Changes in Overall Survival over Time for Patients with de novo Metastatic Breast Cancer
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
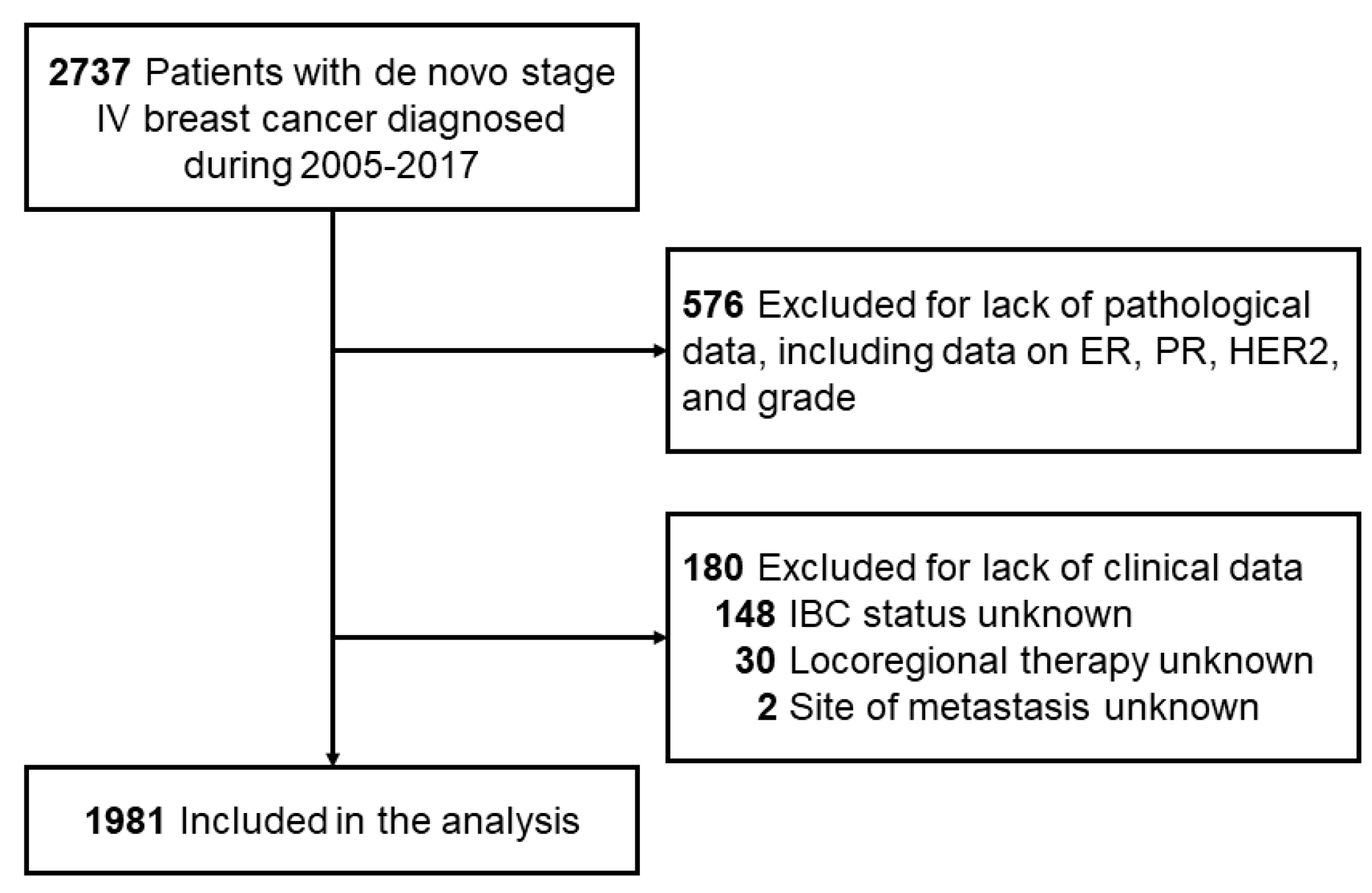
2.1. Inclusion Criteria
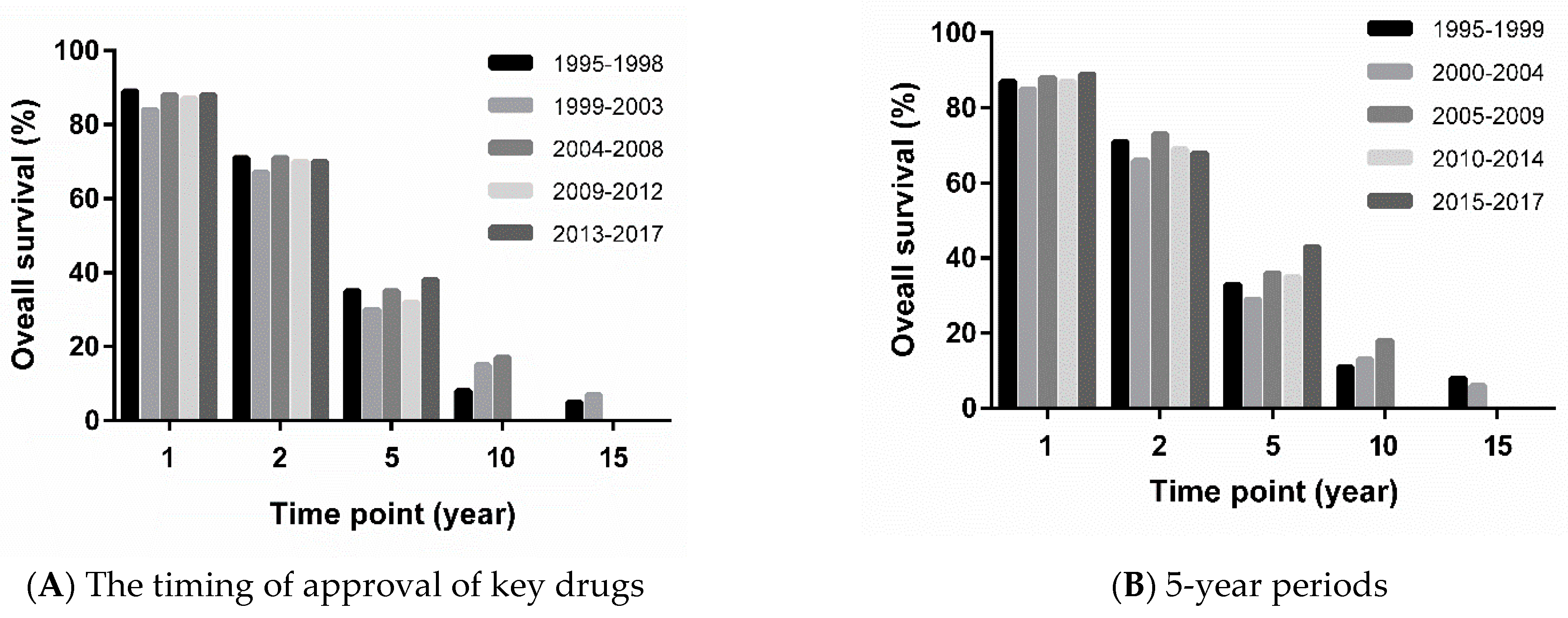
2.2. Definition of Time Periods
