Magnetically Guided Localization Using a Guiding-Marker System® and a Handheld Magnetic Probe for Nonpalpable Breast Lesions: A Multicenter Feasibility Study in Japan
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
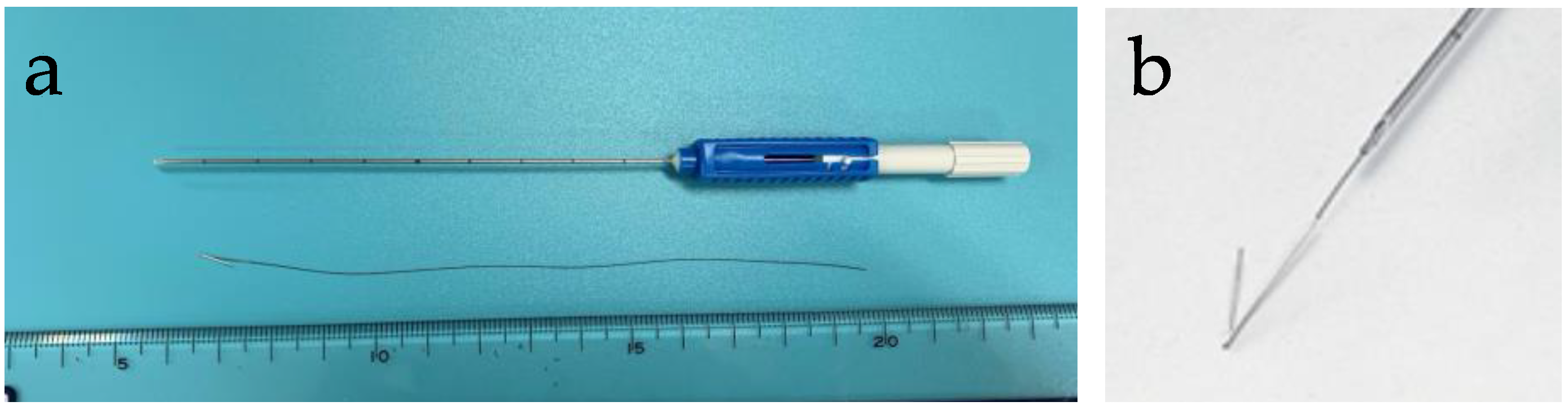
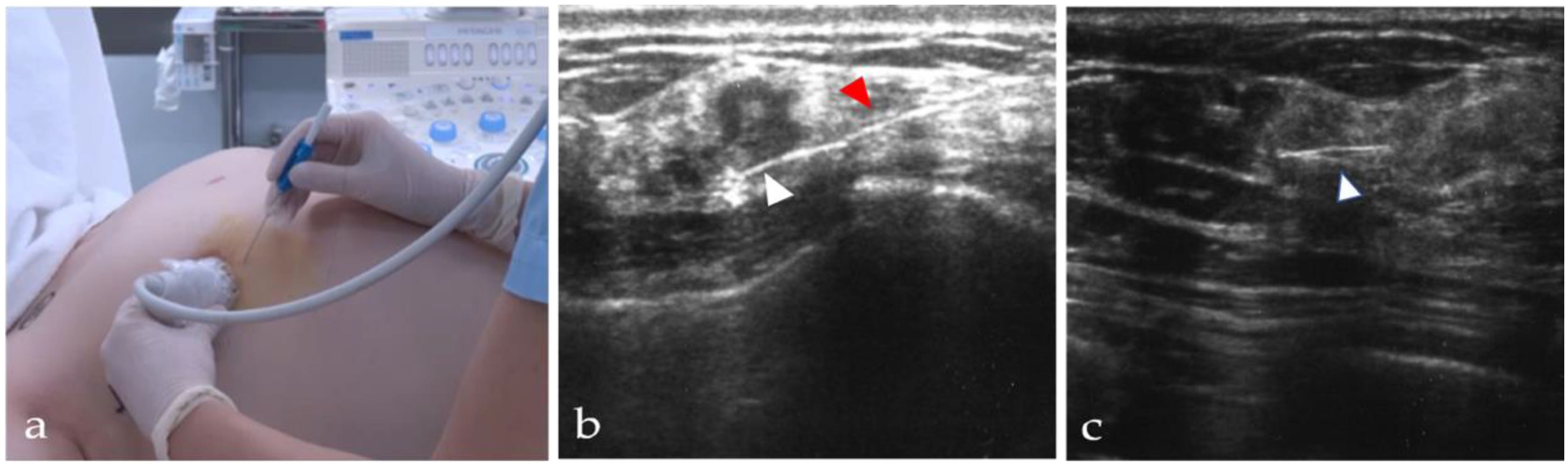
2.2. Materials
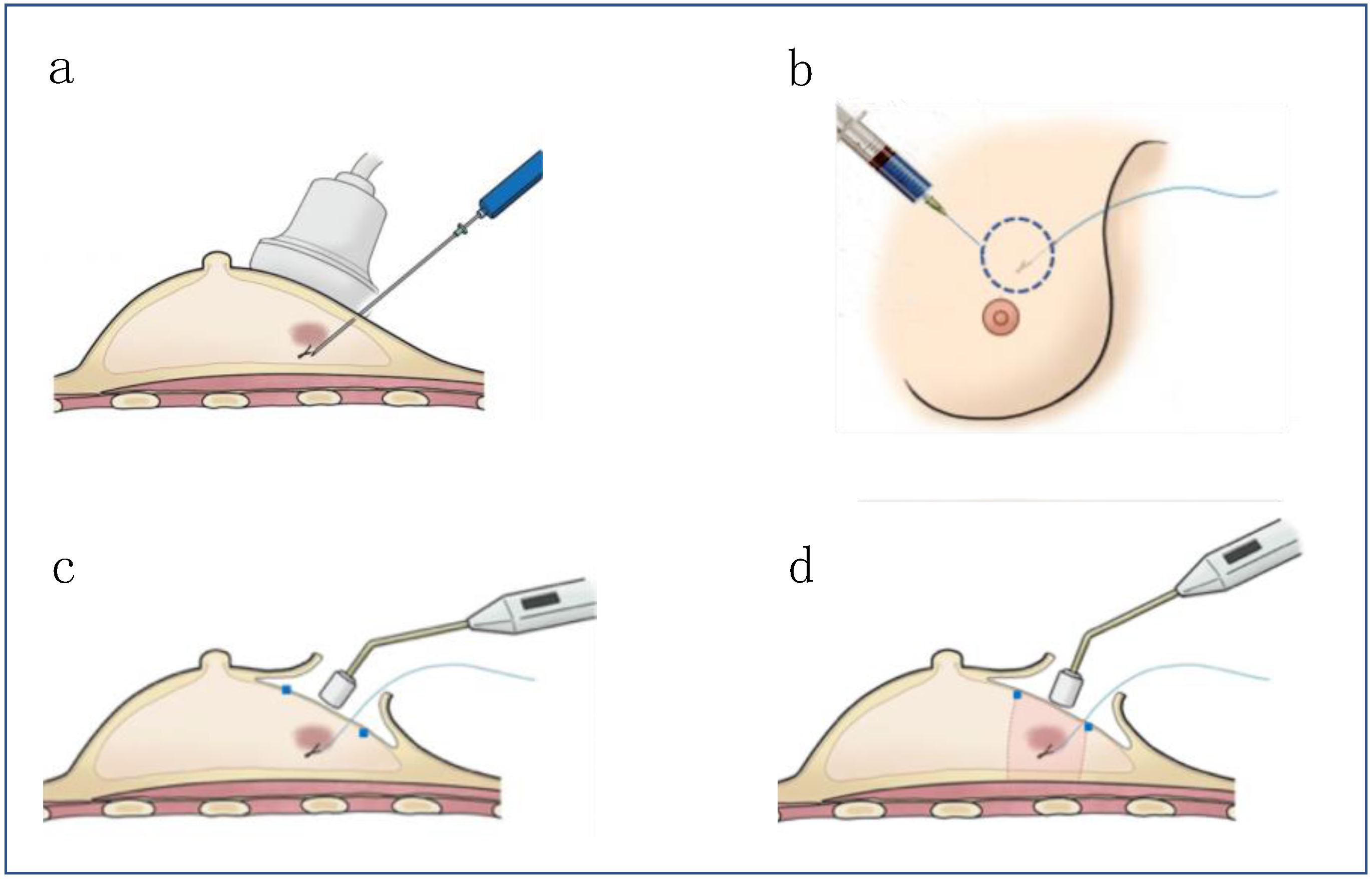
2.3. Surgical Procedures
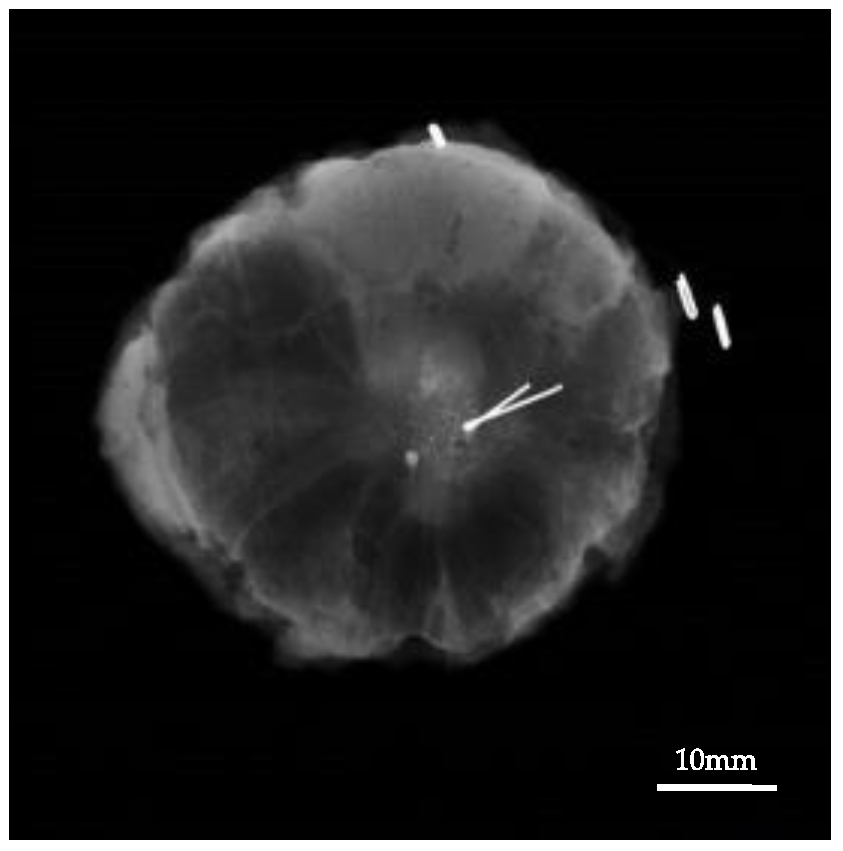
2.4. Pathological Examination
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sharek, D.; Zuley, M.L.; Zhang, J.Y.; Soran, A.; Ahrendt, G.M.; Ganott, M.A. Radioactive Seed Localization Versus Wire Localization for Lumpectomies: A Comparison of Outcomes. Am. J. Roentgenol. 2015, 204, 872–877. [Google Scholar] [CrossRef]
- Lynge, E.; Ponti, A.; James, T.; Májek, O.; von Euler-Chelpin, M.; Anttila, A.; Fitzpatrick, P.; Frigerio, A.; Kawai, M.; Scharpantgen, A.; et al. Variation in detection of ductal carcinoma in situ during screening mammography: A survey within the International Cancer Screening Network. Eur. J. Cancer 2014, 50, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Morrow, M.; Khan, A.J. Locoregional Management After Neoadjuvant Chemotherapy. J. Clin. Oncol. 2020, 38, 2281–2289. [Google Scholar] [CrossRef] [PubMed]
- Benson, J.R.; Jatoi, I.; Keisch, M.; Esteva, F.J.; Makris, A.; Jordan, V.C. Early breast cancer. Lancet 2009, 373, 1463–1479. [Google Scholar] [CrossRef]
- Hong, N.L.; Wright, F.C.; Semple, M.; Nicolae, A.M.; Ravi, A. Results of a phase I, non-randomized study evaluating a Magnetic Occult Lesion Localization Instrument (MOLLI) for excision of non-palpable breast lesions. Breast Cancer Res. Treat. 2019, 179, 671–676. [Google Scholar] [CrossRef]
