Spontaneous Non-Sustained Ventricular Tachycardia and Premature Ventricular Contractions and Their Prognostic Relevance in Patients with Cancer in Routine Care
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. 24-h Electrocardiograms
2.3. Statistical Analyses
3. Results
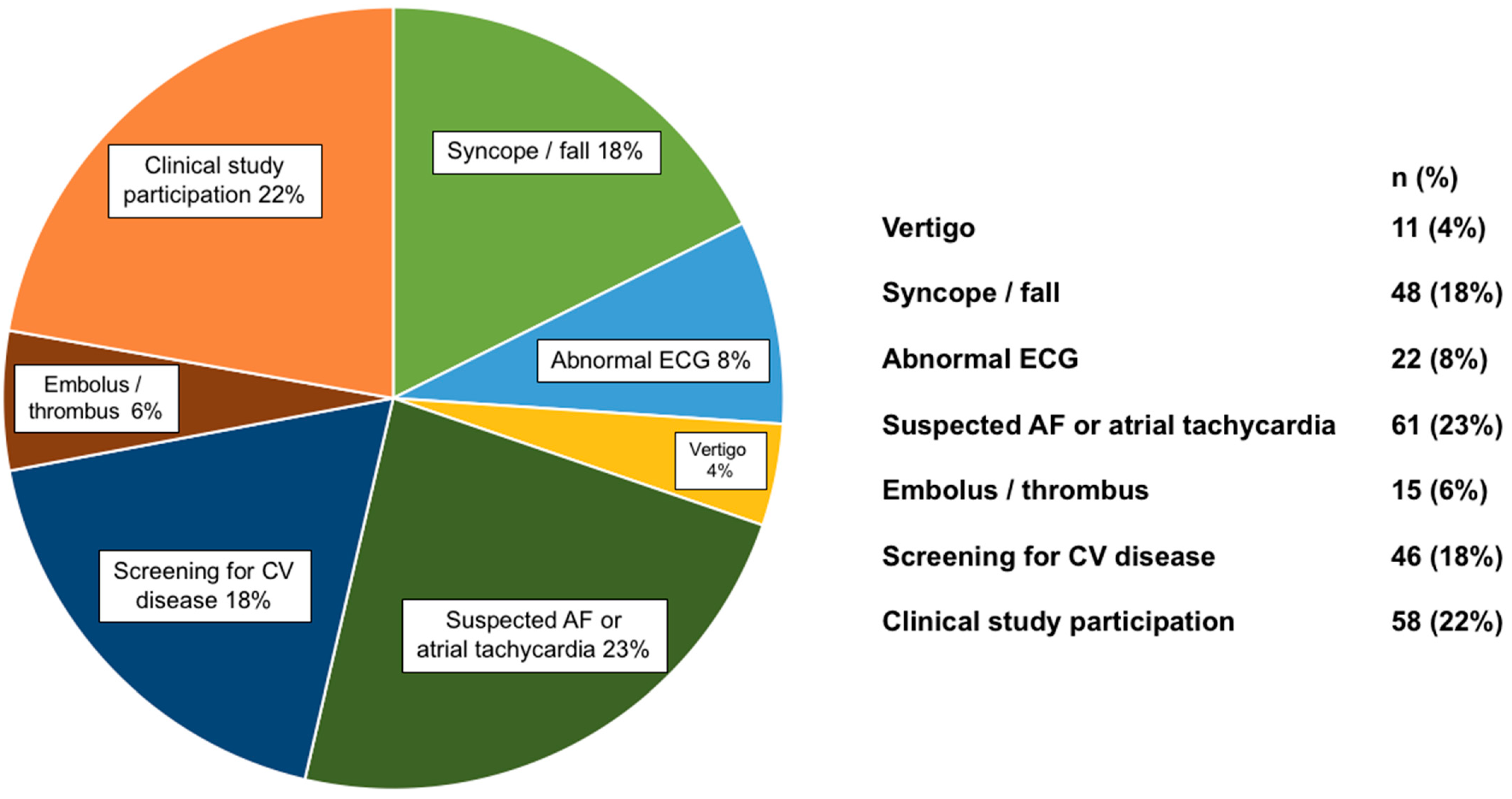
3.1. Study Population
3.2. 24-h Electrocardiograms
3.3. Comparing Patients with and without Ventricular Arrhythmias
3.4. Comparing Patients with and without Death during Follow-Up
3.5. Survival Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Inagaki, J.; Rodriguez, V.; Bodey, G.P. Proceedings: Cause of death in cancer patients. Cancer 1974, 33, 568–573. [Google Scholar] [CrossRef]
- Brown, B.W.; Brauner, C.; Minnotte, M.C. Noncancer deaths in white adult cancer patients. J. Natl. Cancer Inst. 1993, 85, 979–987. [Google Scholar] [CrossRef]
- Zamorano, J.L.; Lancellotti, P.; Rodruguez Munoz, D.; Aboyans, V.; Asteggiano, R.; Galderisi, M.; Habib, G.; Lenihan, D.J.; Lip, G.Y.H.; Lyon, A.R.; et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur. Heart J. 2016, 37, 2768–2801. [Google Scholar] [CrossRef] [PubMed]
- Cardinale, D.; Sandri, M.T.; Colombo, A.; Colombo, N.; Boeri, M.; Lamantia, G.; Civelli, M.; Peccatori, F.; Martinelli, G.; Fiorentini, C.; et al. Prognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapy. Circulation 2004, 109, 2749–2754. [Google Scholar] [CrossRef] [PubMed]
- Anker, M.S.; Ebner, N.; Hildebrandt, B.; Springer, J.; Sinn, M.; Riess, H.; Anker, S.D.; Landmesser, U.; Haverkamp, W.; von Haehling, S. Resting heart rate is an independent predictor of death in patients with colorectal, pancreatic, and non-small cell lung cancer: Results of a prospective cardiovascular long-term study. Eur. J. Heart Fail. 2016, 18, 1524–1534. [Google Scholar] [CrossRef] [PubMed]
- Saltzman, H.E. Arrhythmias and heart failure. Cardiol. Clin. 2014, 32, 125–133. [Google Scholar] [CrossRef]
- Oken, M.M.; Creech, R.H.; Tormey, D.C.; Horton, J.; Davis, T.E.; McFadden, E.T.; Carbone, P.P. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am. J. Clin. Oncol. 1982, 5, 649–655. [Google Scholar] [CrossRef]
- De Medina, E.O.R.; Bernard, R.; Coumel, P.; Damato, A.N.; Fisch, C.; Krikler, D.; Mazur, N.A.; Meijler, F.L.; Mogensen, L.; Moret, P.; et al. Definition of terms related to cardiac rhythm. WHO/ISFC Task Force. Eur. J. Cardiol. 1978, 8, 127–144. [Google Scholar]
