Reflector-Guided Localisation of Non-Palpable Breast Lesions: A Prospective Evaluation of the SAVI SCOUT® System
Abstract
Simple Summary
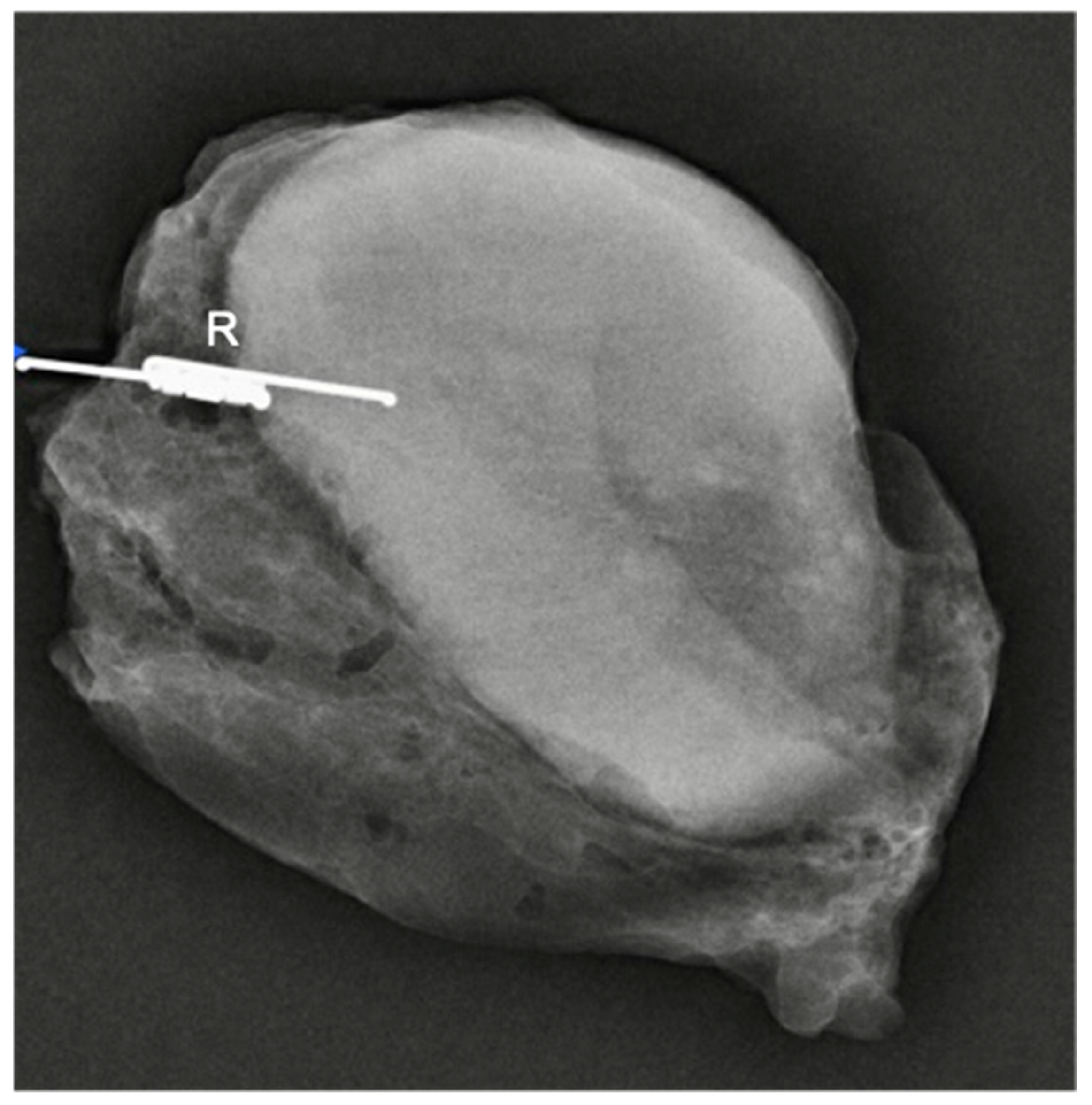
Abstract
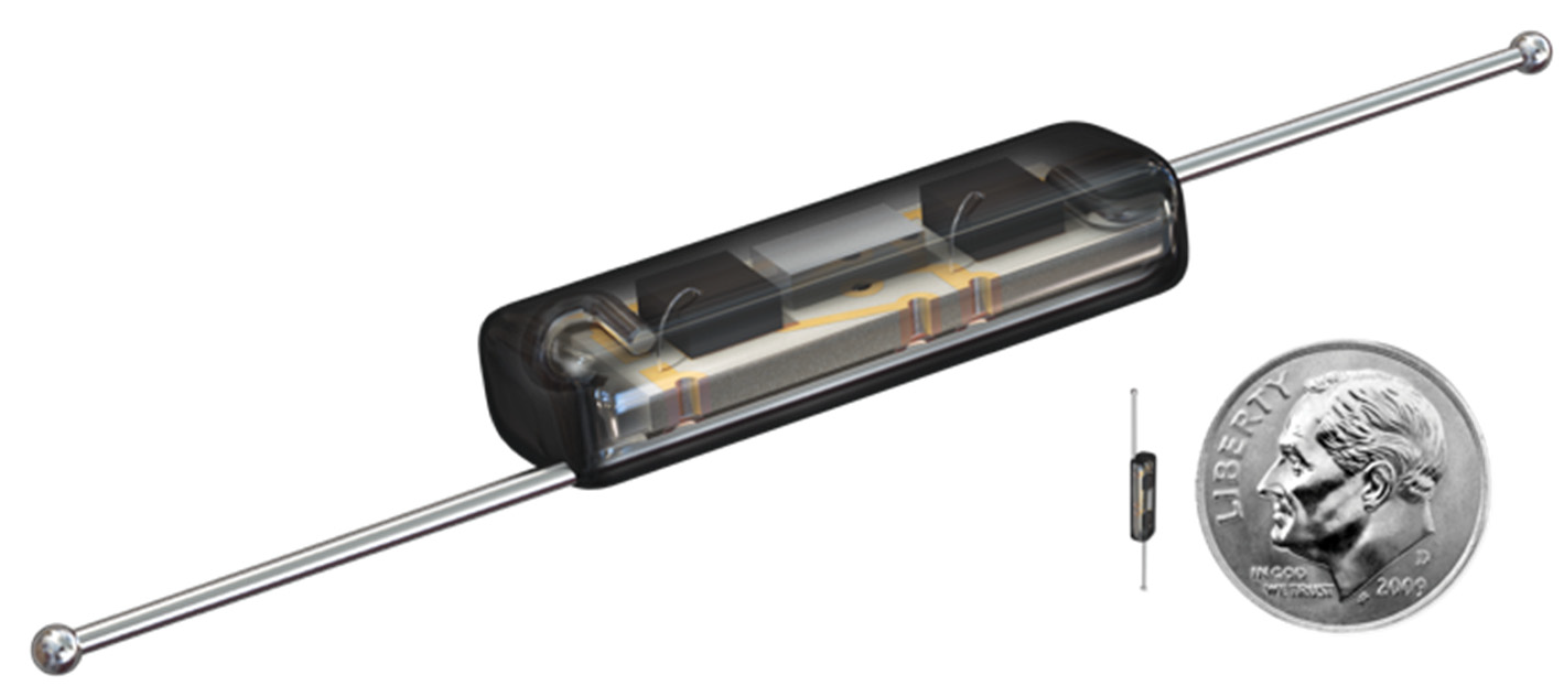
1. Introduction
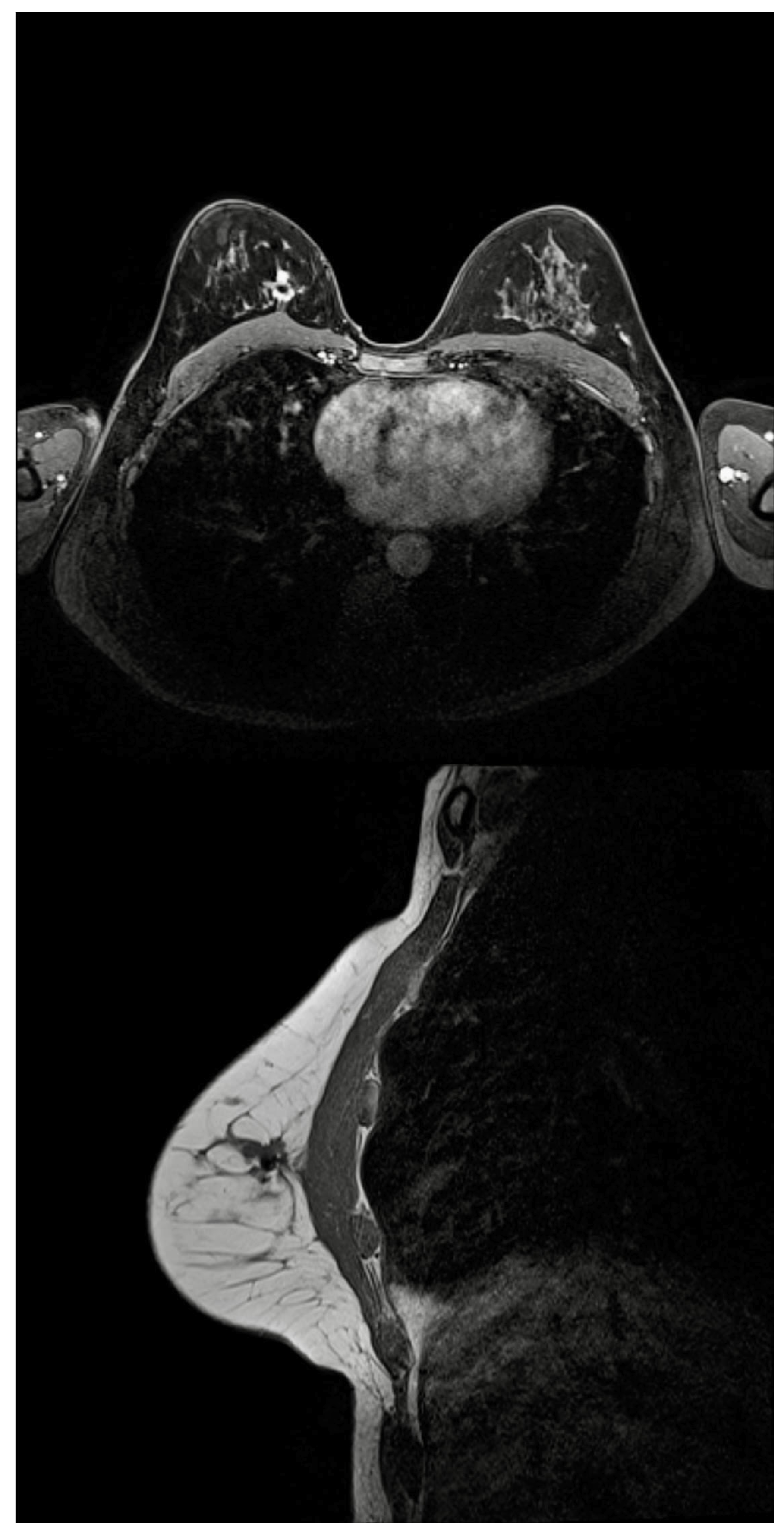
2. Materials and Methods
2.1. Setting
2.2. Data Collection
3. Results
3.1. Radiologists’ and Surgeon’s Acceptance
3.2. Patients’ Acceptance
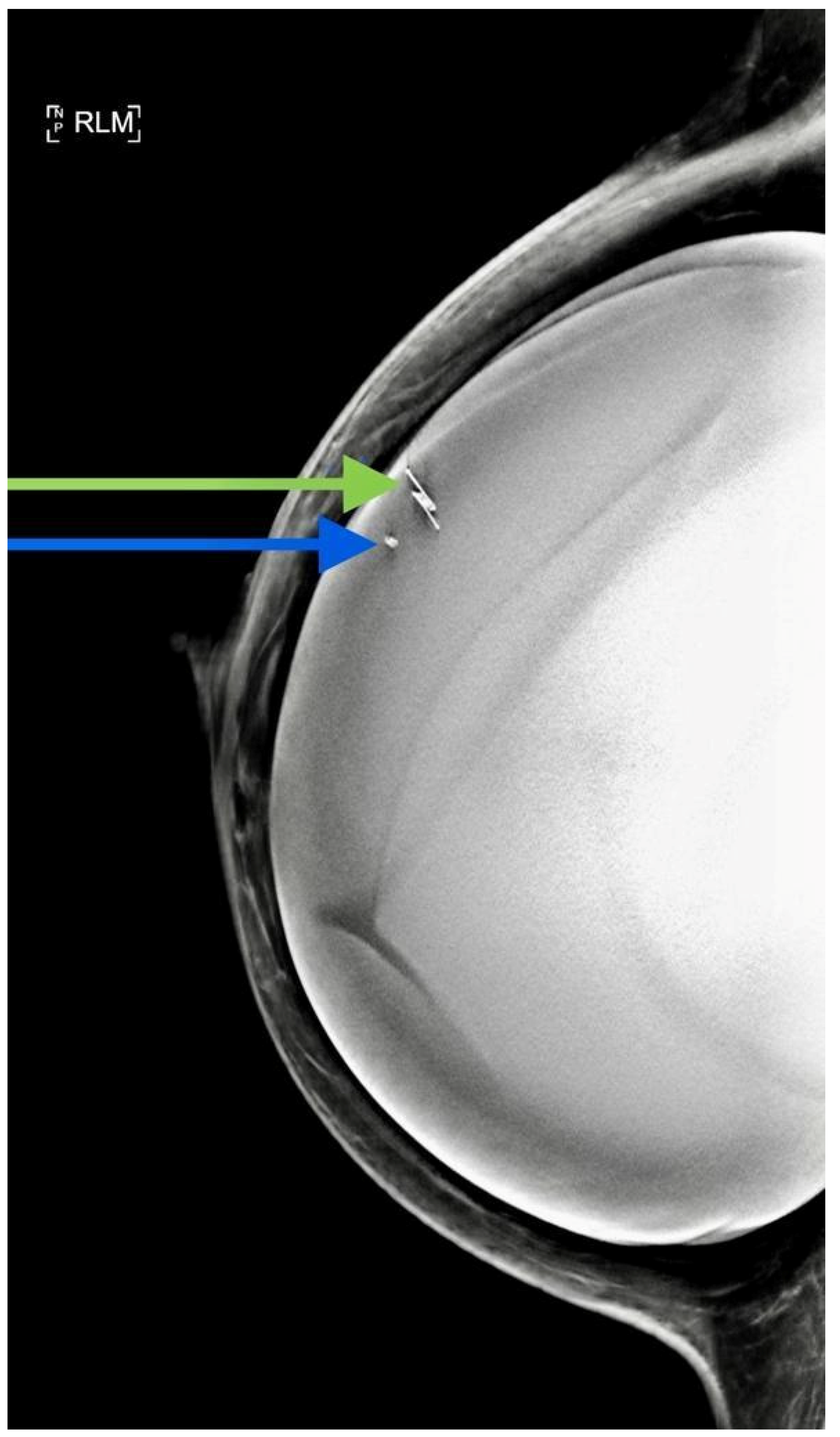
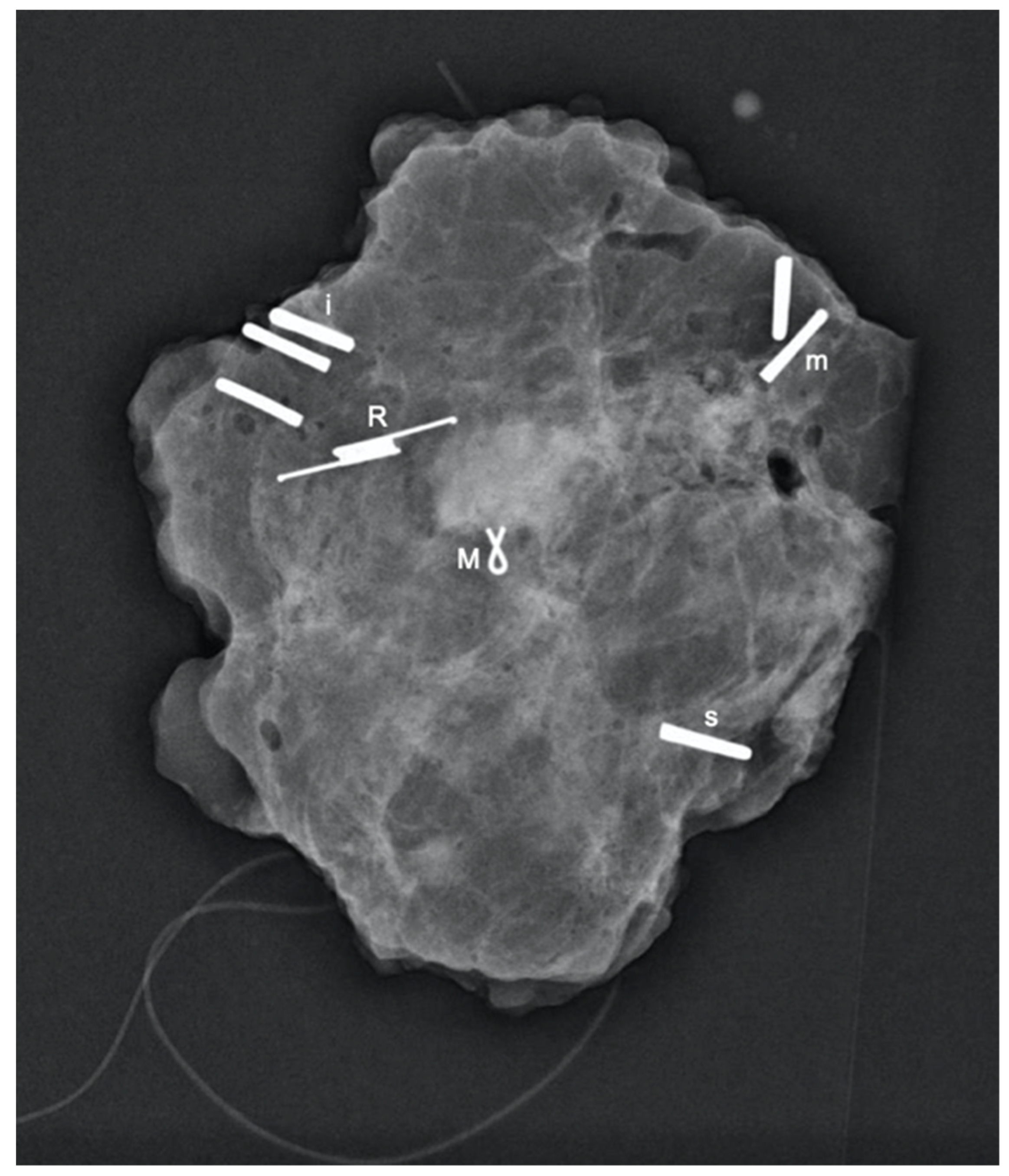
3.3. Retrieval and Migration
3.4. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aydogan, F.; Velidedeoglu, M.; Kilic, F.; Yilmaz, H. Radio-guided localization of clinically occult breast lesions: Current modalities and future directions. Expert Rev. Med. Devices 2014, 11, 53–63. [Google Scholar] [CrossRef]
- Frank, H.A.; Hall, F.M.; Steer, M.L. Preoperative localization of nonpalpable breast lesions demonstrated by mammography. N. Engl. J. Med. 1976, 295, 259–260. [Google Scholar] [CrossRef]
- Corsi, F.; Sorrentino, L.; Bossi, D.; Sartani, A.; Foschi, D. Preoperative localization and surgical margins in conservative breast surgery. Int. J. Surg. Oncol. 2013, 2013, 793819. [Google Scholar] [CrossRef] [PubMed]
- Davis, P.S.; Wechsler, R.J.; Feig, S.A.; March, D.E. Migration of breast biopsy localization wire. AJR Am. J. Roentgenol. 1988, 150, 787–788. [Google Scholar] [CrossRef] [PubMed]