- Cox, C.E.; Garcia-Henriquez, N.; Glancy, M.J.; Whitworth, P.; Cox, J.M.; Themar-Geck, M.; Prati, R.; Jung, M.; Russell, S.; Appleton, K.; et al. Pilot Study of a New Nonradioactive Surgical Guidance Technology for Locating Nonpalpable Breast Lesions. Ann. Surg. Oncol. 2016, 23, 1824–1830. [Google Scholar] [CrossRef] [PubMed]
- Aydogan, T.; Sezgin, E.; Ilvan, S.; Yilmaz, O.C.; Aslan, N.; Golshan, M.; Aydogan, F. Comparison of Radio-guided Occult Lesion Localization (ROLL) and Magnetic Occult Lesion Localization (MOLL) for Non-palpable Lesions: A Phantom Model Study. Clin. Breast Cancer 2020, 20, e9–e13. [Google Scholar] [CrossRef]
- Hall, F.M.; Frank, H.A. Preoperative localization of nonpalpable breast lesions. AJR Am. J. Roentgenol. 1979, 132, 101–105. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ahmed, M.; Anninga, B.; Goyal, S.; Young, P.; Pankhurst, Q.A.; Douek, M.; on behalf of the MagSNOLL Trialists Group. Magnetic sentinel node and occult lesion localization in breast cancer (MagSNOLL Trial). BJS 2015, 102, 646–652. [Google Scholar] [CrossRef]
- Harvey, J.R.; Lim, Y.; Murphy, J.; Howe, M.; Morris, J.; Goyal, A.; Maxwell, A.J. Safety and feasibility of breast lesion localization using magnetic seeds (Magseed): A multi-centre, open-label cohort study. Breast Cancer Res. Treat. 2018, 169, 531–536. [Google Scholar] [CrossRef]
- Price, E.R.; Khoury, A.L.; Esserman, L.J.; Joe, B.N.; Alvarado, M.D. Initial Clinical Experience with an Inducible Magnetic Seed System for Preoperative Breast Lesion Localization. Am. J. Roentgenol. 2018, 210, 913–917. [Google Scholar] [CrossRef] [PubMed]
- Zacharioudakis, K.; Down, S.; Bholah, Z.; Lee, S.; Khan, T.; Maxwell, A.J.; Howe, M.; Harvey, J. Is the future magnetic? Magseed localisation for non palpable breast cancer. A multi-centre non randomised control study. Eur. J. Surg. Oncol. 2019, 45, 2016–2021. [Google Scholar] [CrossRef] [PubMed]
