Colorectal Cancer Survival in 50- to 69-Year-Olds after Introducing the Faecal Immunochemical Test
Abstract
1. Introduction
2. Results
2.1. Cases of CRC Diagnosed Through Population Screening (Group 1)
2.2. Cases of CRC Diagnosed in Symptomatic Patients (Groups 2 and 3)
2.3. Stage and Survival by Group
2.4. Cases of CRC in Patients with Positive FIT in Screening Who Declined Colonoscopy
2.5. Interval Cancers
3. Discussion
3.1. Main Findings
3.2. CCR in FIT-Positive Patients Who Declined Colonoscopy
3.3. Interval Cancer
3.4. Strengths and Weaknesses
3.5. Implications for Research and Practice
4. Materials and Methods
4.1. Study Population
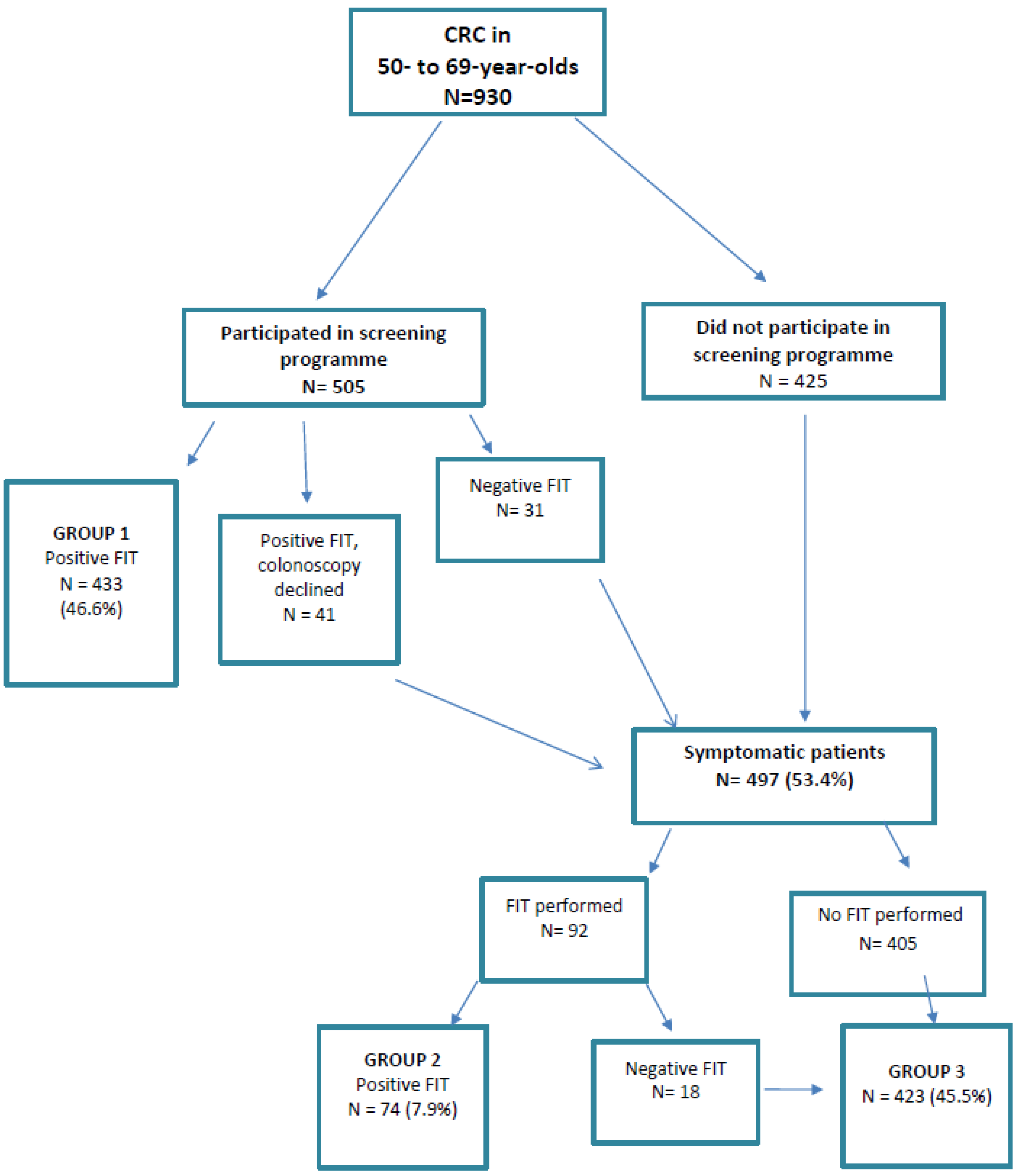
4.2. Design and Groups as a Function of Route to CRC Detection
4.3. Variables
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethics approval and consent to participate
Abbreviations
| CRC | colorectal cancer |
| FIT | faecal immunochemical test |
| f-Hb | faecal haemoglobin concentrations |
| HR | hazard ratio |
| OR | odds ratio |
| CI | confidence interval |
References
- GLOBOCAN. Global Cancer Observatory. Cancer Today [Internet]. Available online: http://gco.iarc.fr/ (accessed on 20 February 2019).
