Impact of Vasectomy on the Development and Progression of Prostate Cancer: Preclinical Evidence
Abstract
1. Introduction
2. Results
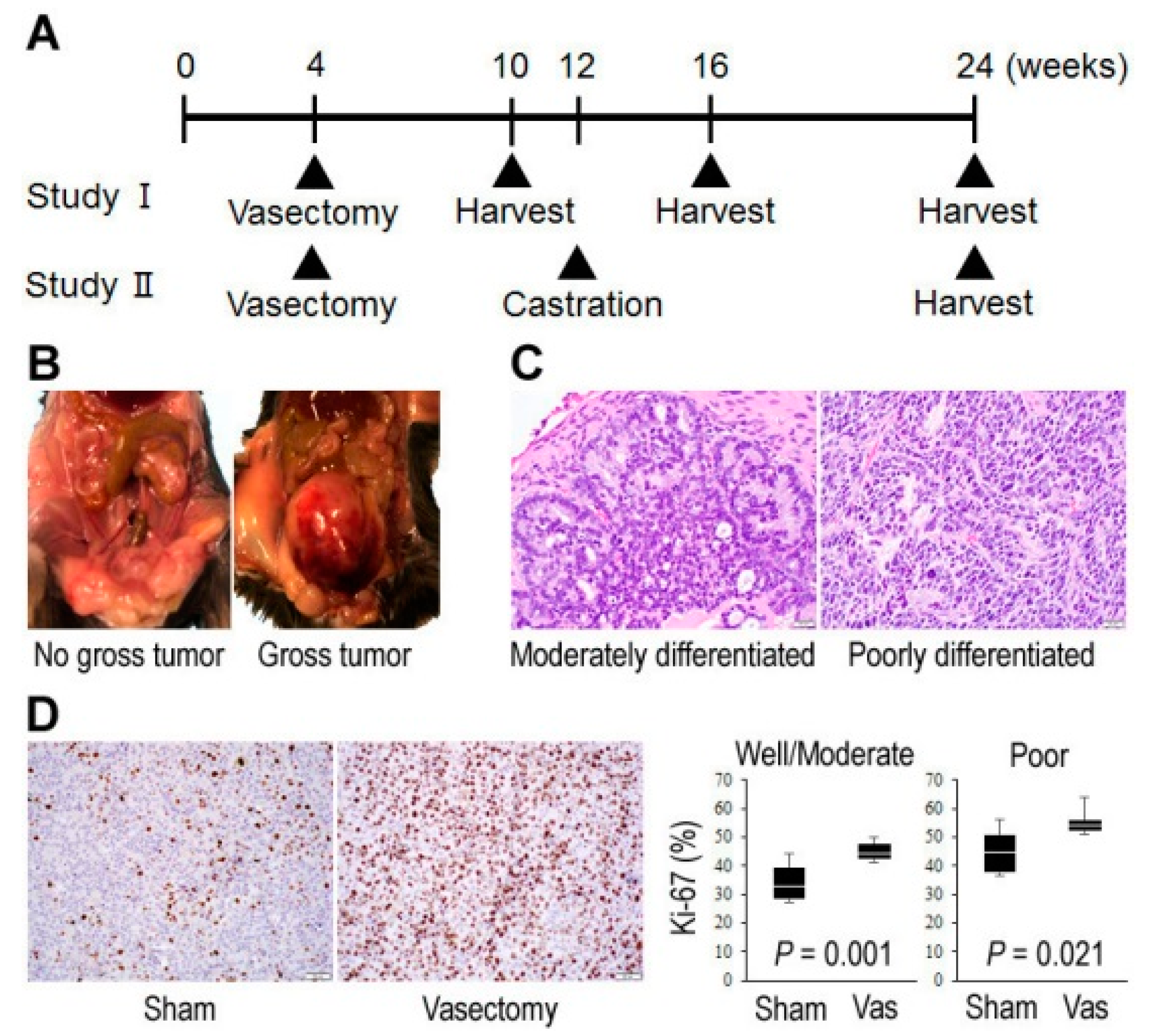
2.1. Vasectomy in TRAMP Mice
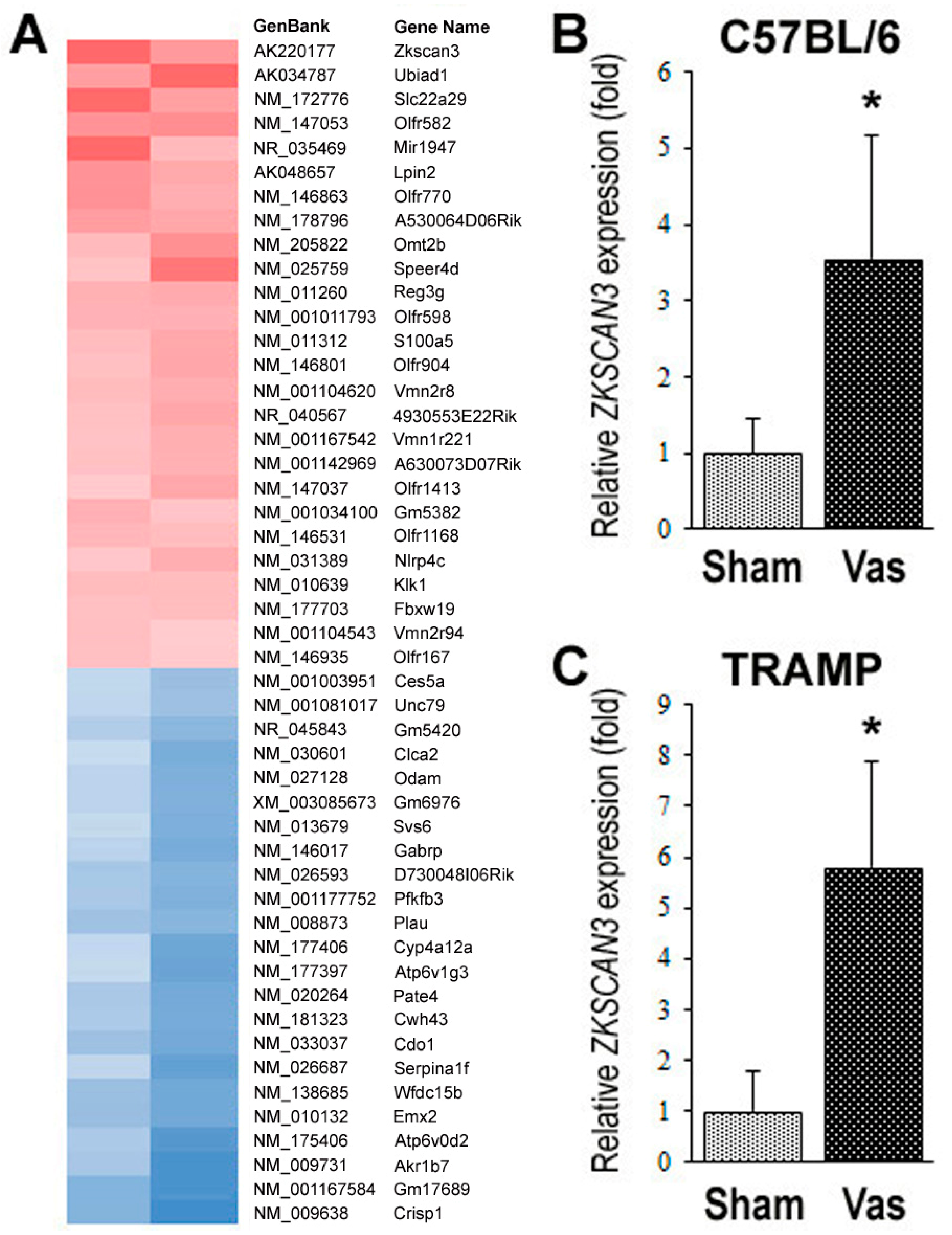
2.2. Identification of ZKSCAN3 as a Molecule whose Expression is Significantly Up-Regulated by Vasectomy
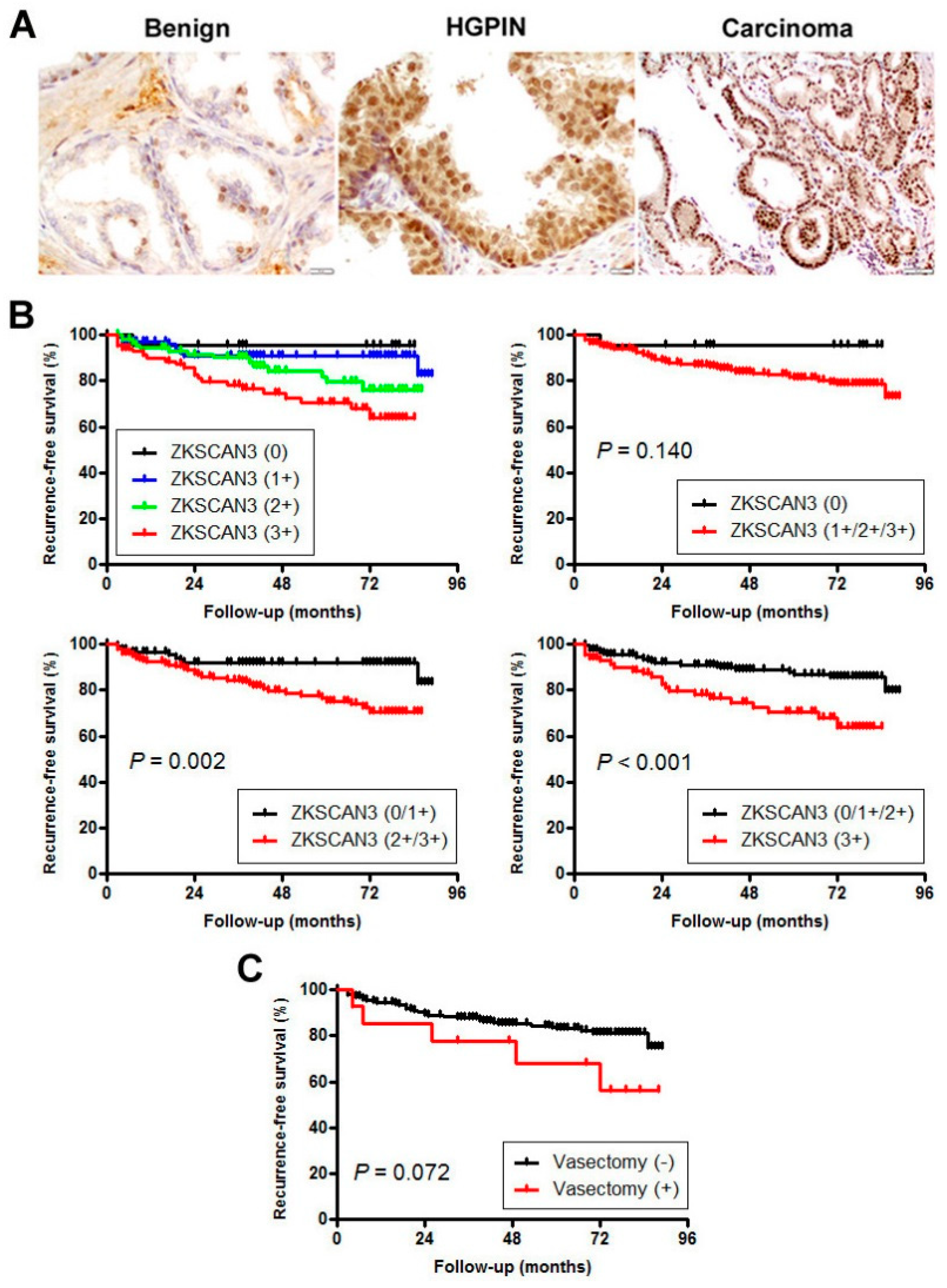
2.3. Expression of ZKSCAN3 in Prostate Cancer Specimens
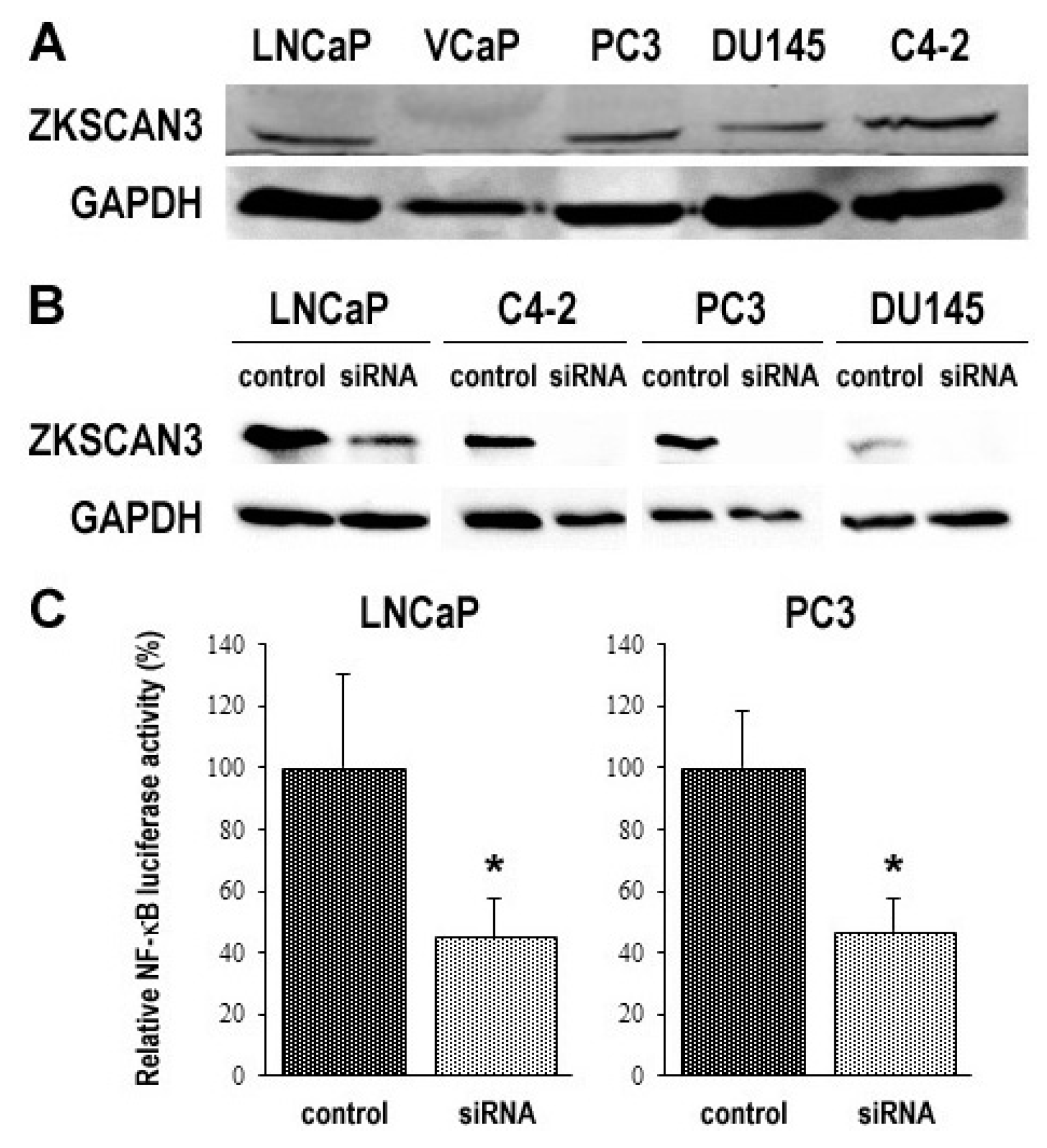
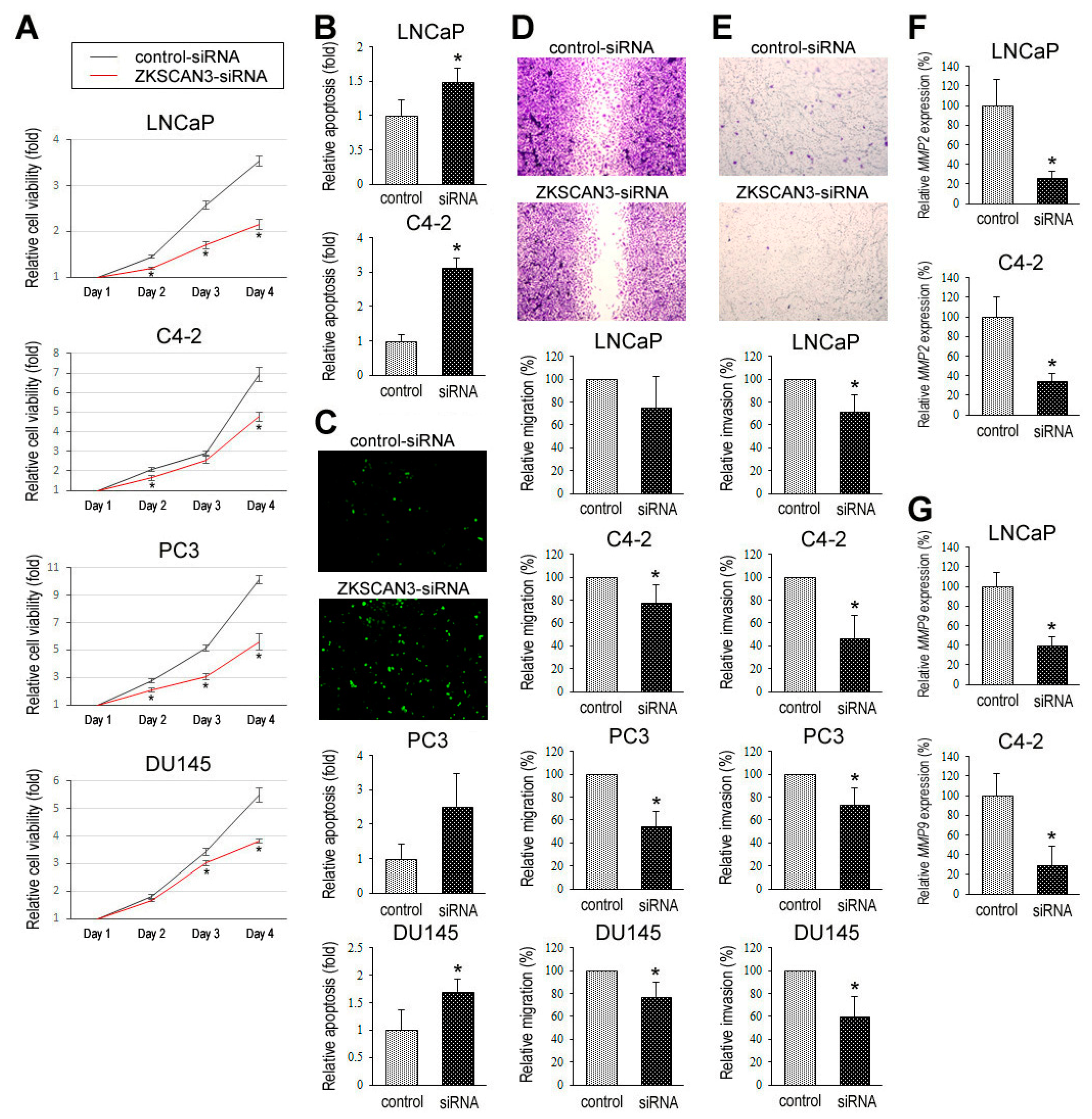
2.4. ZKSCAN3 Expression in Prostate Cancer Lines and Its Silencing Effect on Cell Growth
3. Discussion
4. Materials and Methods
4.1. Animals
4.2. Prostate TMA
4.3. Cell Lines
4.4. Immunohistochemistry
4.5. DNA Microarray
4.6. Real-Time PCR
4.7. Western Blotting
4.8. Reporter Gene Assay
4.9. Cell Proliferation
4.10. Clonogenic Assay
4.11. Apoptosis
4.12. Cell Migration
4.13. Cell Invasion
4.14. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Eisenberg, M.L.; Lipshultz, L.I. Estimating the number of vasectomies performed annually in the United States: Data from the National Survey of Family Growth. J. Urol. 2010, 184, 2068–2072. [Google Scholar] [CrossRef] [PubMed]
- Mosher, W.D.; Jones, J. Use of contraception in the United States: 1982-2008. National Center for Health Statistics. Vital Health Stat. 2010, 23, 1–44. [Google Scholar]
- Richter, S.; Embon, O.; Saghi, N.; Bechar, L. Vasectomy to prevent acute epididymo-orchitis after prostatic adenomectomy: Still a controversy. Urol. Int. 1984, 39, 283–285. [Google Scholar] [CrossRef] [PubMed]
- Honda, G.D.; Bernstein, L.; Ross, R.K.; Greenland, S.; Gerkins, V.; Henderson, B.E. Vasectomy, cigarette smoking, and age at first sexual intercourse as risk factors for prostate cancer in middle-aged men. Br. J. Cancer 1988, 57, 326–331. [Google Scholar] [CrossRef] [PubMed]
- Mettlin, C.; Natarajan, N.; Huben, R. Vasectomy and prostate cancer risk. Am. J. Epidemiol. 1990, 132, 1056–1061. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, L.; Palmer, J.R.; Zauber, A.G.; Warshauer, M.E.; Stolley, P.D.; Shapiro, S. Vasectomy and the risk of prostate cancer. Am. J. Epidemiol. 1990, 132, 1051–1055. [Google Scholar] [CrossRef]