- Pieszko, K.; Wichtowski, M.; Cieciorowski, M.; Jamont, R.; Murawa, D. Evaluation of the nonradioactive inducible magnetic seed system Magseed for preoperative localization of nonpalpable breast lesions—Initial clinical experience. Contem. Oncol. 2020, 24, 51–54. [Google Scholar] [CrossRef] [PubMed]
- Sekino, M.; Kuwahata, A.; Ookubo, T.; Shiozawa, M.; Ohashi, K.; Kaneko, M.; Saito, I.; Inoue, Y.; Ohsaki, H.; Takei, H.; et al. Handheld magnetic probe with permanent magnet and Hall sensor for identifying sentinel lymph nodes in breast cancer patients. Sci. Rep. 2018, 8, 11–95. [Google Scholar] [CrossRef] [PubMed]
- Taruno, K.; Kurita, T.; Kuwahata, A.; Yanagihara, K.; Enokido, K.; Katayose, Y.; Nakamura, S.; Takei, H.; Sekino, M.; Kusakabe, M. Multicenter clinical trial on sentinel lymph node biopsy using superparamagnetic iron oxide nanoparticles and a novel handheld magnetic probe. J. Surg. Oncol. 2019, 120, 1391–1396. [Google Scholar] [CrossRef]
- Zada, A.; Peek, M.C.L.; Ahmed, M.; Anninga, B.; Baker, R.; Kusakabe, M.; Sekino, M.; Klaase, J.M.; Haken, B.T.; Douek, M. Meta-analysis of sentinel lymph node biopsy in breast cancer using the magnetic technique. BJS 2016, 103, 1409–1419. [Google Scholar] [CrossRef]
- Douek, M.; Klaase, J.; Monypenny, I.; Kothari, A.; Zechmeister, K.; Brown, D.; Wyld, L.; Drew, P.; Garmo, H.; Agbaje, O.; et al. Sentinel node biopsy using a magnetic tracer versus standard technique: The SentiMAG multicentre trial. Ann. Surg. Oncol. 2013, 21, 1237–1245. [Google Scholar] [CrossRef]
- Kanazawa, S.; Ando, A.; Yasui, K.; Mitani, M.; Hiraki, Y.; Shimizu, N.; Hamanaka, D.; Kojima, K. Localization of pulmonary nodules for thoracoscopic resection: Experience with a system using a short hookwire and suture. Am. J. Roentgenol. 1998, 170, 332–334. [Google Scholar] [CrossRef][Green Version]
