HCC in the Era of Direct-Acting Antiviral Agents (DAAs): Surgical and Other Curative or Palliative Strategies in the Elderly
Abstract
Simple Summary
Abstract
1. Introduction
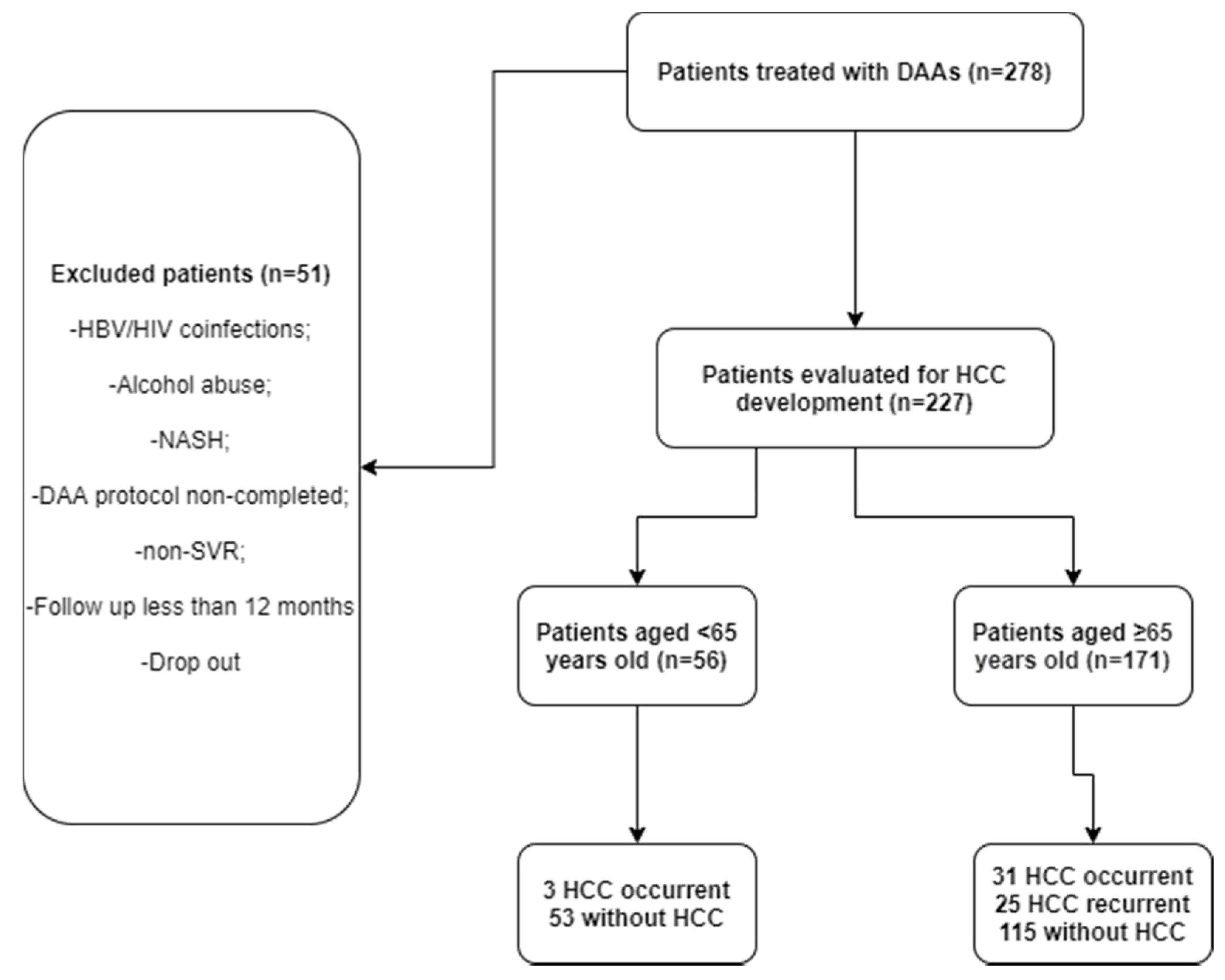