2.3. Definitions of Clinical and Pathological Variables
2.4. Statistical Considerations
3. Results
3.1. Patient Characteristics
3.2. OS by Disease and Treatment Characteristics
3.3. Prognostic Factors for OS
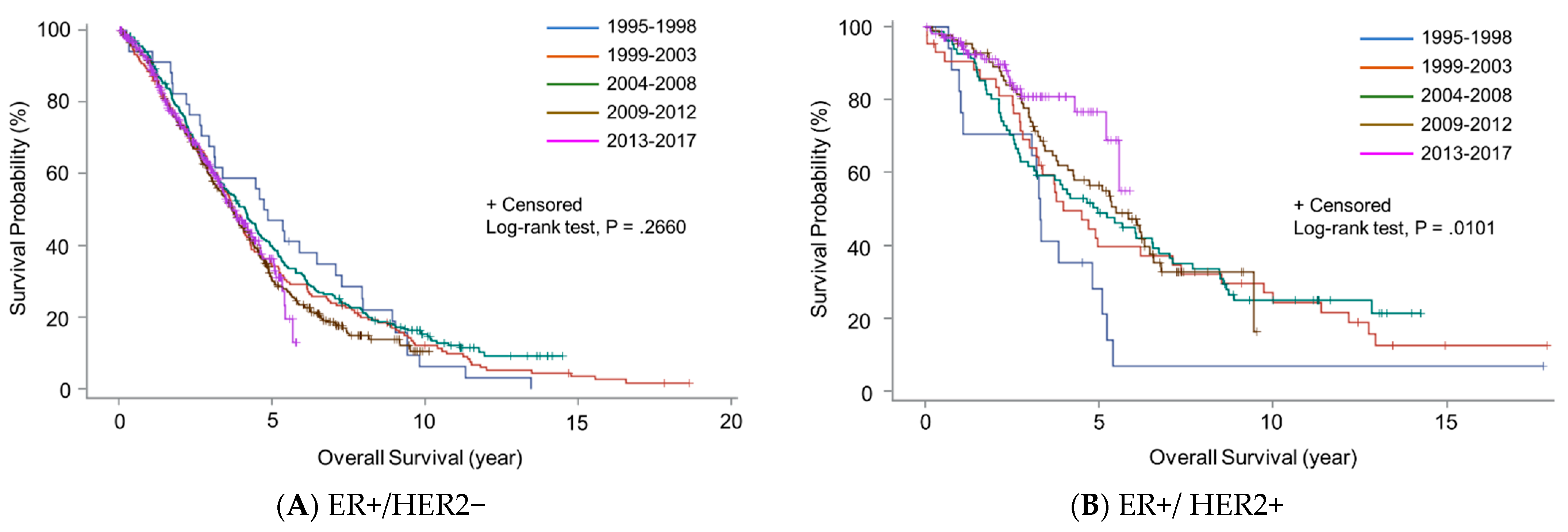