- Sidney, S.; Quesenberry, C.P., Jr.; Sadler, M.C.; Guess, H.A.; Lydick, E.G.; Cattolica, E.V. Vasectomy and the risk of prostate cancer in a cohort of multiphasic health-checkup examinees: Second report. Cancer Causes Control 1991, 2, 113–116. [Google Scholar] [CrossRef]
- Giovannucci, E.; Tosteson, T.D.; Speizer, F.E.; Ascherio, A.; Vessey, M.P.; Colditz, G.A. A retrospective cohort study of vasectomy and prostate cancer in US men. JAMA 1993, 269, 878–882. [Google Scholar] [CrossRef]
- Giovannucci, E.; Ascherio, A.; Rimm, E.B.; Colditz, G.A.; Stampfer, M.J.; Willett, W.C. A prospective cohort study of vasectomy and prostate cancer in US men. JAMA 1993, 269, 873–877. [Google Scholar] [CrossRef]
- Hayes, R.B.; Pottern, L.M.; Greenberg, R.; Schoenberg, J.; Swanson, G.M.; Liff, J.; Schwartz, A.G.; Brown, L.M.; Hoover, R.N. Vasectomy and prostate cancer in US Blacks and Whites. Am. J. Epidemiol. 1993, 137, 263–269. [Google Scholar] [CrossRef]
- Rosenberg, L.; Palmer, J.R.; Zauber, A.G.; Warshauer, M.E.; Strom, B.L.; Hartap, S.; Shapiro, S. The relation of vasectomy to the risk of cancer. Am. J. Epidemiol. 1994, 140, 431–438. [Google Scholar] [CrossRef] [PubMed]
- John, E.M.; Whittemore, A.S.; Wu, A.H.; Kolonel, L.N.; Hislop, T.G.; Howe, G.R.; West, D.W.; Hankin, J.; Dreon, D.M.; Teh, C.-Z.; et al. Vasectomy and prostate cancer: Results from a multiethnic case-control study. J. Natl. Cancer Inst. 1995, 87, 662–669. [Google Scholar] [CrossRef] [PubMed]
- Zhhhu, K.; Stanford, J.L.; Daling, J.R.; McKnight, B.; Stergachis, A.; Brawer, M.K.; Weiss, N.S. Vasectomy and prostate cancer: A case-control study in a health maintenance organization. Am. J. Epidemiol. 1996, 144, 717–722. [Google Scholar] [CrossRef] [PubMed]
- Lesko, S.M.; Louik, C.; Vezina, R.; Rosenberg, L.; Shapiro, S. Vasectomy and prostate cancer. J. Urol. 1999, 161, 1848–1853. [Google Scholar] [CrossRef]
- Stanford, J.L.; Wicklund, K.G.; McKnight, B.; Daling, J.R.; Brawer, M.K. Vasectomy and risk of prostate cancer. Cancer Epidemiol. Biomark. Prev. 1999, 8, 881–886. [Google Scholar]