2. Methods
2.1. Study Setting and Participants
2.2. Statistical Analysis
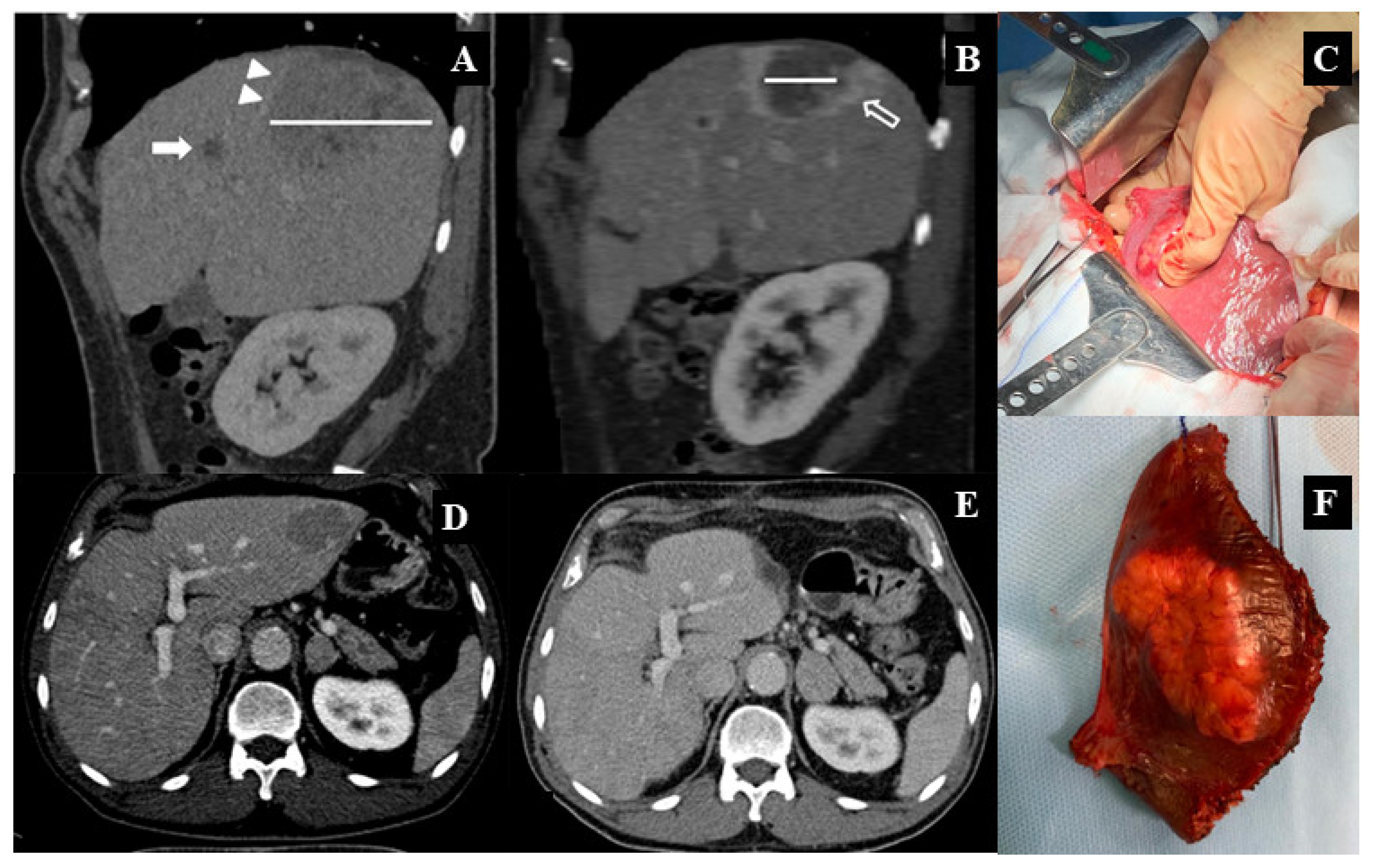
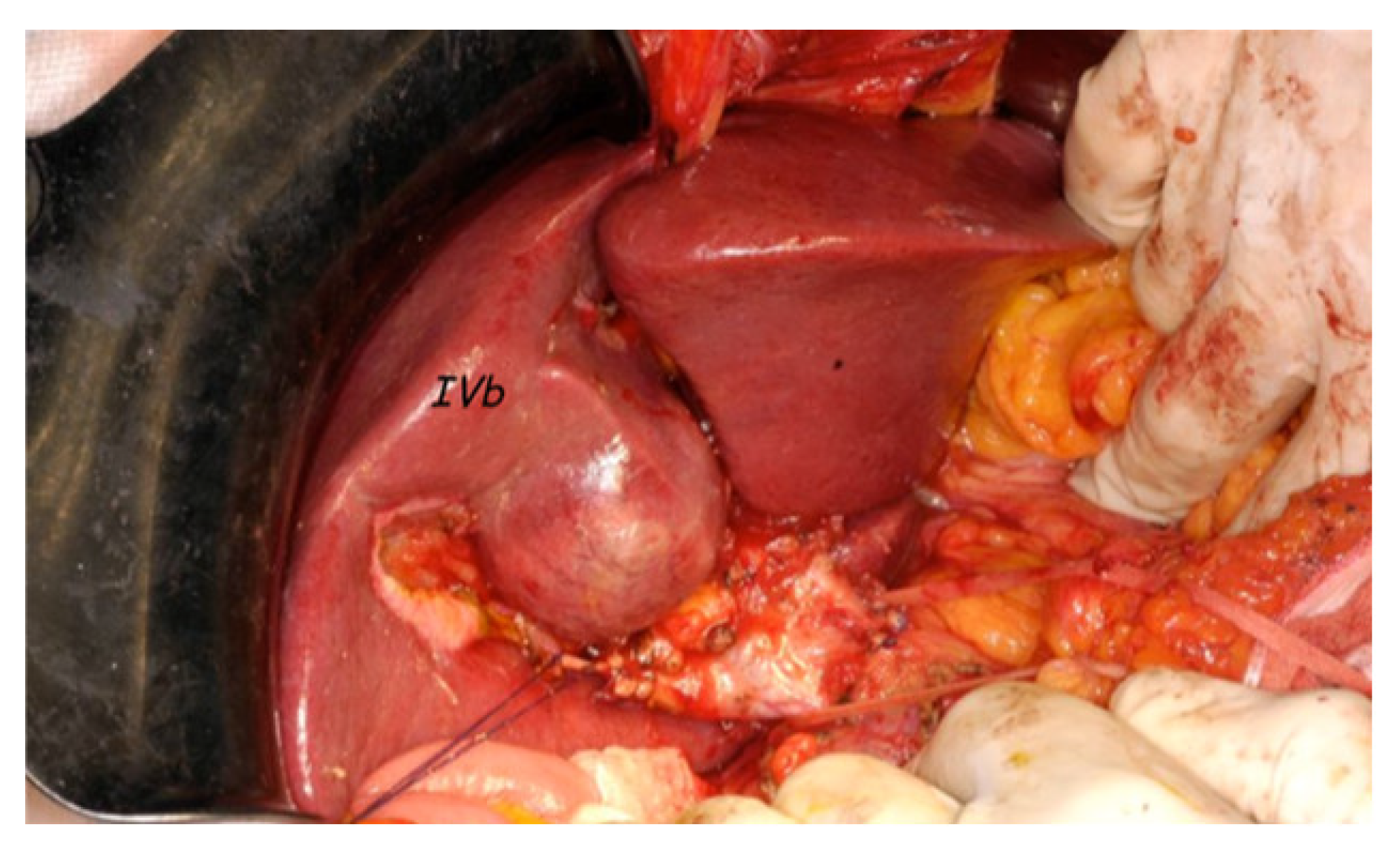
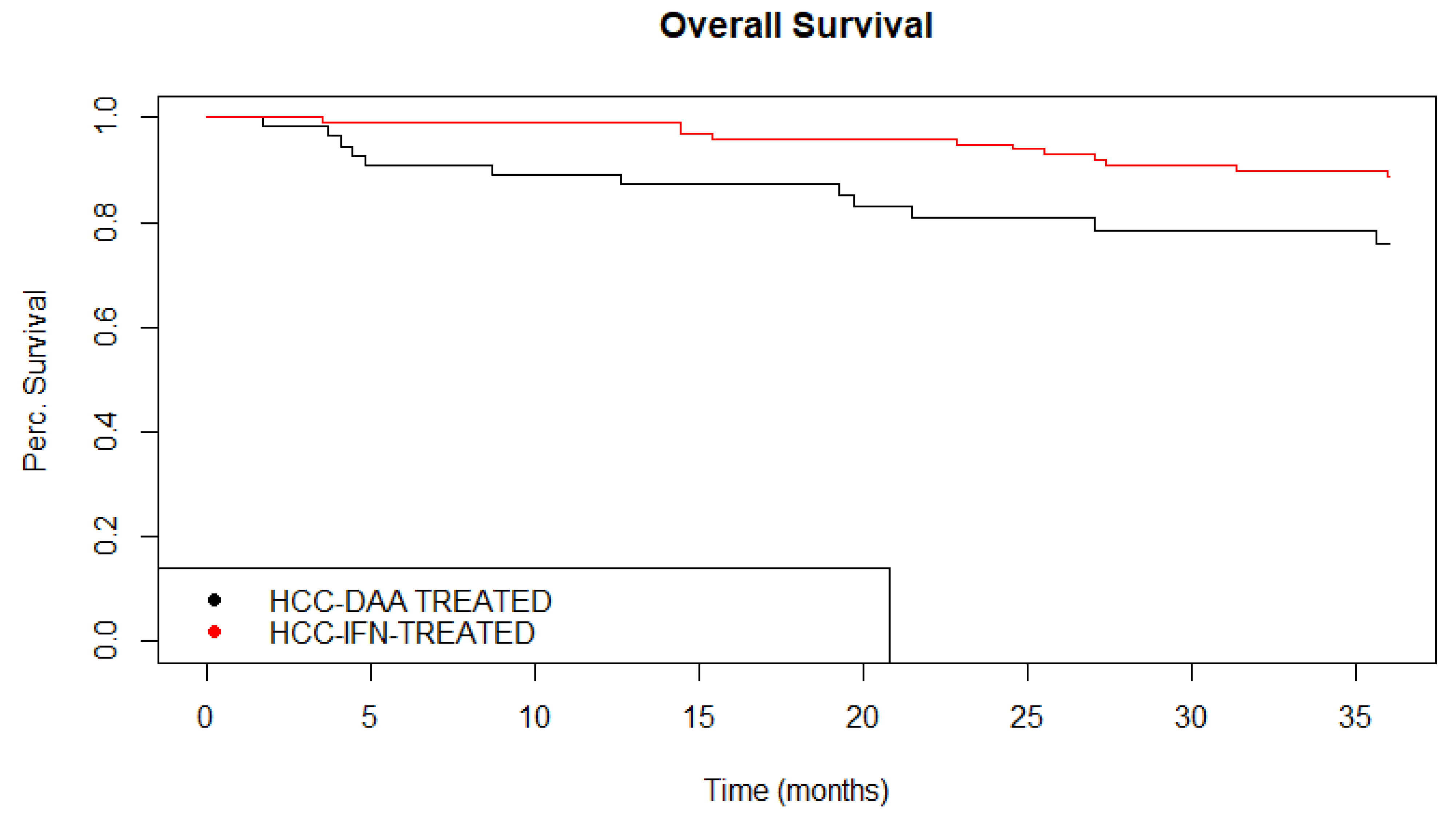
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- World Health Organization, International Agency for Research on Cancer. GLOBOCAN 2020. Available online: http://globocan.iarc.fr (accessed on 15 April 2021).