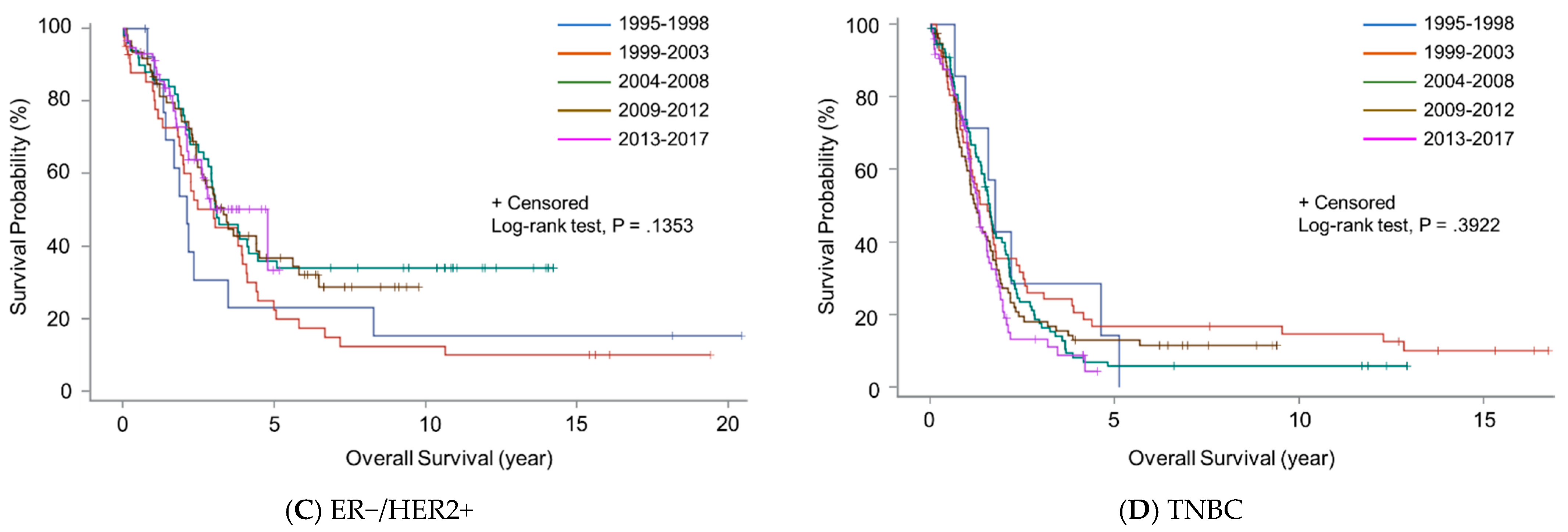
3.4. Changes in OS over Time
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Howlader, N.; Krapcho, M. SEER Cancer Statistics Review, 1975–2012. Available online: http://seer.cancer.gov/csr/1975_2012/ (accessed on 1 November 2020).