- Cheang, E.; Ha, R.; Thornton, C.M.; Mango, V.L. Innovations in image-guided preoperative breast lesion localization. Br. J. Radiol. 2018, 91, 20170740. [Google Scholar] [CrossRef] [PubMed]
- Gilcrease, M.Z.; Dogan, B.E.; Black, D.M.; Contreras, A.; Dryden, M.J.; Jimenez, S.M. Transection of radioactive seeds in breast specimens. Am. J. Surg. Pathol. 2016, 40, 1375–1379. [Google Scholar] [CrossRef]
- Dua, S.M.; Gray, R.J.; Keshtgar, M. Strategies for localisation of impalpable breast lesions. Breast 2011, 20, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Dauway, E.; Saunders, R.; Friedland, J. Innovative diagnostics for breast cancer: New frontiers for the new millennium using radioactive seed localization. In 85th Annual American College of Surgeons Clinic Congress; American College of Surgeons: Chicago, IL, USA, 1999; Volume 50. [Google Scholar]
- Gray, R.J.; Salud, C.; Nguyen, K.; Dauway, E.; Friedland, J.; Berman, C.; Peltz, E.; Whitehead, G.; Cox, C.E. Randomized prospective evaluation of a novel technique for biopsy or lumpectomy of nonpalpable breast lesions: Radioactive seed versus wire localization. Ann. Surg. Oncol. 2001, 8, 711–715. [Google Scholar] [CrossRef] [PubMed]