- Lanini, S.; Ustianowski, A.; Pisapia, R.; Zumla, A.; Ippolito, G. Viral Hepatitis: Etiology, Epidemiology, Transmission, Diagnostics, Treatment, and Prevention. Infect. Dis. Clin. N. Am. 2019, 33, 1045–1062. [Google Scholar] [CrossRef] [PubMed]
- El-Serag, H.B. Hepatocellular carcinoma. N. Engl. J. Med. 2011, 365, 1118–1127. [Google Scholar] [CrossRef] [PubMed]
- Kulik, L.; El-Serag, H.B. Epidemiology and Management of Hepatocellular Carcinoma. Gastroenterology 2019, 156, 477–491. [Google Scholar] [CrossRef] [PubMed]
- Lok, A.S.; Seeff, L.B.; Morgan, T.R.; di Bisceglie, A.M.; Sterling, R.K.; Curto, T.M.; Everson, G.T.; Lindsay, K.L.; Lee, W.M.; Bonkovsky, H.L.; et al. Incidence of hepatocellular carcinoma and associated risk factors in hepatitis c-related advanced liver disease. Gastroenterology 2009, 136, 138–148. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, A.-C.; Moucari, R.; Figueiredo-Mendes, C.; Ripault, M.-P.; Giuily, N.; Castelnau, C.; Boyer, N.; Asselah, T.; Martinot-Peignoux, M.; Maylin, S.; et al. Impact of peginterferon and ribavirin therapy on hepatocellular carcinoma: Incidence and survival in hepatitis C patients with advanced fibrosis. J. Hepatol. 2010, 52, 652–657. [Google Scholar] [CrossRef]
- Coppola, N.; Pisaturo, M.; Tonziello, G.; Sagnelli, C.; Sagnelli, E.; Angelillo, I.F. Efficacy of pegylated interferon α-2a and α-2b in patients with genotype 1 chronic hepatitis C: A meta-analysis. BMC Infect. Dis. 2012, 12, 357. [Google Scholar] [CrossRef][Green Version]
- Wei, L.; Huang, Y.-H. Long-term outcomes in patients with chronic hepatitis C in the current era of direct-acting antiviral agents. Expert Rev. Anti-Infect. Ther. 2019, 17, 311–325. [Google Scholar] [CrossRef]
- Carrat, F.; Fontaine, H.; Dorival, C.; Simony, M.; Diallo, A.; Hezode, C.; De Ledinghen, V.; Larrey, D.; Haour, G.; Bronowicki, J.-P.; et al. Clinical outcomes in patients with chronic hepatitis C after direct-acting antiviral treatment: A prospective cohort study. Lancet 2019, 393, 1453–1464. [Google Scholar] [CrossRef]
- Registri AIFA Per il Monitoraggio Dei Farmaci Anti-HCV (Aggiornamento del 29 March 2021). Available online: https://www.aifa.gov.it/aggiornamento-epatite-c (accessed on 20 April 2021).
- Reig, M.; Mariño, Z.; Perelló, C.; Iñarrairaegui, M.; Ribeiro, A.; Lens, S.; Díaz, A.; Vilana, R.; Darnell, A.; Varela, M.; et al. Unexpected high rate of early tumor recurrence in patients with HCV-related HCC undergoing interferon-free therapy. J. Hepatol. 2016, 65, 719–726. [Google Scholar] [CrossRef]
- Conti, F.; Buonfiglioli, F.; Scuteri, A.; Crespi, C.; Bolondi, L.; Caraceni, P.; Foschi, F.G.; Lenzi, M.; Mazzella, G.; Verucchi, G.; et al. Early occurrence and recurrence of hepatocellular carcinoma in HCV-related cirrhosis treated with direct-acting antivirals. J. Hepatol. 2016, 65, 727–733. [Google Scholar] [CrossRef]
- Romano, A.; Angeli, P.; Piovesan, S.; Noventa, F.; Anastassopoulos, G.; Chemello, L.; Cavalletto, L.; Gambato, M.; Russo, F.P.; Burra, P.; et al. Newly diagnosed hepatocellular carcinoma in patients with advanced hepatitis C treated with DAAs: A prospective population study. J. Hepatol. 2018, 69, 345–352. [Google Scholar] [CrossRef]
- Piñero, F.; Mendizabal, M.; Ridruejo, E.; Wolff, F.H.; Ameigeiras, B.; Anders, M.; Schinoni, M.I.; Reggiardo, V.; Palazzo, A.; Videla, M.; et al. Treatment with direct-acting antivirals for HCV decreases but does not eliminate the risk of hepatocellular carcinoma. Liver Int. 2019, 39, 1033–1043. [Google Scholar] [CrossRef]
- Vallet-Pichard, A.; Mallet, V.; Nalpas, B.; Verkarre, V.; Nalpas, A.; Dhalluin-Venier, V.; Fontaine, H.; Pol, S. FIB-4: An inexpensive and accurate marker of fibrosis in HCV infection. comparison with liver biopsy and fibrotest. Hepatology 2007, 46, 32–36. [Google Scholar] [CrossRef]
