Efficacy of BRAF and MEK Inhibition in Patients with BRAF-Mutant Advanced Melanoma and Germline CDKN2A Pathogenic Variants
Abstract
Simple Summary
Abstract
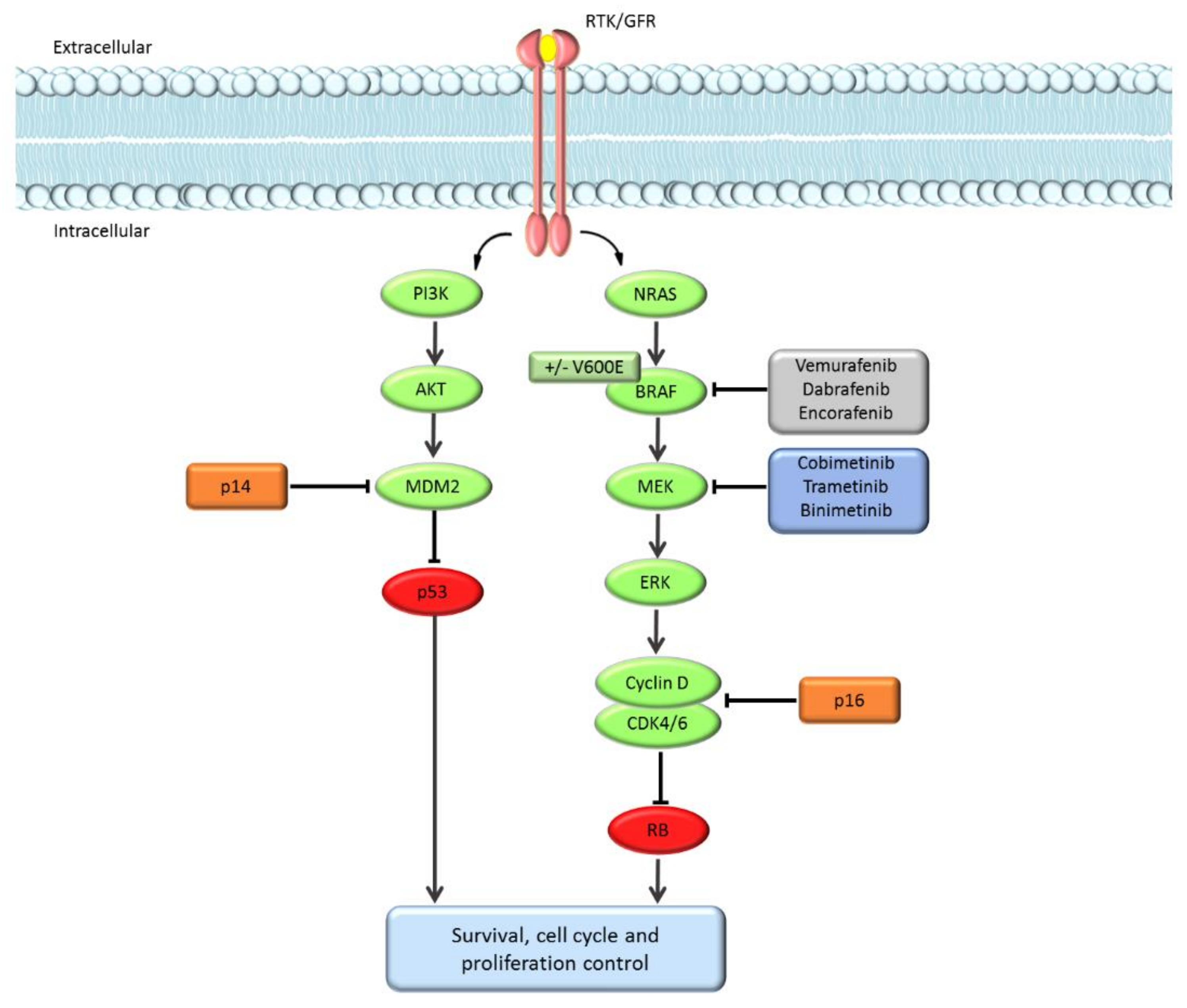
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Goldstein, A.M.; Chan, M.; Harland, M.; Hayward, N.K.; Demenais, F.; Bishop, D.T.; Azizi, E.; Bergman, W.; Bianchi-Scarra, G.; Bruno, W.; et al. Features associated with germline CDKN2A mutations: A GenoMEL study of melanoma-prone families from three continents. J. Med Genet. 2006, 44, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Helgadottir, H.; Höiom, V.; Tuominen, R.; Nielsen, K.; Jönsson, G.; Olsson, H.; Hansson, J. GermlineCDKN2AMutation Status and Survival in Familial Melanoma Cases. J. Natl. Cancer Inst. 2016, 108, djw135. [Google Scholar] [CrossRef] [PubMed]
- Dalmasso, B.; Pastorino, L.; Ciccarese, G.; Andreotti, V.; Grillo, F.; Mastracci, L.; Spagnolo, F.; Ballestrero, A.; Queirolo, P.; Bruno, W.; et al. CDKN2A germline mutations are not associated with poor survival in an Italian cohort of melanoma patients. J. Am. Acad. Dermatol. 2019, 80, 1263–1271. [Google Scholar] [CrossRef] [PubMed]
- Lauss, M.; Donia, M.; Harbst, K.; Andersen, R.; Mitra, S.; Rosengren, F.; Salim, M.; Vallon-Christersson, J.; Törngren, T.; Kvist, A.; et al. Mutational and putative neoantigen load predict clinical benefit of adoptive T cell therapy in melanoma. Nat. Commun. 2017, 8, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Helgadottir, H.; Ghiorzo, P.; van Doorn, R.; Puig, S.; Levin, M.; Kefford, R.; Lauss, M.; Queirolo, P.; Pastorino, L.; Kapiteijn, E.; et al. Efficacy of novel immunotherapy regimens in patients with metastatic melanoma with germline CDKN2A mutations. J. Med. Genet. 2020, 57, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Davies, H.; Bignell, G.R.; Cox, C.; Stephens, P.; Edkins, S.; Clegg, S.; Teague, J.; Woffendin, H.; Garnett, M.J.; Bottomley, W.; et al. Mutations of the BRAF gene in human cancer. Nature 2002, 417, 949–954. [Google Scholar] [CrossRef] [PubMed]