- Jakub, J.; Gray, R. Starting a radioactive seed localization program. Ann. Surg. Oncol. 2015, 22, 3197–3202. [Google Scholar] [CrossRef] [PubMed]
- Goudreau, S.H.; Joseph, J.P.; Seiler, S.J. Preoperative radioactive seed localization for nonpalpable breast lesions: Technique, pitfalls, and solutions. Radiographics 2015, 35, 1319–1334. [Google Scholar] [CrossRef] [PubMed]
- DiNome, M.L.; Kusske, A.M.; Attai, D.J.; Fischer, C.P.; Hoyt, A.C. Microchipping the breast: An effective new technology for localizing non-palpable breast lesions for surgery. Breast Cancer Res. Treat. 2019, 175, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Harvey, J.R.; Lim, Y.; Murphy, J.; Howe, M.; Morris, J.; Goyal, A.; Maxwell, A.J. Safety and feasibility of breast lesion localization using magnetic seeds (magseed): A multi-centre, open-label cohort study. Breast Cancer Res. Treat. 2018, 169, 531–536. [Google Scholar] [CrossRef] [PubMed]
- Cox, C.E.; Russell, S.; Prowler, V.; Carter, E.; Beard, A.; Mehindru, A.; Blumencranz, P.; Allen, K.; Portillo, M.; Whitworth, P.; et al. A prospective, single arm, multi-site, clinical evaluation of a nonradioactive surgical guidance technology for the location of nonpalpable breast lesions during excision. Ann. Surg. Oncol. 2016, 23, 3168–3174. [Google Scholar] [CrossRef] [PubMed]