- Miyoshi, K.; Toyooka, S.; Gobara, H.; Oto, T.; Mimura, H.; Sano, Y.; Kanazawa, S.; Date, H. Clinical outcomes of short hook wire and suture marking system in thoracoscopic resection for pulmonary nodules. Eur. J. Cardio Thorac. Surg. 2009, 36, 378–382. [Google Scholar] [CrossRef]
- Nakamura, S. Image-guided breast conserving surgery based on 3D-MRI. Nihon Geka Gakkai Zasshi 2002, 103, 794–798. [Google Scholar]
- Moran, M.S.; Schnitt, S.J.; Giuliano, A.E.; Harris, J.R.; Khan, S.A.; Horton, J.; Klimberg, S.; Chavez-MacGregor, M.; Freedman, G.; Houssami, N.; et al. Society of Surgical Oncology–American Society for Radiation Oncology Consensus Guideline on Margins for Breast-Conserving Surgery With Whole-Breast Irradiation in Stages I and II Invasive Breast Cancer. Ann. Surg. Oncol. 2014, 21, 704–716. [Google Scholar] [CrossRef]
- Morrow, M.; Van Zee, K.J.; Solin, L.J.; Houssami, N.; Chavez-MacGregor, M.; Harris, J.R.; Horton, J.; Hwang, S.; Johnson, P.L.; Marinovich, M.L.; et al. Society of Surgical Oncology–American Society for Radiation Oncology–American Society of Clinical Oncology Consensus Guideline on Margins for Breast-Conserving Surgery With Whole-Breast Irradiation in Ductal Carcinoma In Situ. J. Clin. Oncol. 2016, 34, 4040–4046. [Google Scholar] [CrossRef]
- Gera, R.; Tayeh, S.; Al-Reefy, S.; Mokbel, K. Evolving Role of Magseed in Wireless Localization of Breast Lesions: Systematic Review and Pooled Analysis of 1,559 Procedures. Anticancer. Res. 2020, 40, 1809–1815. [Google Scholar] [CrossRef] [PubMed]
- Micha, A.E.; Sinnett, V.; Downey, K.; Allen, S.; Bishop, B.; Hector, L.R.; Patrick, E.P.; Edmonds, R.; Barry, P.A.; Krupa, K.D.C.; et al. Patient and clinician satisfaction and clinical outcomes of Magseed compared with wire-guided localisation for impalpable breast lesions. Breast Cancer 2021, 28, 196–205. [Google Scholar] [CrossRef] [PubMed]