- Tanda, E.T.; Vanni, I.; Boutros, A.; Andreotti, V.; Bruno, W.; Ghiorzo, P.; Spagnolo, F. Current State of Target Treatment in BRAF Mutated Melanoma. Front. Mol. Biosci. 2020, 7, 154. [Google Scholar] [CrossRef] [PubMed]
- Smalley, K.S.; Lioni, M.; Palma, M.D.; Xiao, M.; Desai, B.; Egyhazi, S.; Hansson, J.; Wu, H.; King, A.J.; Van Belle, P.; et al. Increased cyclin D1 expression can mediate BRAF inhibitor resistance in BRAF V600E-mutated melanomas. Mol. Cancer Ther. 2008, 7, 2876–2883. [Google Scholar] [CrossRef] [PubMed]
- Nathanson, K.L.; Martin, A.-M.; Wubbenhorst, B.; Greshock, J.; Letrero, R.; D’Andrea, K.; O’Day, S.; Infante, J.R.; Falchook, G.S.; Arkenau, H.-T.; et al. Tumor genetic analyses of patients with metastatic melanoma treated with the BRAF inhibitor dabrafenib (GSK2118436). Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2013, 19, 4868–4878. [Google Scholar] [CrossRef] [PubMed]
- Flaherty, K.; Davies, M.A.; Grob, J.J.; Long, G.V.; Nathan, P.D.; Ribas, A.; Robert, C.; Schadendorf, D.; Frederick, D.T.; Hammond, M.R.; et al. Genomic analysis and 3-y efficacy and safety update of COMBI-d: A phase 3 study of dabrafenib (D) + trametinib (T) vs D monotherapy in patients (pts) with unresectable or metastatic BRAF V600E/K-mutant cutaneous melanoma. J. Clin. Oncol. 2016, 34, 9502. [Google Scholar] [CrossRef]
- Zebary, A.; Omholt, K.; Van Doorn, R.; Ghiorzo, P.; Harbst, K.; Johansson, C.H.; Höiom, V.; Jönsson, G.; Pjanova, D.; Puig, S.; et al. Somatic BRAF and NRAS Mutations in Familial Melanomas with Known Germline CDKN2A Status: A GenoMEL Study. J. Investig. Dermatol. 2014, 134, 287–290. [Google Scholar] [CrossRef] [PubMed]
- Staaf, J.; Harbst, K.; Lauss, M.; Ringnér, M.; Måsbäck, A.; Howlin, J.; Jirström, K.; Harland, M.; Zebary, A.; Palmer, J.M.; et al. Primary Melanoma Tumors from CDKN2A Mutation Carriers Do Not Belong to a Distinct Molecular Subclass. J. Investig. Dermatol. 2014, 134, 3000–3003. [Google Scholar] [CrossRef] [PubMed]