- Pedersen, C.T.; Kay, G.N.; Kalman, J.; Borggrefe, M.; Della-Bella, P.; Dickfeld, T.; Dorian, P.; Huikuri, H.; Kim, Y.-H.; Knight, B.; et al. EHRA/HRS/APHRS expert consensus on ventricular arrhythmias. Europace 2014, 16, 1257–1283. [Google Scholar] [CrossRef]
- Mehta, C.R.; Senchaudhuri, P.J.C.S.C. Conditional versus unconditional exact tests for comparing two binomials. Cytel Softw. Corp. 2003, 675, 1–5. [Google Scholar]
- Barnard, G.J.N. A new test for 2×2 tables. Nature 1945, 156, 177. [Google Scholar] [CrossRef]
- Martín Andrés, A.; Quevedo, M.J.S.; Mato, A.S. Fisher’s Mid-P-value arrangement in 2 × 2 Comparative trials. Comput. Stat. Data Anal. 1998, 29, 107–115. [Google Scholar] [CrossRef]
- Savitz, D.A.; Olshan, A.F. Describing data requires no adjustment for multiple comparisons: A reply from Savitz and Olshan. Am. J. Epidemiol. 1998, 147, 813–814. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Thompson, J.R. Invited Commentary: Re: ‘Multiple Comparisons and Related Issues in the Interpretation of Epidemiologic Data”. Am. J. Epidemiol. 1998, 147, 801–806. [Google Scholar] [CrossRef] [PubMed]
- Anker, M.S.; von Haehling, S.; Coats, A.J.S.; Riess, H.; Eucker, J.; Porthun, J.; Butler, J.; Karakas, M.; Haverkamp, W.; Landmesser, U.; et al. Ventricular tachycardia, premature ventricular contractions, and mortality in unselected patients with lung, colon, or pancreatic cancer: A prospective study. Eur. J. Heart Fail. 2021, 23, 145–153. [Google Scholar] [CrossRef]
- Hingorani, P.; Karnad, D.R.; Rohekar, P.; Kerkar, V.; Lokhandwala, Y.Y.; Kothari, S. Arrhythmias Seen in Baseline 24-Hour Holter ECG Recordings in Healthy Normal Volunteers During Phase 1 Clinical Trials. J. Clin. Pharmacol. 2016, 56, 885–893. [Google Scholar] [CrossRef] [PubMed]
- Priori, S.G.; Blomström-Lundqvist, C.; Mazzanti, A.; Blom, N.; Borggrefe, M.; Camm, J.; Elliott, P.M.; Fitzsimons, D.; Hatala, R.; Hindricks, G.; et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur. Heart J. 2015, 36, 2793–2867. [Google Scholar]
- Mullis, A.H.; Ayoub, K.; Shah, J.; Butt, M.; Suffredini, J.; Czarapata, M.; Delisle, B.; Ogunbayo, G.O.; Darrat, Y.; Elayi, C.S. Fluctuations in premature ventricular contraction burden can affect medical assessment and management. Heart Rhythm 2019, 16, 1570–1574. [Google Scholar] [CrossRef]