- Cox, C.E.; Garcia-Henriquez, N.; Glancy, M.J.; Whitworth, P.; Cox, J.M.; Themar-Geck, M.; Prati, R.; Jung, M.; Russell, S.; Appleton, K.; et al. Pilot study of a new nonradioactive surgical guidance technology for locating nonpalpable breast lesions. Ann. Surg. Oncol. 2016, 23, 1824–1830. [Google Scholar] [CrossRef] [PubMed]
- Tayeh, S.; Gera, R.; Perry, N.; Michell, M.; Malhotra, A.; Mokbel, K. The use of magnetic seeds and radiofrequency identifier tags in breast surgery for non-palpable lesions. Anticancer Res. 2020, 40, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Tardioli, S.; Ballesio, L.; Gigli, S.; Pastena, F.D.; D’Orazi, V.; Giraldi, G.; Monti, M.; Amabile, M.I.; Pasta, V. Wire-guided localization in non-palpable breast cancer: Results from monocentric experience. Anticancer Res. 2016, 36, 2423–2427. [Google Scholar]
- Velazco, C.S.; Wasif, N.; Pockaj, B.A.; Gray, R.J. Radioactive seed localization for breast conservation surgery: Low positive margin rate with no learning curve. Am. J. Surg. 2017, 214, 1091–1093. [Google Scholar] [CrossRef]
- Ansari, B.; Boughey, J.C.; Adamczyk, D.L.; Degnim, A.C.; Jakub, J.W.; Morton, M.J. Should axillary ultrasound be used in patients with a preoperative diagnosis of ductal carcinoma in situ? Am. J. Surg. 2012, 204, 290–293. [Google Scholar] [CrossRef] [PubMed]