- Zorzi, M.; Fedeli, U.; Schievano, E.; Bovo, E.; Guzzinati, S.; Baracco, S.; Fedato, C.; Saugo, M.; Dei Tos, A.P. Impact on colorectal cancer mortality of screening programmes based on the faecal immunochemical test. Gut 2015, 64, 784–790. [Google Scholar] [CrossRef] [PubMed]
- Idigoras, I.; Arrospide, A.; Portillo, I.; Arana-Arri, E.; Martínez-Indart, L.; Mar, J.; de Koning, H.J.; Lastra, R.; Soto-Gordoa, M.; van der Meulen, M.; et al. Evaluation of the colorectal cancer screening Programme in the Basque Country (Spain) and its effectiveness based on the Miscan-colon model. BMC Public Health 2017, 18, 189. [Google Scholar] [CrossRef] [PubMed]
- Elmunzer, B.J.; Singal, A.G.; Sussman, J.B.; Deshpande, A.R.; Sussman, D.A.; Conte, M.L.; Dwamena, B.A.; Rogers, M.A.M.; Schoenfeld, P.S.; Inadomi, J.M.; et al. Comparing the effectiveness of competing tests for reducing colorectal cancer mortality: A network meta-analysis. Gastroint. Endosc. 2015, 81, 700–709. [Google Scholar] [CrossRef]
- Council of the European Union. Council Recommendation of 2 December 2003 on cancer screening (2003/878/EC). Off. J. Eur. Union 2003, L327, 34–38. [Google Scholar]
- Cancer Strategy of the Spanish National Health System 2009; Ministry of Health, Social Services and Equality: Madrid, Spain, 2009; Available online: https://www.mscbs.gob.es/organizacion/sns/planCalidadSNS/pdf/Cancer_Strategy_of_the_Spanish_2009pdf (accessed on 4 April 2020).