- Zaorsky, N.G.; Churilla, T.M.; Egleston, B.L.; Fisher, S.G.; Ridge, J.A.; Horwitz, E.M.; Meyer, J.E. Causes of death among cancer patients. Ann. Oncol. 2017, 28, 400–407. [Google Scholar] [CrossRef]
- Anker, M.S.; Hülsmann, M.; Cleland, J.G. What do patients with heart failure die from? A single assassin or a conspiracy? Eur. J. Heart Fail. 2019. [Google Scholar] [CrossRef]
- Cramer, L.; Hildebrandt, B.; Kung, T.; Wichmann, K.; Springer, J.; Doehner, W.; Sandek, A.; Valentova, M.; Stojakovic, T.; Scharnagl, H.; et al. Cardiovascular function and predictors of exercise capacity in patients with colorectal cancer. J. Am. Coll. Cardiol. 2014, 64, 1310–1319. [Google Scholar] [CrossRef]
- Anker, M.S.; Sanz, A.P.; Zamorano, J.L.; Mehra, M.R.; Butler, J.; Riess, H.; Coats, A.J.S.; Anker, S.D. Advanced cancer is also a heart failure syndrome: A hypothesis. J. Cachexia Sarcopenia Muscle 2021. [Google Scholar] [CrossRef] [PubMed]
- Anker, M.S.; Sanz, A.P.; Zamorano, J.L.; Mehra, M.R.; Butler, J.; Riess, H.; Coats, A.J.S.; Anker, S.D. Advanced cancer is also a heart failure syndrome: A hypothesis. Eur. J. Heart Fail. 2021, 23, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Shibata, H. Cancer and electrolytes imbalance. Gan Kagaku Ryoho 2010, 37, 1006–1010. [Google Scholar]
- Karlstaedt, A.; Zhang, X.; Vitrac, H.; Harmancey, R.; Vasquez, H.; Wang, J.H.; Goodell, M.A.; Taegtmeyer, H. Oncometabolite d-2-hydroxyglutarate impairs α-ketoglutarate dehydrogenase and contractile function in rodent heart. Proc. Natl. Acad. Sci. USA 2016, 113, 10436–10441. [Google Scholar] [CrossRef] [PubMed]
- Tian, M.; Nishijima, Y.; Asp, M.L.; Stout, M.B.; Reiser, P.J.; Belury, M.A. Cardiac alterations in cancer-induced cachexia in mice. Int. J. Oncol. 2010, 37, 347–353. [Google Scholar]
- Mühlfeld, C.; Das, S.K.; Heinzel, F.R.; Schmidt, A.; Post, H.; Schauer, S.; Papadakis, T.; Kummer, W.; Hoefler, G. Cancer induces cardiomyocyte remodeling and hypoinnervation in the left ventricle of the mouse heart. PLoS ONE 2011, 6, e20424. [Google Scholar]
- Barkhudaryan, A.; Scherbakov, N.; Springer, J.; Doehner, W. Cardiac muscle wasting in individuals with cancer cachexia. ESC Heart Fail. 2017, 4, 458–467. [Google Scholar] [CrossRef] [PubMed]