- Wazir, U.; Tayeh, S.; Perry, N.; Michell, M.; Malhotra, A.; Mokbel, K. Wireless breast localization using radio-frequency identification tags: The first reported european experience in breast cancer. In Vivo 2020, 34, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Schermers, B.; van der Hage, J.A.; Loo, C.E.; Vrancken Peeters, M.; Winter-Warnars, H.A.O.; van Duijnhoven, F.; Ten Haken, B.; Muller, S.H.; Ruers, T.J.M. Feasibility of magnetic marker localisation for non-palpable breast cancer. Breast 2017, 33, 50–56. [Google Scholar] [CrossRef]
- Malter, W.; Holtschmidt, J.; Thangarajah, F.; Mallmann, P.; Krug, B.; Warm, M.; Eichler, C. First reported use of the faxitron localizer radiofrequency identification (rfid) system in europe—A feasibility trial, surgical guide and review for non-palpable breast lesions. In Vivo 2019, 33, 1559–1564. [Google Scholar] [CrossRef]
- Srour, M.K.; Kim, S.; Amersi, F.; Giuliano, A.E.; Chung, A. Comparison of wire localization, radioactive seed, and savi scout((r)) radar for management of surgical breast disease. Breast J. 2019, 26, 406–413. [Google Scholar] [CrossRef] [PubMed]
- Nhs Breast Screening Programme and Abs an Audit of Screen Detected Breast Cancers for the Year of Screening April 2013 to March 2014. Available online: https://associationofbreastsurgery.org.uk/audit/nhs-breast-screening-programme-audit/ (accessed on 12 September 2019).