- Rohrmann, S.; Paltoo, D.N.; Platz, E.A.; Hoffman, S.C.; Comstock, G.W.; Helzlsouer, K.J. Association of vasectomy and prostate cancer among men in a Maryland cohort. Cancer Causes Control 2005, 16, 1189–1192. [Google Scholar] [CrossRef]
- Holt, S.K.; Salinas, C.A.; Stanford, J.L. Vasectomy and the risk of prostate cancer. J. Urol. 2008, 180, 2565–2568. [Google Scholar] [CrossRef]
- Weinmann, S.; Shapiro, J.A.; Rybicki, B.A.; Enger, S.M.; Van Den Eeden, S.K.; Richert-Boe, K.E.; Weiss, N.S. Medical history, body size, and cigarette smoking in relation to fatal prostate cancer. Cancer Causes Control 2010, 21, 117–125. [Google Scholar] [CrossRef]
- Siddiqui, M.M.; Wilson, K.M.; Epstein, M.M.; Rider, J.R.; Martin, N.E.; Stampfer, M.J.; Giovannucci, E.L.; Mucci, L.A. Vasectomy and risk of aggressive prostate cancer: A 24-year follow-up study. J. Clin. Oncol. 2014, 32, 3033–3038. [Google Scholar] [CrossRef]
- Jacobs, E.J.; Anderson, R.L.; Stevens, V.L.; Newton, C.C.; Gansler, T.; Gapstur, S.M. Vasectomy and prostate cancer incidence and mortality in a large US cohort. J. Clin. Oncol. 2016, 34, 3880–3885. [Google Scholar] [CrossRef]
- Shoag, J.; Savenkov, O.; Christos, P.J.; Mittal, S.; Halpern, J.A.; Askin, G.; Shoag, D.; Golan, R.; Lee, D.J.; O’Malley, P.; et al. Vasectomy and risk of prostate cancer in a screening trial. Cancer Epidemiol. Biomark. Prev. 2017, 26, 1653–1659. [Google Scholar] [CrossRef] [PubMed]
- Daaavenport, M.T.; Zhang, C.A.; Leppert, J.T.; Brooks, J.D.; Eisenberg, M.L. Vasectomy and the risk of prostate cancer in a prospective US cohort: Data from the NIH-AARP Diet and Health Study. Andrology 2019, 7, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Dennis, L.K.; Dawson, D.V.; Resnick, M.I. Vasectomy and the risk of prostate cancer: A meta-analysis examining vasectomy status, age at vasectomy, and time since vasectomy. Prostate Cancer Prostatic Dis. 2002, 5, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Shang, Y.; Han, G.; Li, J.; Zhao, J.; Cui, D.; Liu, C.; Yi, S. Vasectomy and prostate cancer risk: A meta-analysis of cohort studies. Sci. Rep. 2015, 5, 9920. [Google Scholar] [CrossRef]