- Mansouri, D.; McMillan, D.C.; Crearie, C.; Morrison, D.S.; Crighton, E.M.; Horgan, P.G. Temporal trends in mode, site and stage of presentation with the introduction of colorectal cancer screening: A decade of experience from the West of Scotland. Br. J. Cancer 2015, 113, 556–561. [Google Scholar] [CrossRef] [PubMed]
- Morris, E.J.A.; Whitehouse, L.E.; Farrell, T.; Nickerson, C.; Thomas, J.D.; Quirke, P.; Rutter, M.D.; Rees, C.; Finan, P.J.; Wilkinson, J.R.; et al. A retrospective observational study examining the characteristics and outcomes of tumours diagnosed within and without of the English NHS Bowel Cancer Screening Programme. Br. J. Cancer 2012, 107, 757–764. [Google Scholar] [CrossRef] [PubMed]
- Pin Vieito, N.; Zarraquiños, S.; Cubiella, J. High-risk symptoms and quantitative faecal immunochemical test accuracy: Systematic review and meta-analysis. World J. Gastroenterol. 2019, 25, 2383–2401. [Google Scholar] [CrossRef]
- Westwood, M.; Lang, S.; Armstrong, N.; van Turenhout, S.; Cubiella, J.; Stirk, L.; Ramos, I.C.; Luyendijk, M.; Zaim, R.; Kleijnen, J.; et al. Faecal immunochemical tests (FIT) can help to rule out colorectal cancer in patients presenting in primary care with lower abdominal symptoms: A systematic review conducted to inform new NICE DG30 diagnostic guidance. BMC Med. 2017, 15, 189. [Google Scholar] [CrossRef]
- Katsoula, A.; Paschos, P.; Haidich, A.B.; Tsapas, A.; Giouleme, O. Diagnostic accuracy of fecal immunochemical test in patients at increased risk for colorectal cancer: A meta-analysis. JAMA Intern. Med. 2017, 177, 1110–1118. [Google Scholar] [CrossRef]
- Stonestreet, J.; Chandrapalan, S.; Woolley, D.; Uthman, U.; Arasaradnam, R.P. Systematic review and meta-analysis: Diagnostic accuracy of faecal immunochemical testing for haemoglobin (FIT) in detecting colorectal cancer for both symptomatic and screening population. Acta Gastroenterol. Belg. 2019, 82, 291–299. [Google Scholar]
- Cubiella, J.; Salve, M.; Díaz-Ondina, M.; Vega, P.; Alves, M.T.; Iglesias, F.; Sánchez, E.; Macía, P.; Blanco, I.; Bujanda, L.; et al. Diagnostic accuracy of the faecal immunochemical test for colorectal cancer in symptomatic patients: Comparison with NICE and SIGN referral criteria. Colorectal Dis. 2014, 16, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Meklin, J.; SyrjÄnen, K.; Eskelinen, M. Fecal Occult Blood Tests in Colorectal Cancer Screening: Systematic Review and Meta-analysis of Traditional and New-generation Fecal Immunochemical Tests. Anticancer Res. 2020, 40, 3591–3604. [Google Scholar] [CrossRef] [PubMed]