| Variable | Healthy Controls (n = 35) | Cancer Patients (n = 261) | p-Value | Cancer Deaths (n = 158) | Cancer Survivors (n = 103) | p-Value |
|---|---|---|---|---|---|---|
| Clinical characteristics | ||||||
| Age (years) | 68 ± 6 (IQR 62–73) | 68 ± 12 (IQR 61–76) | 0.86 | 69 ± 10 (IQR 62–75) | 65 ± 17 (IQR 58–76) | 0.016 |
| Female sex, n (%) | 19 (54) | 132 (51) | 0.68 | 76 (48) | 56 (54) | 0.32 |
| BMI (kg/m2) | 26 ± 4 | 24 ± 5 | 0.28 | 25 ± 5 | 26 ± 5 | 0.049 |
| Cancer stage ≥III, n (%) | – | 188 (72) | – | 123 (78) | 65 (63) | 0.0095 |
| Cancer type: solid, n (%) | – | 129 (49) | – | 93 (59) | 36 (35) | 0.0002 |
| ECOG performance status ≥2, n (%) | – | 111 (43) | – | 75 (47) | 36 (35) | 0.046 |
| Prior potentially cardiotoxic anti-cancer drugs, n (%) | – | 162 (62) | – | 104 (66) | 58 (56) | 0.12 |
| Left ventricular ejection fraction (%) | 64 ± 7 | 65 ± 7 (n = 181) | 0.81 | 64 ± 8 (n = 100) | 65 ± 7 (n = 81) | 0.27 |
| Laboratory parameters | ||||||
| Haemoglobin (g/dL) | 14.2 ± 1.3 | 10.8 ± 2.0 | <0.0001 | 10.6 ± 1.9 | 11.1 ± 2.1 | 0.040 |
| Leucocytes (/nL) | 6.6 (5.5–7.6) | 6.5 (4.3-9.6) | 0.99 | 6.9 (4.4–9.9) | 6.1 (4.3–9.2) | 0.40 |
| Platelets (/nL) | 227 ± 46 | 225 ± 166 | 0.97 | 231 ± 195 | 217 ± 108 | 0.48 |
| Sodium (mmol/L) | 141 ± 2 | 139 ± 4 | 0.0002 | 138 ± 4 | 140 ± 3 | 0.0027 |
| Potassium (mmol/L) | 4.2 ± 0.4 | 3.9 ± 0.5 | 0.0004 | 3.9 ± 0.5 | 3.9 ± 0.5 | 0.91 |
| Creatinine (mg/dL) | 0.87 ± 0.19 | 1.00 ± 0.59 | 0.22 | 1.03 ± 0.68 | 0.94 ± 0.40 | 0.23 |
| GOT (U/L) | 26 (22–28) | 26 (19-37) (n = 171) | 0.75 | 27 (19–39) (n = 101) | 25 (19–34) (n = 70) | 0.34 |
| Secondary diagnoses | ||||||
| Arterial hypertension, n (%) | 7 (20) | 132 (51) | 0.0007 | 79 (50) | 53 (51) | 0.82 |
| Coronary artery disease, (%) | 0 | 34 (13) | 0.0040 | 22 (14) | 12 (12) | 0.59 |
| Atrial fibrillation, n (%) | 0 | 14 (5) | 0.08 | 8 (5) | 6 (6) | 0.79 |
| Previous myocardial infarction, n (%) | 0 | 20 (8) | 0.033 | 13 (8) | 7 (7) | 0.67 |
| Diabetes mellitus type 2, n (%) | 0 | 50 (19) | 0.0003 | 31 (20) | 19 (18) | 0.81 |
| Chronic kidney disease, n (%) | 0 | 41 (16) | 0.0014 | 28 (18) | 13 (13) | 0.27 |
| Previous stroke, n (%) | 0 | 27 (10) | 0.011 | 17 (11) | 10 (10) | 0.79 |