- Bhindi, B.; Wallis, C.J.D.; Nayan, M.; Farrell, A.M.; Trost, L.W.; Hamilton, R.J.; Kulkarni, G.S.; Finelli, A.; Fleshner, N.E.; Boorjian, S.A.; et al. The association between vasectomy and prostate cancer: A systematic review and meta-analysis. JAMA Intern. Med. 2017, 177, 1273–1286. [Google Scholar] [CrossRef]
- van Leeuwen, P.J.; van den Bergh, R.C.N.; Wolters, T.; Zhu, X.; Bul, M.; Schröder, F.H.; Bangma, C.H.; Roobol, M.J. Critical assessment of prebiopsy parameters for predicting prostate cancer metastasis and mortality. Can. J. Urol. 2011, 18, 6018–6024. [Google Scholar]
- Canacci, A.M.; Izumi, K.; Zheng, Y.; Gordetsky, J.; Yao, J.L.; Miyamoto, H. Expression of semenogelins I and II and its prognostic significance in human prostate cancer. Prostate 2011, 71, 1108–1114. [Google Scholar] [CrossRef]
- Izumi, K.; Li, Y.; Zheng, Y.; Gordetsky, J.; Yao, J.L.; Miyamoto, H. Seminal plasma proteins in prostatic carcinoma: Increased nuclear semenogelin I expression is a predictor of biochemical recurrence after radical prostatectomy. Hum. Pathol. 2012, 43, 1991–2000. [Google Scholar] [CrossRef]
- Ishiguro, H.; Izumi, K.; Kashiwagi, E.; Zheng, Y.; Li, Y.; Kawahara, T.; Miyamoto, H. Semenogelin I promotes prostate cancer cell growth via functioning as an androgen receptor coactivator and protecting against zinc cytotoxicity. Am. J. Cancer Res. 2015, 5, 738–747. [Google Scholar] [CrossRef]
- Li, P.; Chen, J.; Kashiwagi, E.; Mizushima, T.; Han, B.; Inoue, S.; Ide, H.; Izumi, K.; Miyamoto, H. The interaction between androgen receptor and semenogelin I: A synthetic peptide antagonist inhibits the growth of prostate cancer cells. Br. J. Cancer 2018, 118, 416–420. [Google Scholar] [CrossRef]
- Kaplan-Lefko, P.J.; Chen, T.M.; Ittmann, M.M.; Barrios, R.J.; Ayala, G.E.; Huss, W.J.; Maddison, L.A.; Foster, B.A.; Greenberg, N.M. Pathobiology of autochthonous prostate cancer in a pre-clinical transgenic mouse model. Prostate 2003, 55, 219–237. [Google Scholar] [CrossRef] [PubMed]