- Schermers, B.; van der Hage, J.; Loo, C.; Peeters, M.V.; Winter-Warnars, H.; van Duijnhoven, F.; Haken, B.T.; Muller, S.; Ruers, T.J.M. Feasibility of magnetic marker localisation for non-palpable breast cancer. Breast 2017, 33, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Noguchi, M.; Yokoi-Noguchi, M.; Ohno, Y.; Morioka, E.; Nakano, Y.; Kosaka, T.; Kurita, T. Oncoplastic breast conserving surgery: Volume replacement vs. volume displacement. Eur. J. Surg. Oncol. 2016, 42, 926–934. [Google Scholar] [CrossRef] [PubMed]
- Besic, N.; Zgajnar, J.; Hocevar, M.; Rener, M.; Frkovic-Grazio, S.; Snoj, N.; Lindtner, J. Breast biopsy with wire localization: Factors influencing complete excision of nonpalpable carcinoma. Eur. Radiol. 2002, 12, 2684–2689. [Google Scholar] [CrossRef]
- van der Noordaa, M.; Pengel, K.; Groen, E.; van Werkhoven, E.; Rutgers, E.; Loo, C.; Vogel, W.; Peeters, M.V. The use of radioactive iodine-125 seed localization in patients with non-palpable breast cancer: A comparison with the radioguided occult lesion localization with 99m technetium. Eur. J. Surg. Oncol. 2015, 41, 553–558. [Google Scholar] [CrossRef]
- Gerrard, A.D.; Shrotri, A. Surgeon-led Intraoperative Ultrasound Localization for Nonpalpable Breast Cancers: Results of 5 Years of Practice. Clin. Breast Cancer 2019, 19, e748–e752. [Google Scholar] [CrossRef]
- Nicolae, A.; Dillon, J.; Semple, M.; Hong, N.L.; Ravi, A. Evaluation of a Ferromagnetic Marker Technology for Intraoperative Localization of Nonpalpable Breast Lesions. Am. J. Roentgenol. 2019, 212, 727–733. [Google Scholar] [CrossRef]

| Gen.1 | Gen.2 | Total | |
|---|---|---|---|
| No. of patients | n = 39 | n = 48 | n = 87 |
| Ages, y/o (mean) | 40–76 (54.4) | 33–88 (54.4) | 33–88 (54.4) |
| Menopausal status (Pre/Post/unknown) | 14/25/0 | 22/23/3 | 36/48/3 |
| Tumor status | |||
| Tumor/low echoic lesion | 34 (87.2%) | 37 (77.1%) | 71 (81.6%) |
| Microcalcification | 5 (12.8%) | 11(22.9%) | 16 (18.4%) |