| Current use of antibiotics, n (%) | 0 | 45 (17) | 0.0007 | 33 (21) | 12 (12) | 0.054 |
| 24 h-ECG | ||||||
| Average 24 h heart rate (bpm) | 70 ± 9 | 78 ± 14 | 0.0007 | 79 ± 16 | 77 ± 11 | 0.41 |
| No. of premature atrial contractions/24 h | 82 (27–302) | 195 (27–1167) | 0.22 | 227 (32–1226) | 146 (24–761) | 0.20 |
| No. of premature ventricular contractions/24 h | 9 (1–43) | 26 (2–360) | 0.06 | 54 (4–467) | 12 (1–280) | 0.013 |
| ≥20 Premature ventricular contractions/24 h, n (%) | 13 (37) | 139 (53) | 0.07 | 95 (60) | 44 (43) | 0.0059 |
| ≥50 Premature ventricular contractions/24 h, n (%) | 8 (23) | 117 (45) | 0.013 | 80 (51) | 37 (36) | 0.020 |
| NSVT with ≥3 beats & ≥100 bpm, n (%) | 0 | 44 (17) | 0.0008 | 31 (20) | 13 (13) | 0.14 |
| NSVT with ≥4 beats & ≥100 bpm, n (%) | 0 | 25 (10) | 0.016 | 21 (13) | 4 (4) | 0.0066 |
| Variable | Univariate Model | |||||||
| HR | 95% CI | χ2 | p-Value | |||||
| Significant and Clinically Relevant Variables | ||||||||
| NSVT ≥4 beats & ≥100 bpm (yes vs. no) | 1.66 | 1.04–2.63 | 4.6 | 0.033 | ||||
| ≥20 Premature ventricular contractions/24 h (yes vs. no) | 1.67 | 1.21–2.30 | 9.9 | 0.0017 | ||||
| Age (per 1 year) | 1.01 | 1.001–1.03 | 4.3 | 0.039 | ||||
| BMI (per 1 kg/m2) | 0.95 | 0.91–0.98 | 8.1 | 0.0043 | ||||
| Cancer stage (≥III vs. I/II) | 1.66 | 1.14–2.42 | 7.0 | 0.0082 | ||||
| Cancer type (solid vs. haematologic) | 2.09 | 1.52–2.87 | 20.3 | <0.0001 | ||||
| ECOG performance status (≥2 vs. 0/1) | 1.58 | 1.15–2.17 | 8.2 | 0.0043 | ||||
| Haemoglobin (per 1 g/dL) | 0.91 | 0.84–0.99 | 5.3 | 0.021 | ||||
| Sodium (per 1 mmol/L) | 0.94 | 0.90–0.98 | 10.4 | 0.0013 | ||||
| Opioids (yes vs. no) | 1.67 | 1.13–2.47 | 6.7 | 0.0097 | ||||
| Antidepressants (yes vs. no) | 1.85 | 1.14–2.99 | 6.2 | 0.013 | ||||
| Prior potentially cardiotoxic anti-cancer drugs (yes vs. no) | 1.41 | 1.02–1.96 | 4.2 | 0.039 | ||||
| Sex (female vs. male) | 0.80 | 0.59–1.10 | 1.9 | 0.17 | ||||
| Potassium (per 1 mmol/L) | 1.07 | 0.78–1.48 | 0.2 | 0.66 | ||||
| Current use of antibiotics (yes vs. no) | 1.29 | 0.88–1.90 | 1.7 | 0.19 | ||||
| Coronary artery disease (yes vs. no) | 0.99 | 0.63–1.56 | 0.001 | 0.98 | ||||
| Variable | Multivariate Model 1 | Multivariate Model 2 | ||||||
| HR | 95% CI | χ2 | p-Value | HR | 95% CI | χ2 | p-Value | |