- Cubiella, J.; Marzo-Castillejo, M.; Mascort-Roca, J.J.; Amador-Romero, F.J.; Bellas-Beceiro, B.; Clofent-Vilaplana, J.; Carballal, S.; Ferrándiz-Santos, J.; Gimeno-García, A.Z.; Jover, R.; et al. Clinical practice guideline. Diagnosis and prevention of colorectal cancer. 2018 Update. Gastroenterol. Hepatol. 2018, 41, 585–596. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence (NICE). Quantitative Faecal Immunochemical Tests to Guide Referral for Colorectal Cancer in Primary Care. Diagnostics Guidance DG30. 2017. Available online: https://www.nice.org.uk/guidance/dg30 (accessed on 20 February 2019).
- Gutierrez-Stampa, M.A.; Aguilar, V.; Sarasqueta, C.; Cubiella, J.; Portillo, I.; Bujanda, L. Impact of the faecal immunochemical test on colorectal cancer survival. BMC Cancer 2020, 20, 616. [Google Scholar] [CrossRef] [PubMed]
- Mosquera, I.; Mendizabal, N.; Martín, U.; Bacigalupe, A.; Aldasoro, E.; Portillo, I. Inequalities in participation in colorectal cancer screening programmes: A systematic review. Eur. J. Public Health 2020, 30, 558–567. [Google Scholar] [CrossRef] [PubMed]
- Portillo, I.; Arana-Arri, E.; Gutiérrez-Ibarluzea, I.; Bilbao, I.; Luis Hurtado, J.; Sarasqueta, C.; Idigoras, I.; Bujanda, L.; Hurtado, J.L.; de No, C.; et al. Factors related to the participation and detection of lesions in colorectal cancer screening programme-based faecal immunochemical test. Eur. J. Public Health 2018, 28, 1143–1148. [Google Scholar] [CrossRef]
- Portillo, I.; Idígoras, I.; Ojembarrena, E.; Arana-Arri, E.; Zubero, M.B.; Pijoán, J.I.; López Urrutia, A.; Marqués, M.L. [Main results of the colorectal cancer screening program in the Basque Country (Spain)]. Gac. Sanit. 2013, 27, 358–361. [Google Scholar] [CrossRef][Green Version]
- Clarke, N.; Sharp, L.; Osborne, A.; Kearney, P.M. Comparison of Uptake of Colorectal Cancer Screening Based on Fecal Immunochemical Testing (FIT) in Males and Females: A Systematic Review and Meta-analysis. Cancer Epidemiol. Biomarkers Prev. 2015, 24, 39–47. [Google Scholar] [CrossRef]
- Frederiksen, B.L.; Jørgensen, T.; Brasso, K.; Holten, I.; Osler, M. Socioeconomic position and participation in colorectal cancer screening. Br. J. Cancer 2010, 103, 1496–1501. [Google Scholar] [CrossRef]
- Hurtado, J.L.; Bacigalupe, A.; Calvo, M.; Esnaola, S.; Mendizabal, N.; Portillo, I.; Idigoras, I.; Millán, E.; Arana-Arri, E. Social inequalities in a population based colorectal cancer screening programme in the Basque Country. BMC Public Health 2015, 15. [Google Scholar] [CrossRef]
- Von Wagner, C.; Baio, G.; Raine, R.; Snowball, J.; Morris, S.; Atkin, W.; Obichere, A.; Handley, G.; Logan, R.F.; Rainbow, S.; et al. Inequalities in participation in an organized national colorectal cancer screening programme: Results from the first 2.6 million invitations in England. Int. J. Epidemiol. 2011, 40, 712–718. [Google Scholar] [CrossRef] [PubMed]