- Berquin, I.M.; Min, Y.; Wu, R.; Wu, H.; Chen, Y.Q. Expression signature of the mouse prostate. J. Biol. Chem. 2005, 280, 36442–36451. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Zhang, L.; Wu, Q.; Boyd, D.D. Unbiased screening for transcriptional targets of ZKSCAN3 identifies integrin β4 and vascular endothelial growth factor as downstream targets. J. Biol. Chem. 2008, 283, 35295–35304. [Google Scholar] [CrossRef] [PubMed]
- Anderson, D.J.; Alexander, N.J.; Fulgham, D.L.; Palotay, J.L. Spontaneous tumors in long-term–vasectomized mice. Increased incidence and association with antisperm immunity. Am. J. Pathol. 1983, 111, 129–139. [Google Scholar]
- Bettencourt, M.C.; Bauer, J.J.; Sesterhenn, I.A.; Mostofi, F.K.; McLeod, D.G.; Moul, J.W. Ki-67 expression is a prognostic marker of prostate cancer recurrence after radical prostatectomy. J. Urol. 1996, 156, 1064–1068. [Google Scholar] [CrossRef]
- Pollack, A.; DeSilvio, M.; Khor, L.Y.; Li, R.; Al-Saleem, T.I.; Hammond, M.E.; Venkatesan, V.; Lawton, C.A.; Roach, M., III; Shipley, W.U.; et al. Ki-67 staining is a strong predictor of distant metastasis and mortality for men with prostate cancer treated with radiotherapy plus androgen deprivation: Radiation Therapy Oncology Group Trial 92-02. J. Clin. Oncol. 2004, 22, 2133–2140. [Google Scholar] [CrossRef]
- Isaacs, J.T. Prostatic structure and function in relation to the etiology of prostatic cancer. Prostate 1983, 4, 351–366. [Google Scholar] [CrossRef]
- Jakobsen, H.; Torp-Pederson, S.; Juul, N.; Hald, T. The long-term influence of vasectomy on prostatic volume and morphology in man. Prostate 1988, 13, 57–67. [Google Scholar] [CrossRef]
- Mo, Z.N.; Huang, X.; Zhang, S.C.; Yang, J.R. Early and late long-term effects of vasectomy on serum testosterone, dihydrotestosterone, luteinizing hormone and follicle-stimulating hormone levels. J. Urol. 1995, 154, 2065–2069. [Google Scholar] [CrossRef]
- Jarow, J.P.; Goluboff, E.T.; Chang, T.S.; Marshall, F.F. Relationship between antisperm antibodies and testicular histologic changes in humans after vasectomy. Urology 1994, 43, 521–524. [Google Scholar] [CrossRef]
- Ovesen, P.; Flyvbjerg, A.; Orskov, H. Insulin-like growth factor I (IGF-I) and IGF binding proteins in seminal plasma before and after vasectomy in normal men. Fertil. Steril. 1995, 63, 913–918. [Google Scholar] [CrossRef]