- Kasem, I.; Mokbel, K. Savi scout(r) radar localisation of non-palpable breast lesions: Systematic review and pooled analysis of 842 cases. Anticancer Res. 2020, 40, 3633–3643. [Google Scholar] [CrossRef] [PubMed]
- Gera, R.; Tayeh, S.; Al-Reefy, S.; Mokbel, K. Evolving role of magseed in wireless localization of breast lesions: Systematic review and pooled analysis of 1559 procedures. Anticancer Res. 2020, 40, 1809–1815. [Google Scholar] [CrossRef] [PubMed]
- Micha, A.E.; Sinnett, V.; Downey, K.; Allen, S.; Bishop, B.; Hector, L.R.; Patrick, E.P.; Edmonds, R.; Barry, P.A.; Krupa, K.D.C.; et al. Patient and clinician satisfaction and clinical outcomes of magseed compared with wire-guided localisation for impalpable breast lesions. Breast Cancer 2021, 28, 196–205. [Google Scholar] [CrossRef] [PubMed]
- Tayeh, S.; Muktar, S.; Heeney, J.; Michell, M.J.; Perry, N.; Suaris, T.; Evans, D.; Malhotra, A.; Mokbel, K. Reflector-guided localization of non-palpable breast lesions: The first reported european evaluation of the savi scout(r) system. Anticancer Res. 2020, 40, 3915–3924. [Google Scholar] [CrossRef] [PubMed]
- Hayes, M.K. Update on preoperative breast localization. Radiol. Clin. N. Am. 2017, 55, 591–603. [Google Scholar] [CrossRef]
- Taback, B.; Jadeja, P.; Ha, R. Enhanced axillary evaluation using reflector-guided sentinel lymph node biopsy: A prospective feasibility study and comparison with conventional lymphatic mapping techniques. Clin. Breast Cancer 2018, 18, e869–e874. [Google Scholar] [CrossRef]
- Falcon, S.; Weinfurtner, R.J.; Mooney, B.; Niell, B.L. Savi scout(r) localization of breast lesions as a practical alternative to wires: Outcomes and suggestions for trouble-shooting. Clin. Imaging 2018, 52, 280–286. [Google Scholar] [CrossRef]
- Sun, J.; Henry, D.A.; Carr, M.J.; Yazdankhahkenary, A.; Laronga, C.; Lee, M.C.; Hoover, S.J.; Sun, W.; Czerniecki, B.J.; Khakpour, N.; et al. Feasibility of axillary lymph node localization and excision using radar reflector localization. Clin. Breast Cancer 2020, in press. [Google Scholar] [CrossRef] [PubMed]
- Kalambo, M.; Parikh, J.R. Implementing the savi scout system in community radiology practice. J. Am. Coll. Radiol. 2017, 14, 1234–1238. [Google Scholar] [CrossRef]
- Jeffries, D.O.; Dossett, L.A.; Jorns, J.M. Localization for breast surgery: The next generation. Arch. Pathol. Lab. Med. 2017, 141, 1324–1329. [Google Scholar] [CrossRef]
- Mango, V.L.; Wynn, R.T.; Feldman, S.; Friedlander, L.; Desperito, E.; Patel, S.N.; Gomberawalla, A.; Ha, R. Beyond wires and seeds: Reflector-guided breast lesion localization and excision. Radiology 2017, 284, 365–371. [Google Scholar] [CrossRef]

| Case | Age | Distance of Scout to Target on Mammogram (mm) | Duration of Localisation (Minutes) | Duration of Identification and Retrieval (Minutes) | Specimen Weight (g) | Radiologist’s Feedback Compared with Wire Localisation | Patient’s Satisfaction | Pathological TNM Stage | Radial Margins’ Status | Time Interval between Localisation and Surgery (Days) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 52 | 0 | 5 | 31 | 20 | neutral | 10 | pT1c (multi) N0 | clear | 4 |