- European Colorectal Cancer Screening Guidelines Working Group; von Karsa, L.; Patnick, J.; Segnan, N.; Atkin, W.; Halloran, S.; Lansdorp-Vogelaar, I.; Malila, N.; Minozzi, S.; Moss, S.; et al. European guidelines for quality assurance in colorectal cancer screening and diagnosis: Overview and introduction to the full supplement publication. Endoscopy 2013, 45, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Borowski, D.W.; Cawkwell, S.; Zaidi, S.M.A.; Toward, M.; Maguire, N.; Garg, D.K.; Gill, T.S. The NHS Bowel cancer screening programme achieves the anticipated survival improvement, but participation must be improved. Int. J. Health Care Qual. Assur. 2018, 31, 106–115. [Google Scholar] [CrossRef] [PubMed]
- Idigoras Rubio, I.; Arana-Arri, E.; Portillo Villares, I.; Bilbao Iturribarrria, I.; Martínez-Indart, L.; Imaz-Ayo, N.; de la Cruz, M.; de Castro, V.; López de Munain, A.; Torrejón Perez, I.; et al. Participation in a population-based screening for colorectal cancer using the faecal immunochemical test decreases mortality in 5 years. Eur. J. Gastroenterol. Hepatol. 2019, 31, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Chiu, H.-M.; Chen, S.L.-S.; Yen, A.M.-F.; Chiu, S.Y.-H.; Fann, J.C.-Y.; Lee, Y.-C.; Pan, S.-L.; Wu, M.-S.; Liao, C.-S.; Chen, H.-H.; et al. Effectiveness of fecal immunochemical testing in reducing colorectal cancer mortality from the One Million Taiwanese Screening Program. Cancer 2015, 121, 3221–3229. [Google Scholar] [CrossRef]
- Gini, A.; Jansen, E.E.L.; Zielonke, N.; Meester, R.G.S.; Senore, C.; Anttila, A.; Segnan, N.; Mlakar, D.N.; de Koning, H.J.; Lansdorp-Vogelaar, I.; et al. Impact of colorectal cancer screening on cancer-specific mortality in Europe: A systematic review. Eur. J. Cancer 2020. [Google Scholar] [CrossRef]
- Rossi, P.G.; Vicentini, M.; Sacchettini, C.; Di Felice, E.; Caroli, S.; Ferrari, F.; Mangone, L.; Pezzarossi, A.; Roncaglia, F.; Campari, C.; et al. Impact of Screening Program on Incidence of Colorectal Cancer: A Cohort Study in Italy. Am. J. Gastroenterol. 2015, 110, 1359–1366. [Google Scholar] [CrossRef]
- Ventura, L.; Mantellini, P.; Grazzini, G.; Castiglione, G.; Buzzoni, C.; Rubeca, T.; Sacchettini, C.; Paci, E.; Zappa, M. The impact of immunochemical faecal occult blood testing on colorectal cancer incidence. Dig. Liver Dis. 2014, 46, 82–86. [Google Scholar] [CrossRef]