- Zhang, X.; Jingm, Y.; Qin, Y.; Hunsucker, S.; Meng, H.; Sui, J.; Jiang, Y.; Gao, L.; An, G.; Yang, N.; et al. The zinc finger transcription factor ZKSCAN3 promotes prostate cancer cell migration. Int. J. Biochem. Cell Biol. 2012, 44, 1166–1173. [Google Scholar] [CrossRef]
- Kawahara, T.; Inoue, S.; Ide, H.; Kashiwagi, E.; Ohtake, S.; Mizushima, T.; Li, P.; Li, Y.; Zheng, Y.; Uemura, H.; et al. ZKSCAN3 promotes bladder cancer cell proliferation, migration, and invasion. Oncotarget 2016, 7, 53599–53610. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Hamilton, S.R.; Sood, A.; Kuwai, T.; Ellis, L.; Sanguino, A.; Lopez-Berestein, G.; Boyd, D.D. The previously undescribed ZKSCAN3 (ZNF306) is a novel “driver” of colorectal cancer progression. Cancer Res. 2008, 68, 4321–4330. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Wang, H.; Kornblau, S.M.; Graber, D.A.; Zhang, N.; Matthews, J.A.; Wang, M.; Weber, D.M.; Thomas, S.K.; Shah, J.J.; et al. Evidence of a role for the novel zinc-finger transcription factor ZKSCAN3 in modulating Cyclin D2 expression in multiple myeloma. Oncogene 2011, 30, 1329–1340. [Google Scholar] [CrossRef]
- Chi, Y.; Xu, H.; Wang, F.; Chen, X.; Shan, Z.; Sun, Y.; Fan, Q. ZKSCAN3 promotes breast cancer cell proliferation, migration and invasion. Biochem. Biophys. Res. Commun. 2018, 503, 2583–2589. [Google Scholar] [CrossRef]
- Kawahara, T.; Kashiwagi, E.; Ide, H.; Li, Y.; Zheng, Y.; Ishiguro, H.; Miyamoto, H. The role of NFATc1 in prostate cancer progression: Cyclosporine A and tacrolimus inhibit cell proliferation, migration, and invasion. Prostate 2015, 75, 573–584. [Google Scholar] [CrossRef]
- Kawahara, T.; Aljarah, A.K.; Shareef, H.K.; Inoue, S.; Ide, H.; Patterson, J.D.; Kashiwagi, E.; Han, B.; Li, Y.; Zheng, Y.; et al. Silodosin inhibits prostate cancer cell growth via ELK1 inactivation and enhances the cytotoxic activity of gemcitabine. Prostate 2016, 76, 744–756. [Google Scholar] [CrossRef]