- Ioannou, G.N.; Beste, L.A.; Green, P.K.; Singal, A.G.; Tapper, E.B.; Waljee, A.K.; Sterling, R.K.; Feld, J.J.; Kaplan, D.E.; Taddei, T.H.; et al. Increased risk for hepatocellular carcinoma persists up to 10 years after hcv eradication in patients with baseline cirrhosis or high FIB-4 scores. Gastroenterology 2019, 157, 1264–1278.e4. [Google Scholar] [CrossRef]
- Maurice, J.; Pinzani, M. The stratification of cirrhosis. Hepatol. Res. 2020, 50, 535–541. [Google Scholar] [CrossRef]
- Pawlotsky, J.-M.; Negro, F.; Aghemo, A.; Berenguer, M.; Dalgard, O.; Dusheiko, G.; Marra, F.; Puoti, M.; Wedemeyer, H. EASL Recommendations on Treatment of Hepatitis C 2018. J. Hepatol. 2018, 69, 461–511. [Google Scholar] [CrossRef] [PubMed]
- Llovet, J.M.; Brú, C.; Bruix, J. Prognosis of Hepatocellular Carcinoma: The BCLC Staging Classification. Semin. Liver Dis. 1999, 19, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Subramaniam, S.; Kelley, R.K.; Venook, A.P. A review of hepatocellular carcinoma (HCC) staging systems. Chin. Clin. Oncol. 2013, 2, 33. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver. Electronic address eee, European Association for the Study of the L. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Saviano, A.; Erstad, D.J.; Hoshida, Y.; Fuchs, B.C.; Baumert, T.; Tanabe, K.K. Risk Factors, Pathogenesis, and Strategies for Hepatocellular Carcinoma Prevention: Emphasis on Secondary Prevention and Its Translational Challenges. J. Clin. Med. 2020, 9, 3817. [Google Scholar] [CrossRef]
- Hu, C.-C.; Weng, C.-H.; Hua, M.-C.; Chang, P.-H.; Lin, C.-L.; Chen, Y.-T.; Chien, C.-H.; Lin, S.-T.; Chien, R.-N. New Scoring Method to Predict Risk of Hepatocellular Carcinoma in Patients with Chronic Hepatitis C After Pegylated Interferon and Ribavirin Therapy. J. Interf. Cytokine Res. 2020, 40, 82–91. [Google Scholar] [CrossRef]
- Dash, S.; Aydin, Y.; Widmer, K.E.; Nayak, L. Hepatocellular Carcinoma Mechanisms Associated with Chronic HCV Infection and the Impact of Direct-Acting Antiviral Treatment. J. Hepatocell. Carcinoma 2020, 7, 45–76. [Google Scholar] [CrossRef] [PubMed]
- Kozbial, K.; Moser, S.; Schwarzer, R.; Laferl, H.; Al-Zoairy, R.; Stauber, R.; Stättermayer, A.F.; Beinhardt, S.; Graziadei, I.; Freissmuth, C.; et al. Unexpected high incidence of hepatocellular carcinoma in cirrhotic patients with sustained virologic response following interferon-free direct-acting antiviral treatment. J. Hepatol. 2016, 65, 856–858. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, H.; Vale, A.M.; Rodrigues, S.; Gonçalves, R.; Albuquerque, A.; Pereira, P.; Lopes, S.; Silva, M.; Andrade, P.; Morais, R.; et al. High incidence of hepatocellular carcinoma following successful interferon-free antiviral therapy for hepatitis C associated cirrhosis. J. Hepatol. 2016, 65, 1070–1071. [Google Scholar] [CrossRef] [PubMed]
- Ravi, S.; Axley, P.; Jones, D.; Kodali, S.; Simpson, H.; McGuire, B.M.; Singal, A.K. Unusually High Rates of Hepatocellular Carcinoma After Treatment with Direct-Acting Antiviral Therapy for Hepatitis C Related Cirrhosis. Gastroenterology 2017, 152, 911–912. [Google Scholar] [CrossRef] [PubMed]
- Mashiba, T.; Joko, K.; Kurosaki, M.; Ochi, H.; Osaki, Y.; Kojima, Y.; Nakata, R.; Goto, T.; Takehiro, A.; Kimura, H.; et al. Does interferon-free direct-acting antiviral therapy for hepatitis C after curative treatment for hepatocellular carcinoma lead to unexpected recurrences of HCC? A multicenter study by the Japanese Red Cross Hospital Liver Study Group. PLoS ONE 2018, 13, e0194704. [Google Scholar] [CrossRef]