| The size of the lesion | |||
| Clinical tumor size, exclude microcalcification, mm (mean) | 0–23 (10.2) | 5–30 (11.8) | 0–33 (11.1) |
| Pathological size of lesion, mm (mean) | 0–60 (18.4) | 0–40 (14.6) | 0–60 (16.8) |
| Histological type of lesion | |||
| Carcinoma in situ | 6/39 (15.4%) | 17/48 (35.4%) | 23/87 (26.4%) |
| IDC | 31/39 (79.5%) | 27/48 | 58/87 (66.6%) |
| ILC | 0/39 (0%) | 3/48 (6.3%) | 3/87 (3.5%) |
| Other invasive carcinoma | 2/39 (5.1%) | 1/48 (2.1%) | 3/87 (3.5%) |
| Histological subtype of breast cancer | |||
| Luminal A | 29/39 (74.4%) | 41/48 (85.4%) | 70/87 (80.5%) |
| Luminal B | 3/39 (7.7%) | 4/48 (8.3%) | 7/87 (8.0%) |
| HER2 enriched | 3/39 (7.7%) | 2/48(4.2%) | 5/87 (5.7%) |
| Triple negative | 4/39 (10.2%) | 1/48 (2.1%) | 5/87(5.7%) |
| Neoadjuvant chemotherapy | 6/39 (15.4%) | 3/48 (6.3%) | 9/87 (10.3%) |
| Pathological complete response | 3/39 (7.7%) | 0/48 (0%) | 3/87 (3.5%) |
| Gen.1 | Gen.2 | Total | ||
|---|---|---|---|---|
| Surgery | Partial mastectomy | 37/39 (94.9%) | 43/45 (93.8%) | 82/87 (94.3%) |
| Tumor excision | 2/39 (5.1%) | 3/45 (6.2%) | 5/87 (5.7%) | |
| Specimen weight, g (mean) | 2–131 (38.7) | 5–184 (41.9) | 2–184 (39.9) | |
| Detectable rate of the Guiding-Marker System® | Transcutaneous | 38/39 (97.4%) | 47/48 (97.9%) | 85/87 (97.7%) |
| Intramammary | 39/39 (100%) | 48/48 (100%) | 87/87 (100%) | |
| Removal rate of the marker in the specimen | 39/39 (100%) | 48/48 (100%) | 87/87 (100%) | |
| Histological examination of surgical margin | Intraoperative frozen section | 7 /37 (18.9%) | 9/45 (20.0%) | 16 /82 (19.5%) |
| Postoperative permanent section | 30/37 (82.1%) | 36/45 (80.0%) | 66/82 (80.4%) | |
| Positive margin status on initial resection | Intraoperative re-excision | 3/37 (8.1%) | 2 /45(4.4%) | 5/82 (6.1%) |
| Re-excision on second operation | 1/37 (2.7%) | 0 /45(0%) | 1/82 (1.2%) | |