- Inoue, S.; Ide, H.; Mizushima, T.; Jiang, G.; Netto, G.J.; Gotoh, M.; Miyamoto, H. Nuclear factor-κB promotes urothelial tumorigenesis and cancer progression via cooperation with androgen receptor signaling. Mol. Cancer Ther. 2018, 17, 1303–1314. [Google Scholar] [CrossRef]
| 10 Weeks | 16 Weeks | 24 Weeks | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Sham (n = 15) | Vasectomy (n = 15) | p | Sham (n = 12) | Vasectomy (n = 12) | p | Sham (n = 12) | Vasectomy (n = 12) | p | |
| Gross tumor | 0 (0%) | 0 (0%) | 1.000 | 0 (0%) | 2 (17%) | 0.478 | 2 (17%) | 7 (58%) | 0.089 |
| Carcinoma | 9 (60%) | 7 (47%) | 0.715 | 8 (67%) | 7 (58%) | 1.000 | 12 (100%) | 12 (100%) | 1.000 |
| Well/moderately differentiated | 9 (60%) | 7 (47%) | 0.715 | 8 (67%) | 7 (58%) | 1.000 | 10 (83%) | 4 (33%) | 0.036 |
| Poorly differentiated | 0 (0%) | 0 (0%) | 1.000 | 0 (0%) | 0 (0%) | 1.000 | 2 (17%) | 8 (67%) | 0.036 |
| Metastasis | 0 (0%) | 0 (0%) | 1.000 | 0 (0%) | 0 (0%) | 1.000 | 2 (17%) | 4 (33%) | 0.640 |
| n | Levels of ZKSCAN3 Expression | p | IHC Score (mean ± SD) | p (t-Test) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1+ | 2+ | 3+ | 1+/2+/3+ | 0 vs. 1+/2+/3+ | 0/1+ vs. 2+/3+ | 0/1+/2+ vs. 3+ | ||||
| Benign | 150 | 99 (66%) | 44 (29%) | 6 (4%) | 1 (1%) | 51 (34%) | <0.001 *1 | <0.001 *1 | 0.301 *1 | 1.65 ± 1.41 | <0.001 *1 |
| HGPIN | 146 | 54 (37%) | 68 (47%) | 21 (14%) | 3 (2%) | 92 (63%) | <0.001 *2 | <0.001 *2 | <0.001 *2 | 2.58 ± 1.66 | <0.001 *2 |
| Carcinoma | 300 | 21 (7%) | 99 (33%) | 95 (32%) | 85 (28%) | 279 (93%) | <0.001 *3 | <0.001 *3 | <0.001 *3 | 5.20 ± 2.33 | <0.001 *3 |
| Age (mean ± SD, year) | 300 | 58.0 ± 4.8 | 60.2 ± 6.4 | 60.2 ± 6.1 | 60.8 ± 6.1 | 60.4 ± 6.2 | 0.079 | 0.363 | 0.275 | NA | |
| PSA (mean ± SD, ng/mL) | 300 | 5.72 ± 3.27 | 6.02 ± 3.07 | 7.21 ± 4.88 | 6.44 ± 3.87 | 6.31 ± 3.91 | 0.441 | 0.243 | 0.623 | NA | |
| Gleason score (GS)/Grade Group (GG) | |||||||||||
| GS ≤ 6/GG 1 | 107 | 11 (10%) | 32 (30%) | 44 (41%) | 20 (19%) | 96 (90%) | 0.097 *4 | 0.961 *4 | 0.006 *4 | 4.91 ± 2.15 | 0.099 *4 |
| GS 3 + 4 = 7/GG 2 | 127 | 9 (7%) | 52 (41%) | 36 (28%) | 30 (24%) | 118 (93%) | 0.048 *5 | 0.003 *5 | <0.001 *5 | 4.85 ± 2.34 | <0.001 *5 |