- Guarino, M.; Sessa, A.; Cossiga, V.; Morando, F.; Caporaso, N.; Morisco, F. Direct-acting antivirals and hepatocellular carcinoma in chronic hepatitis C: A few lights and many shadows. World J. Gastroenterol. 2018, 24, 2582–2595. [Google Scholar] [CrossRef]
- Yamada, R.; Hiramatsu, N.; Oze, T.; Urabe, A.; Tahata, Y.; Morishita, N.; Kodama, T.; Hikita, H.; Sakamori, R.; Yakushijin, T.; et al. Incidence and risk factors of hepatocellular carcinoma change over time in patients with hepatitis C virus infection who achieved sustained virologic response. Hepatol. Res. 2019, 49, 570–578. [Google Scholar] [CrossRef]
- Issa, D.; Dessie, S.; Matherly, S. Unusually Aggressive Hepatocellular Carcinoma Developing After Treatment of Hepatitis C with Direct-Acting Antivirals. Am. J. Gastroenterol. 2017, 112, 1184–1185. [Google Scholar] [CrossRef]
- El Fayoumie, M.; Abdelhady, M.; Gawish, A.; Hantour, U.; Abdelkhaleek, I.; Abdelraheem, M.; Alsawak, A.; Alwassief, A.; Elbahrawy, A. Changing Patterns of Hepatocellular Carcinoma after Treatment with Direct Antiviral Agents. Gastrointest. Tumors 2020, 7, 1–10. [Google Scholar] [CrossRef]
- Brozzetti, S.; Bini, S.; Fazzi, K.; Chiarella, L.L.; Ceccarossi, V.; De Lucia, C.; De Toma, G. Case-report: Metastases in a low-stage middle-graded HCC in cleared HCV infection, non-cirrhotic liver: Surgical therapy. Int. J. Surg. Case Rep. 2018, 47, 19–21. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.; Sandhu, S.; Lai, J.-P.; Sandhu, D.S. Hepatocellular carcinoma in non-cirrhotic liver: A comprehensive review. World J. Hepatol. 2019, 11, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Yeh, M.M.; Daniel, H.D.-J.; Torbenson, M. Hepatitis C-associated hepatocellular carcinomas in non-cirrhotic livers. Mod. Pathol. 2009, 23, 276–283. [Google Scholar] [CrossRef]
- Goossens, N.; Hoshida, Y. Hepatitis C virus-induced hepatocellular carcinoma. Clin. Mol. Hepatol. 2015, 21, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Shirvani-Dastgerdi, E.; Schwartz, R.E.; Ploss, A. Hepatocarcinogenesis associated with hepatitis B, delta and C viruses. Curr. Opin. Virol. 2016, 20, 1–10. [Google Scholar] [CrossRef]
- Liu, P.; Ge, M.; Hu, J.; Li, X.; Che, L.; Sun, K.; Cheng, L.; Huang, Y.; Pilo, M.G.; Cigliano, A.; et al. A functional mammalian target of rapamycin complex 1 signaling is indispensable for c-Myc-driven hepatocarcinogenesis. Hepatology 2017, 66, 167–181. [Google Scholar] [CrossRef] [PubMed]
- Chu, P.-S.; Nakamoto, N.; Taniki, N.; Ojiro, K.; Amiya, T.; Makita, Y.; Murata, H.; Yamaguchi, A.; Shiba, S.; Miyake, R.; et al. On-treatment decrease of NKG2D correlates to early emergence of clinically evident hepatocellular carcinoma after interferon-free therapy for chronic hepatitis C. PLoS ONE 2017, 12, e0179096. [Google Scholar] [CrossRef] [PubMed]
- Collins, J.M.; Raphael, K.L.; Terry, C.; Cartwright, E.J.; Pillai, A.A.; Anania, F.A.; Farley, M.M. Hepatitis B Virus Reactivation During Successful Treatment of Hepatitis C Virus with Sofosbuvir and Simeprevir. Clin. Infect. Dis. 2015, 61, 1304–1306. [Google Scholar] [CrossRef]
- Fernández-Carrillo, C.; Londoño, M.-C.; Arias-Loste, T.; Hernández-Conde, M.; Llerena, S.; Crespo, J.; Forns, X.; Calleja, J.L. Reactivation of Herpesvirus in Patients with Hepatitis C Treated with Direct-Acting Antiviral Agents. Clin. Gastroenterol. Hepatol. 2016, 14, 1662–1666. [Google Scholar] [CrossRef]
| Variable | HCC-O (n = 31) | HCC-R (n = 25) | Without HCC (n = 115) | Total (n = 171) | p Value |
|---|---|---|---|---|---|
| Age, years, median (IQR) | 73 (67–81.50) | 69 (67–75) | 74 (67–80) | 73 (67–80) | 0.315 |
| Male, n (%) | 25 (80.65) | 18 (72) | 54 (46.96) | 97 (56.73) | <0.001 |
| Female, n (%) | 6 (19.35) | 7 (28) | 61 (53.04) | 74 (43.27) | |
| BMI, kg/m2, median (IQR) | 26.10 (25.5–26.5) | 26.10 (26–26.5) | 26 (25.5–26.8) | 26 (25.5–26.7) | 0.672 |