- Tripathy, D.; Brufsky, A.; Cobleigh, M.; Jahanzeb, M.; Kaufman, P.A.; Mason, G.; O’Shaughnessy, J.; Rugo, H.S.; Swain, S.M.; Yardley, D.A.; et al. De Novo Versus Recurrent HER2-Positive Metastatic Breast Cancer: Patient Characteristics, Treatment, and Survival from the SystHERs Registry. Oncologist 2020, 25, e214–e222. [Google Scholar] [CrossRef] [PubMed]
- Dawood, S.; Broglio, K.; Ensor, J.; Hortobagyi, G.N.; Giordano, S.H. Survival differences among women with de novo stage IV and relapsed breast cancer. Ann. Oncol. 2010, 21, 2169–2174. [Google Scholar] [CrossRef] [PubMed]
- Balduzzi, S.; Mantarro, S.; Guarneri, V.; Tagliabue, L.; Pistotti, V.; Moja, L.; D’Amico, R. Trastuzumab-containing regimens for metastatic breast cancer. Cochrane Database Syst. Rev. 2014, 2014, Cd006242. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Angulo, A.M.; Timms, K.M.; Liu, S.; Chen, H.; Litton, J.K.; Potter, J.; Lanchbury, J.S.; Stemke-Hale, K.; Hennessy, B.T.; Arun, B.K.; et al. Incidence and outcome of BRCA mutations in unselected patients with triple receptor-negative breast cancer. Clin. Cancer Res. 2011, 17, 1082–1089. [Google Scholar] [CrossRef]
- Hartman, A.R.; Kaldate, R.R.; Sailer, L.M.; Painter, L.; Grier, C.E.; Endsley, R.R.; Griffin, M.; Hamilton, S.A.; Frye, C.A.; Silberman, M.A.; et al. Prevalence of BRCA mutations in an unselected population of triple-negative breast cancer. Cancer 2012, 118, 2787–2795. [Google Scholar] [CrossRef]
- Wong-Brown, M.W.; Meldrum, C.J.; Carpenter, J.E.; Clarke, C.L.; Narod, S.A.; Jakubowska, A.; Rudnicka, H.; Lubinski, J.; Scott, R.J. Prevalence of BRCA1 and BRCA2 germline mutations in patients with triple-negative breast cancer. Breast Cancer Res. Treat. 2015, 150, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Malmgren, J.A.; Mayer, M.; Atwood, M.K.; Kaplan, H.G. Differential presentation and survival of de novo and recurrent metastatic breast cancer over time: 1990–2010. Breast Cancer Res. Treat. 2018, 167, 579–590. [Google Scholar] [CrossRef] [PubMed]
- Schmid, P.; Adams, S.; Rugo, H.S.; Schneeweiss, A.; Barrios, C.H.; Iwata, H.; Diéras, V.; Hegg, R.; Im, S.-A.; Wright, G.S.; et al. Atezolizumab and Nab-Paclitaxel in Advanced Triple-Negative Breast Cancer. N. Engl. J. Med. 2018, 379, 2108–2121. [Google Scholar] [CrossRef] [PubMed]
- Swain, S.M.; Baselga, J.; Kim, S.-B.; Ro, J.; Semiglazov, V.; Campone, M.; Ciruelos, E.; Ferrero, J.-M.; Schneeweiss, A.; Heeson, S.; et al. Pertuzumab, Trastuzumab, and Docetaxel in HER2-Positive Metastatic Breast Cancer. N. Engl. J. Med. 2015, 372, 724–734. [Google Scholar] [CrossRef] [PubMed]
- Robertson, J.F.R.; Bondarenko, I.M.; Trishkina, E.; Dvorkin, M.; Panasci, L.; Manikhas, A.; Shparyk, Y.; Cardona-Huerta, S.; Cheung, K.-L.; Philco-Salas, M.J.; et al. Fulvestrant 500 mg versus anastrozole 1 mg for hormone receptor-positive advanced breast cancer (FALCON): An international, randomised, double-blind, phase 3 trial. Lancet 2016, 388, 2997–3005. [Google Scholar] [CrossRef]
- Hortobagyi, G.N.; Stemmer, S.M.; Burris, H.A.; Yap, Y.S.; Sonke, G.S.; Paluch-Shimon, S.; Campone, M.; Petrakova, K.; Blackwell, K.L.; Winer, E.P.; et al. Updated results from MONALEESA-2, a phase III trial of first-line ribociclib plus letrozole versus placebo plus letrozole in hormone receptor-positive, HER2-negative advanced breast cancer. Ann. Oncol. 2018, 29, 1541–1547. [Google Scholar] [CrossRef] [PubMed]