- Parente, F.; Vailati, C.; Boemo, C.; Bonoldi, E.; Ardizzoia, A.; Ilardo, A.; Tortorella, F.; Cereda, D.; Cremaschini, M.; Moretti, R. Improved 5-year survival of patients with immunochemical faecal blood test-screen-detected colorectal cancer versus non-screening cancers in northern Italy. Dig. Liver Dis. 2015, 47, 68–72. [Google Scholar] [CrossRef]
- Van der Vlugt, M.; Grobbee, E.J.; Bossuyt, P.M.M.; Bos, A.; Bongers, E.; Spijker, W.; Kuipers, E.J.; Lansdorp-Vogelaar, I.; Spaander, M.C.W.; Dekker, E. Interval Colorectal Cancer Incidence Among Subjects Undergoing Multiple Rounds of Fecal Immunochemical Testing. Gastroenterology 2017, 153, 439–447. [Google Scholar] [CrossRef]
- Gill, M.D.; Bramble, M.G.; Hull, M.A.; Mills, S.J.; Morris, E.; Bradburn, D.M.; Bury, Y.; Parker, C.E.; Lee, T.J.W.; Rees, C.J. Screen-detected colorectal cancers are associated with an improved outcome compared with stage-matched interval cancers. Br. J. Cancer 2014, 111, 2076–2081. [Google Scholar] [CrossRef] [PubMed]
- Domènech, X.; Garcia, M.; Benito, L.; Binefa, G.; Vidal, C.; Milà, N.; Moreno, V. Cánceres de intervalo y sensibilidad de los programas poblacionales de cribado de cáncer colorrectal. Gac Sanit. 2015, 29, 464–471. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gingold-Belfer, R.; Leibovitzh, H.; Boltin, D.; Issa, N.; Tsadok Perets, T.; Dickman, R.; Niv, Y. The compliance rate for the second diagnostic evaluation after a positive fecal occult blood test: A systematic review and meta-analysis. United Eur. Gastroenterol. J. 2019, 7, 424–448. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-C.; Fann, J.C.-Y.; Chiang, T.-H.; Chuang, S.-L.; Chen, S.L.-S.; Chiu, H.-M.; Yen, A.M.-F.; Chiu, S.Y.-H.; Hsu, C.-Y.; Hsu, W.-F.; et al. Time to Colonoscopy and Risk of Colorectal Cancer in Patients With Positive Results From Fecal Immunochemical Tests. Clin. Gastroenterol. Hepatol. 2019, 17, 1332–1340. [Google Scholar] [CrossRef]
- Corley, D.A.; Jensen, C.D.; Quinn, V.P.; Doubeni, C.A.; Zauber, A.G.; Lee, J.K.; Schottinger, J.E.; Marks, A.R.; Zhao, W.K.; Ghai, N.R.; et al. Association Between Time to Colonoscopy After a Positive Fecal Test Result and Risk of Colorectal Cancer and Cancer Stage at Diagnosis. JAMA 2017, 317, 1631. [Google Scholar] [CrossRef]
- Meester, R.G.S.; Zauber, A.G.; Doubeni, C.A.; Jensen, C.D.; Quinn, V.P.; Helfand, M.; Dominitz, J.A.; Levin, T.R.; Corley, D.A.; Lansdorp-Vogelaar, I. Consequences of Increasing Time to Colonoscopy Examination After Positive Result From Fecal Colorectal Cancer Screening Test. Clin. Gastroenterol. Hepatol. 2016, 14, 1445–1451. [Google Scholar] [CrossRef]
- Benedict, M.; Galvao Neto, A.; Zhang, X. Interval colorectal carcinoma: An unsolved debate. World J. Gastroenterol. 2015, 21, 12735–12741. [Google Scholar] [CrossRef]