| GS 4 + 3 = 7/GG 3 | 46 | 1 (2%) | 11 (24%) | 9 (20%) | 25 (54%) | 45 (98%) | 0.204 *6 | 0.059 *6 | 0.026 *6 | 6.26 ± 2.28 | 0.010 *6 |
| GS ≥ 8/GG 4–5 | 20 | 0 (0%) | 4 (20%) | 6 (30%) | 10 (50%) | 20 (100%) | 6.50 ± 2.09 | ||||
| Pathologic stage (pT) | |||||||||||
| 2 | 235 | 15 (6%) | 88 (37%) | 79 (34%) | 53 (23%) | 220 (94%) | 0.426 *7 | 0.010 *7 | <0.001 *7 | 4.95 ± 2.19 | <0.001 *7 |
| 3a | 47 | 6 (13%) | 9 (19%) | 13 (28%) | 19 (40%) | 41 (87%) | 0.230 *8 | 0.010 *8 | <0.001 *8 | 5.51 ± 2.58 | <0.001 *8 |
| 3b | 18 | 0 (0%) | 2 (11%) | 3 (17%) | 13 (72%) | 18 (100%) | 7.61 ± 1.90 | ||||
| Lymph node metastasis (pN) | 0.326 | 0.075 | 0.021 | 0.002 | |||||||
| 0 | 154 | 15 (10%) | 48 (31%) | 45 (29%) | 46 (30%) | 139 (90%) | 5.05 ± 2.46 | ||||
| 1 | 9 | 0 (0%) | 1 (11%) | 2 (22%) | 6 (67%) | 9 (100%) | 7.67 ± 1.94 | ||||
| History of vasectomy | 0.293 | 0.044 | 0.217 | 0.018 | |||||||
| No | 286 | 21 (7%) | 97 (34%) | 89 (31%) | 79 (28%) | 265 (93%) | 5.13 ± 2.33 | ||||
| Yes | 14 | 0 (0%) | 2 (14%) | 6 (43%) | 6 (43%) | 14 (100%) | 6.64 ± 1.79 | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kawahara, T.; Teramoto, Y.; Li, Y.; Ishiguro, H.; Gordetsky, J.; Yang, Z.; Miyamoto, H. Impact of Vasectomy on the Development and Progression of Prostate Cancer: Preclinical Evidence. Cancers 2020, 12, 2295. https://doi.org/10.3390/cancers12082295
Kawahara T, Teramoto Y, Li Y, Ishiguro H, Gordetsky J, Yang Z, Miyamoto H. Impact of Vasectomy on the Development and Progression of Prostate Cancer: Preclinical Evidence. Cancers. 2020; 12(8):2295. https://doi.org/10.3390/cancers12082295
Chicago/Turabian StyleKawahara, Takashi, Yuki Teramoto, Yi Li, Hitoshi Ishiguro, Jennifer Gordetsky, Zhiming Yang, and Hiroshi Miyamoto. 2020. "Impact of Vasectomy on the Development and Progression of Prostate Cancer: Preclinical Evidence" Cancers 12, no. 8: 2295. https://doi.org/10.3390/cancers12082295
APA StyleKawahara, T., Teramoto, Y., Li, Y., Ishiguro, H., Gordetsky, J., Yang, Z., & Miyamoto, H. (2020). Impact of Vasectomy on the Development and Progression of Prostate Cancer: Preclinical Evidence. Cancers, 12(8), 2295. https://doi.org/10.3390/cancers12082295