- Im, S.-A.; Lu, Y.-S.; Bardia, A.; Harbeck, N.; Colleoni, M.; Franke, F.; Chow, L.; Sohn, J.; Lee, K.-S.; Campos-Gomez, S.; et al. Overall Survival with Ribociclib plus Endocrine Therapy in Breast Cancer. N. Engl. J. Med. 2019, 381, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Zeichner, S.B.; Herna, S.; Mani, A.; Ambros, T.; Montero, A.J.; Mahtani, R.L.; Ahn, E.R.; Vogel, C.L. Survival of patients with de-novo metastatic breast cancer: Analysis of data from a large breast cancer-specific private practice, a university-based cancer center and review of the literature. Breast Cancer Res. Treat. 2015, 153, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Lane, W.O.; Thomas, S.M.; Blitzblau, R.C.; Plichta, J.K.; Rosenberger, L.H.; Fayanju, O.M.; Hyslop, T.; Hwang, E.S.; Greenup, R.A. Surgical Resection of the Primary Tumor in Women With De Novo Stage IV Breast Cancer: Contemporary Practice Patterns and Survival Analysis. Ann. Surg. 2019, 269, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Badwe, R.; Hawaldar, R.; Nair, N.; Kaushik, R.; Parmar, V.; Siddique, S.; Budrukkar, A.; Mittra, I.; Gupta, S. Locoregional treatment versus no treatment of the primary tumour in metastatic breast cancer: An open-label randomised controlled trial. Lancet Oncol. 2015, 16, 1380–1388. [Google Scholar] [CrossRef]
- Soran, A.; Ozmen, V.; Ozbas, S.; Karanlik, H.; Muslumanoglu, M.; Igci, A.; Canturk, Z.; Utkan, Z.; Ozaslan, C.; Evrensel, T.; et al. Randomized Trial Comparing Resection of Primary Tumor with No Surgery in Stage IV Breast Cancer at Presentation: Protocol MF07-01. Ann. Surg. Oncol. 2018, 25, 3141–3149. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.A.; Zhao, F.; Solin, L.J.; Goldstein, L.J.; Cella, D.; Basik, M.; Golshan, M.; Julian, T.B.; Pockaj, B.A.; Lee, C.A.; et al. A randomized phase III trial of systemic therapy plus early local therapy versus systemic therapy alone in women with de novo stage IV breast cancer: A trial of the ECOG-ACRIN Research Group (E2108). J. Clin. Oncol. 2020, 38, LBA2. [Google Scholar] [CrossRef]
- Shien, T.; Mizutani, T.; Tanaka, K.; Kinoshita, T.; Hara, F.; Fujisawa, T.; Masuda, N.; Tamura, K.; Hojo, T.; Kanbayashi, C.; et al. A randomized controlled trial comparing primary tumor resection plus systemic therapy with systemic therapy alone in metastatic breast cancer (JCOG1017 PRIM-BC). J. Clin. Oncol. 2017, 35, TPS588. [Google Scholar] [CrossRef]
| Characteristic | Number of Patients (%) | |
|---|---|---|
| Year of diagnosis, grouping 1 (based on the date of approval of key agents) | 1995–1998 | 72 (4) |
| 1999–2003 | 305 (15) | |
| 2004–2008 | 469 (24) | |
| 2009–2012 | 564 (29) | |
| 2013–2017 | 571 (29) | |
| Year of diagnosis, grouping 2 | 1995–1999 | 100 (5) |
| (5-year periods) | 2000–2004 | 353 (18) |
| 2005–2009 | 517 (26) | |
| 2010–2014 | 676 (34) | |
| 2015–2017 | 335 (17) | |
| Age at diagnosis, median (range), year | 52 (22–93) | |
| ER status | Positive | 1398 (71) |
| Negative | 580 (29) | |
| Unknown | 3 | |