| Radiation | Whole breast radiation | 39/39 (100%) | 48/48 (100%) | 87/87 (100%) |
| Boost radiation | 1/37 (2.7%) | 5/45 (11.1%) | 6/82 (7.5%) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kurita, T.; Taruno, K.; Nakamura, S.; Takei, H.; Enokido, K.; Kuwayama, T.; Kanada, Y.; Akashi-Tanaka, S.; Matsuyanagi, M.; Hankyo, M.; et al. Magnetically Guided Localization Using a Guiding-Marker System® and a Handheld Magnetic Probe for Nonpalpable Breast Lesions: A Multicenter Feasibility Study in Japan. Cancers 2021, 13, 2923. https://doi.org/10.3390/cancers13122923
Kurita T, Taruno K, Nakamura S, Takei H, Enokido K, Kuwayama T, Kanada Y, Akashi-Tanaka S, Matsuyanagi M, Hankyo M, et al. Magnetically Guided Localization Using a Guiding-Marker System® and a Handheld Magnetic Probe for Nonpalpable Breast Lesions: A Multicenter Feasibility Study in Japan. Cancers. 2021; 13(12):2923. https://doi.org/10.3390/cancers13122923
Chicago/Turabian StyleKurita, Tomoko, Kanae Taruno, Seigo Nakamura, Hiroyuki Takei, Katsutoshi Enokido, Takashi Kuwayama, Yoko Kanada, Sadako Akashi-Tanaka, Misaki Matsuyanagi, Meishi Hankyo, and et al. 2021. "Magnetically Guided Localization Using a Guiding-Marker System® and a Handheld Magnetic Probe for Nonpalpable Breast Lesions: A Multicenter Feasibility Study in Japan" Cancers 13, no. 12: 2923. https://doi.org/10.3390/cancers13122923
APA StyleKurita, T., Taruno, K., Nakamura, S., Takei, H., Enokido, K., Kuwayama, T., Kanada, Y., Akashi-Tanaka, S., Matsuyanagi, M., Hankyo, M., Yanagihara, K., Sakatani, T., Sakamaki, K., Kuwahata, A., Sekino, M., & Kusakabe, M. (2021). Magnetically Guided Localization Using a Guiding-Marker System® and a Handheld Magnetic Probe for Nonpalpable Breast Lesions: A Multicenter Feasibility Study in Japan. Cancers, 13(12), 2923. https://doi.org/10.3390/cancers13122923