| 2 | 50 | 0 | 5 | 29 | 31 | better | 10 | pTis 41 mm | clear | 3 |
| 3 | 46 | 0 | 5 | 15 | 14.5 | much better | 9 | pT1bN0 | clear | 1 |
| 4 | 55 | 0 | 5 | 50 | 25 | better | 10 | pT1cN0 | clear | 1 |
| 5 | 58 | 0 | 5 | 23 | 19 | much better | 9 | ypT2 (multi) N1mic | clear | 1 |
| 0 | 5 | clear | ||||||||
| 6 | 66 | 0 | 4 | 15 | 12 | much better | 10 | pT1bN0 | clear | 1 |
| 7 | 74 | 3 | 5 | 28 | 10.5 | better | 10 | pT2 N0 | clear | 1 |
| 8 | 60 | 0 | 3 | 25 | 21.5 | much better | 10 | pT2N1 | clear | 0 |
| 9 | 74 | 0 (stereotactic) | 10 | 38 | 39.5 | better | 9 | pT1aN0 | clear | 7 |
| 10 | 53 | 0 | 15 | 40 | 34 | better | 10 | pT1cN0 | clear | 1 |
| 11 | 76 | 0 | 2 | 19 | 7.5 | - | 10 | pTis | clear | |
| 12 | 50 | 0 | 3 | 45 | 11.5 | better | 10 | ypT1N0 | clear | 34 |
| 13 | 59 | 0 | 2 | 23 | 70 | better | 10 | T1cN0 | clear | 0 |
| 14 | 27 | 3 | 3 | 26 | 16 | better | 10 | ypT1aN0 | clear | 0 |
| 15 | 45 | 3 | 5 | 20 | 14.5 | much better | ypT0N0 | clear | 8 | |
| 16 | 36 | 0 | 4 | 37 | 19.5 | better | 7 | T3N0 | focally positive for DCIS | 0 |
| 17 | 62 | 4.5 | 15 | 22 | 13 | better | 10 | Tis | clear | 0 |
| 18 | 53 | 2 | 8 | 30 | 13 | better | 9 | ypT0N0 | clear | 7 |
| 19 | 63 | 0 | 4 | 25 | 32 | neutral | 10 | pT1N0 | clear | 0 |
| 20 | 42 | 0 | 3 | 28 | 31.5 | better | 10 | pT2NxM1 | clear | 0 |
| 21 | 60 | 0 | 3 | 30 | 9.5 | better | pTis | clear | 14 | |
| 22 | 53 | 2 | 8 | 30 | 13 | better | 10 | ypT0N0 | clear | 19 |
| 23 | 74 | 3 | 5 | 30 | 17 | neutral | 10 | pTisN0 | clear | 0 |
| 24 | 48 | 1 | 5 | 30 | 32 | much better | 9 | pT1N0 | clear | 1 |
| 25 | 59 | 0 | 5 | 30 | 51.5 | better | 10 | pT3N1 | positive | 0 |
| 0 | 5 | 30 | 38.5 | better | pT1N0 | |||||
| 26 | 36 | 0 | 5 | 28 | - | better | 10 | pT1cN0 | clear | 0 |
| 27 | 53 | 0 | 5 | 25 | 23 | much better | 10 | pT1cN0 | clear | 11 |
| 28 | 40 | 30 | 4.5 | - | pT2N0 | positive | 5 | |||
| 29 | 47 | 0 | 7 | 29 | 14 | neutral | 10 | pT1cN0 | clear | 3 |
| 30 | 32 | 0 | 5 | 25 | 13 | better | 9 | ypT0N0 | clear | 210 |
| 31 | 47 | 0 | 3 | 23 | 7.5 | better | 10 | ypTisN0 | clear | 101 |
| 32 | 63 | 20 (stereotactic) | 10 | 25 | - | better | 10 | pTis | clear | 3 |
| 33 | 44 | 0 | 10 | 26 | - | much better | 10 | pT1N0 multifocal | clear | 3 |
| 34 | 58 | 0 | 5 | 38 | 32.5 | much better | 8 | pT2N0 | clear | 2 |
| 35 | 42 | 0 | 5 | 22 | - | - | pTis (16 mm) | clear | 0 | |
| 36 | 46 | 16 (stereotactic) | 5 | 55 | 8 | less favourable than wire | 10 | pT1 | clear | 0 |
| 37 | 46 | 0 | 5 | 38 | 26.5 | better | 10 | pT1N0 | clear | 0 |
| 38 | 64 | 0 | 2 | 35 | 20 | better | 10 | pT1N0 | clear | 3 |
| 39 | 58 | 0 | 3 | 22 | - | better | pT2N0 | clear | 5 | |
| 40 | 51 | 0 | 6 | 32 | 35 | - | pTis (21 mm) | positive (1 mm: radial margin) | 2 | |
| 41 | 52 | 0 | 5 | 31 | 33.5 | better | 10 | ypTisN0 | clear | 1 |
| 42 | 73 | 0 | 2 | 25 | 34.5 | - | 10 | ypT0N0 | clear | 97 |
| 43 | 55 | 0 | 5 | 35 | 68.5 | better | pT2N0 | clear | 5 | |
| 44 | 55 | 0 | 10 | 21 | 38 | much better | 10 | pT1N0 multifocal | clear | 24 |
| 15 | 10 | 21 | ||||||||