- Brierley, J.D.; Gospodarowicz, M.K.; Wittekind, C. (Eds.) TNM Classification of Malignant Tumours, 8th ed.; Wiley-Blackwell: West Sussex, UK, 2017. [Google Scholar]
| Variables | 930 Patients n (%) |
|---|---|
| Mean age, years (SD) | 61.93 (SD 5.2) |
| SEX | |
| Man | 575 (61.8) |
| Woman | 355 (38.2) |
| SITE * | |
| Rectum | 213 (22.9) |
| Distal colon | 450 (48.4) |
| Proximal colon | 255 (27.4) |
| Colon (not specified further) | 12 (1.3) |
| HISTOLOGY | |
| Adenocarcinoma | 893 (96.0) |
| Mucinous adenocarcinoma | 25 (2.7) |
| Other ** | 12 (1.3) |
| ROUTE TO DIAGNOSIS | |
| Group 1 | 433 (46.5) |
| Group 2 | 74 (8.0) |
| Group 3 | 423 (45.5) |
| STAGE | |
| Stage I | 309 (33.2) |
| Stage II | 248 (26.7) |
| Stage III | 210 (22.6) |
| Stage IV | 162 (17.4) |
| Unknown | 1 (0.1) |
| Variables | Group 1 | Group 2 | Group 3 | p |
|---|---|---|---|---|
| n = 433 | n = 74 | n = 423 | ||
| n (%) | n (%) | n (%) | ||
| AGE, years (SD) | 61.8 (SD 5.3) | 61.2 (SD 5.4) | 62.1 (SD 5.1) | 0.28 |
| SEX | ||||
| (% MEN) | 264 (60.9) | 48 (64.8) | 263 (62.2) | 0.8 |
| SITE * | ||||
| Rectum | 79 (18.2) | 21 (28.4) | 113 (26.7) | |
| Distal | 235 (54.3) | 28 (37.8) | 187 (44.2) | Group1/group2: 0.05 |
| Proximal | 116 (26.8) | 24 (32.4) | 115 (27.2) | Group2/group3: 0.71 |
| Colon (not specified further) | 3 (0.7) | 1 (1.4) | 8 (1.9) | Group1/group3: 0.003 |
| HISTOLOGY | ||||
| Adenocarcinoma | 423 (97.7) | 71 (95.9) | 399 (94.3) | Group1/group2: 0.03 |
| Mucinous adenocarcinoma | 9 (2.1) | 1 (1.4) | 15 (3.6) | Group2/group3: 0.6 |
| Others ** | 1 (0.2) | 2 (2.7) | 9 (2.1) | Group1/group3: 0.01 |
| STAGE | ||||
| Stage I | 217 (50.1) | 18 (24.3) | 74 (17.5) | Group1/group2: < 0.0005 |
| Stage II | 93 (21.5) | 21 (28.4) | 134 (31.7) | Group2/group3: 0.46 |
| Stage III | 91 (21.0) | 19 (25.7) | 100 (23.7) | Group1/group3 < 0.0005 |
| Stage IV | 32 (7.4) | 16 (21.6) | 114 (26.9) | |
| Unknown | - | - | 1 (0.2) | |
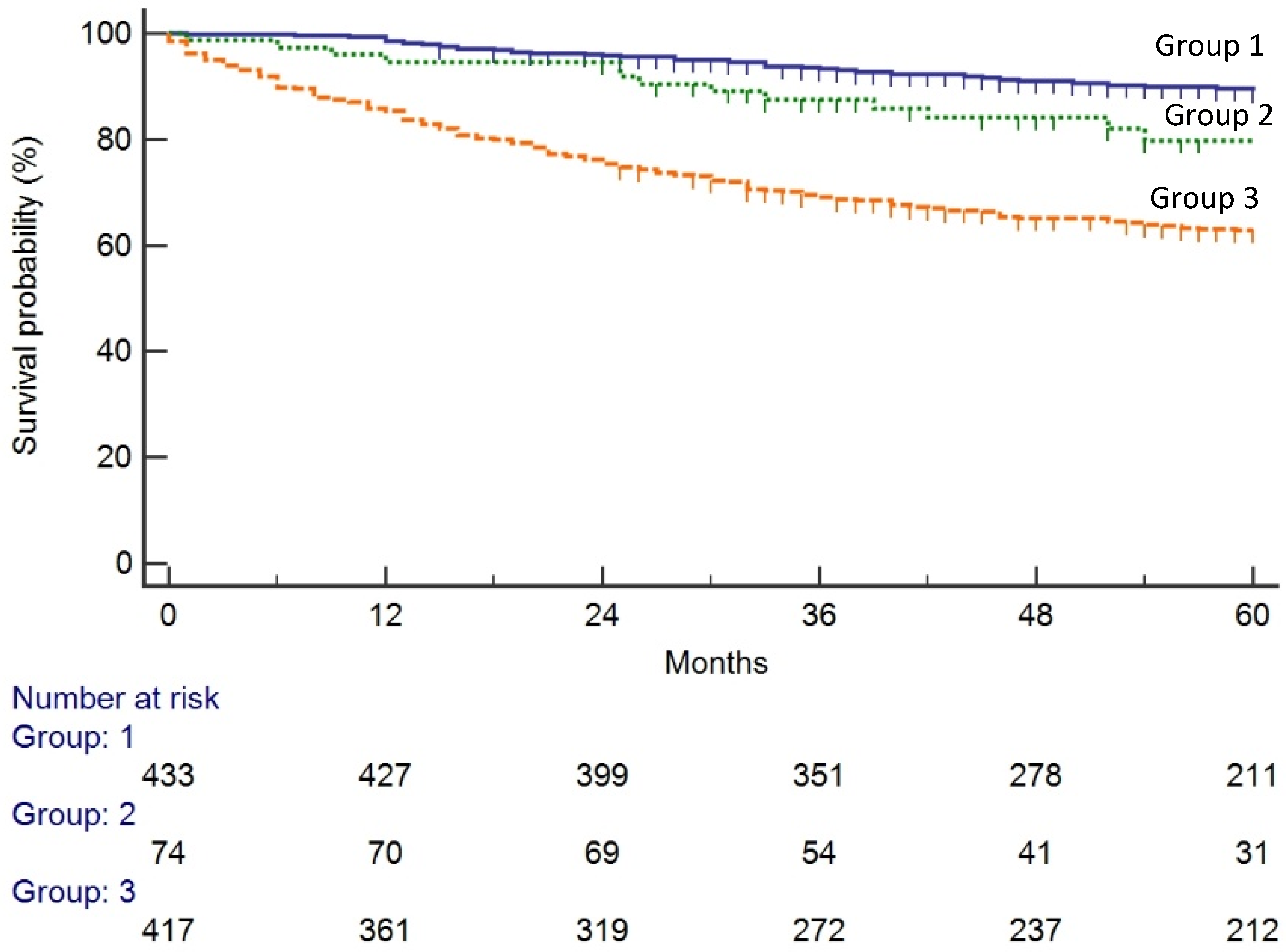
| 3-year survival | 93.0% | 87.5% | 69.5% | Group1/group2: 0.02 Group2/group3: 0.007 Group1/group3 < 0.0005 |
| 5-year survival | 89% | 77% | 63% | Group1/group2: 0.02 Group2/group3: 0.007 Group1/group3 < 0.0005 |
| Variables | UNIVARIATE ANALYSIS | MULTIVARIATE ANALYSIS | ||||
|---|---|---|---|---|---|---|
| HR * | 95% CI ** | p | HR * | 95% CI ** | p | |
| GROUPS | ||||||
| Group 3 | 1 | 1 | ||||
| Group 1 | 0.26 | 0.19–0.36 | 0.0005 | 0.42 | 0.30–0.58 | 0.0005 |
| Group 2 | 0.51 | 0.3–0.85 | 0.009 | 0.51 | 0.29–0.87 | 0.01 |
| AGE, years | 1.03 | 1.007–1.06 | 0.01 | 1.04 | 1.009–1.06 | 0.009 |
| SEX | ||||||
| Men | 1 | |||||
| Women | 0.88 | 0.67–1.15 | 0.35 | |||
| SITES | ||||||
| Rectum | 1 | 1 | ||||
