
| Digestive/gastrointestinal ** | 79 | 0.95 (0.65, 1. 39) | 1.02 (0.63, 1.64) |
| Skin ** | 104 | 1.39 (0.87, 2.20) | 1.39 (0.87, 2.21) |
| Other ** | 134 | 1.32 (0.84, 2.06) | 1.14 (0.78, 1.66) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petrova, D.; Catena, A.; Rodríguez-Barranco, M.; Redondo-Sánchez, D.; Bayo-Lozano, E.; Garcia-Retamero, R.; Jiménez-Moleón, J.-J.; Sánchez, M.-J. Physical Comorbidities and Depression in Recent and Long-Term Adult Cancer Survivors: NHANES 2007–2018. Cancers 2021, 13, 3368. https://doi.org/10.3390/cancers13133368
Petrova D, Catena A, Rodríguez-Barranco M, Redondo-Sánchez D, Bayo-Lozano E, Garcia-Retamero R, Jiménez-Moleón J-J, Sánchez M-J. Physical Comorbidities and Depression in Recent and Long-Term Adult Cancer Survivors: NHANES 2007–2018. Cancers. 2021; 13(13):3368. https://doi.org/10.3390/cancers13133368
Chicago/Turabian StylePetrova, Dafina, Andrés Catena, Miguel Rodríguez-Barranco, Daniel Redondo-Sánchez, Eloísa Bayo-Lozano, Rocio Garcia-Retamero, José-Juan Jiménez-Moleón, and María-José Sánchez. 2021. "Physical Comorbidities and Depression in Recent and Long-Term Adult Cancer Survivors: NHANES 2007–2018" Cancers 13, no. 13: 3368. https://doi.org/10.3390/cancers13133368
APA StylePetrova, D., Catena, A., Rodríguez-Barranco, M., Redondo-Sánchez, D., Bayo-Lozano, E., Garcia-Retamero, R., Jiménez-Moleón, J.-J., & Sánchez, M.-J. (2021). Physical Comorbidities and Depression in Recent and Long-Term Adult Cancer Survivors: NHANES 2007–2018. Cancers, 13(13), 3368. https://doi.org/10.3390/cancers13133368