- Helgadottir, H.; Höiom, V.; Jönsson, G.; Tuominen, R.; Ingvar, C.; Borg, Å.; Olsson, H.; Hansson, J. High risk of tobacco-related cancers in CDKN2A mutation-positive melanoma families. J. Med. Genet. 2014, 51, 545. [Google Scholar] [CrossRef] [PubMed]
- Harland, M.; E Cust, A.; Badenas, C.; Chang, Y.-M.; A Holland, E.; Aguilera, P.; Aitken, J.F.; Armstrong, B.K.; Barrett, J.H.; Carrera, C.; et al. Prevalence and predictors of germline CDKN2A mutations for melanoma cases from Australia, Spain and the United Kingdom. Hered. Cancer Clin. Pr. 2014, 12, 20. [Google Scholar] [CrossRef] [PubMed]
- Potjer, T.P.; Helgadottir, H.; Leenheer, M.; van der Stoep, N.; Gruis, N.A.; Höiom, V.; Olsson, H.; van Doorn, R.; Vasen, H.F.A.; van Asperen, C.J.; et al. CM-Score: A validated scoring system to predict CDKN2A germline mutations in melanoma families from Northern Europe. J. Med. Genet. 2018, 55, 661. [Google Scholar] [CrossRef] [PubMed]
- Puig, S.; Malvehy, J.; Badenas, C.; Ruiz, A.; Jimenez, D.; Cuellar, F.; Azon, A.; Gonzàlez, U.; Castel, T.; Campoy, A.; et al. Role of the CDKN2A Locus in Patients With Multiple Primary Melanomas. J. Clin. Oncol. 2005, 23, 3043–3051. [Google Scholar] [CrossRef] [PubMed]
- Bruno, W.; Ghiorzo, P.; Battistuzzi, L.; Ascierto, P.A.; Barile, M.; Gargiulo, S.; Gensini, F.; Gliori, S.; Guida, M.; Lombardo, M.; et al. Clinical genetic testing for familial melanoma in Italy: A cooperative study. J. Am. Acad. Dermatol. 2009, 61, 775–782. [Google Scholar] [CrossRef] [PubMed]
- Bruno, W.; Pastorino, L.; Ghiorzo, P.; Andreotti, V.; Martinuzzi, C.; Menin, C.; Elefanti, L.; Stagni, C.; Vecchiato, A.; Rodolfo, M.; et al. Multiple primary melanomas (MPMs) and criteria for genetic assessment: MultiMEL, a multicenter study of the Italian Melanoma Intergroup. J. Am. Acad. Dermatol. 2016, 74, 325–332. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria; R Core Team: Vienna, Austria, 2019; Available online: https://www.R-project.org/ (accessed on 10 March 2021).