| Comorbidities, n (%) | |||||
| Obesity | 2 (6.45) | 1 (4) | 16 (13.91) | 19 (11.11) | 0.373 |
| Diabetes mellitus 2 | 7 (22.58) | 4 (16) | 13 (11.3) | 24 (14.04) | 0.239 |
| Metabolic syndrome | 5 (16.13) | 3 (12) | 12 (10.43) | 20 (11.17) | 0.592 |
| Chronic obstructive pulmonary diseases | 3 (9.68) | 2 (8) | 4 (3.48) | 9 (5.26) | 0.203 |
| Cardiovascular diseases | 5 (16.13) | 4 (16) | 0 (0) | 9 (5.26) | <0.001 |
| Kidney failure | 4 (12.9) | 3 (12) | 17 (14.78) | 24 (14.04) | 1 |
| Hypertension | 11 (35.48) | 7 (28) | 27 (23.48) | 45 (26.32) | 0.372 |
| Hemoglobin disorders | 2 (6.45) | 2 (8) | 5 (4.35) | 9 (5.26) | 0.666 |
| Autoimmune diseases | 3 (9.68) | 2 (8) | 2 (1.74) | 7 (4.09) | 0.053 |
| ASA, n (%) | 0.336 | ||||
| I | 21 (67.74) | 13 (52) | 60 (52.17) | 94 (54.97) | |
| II | 9 (29.03) | 11 (44) | 55 (47.83) | 75 (43.86) | |
| III | 1 (3.23) | 1 (4) | 0 (0) | 2 (1.17) | |
| HCV Genotype, n (%) | 0.8693 | ||||
| 1 | 19 (61.29) | 17 (68) | 73 (63.48) | 109 (63.74) | |
| Non-1 | 12 (38.71) | 8 (32) | 42 (36.52) | 62 (36.26) | |
| Child–Turcotte–Pugh score, n (%) | 1 | ||||
| A | 29 (93.55) | 108 (93.91) | 161 (94.15) | ||
| B | 2 (6.45) | 7 (6.09) | 10 (5.85) | ||
| C | 0 (0) | 0 (0) | 0 (0) | ||
| MELD, median (IQR) | 9 (7–11.5) | 9 (7–11) | 8 (7–9) | 8 (7–10) | 0.095 |
| METAVIR, n (%) | 0.385 | ||||
| F0-1 | 7 (22.58) | 11 (44) | 32 (27.83) | 50 (29.24) | |
| F2 | 4 (12.90) | 2 (8) | 17 (14.78) | 23 (13.45) | |
| F3 | 5 (16.13) | 4 (16) | 10 (8.70) | 19 (11.11) | |
| F4 | 15 (48.39) | 8 (32) | 56 (48.70) | 79 (46.20) | |
| FIB-4, median (IQR) | 4 (2.34–5.83) | 4.19 (2.95–6) | 3.21 (1.74–6.17) | 3.56 (1.95–6.08) | 0.246 |
| Stiffness, median (IQR) | 12 (8.63–16.8) | 10.4 (6–14) | 12.5 (6.8–18.6) | 11.8 (6.4–17.05) | 0.218 |
| Steatosis | 2 (6.45) | 2 (8) | 26 (22.61) | 30 (17.54) | 0.055 |
| Platelets, 109/L, median (Range) | 147 (42–362) | 153 (32–464) | 143 (29–350) | 147 (29–464) | 0.899 |
| Varices, n (%) | 0.072 | ||||
| 0 | 22 (70.97) | 12 (48) | 84 (73.04) | 118 (69.01) | |
| 1 | 8 (25.81) | 13 (52) | 27 (23.48) | 48 (28.07) | |
| 2 | 1 (3.23) | 0 (0) | 4 (3.48) | 5 (2.92) | |
| AFP pre-DAA, UI/L, median (IQR) | 4.5 (2.8–9.32) | 4.6 (3–6.4) | 2.4 (1.12–4.11) | 3 (1.45–5.05) | <0.001 |
| DAA, n (%) | 0.9164 | ||||
| SOF-Based | 26 (83.87) | 20 (80) | 92 (80) | 138 (80.70) | |
| Non-SOF-Based | 5 (16.13) | 5 (20) | 23 (20) | 33 (19.30) |
| Variable | HCC-O | HCC-R | TOTAL | p Value |
|---|---|---|---|---|
| Age, years, median (IQR) | 73 (67–81.50) | 69 (67–75) | 70 (66.75–80) | 0.271 |
| Male, n (%) | 25 (80.65) | 18 (72) | 43 (76.79) | 0.657 |
| Female, n (%) | 6 (19.35) | 7 (28) | 13 (23.21) | |
| BMI, kg/m2, median (IQR) | 26.10 (25.5–26.5) | 26.10 (26–26.5) | 26.10 (25.65–26.5) | 0.409 |
| HCV Genotype, n (%) | 0.81 | |||
| 1 | 19 (61.29) | 17 (68) | 36 (64.29) | |
| Non-1 | 12 (38.71) | 8 (32) | 20 (35.71) | |
| DAA, n (%) | 0.738 | |||
| SOF-Based | 26 (83.87) | 20 (80) | 46 (82.14) | |
| Non-SOF-Based | 5 (16.13) | 5 (20) | 10 (17.86) | |
| Onset from SVR (months), median (IQR), (Range) | 14 (7.5–23.5) | 13 (5–22) | 14 (7–23.25) | 0.287 |
| (3–57) | (1–41) | (1–57) | ||
| Numbers of nodules, n (%) | 0.631 | |||
| 1 | 11 (35.48) | 12 (48) | 23 (41.07) | |
| 2 | 6 (19.35) | 3 (12) | 9 (16.07) | |
| 3 | 14 (45.16) | 10 (40) | 24 (42.86) | |
| HCC size (cm), median, (Range) | 2.8 (1–8) | 2.2 (0.8–5.1) | 2.6 (0.8–8) | 0.225 |
| Site, n (%) | 0.958 | |||
| Right liver | 21 (67.74) | 18 (72) | 39 (69.64) | |
| Left liver | 10 (32. 26) | 7 (28) | 17 (30.36) | |
| BCLC STAGE, n (%) | 0.874 | |||
| 0-A | 13 (41.935) | 12 (48) | 25 (44.64) | |
| B | 13 (41.935) | 9 (36) | 22 (39.29) | |
| C | 5 (16.13) | 4 (16) | 9 (16.07) | |
| I Treatment, n (%) | 1 | |||