| PR status | Positive | 1051 (53) |
| Negative | 920 (47) | |
| Unknown | 10 | |
| HER2 status | Positive | 555 (28) |
| Negative | 1426 (72) | |
| Subtype | ER+/HER2+ | 330 (17) |
| ER+/HER2− | 1120 (57) | |
| ER−/HER2+ | 225 (11) | |
| TNBC | 306 (15) | |
| Nuclear grade | 1 | 96 (5) |
| 2 | 754 (38) | |
| 3 | 1131 (57) | |
| IBC | Yes | 339 (17) |
| No | 1642 (83) | |
| Locoregional therapy | Yes | 775 (39) |
| No | 1206 (61) | |
| Metastasis to a single organ | Yes | 1227 (62) |
| No | 754 (38) |
| Variables | HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
|---|---|---|---|---|---|
| Year of diagnosis, grouping 1 | 1995–1998 vs. 2013–2017 | 1.12 (0.85–1.48) | 0.4117 | ||
| 1999–2003 vs. 2013–2017 | 1.11 (0.92–1.32) | 0.2683 | |||
| 2004–2008 vs. 2013–2017 | 1 (0.85–1.18) | 0.9985 | |||
| 2009–2012 vs. 2013–2017 | 1.07 0(.91–1.26) | 0.3952 | |||
| Year of diagnosis, grouping 2 | 1995–1999 vs. 2000–2004 | 0.91 (0.72–1.15) | 0.4188 | ||
| 2005–2009 vs. 2000–2004 | 0.8 (0.69–0.93) | 0.0029 | |||
| 2010–2014 vs. 2000–2004 | 0.91 (0.78–1.05) | 0.1857 | |||
| 2015–2017 vs. 2000–2004 | 0.88 (0.7–1.1) | 0.2541 | |||
| Age at diagnosis | 1.008 (1.004–1.013) | 0.0002 | |||
| ER status | Positive vs. Negative | 0.59 (0.53–0.59) | <0.0001 | ||
| PR status | Positive vs. Negative | 0.64 (0.57-0.64) | <0.0001 | ||
| HER2 status | Positive vs. Negative | 0.64 (0.56–0.64) | <0.0001 | ||
| Subtype | ER+/HER2− vs. ER+/HER2+ | 1.54 (1.31–1.54) | <0.0001 | 1.71 (1.45–2.02) | <0.0001 |
| ER−/HER2+ vs. ER+/HER2+ | 1.41 (1.13–1.41) | <0.0001 | 1.49 (1.2–1.87) | 0.0004 | |
| TNBC vs. ER+/HER2+ | 3.7 (3.05–3.7) | <0.0001 | 3.93 (3.23–4.78) | <0.0001 | |
| Nuclear grade | 2 vs. 1 | 1.07 (0.82–1.07) | 0.0023 | 1.21 (0.92–1.6) | 0.1677 |
| 3 vs. 1 | 1.51 (1.16–1.51) | <0.0001 | 1.74 (1.32–2.29) | <0.0001 | |
| IBC | Yes vs. No | 1.18 (1.03–1.18) | 0.0212 | ||
| Locoregional therapy | Yes vs. No | 0.53 (0.47–0.53) | <0.0001 | 0.5 (0.45–0.56) | <0.0001 |
| Metastasis to a single organ | Yes vs. No | 0.59 (0.53–0.59) | <0.0001 | 0.64 (0.58–0.72) | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iwase, T.; Shrimanker, T.V.; Rodriguez-Bautista, R.; Sahin, O.; James, A.; Wu, J.; Shen, Y.; Ueno, N.T. Changes in Overall Survival over Time for Patients with de novo Metastatic Breast Cancer. Cancers 2021, 13, 2650. https://doi.org/10.3390/cancers13112650
Iwase T, Shrimanker TV, Rodriguez-Bautista R, Sahin O, James A, Wu J, Shen Y, Ueno NT. Changes in Overall Survival over Time for Patients with de novo Metastatic Breast Cancer. Cancers. 2021; 13(11):2650. https://doi.org/10.3390/cancers13112650
Chicago/Turabian StyleIwase, Toshiaki, Tushaar Vishal Shrimanker, Ruben Rodriguez-Bautista, Onur Sahin, Anjali James, Jimin Wu, Yu Shen, and Naoto T. Ueno. 2021. "Changes in Overall Survival over Time for Patients with de novo Metastatic Breast Cancer" Cancers 13, no. 11: 2650. https://doi.org/10.3390/cancers13112650
APA StyleIwase, T., Shrimanker, T. V., Rodriguez-Bautista, R., Sahin, O., James, A., Wu, J., Shen, Y., & Ueno, N. T. (2021). Changes in Overall Survival over Time for Patients with de novo Metastatic Breast Cancer. Cancers, 13(11), 2650. https://doi.org/10.3390/cancers13112650