| Multivariate Survival Analyses in Cancer Patients with NSVT ≥4 beats & ≥100 bpm | ||||||||
| NSVT ≥4 beats & ≥100 bpm (yes vs. no) | 1.82 | 1.13–2.94 | 6.0 | 0.015 | 1.76 | 1.09–2.84 | 5.3 | 0.022 |
| Age (per 1 year) | 1.02 | 1.01–1.04 | 8.4 | 0.0038 | 1.02 | 1.01–1.04 | 8.2 | 0.0041 |
| Sodium (per 1 mmol/L) | 0.96 | 0.92–1.002 | 3.5 | 0.061 | 0.96 | 0.92–1.003 | 3.4 | 0.07 |
| Haemoglobin (per 1 g/dL) | 0.92 | 0.84–1.0003 | 3.8 | 0.051 | 0.92 | 0.84–1.004 | 3.5 | 0.06 |
| BMI (per 1 kg/m2) | 0.96 | 0.93–0.996 | 4.7 | 0.031 | 0.96 | 0.92–0.998 | 4.2 | 0.041 |
| Opioids (yes vs. no) | 1.33 | 0.88–2.03 | 1.8 | 0.18 | 1.33 | 0.87–2.04 | 1.7 | 0.19 |
| Antidepressants (yes vs. no) | 1.50 | 0.91–2.47 | 2.6 | 0.11 | 1.60 | 0.97–2.64 | 3.4 | 0.07 |
| Cancer stage (≥III vs. I/II) | 1.50 | 1.01–2.21 | 4.1 | 0.043 | 1.52 | 1.03–2.24 | 4.4 | 0.037 |
| Cancer type (solid vs. haematologic) | 2.46 | 1.75–3.46 | 26.9 | <0.0001 | 2.54 | 1.80–3.59 | 27.7 | <0.0001 |
| ECOG performance status (≥2 vs. 0/1) | 1.23 | 0.87–1.73 | 1.4 | 0.24 | 1.40 | 0.97–2.01 | 3.3 | 0.07 |
| Prior potentially cardiotoxic anti-cancer drugs (yes vs. no) | 1.68 | 1.18–2.40 | 8.2 | 0.0041 | 1.70 | 1.19–2.43 | 8.4 | 0.0037 |
| Sex (female vs. male) | 0.68 | 0.48–0.95 | 5.1 | 0.024 | ||||
| Potassium (per 1 mmol/L) | 1.15 | 0.83–1.59 | 0.7 | 0.40 | ||||
| Current use of antibiotics (yes vs. no) | 1.33 | 0.88–1.99 | 1.8 | 0.18 | ||||
| Coronary artery disease (yes vs. no) | 1.02 | 0.62–1.67 | 0.004 | 0.95 | ||||
| Multivariate Survival Analyses in Cancer Patients with ≥20 Premature Ventricular Contractions | ||||||||
| ≥20 Premature ventricular contractions/24 h (yes vs. no) | 1.71 | 1.22–2.40 | 9.7 | 0.0019 | 1.63 | 1.15–2.31 | 7.4 | 0.0064 |
| Age (per 1 year) | 1.01 | 0.9991–1.03 | 3.4 | 0.07 | 1.02 | 0.99995–1.03 | 3.8 | 0.05 |
| Sodium (per 1 mmol/L) | 0.97 | 0.92–1.008 | 2.6 | 0.11 | 0.96 | 0.92–1.008 | 2.6 | 0.11 |
| Haemoglobin (per 1 g/dL) | 0.91 | 0.83–0.989 | 4.9 | 0.027 | 0.91 | 0.83–0.991 | 4.7 | 0.031 |
| BMI (per 1 kg/m2) | 0.96 | 0.92–0.993 | 5.3 | 0.021 | 0.96 | 0.92–0.996 | 4.6 | 0.032 |
| Opioids (yes vs. no) | 1.21 | 0.80–1.84 | 0.84 | 0.36 | 1.22 | 0.79–1.86 | 0.8 | 0.37 |
| Antidepressants (yes vs. no) | 1.60 | 0.97–2.64 | 3.5 | 0.06 | 1.67 | 1.01–2.75 | 4.1 | 0.044 |
| Cancer stage (≥III vs. I/II) | 1.64 | 1.11–2.42 | 6.1 | 0.014 | 1.63 | 1.10–2.41 | 6.0 | 0.014 |