| 45 | 55 | 0 | 10 | 17 | 14.4 | much better | pT1b (multi) N1 (micro) | clear | 3 | |
| 46 | 64 | 0 | 3 | 25 | 5.3 | much better | 10 | ypT0N0 | clear | 197 |
| 47 | 45 | 0 | - | 19 | 19.8 | better | pT1N0 | clear | 8 | |
| 48 | 78 | 0 | 3 | 16 | 10.5 | - | pT1N0 | clear | 19 | |
| 49 | 41 | 0 | 2 | 20 | 7.5 | better | 10 | pTis | clear | 3 |
| 50 | 71 | 0 | 3 | 19 | 3.5 | much better | 10 | pT1cN0 | clear | 8 |
| 51 | 62 | 0 | 5 | 34 | 27 | much better | 10 | pTis (multi) | clear | 36 |
| Stereotactic | ||||||||||
| 52 | 80 | 0 | 2 | 26 | 56 | much better | 10 | pT1c (multi) N0 | clear | 3 |
| 0 | 2 | |||||||||
| 53 | 81 | 0 | 3 | 15 | 14.5 | better | pT1bN0 | clear | 3 | |
| 54 | 71 | - | 5 | 17 | 17.5 | better | ypTisN2M1 | clear | 3 | |
| 55 | 48 | 0 | 5 | 30 | - | - | pT2N0 | clear | 3 | |
| 56 | 50 | 0 | 3 | 45 | 24 | much better | pT2N0 | clear | 1 | |
| 57 | 50 | 0 | 5 | 35 | 24 | - | ypT1N0 | clear | 188 |
| Case | Age | Distance of Scout to Target on Mammogram (mm) | Duration of Localisation (minutes) | Duration of Identification and Retrieval (minutes) | Specimen Weight (g) | Radiologist’s Feedback Compared with Wire Localisation | Patient’s Satisfaction | Pathology | Time Interval between Localisation and Surgery (Days) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 58 | 0 | 1 | 18 | 7.5 | much better | 10 | Papilloma | 0 |
| 2 | 47 | 0 | 4 | 19 | 11.5 | much better | 10 | Benign breast change | 0 |
| 0 | 4 | 19 | 13.5 | Papilloma | |||||
| 3 | 69 | 0 | 15 | 15 | 18.5 | better | Malignant adenomyoepithelioma + papillomatosis | 0 | |
| 4 | 68 | 0 | 3 | 16 | - | much better | ADH | 0 | |
| 5 | 48 | 0 | 5 | 15 | 7.5 | neutral | CSL | ||
| 6 | 28 | 0 | 5 | 15 | 3 | better | Fibroadenoma | 0 | |
| 7 | 34 | 1 (stereotactic) | 5 | 24 | 11 | - | LCIS/ALH/CSL | 0 | |
| 8 | 36 | 1 | 5 | 17 | 5 | better | papilloma | 0 | |
| 9 | 38 | 0 | 4 | 16 | 8 | better | Atypical columnar change | 3 | |
| 10 | 44 | 0 | 5 | 17 | 18 | better | 10 | CSL | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wazir, U.; Kasem, I.; Michell, M.J.; Suaris, T.; Evans, D.; Malhotra, A.; Mokbel, K. Reflector-Guided Localisation of Non-Palpable Breast Lesions: A Prospective Evaluation of the SAVI SCOUT® System. Cancers 2021, 13, 2409. https://doi.org/10.3390/cancers13102409
Wazir U, Kasem I, Michell MJ, Suaris T, Evans D, Malhotra A, Mokbel K. Reflector-Guided Localisation of Non-Palpable Breast Lesions: A Prospective Evaluation of the SAVI SCOUT® System. Cancers. 2021; 13(10):2409. https://doi.org/10.3390/cancers13102409
Chicago/Turabian StyleWazir, Umar, Iham Kasem, Michael J. Michell, Tamara Suaris, David Evans, Anmol Malhotra, and Kefah Mokbel. 2021. "Reflector-Guided Localisation of Non-Palpable Breast Lesions: A Prospective Evaluation of the SAVI SCOUT® System" Cancers 13, no. 10: 2409. https://doi.org/10.3390/cancers13102409
APA StyleWazir, U., Kasem, I., Michell, M. J., Suaris, T., Evans, D., Malhotra, A., & Mokbel, K. (2021). Reflector-Guided Localisation of Non-Palpable Breast Lesions: A Prospective Evaluation of the SAVI SCOUT® System. Cancers, 13(10), 2409. https://doi.org/10.3390/cancers13102409