- Robert, C.; Grob, J.J.; Stroyakovskiy, D.; Karaszewska, B.; Hauschild, A.; Levchenko, E.; Sileni, V.C.; Schachter, J.; Garbe, C.; Bondarenko, I.; et al. Five-Year Outcomes with Dabrafenib plus Trametinib in Metastatic Melanoma. N. Engl. J. Med. 2019, 381, 626–636. [Google Scholar] [CrossRef] [PubMed]
| Patients’ Characteristics | Cohort 1 (BRAFi) n = 7 | Cohort 2 (BRAFi + MEKi) n = 12 | All Patients n = 19 |
|---|---|---|---|
| Gender, n (%) | |||
| Male | 5 (71%) | 5 (42%) | 10 (53%) |
| Female | 2 (29%) | 7 (58%) | 9 (47%) |
| Age, years Median (range) | 54 (29–69) | 58 (34–69) | 57 (29–69) |
| AJCC 8th edition stage, n (%) | |||
| M0 | 0 (0%) | 0 (0%) | 0 (0%) |
| M1a | 0 (0%) | 2 (17%) | 2 (11%) |
| M1b | 1 (14%) | 0 (0%) | 1 (5%) |
| M1c | 4 (57%) | 7 (58%) | 11 (58%) |
| M1d | 2 (29%) | 3 (25%) | 5 (26%) |
| Baseline LDH *, n (%) | |||
| Normal | 0 (0%) | 3 (25%) | 3 (33%) |
| Elevated | 2 (100%) | 4 (75%) | 6 (67%) |
| Unknown | 5 | 5 | 10 |
| Best response, n (%) | |||
| Complete response | 0 (0%) | 0 (0%) | 0 (0%) |
| Partial response | 4 (57%) | 12 (100%) | 16 (84%) |
| Stable disease | 1 (14%) | 0 (0%) | 1 (5%) |
| Progressive disease | 2 (29%) | 0 (0%) | 2 (11%) |
| PFS, median (range) Median PFS (months) | 3.0 (2–30) | 9.5 (3–30) | 6.0 (2–30) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spagnolo, F.; Dalmasso, B.; Tanda, E.; Potrony, M.; Puig, S.; van Doorn, R.; Kapiteijn, E.; Queirolo, P.; Helgadottir, H.; Ghiorzo, P. Efficacy of BRAF and MEK Inhibition in Patients with BRAF-Mutant Advanced Melanoma and Germline CDKN2A Pathogenic Variants. Cancers 2021, 13, 2440. https://doi.org/10.3390/cancers13102440
Spagnolo F, Dalmasso B, Tanda E, Potrony M, Puig S, van Doorn R, Kapiteijn E, Queirolo P, Helgadottir H, Ghiorzo P. Efficacy of BRAF and MEK Inhibition in Patients with BRAF-Mutant Advanced Melanoma and Germline CDKN2A Pathogenic Variants. Cancers. 2021; 13(10):2440. https://doi.org/10.3390/cancers13102440
Chicago/Turabian StyleSpagnolo, Francesco, Bruna Dalmasso, Enrica Tanda, Miriam Potrony, Susana Puig, Remco van Doorn, Ellen Kapiteijn, Paola Queirolo, Hildur Helgadottir, and Paola Ghiorzo. 2021. "Efficacy of BRAF and MEK Inhibition in Patients with BRAF-Mutant Advanced Melanoma and Germline CDKN2A Pathogenic Variants" Cancers 13, no. 10: 2440. https://doi.org/10.3390/cancers13102440
APA StyleSpagnolo, F., Dalmasso, B., Tanda, E., Potrony, M., Puig, S., van Doorn, R., Kapiteijn, E., Queirolo, P., Helgadottir, H., & Ghiorzo, P. (2021). Efficacy of BRAF and MEK Inhibition in Patients with BRAF-Mutant Advanced Melanoma and Germline CDKN2A Pathogenic Variants. Cancers, 13(10), 2440. https://doi.org/10.3390/cancers13102440