| Cancer type (solid vs. haematologic) | 2.44 | 1.74–3.43 | 26.5 | <0.0001 | 2.49 | 1.77–3.52 | 27.0 | <0.0001 |
| ECOG performance status (≥2 vs. 0/1) | 1.30 | 0.92–1.84 | 2.3 | 0.13 | 1.47 | 1.02–2.11 | 4.4 | 0.037 |
| Prior potentially cardiotoxic anti-cancer drugs (yes vs. no) | 1.53 | 1.07–2.17 | 5.5 | 0.019 | 1.54 | 1.08–2.20 | 5.6 | 0.018 |
| Sex (female vs. male) | 0.69 | 0.49–0.97 | 4.6 | 0.03 | ||||
| Potassium (per 1 mmol/L) | 1.14 | 0.83–1.57 | 0.6 | 0.42 | ||||
| Current use of antibiotics (yes vs. no) | 1.24 | 0.82–1.86 | 1.0 | 0.31 | ||||
| Coronary artery disease (yes vs. no) | 0.91 | 0.55–1.50 | 0.1 | 0.71 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Albrecht, A.; Porthun, J.; Eucker, J.; Coats, A.J.S.; von Haehling, S.; Pezzutto, A.; Karakas, M.; Riess, H.; Keller, U.; Landmesser, U.; et al. Spontaneous Non-Sustained Ventricular Tachycardia and Premature Ventricular Contractions and Their Prognostic Relevance in Patients with Cancer in Routine Care. Cancers 2021, 13, 2303. https://doi.org/10.3390/cancers13102303
Albrecht A, Porthun J, Eucker J, Coats AJS, von Haehling S, Pezzutto A, Karakas M, Riess H, Keller U, Landmesser U, et al. Spontaneous Non-Sustained Ventricular Tachycardia and Premature Ventricular Contractions and Their Prognostic Relevance in Patients with Cancer in Routine Care. Cancers. 2021; 13(10):2303. https://doi.org/10.3390/cancers13102303
Chicago/Turabian StyleAlbrecht, Annemarie, Jan Porthun, Jan Eucker, Andrew J.S. Coats, Stephan von Haehling, Antonio Pezzutto, Mahir Karakas, Hanno Riess, Ulrich Keller, Ulf Landmesser, and et al. 2021. "Spontaneous Non-Sustained Ventricular Tachycardia and Premature Ventricular Contractions and Their Prognostic Relevance in Patients with Cancer in Routine Care" Cancers 13, no. 10: 2303. https://doi.org/10.3390/cancers13102303
APA StyleAlbrecht, A., Porthun, J., Eucker, J., Coats, A. J. S., von Haehling, S., Pezzutto, A., Karakas, M., Riess, H., Keller, U., Landmesser, U., Haverkamp, W., Anker, S. D., & Anker, M. S. (2021). Spontaneous Non-Sustained Ventricular Tachycardia and Premature Ventricular Contractions and Their Prognostic Relevance in Patients with Cancer in Routine Care. Cancers, 13(10), 2303. https://doi.org/10.3390/cancers13102303