| Distal | 0.72 | 0.52–0.99 | 0.04 | 0.95 | 0.68–1.31 | 0.73 |
| Proximal | 0.92 | 0.65–1.3 | 0.65 | 1.22 | 0.86–1.73 | 0.27 |
| HISTOLOGY | ||||||
| Adenocarcinoma | 1 | |||||
| Mucinous adenocarcinoma | 1.48 | 0.76–2.86 | 0.25 | |||
| Other *** | 1.42 | 0.53–81 | 0.49 | |||
| STAGE | ||||||
| Stage I | 1 | 1 | ||||
| Stage II | 1.72 | 1.03–2.87 | 0.004 | 1.33 | 0.78–2.26 | 0.29 |
| Stage III | 3.43 | 2.14–5.51 | 0.0005 | 2.71 | 1.66–4.42 | 0.0005 |
| Stage IV | 19.07 | 12.35–19.45 | 0.0005 | 14.32 | 9.03–22.78 | 0.0005 |
| Variables | Group 1 | FIT-Positive Patients Who Declined Colonoscopy | Interval Cancer | p |
|---|---|---|---|---|
| n = 433 | n = 41 | n = 31 | ||
| n (%) | n (%) | n (%) | ||
| Age, years | 61.8 (SD 5.3) | 62.5 (SD 4.8) | 63.6 (SD 4.3) | 0.1 |
| SEX | ||||
| (% MEN) | 264 (60.9) | 24 (58.5) | 14 (45.2) | 0.22 |
| SITE | ||||
| Rectum | 79 (18.2) | 14 (34.1) | 9 (29.0) | |
| Distal | 235 (54.3) | 10 (24.4) | 10 (32.3) | |
| Proximal | 116 (26.8) | 16 (39.1) | 12 (38.7) | 0.001 |
| Colon (not specified further) | 3 (0.7) | 1 (2.4) | - | |
| HISTOLOGY | ||||
| Adenocarcinoma | 423 (97.7) | 39 (95.1) | 26 (83.9) | |
| Mucinous adenocarcinoma | 9 (2.1) | 2 (4.9) | 3 (9.7) | |
| Other ** | 1 (0.2) | 2 (6.4) | 0.0005 | |
| STAGE | ||||
| Stage I | 217 (50.1) | 10 (24.4) | 6 (19.3) | |
| Stage II | 93 (21.5) | 10 (24.4) | 8 (25.8) | |
| Stage III | 91 (21.0) | 11 (26.8) | 8 (25.8) | |
| Stage IV | 32 (7.4) | 10 (24.4) | 9 (29.1) | 0.0005 |
| 3-year survival | 93.5% | 75.6% | 74.2% | 0.0005 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gutierrez-Stampa, M.A.; Aguilar, V.; Sarasqueta, C.; Cubiella, J.; Portillo, I.; Bujanda, L. Colorectal Cancer Survival in 50- to 69-Year-Olds after Introducing the Faecal Immunochemical Test. Cancers 2020, 12, 2412. https://doi.org/10.3390/cancers12092412
Gutierrez-Stampa MA, Aguilar V, Sarasqueta C, Cubiella J, Portillo I, Bujanda L. Colorectal Cancer Survival in 50- to 69-Year-Olds after Introducing the Faecal Immunochemical Test. Cancers. 2020; 12(9):2412. https://doi.org/10.3390/cancers12092412
Chicago/Turabian StyleGutierrez-Stampa, María Angeles, Vanessa Aguilar, Cristina Sarasqueta, Joaquín Cubiella, Isabel Portillo, and Luis Bujanda. 2020. "Colorectal Cancer Survival in 50- to 69-Year-Olds after Introducing the Faecal Immunochemical Test" Cancers 12, no. 9: 2412. https://doi.org/10.3390/cancers12092412
APA StyleGutierrez-Stampa, M. A., Aguilar, V., Sarasqueta, C., Cubiella, J., Portillo, I., & Bujanda, L. (2020). Colorectal Cancer Survival in 50- to 69-Year-Olds after Introducing the Faecal Immunochemical Test. Cancers, 12(9), 2412. https://doi.org/10.3390/cancers12092412