| Curative treatments | 12 (38.71) | 10 (40) | 22 (39.29) | |
| Palliative treatments | 19 (61.29) | 15 (60) | 34 (60.71) | |
| II Treatments, n (%) | 8 (25.81) | 9 (36) | 17 (30.36) | 0.594 |
| Curative treatments | 2 (25) | 2 (22.2) | 4 (23.53) | |
| Palliative treatments | 6 (75) | 7 (77.8) | 13 (76.47) | |
| III treatments, n (%) | 2 (6.45) | 3 (12) | 5 (8.93) | 0.647 |
| Curative treatments | 0 (0) | 1 (33.33) | 1 (20) | |
| Palliative treatments | 2 (100) | 2 (66.67) | 4 (80) |
| Variable | DAA-HCC (n = 56) | h-HCC (n = 100) | p Value |
|---|---|---|---|
| Age, years, median (IQR) | 70 (66.75–80) | 74.50 (70–79) | 0.064 |
| Male, n (%) | 43 (76.69) | 67 (67) | 0.270 |
| Female, n (%) | 13 (23.21) | 33 (33) | |
| BMI, Kg/m2, median (IQR) | 26.10 (25.65–26.5) | 27 (26–28) | <0.001 |
| Comorbidities, n (%) | |||
| Hypertension | 7 (12.5) | 71 (71) | <0.001 |
| Cardiovascular diseases | 5 (8.93) | 19 (19) | 0.149 |
| Pulmonary diseases | 5 (8.93) | 41 (41) | <0.001 |
| Kidney failure | 9 (16.07) | 1 (1) | <0.001 |
| Diabetes mellitus 2 | 11 (19.64) | 20 (20) | 1 |
| Metabolic syndrome | 8 (14.26) | 2 (2) | 0.004 |
| Malnutrition | 0 (0) | 3 (3) | 0.553 |
| Characteristics of nodules | 0.035 | ||
| Single | 23 (41.07) | 60 (60) | |
| Multiple | 33 (58.93) | 40 (40) | |
| HCC size (cm), median, (Range) | 2.6 (0.8–8) | 2.65 (1–12.3) | 0.629 |
| Site, n (%) | 0.433 | ||
| Right liver | 39 (69.64) | 62 (62) | |
| Left liver | 17 (30.36) | 38 (38) | |
| I Treatment, n (%) | <0.001 | ||
| Curative treatments | 22 (39.29) | 72 (72) | |
| Palliative treatments | 34 (60.71) | 28 (28) | |
| II treatment, n (%) | 17 (30.36) | 70 (70) | <0.001 |
| Curative treatments | 4 (23.53) | 40 (57.14) | 0.027 |
| Palliative treatments | 13 (76.47) | 30 (42.86) | |
| 3-year OS, survival % | 76.02 | 88.93 | 0.6 |
| (IC 95%) | (64.90–89.04) | (82.96–95.32) | |
| Death, n (%) | 13 (23.21) | 52 (52) | 0.008 |
| Cause of death, n (%) | |||
| HCC | 7 (53.85) | 13 (25) | 0.089 |
| Liver disease/Cirrhosis | 2 (15.38) | 24 (46.15) | 0.059 |
| Other | 4 (30.77) | 15 (28.85) | 1 |
| HCC vs. Liver disease/Cirrhosis, n (%) | 0.0288 | ||
| HCC | 7 (77.78) | 13 (35.14) | |
| Liver disease/Cirrhosis | 2 (22.22) | 24 (64.86) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brozzetti, S.; Tancredi, M.; Bini, S.; De Lucia, C.; Antimi, J.; D’Alterio, C.; De Sanctis, G.M.; Furlan, C.; Malpassuti, V.C.; Lucatelli, P.; et al. HCC in the Era of Direct-Acting Antiviral Agents (DAAs): Surgical and Other Curative or Palliative Strategies in the Elderly. Cancers 2021, 13, 3025. https://doi.org/10.3390/cancers13123025
Brozzetti S, Tancredi M, Bini S, De Lucia C, Antimi J, D’Alterio C, De Sanctis GM, Furlan C, Malpassuti VC, Lucatelli P, et al. HCC in the Era of Direct-Acting Antiviral Agents (DAAs): Surgical and Other Curative or Palliative Strategies in the Elderly. Cancers. 2021; 13(12):3025. https://doi.org/10.3390/cancers13123025
Chicago/Turabian StyleBrozzetti, Stefania, Marsia Tancredi, Simone Bini, Chiara De Lucia, Jessica Antimi, Chiara D’Alterio, Giuseppe Maria De Sanctis, Caterina Furlan, Vittoria Carolina Malpassuti, Pierleone Lucatelli, and et al. 2021. "HCC in the Era of Direct-Acting Antiviral Agents (DAAs): Surgical and Other Curative or Palliative Strategies in the Elderly" Cancers 13, no. 12: 3025. https://doi.org/10.3390/cancers13123025
APA StyleBrozzetti, S., Tancredi, M., Bini, S., De Lucia, C., Antimi, J., D’Alterio, C., De Sanctis, G. M., Furlan, C., Malpassuti, V. C., Lucatelli, P., Di Martino, M., Bezzi, M., Ciardi, A., & Pascale, R. M. (2021). HCC in the Era of Direct-Acting Antiviral Agents (DAAs): Surgical and Other Curative or Palliative Strategies in the Elderly. Cancers, 13(12), 3025. https://doi.org/10.3390/cancers13123025







