Conditional Probability of Survival and Prognostic Factors in Long-Term Survivors of High-Grade Serous Ovarian Cancer
Abstract
1. Introduction
2. Results
2.1. Patients
2.2. Treatment
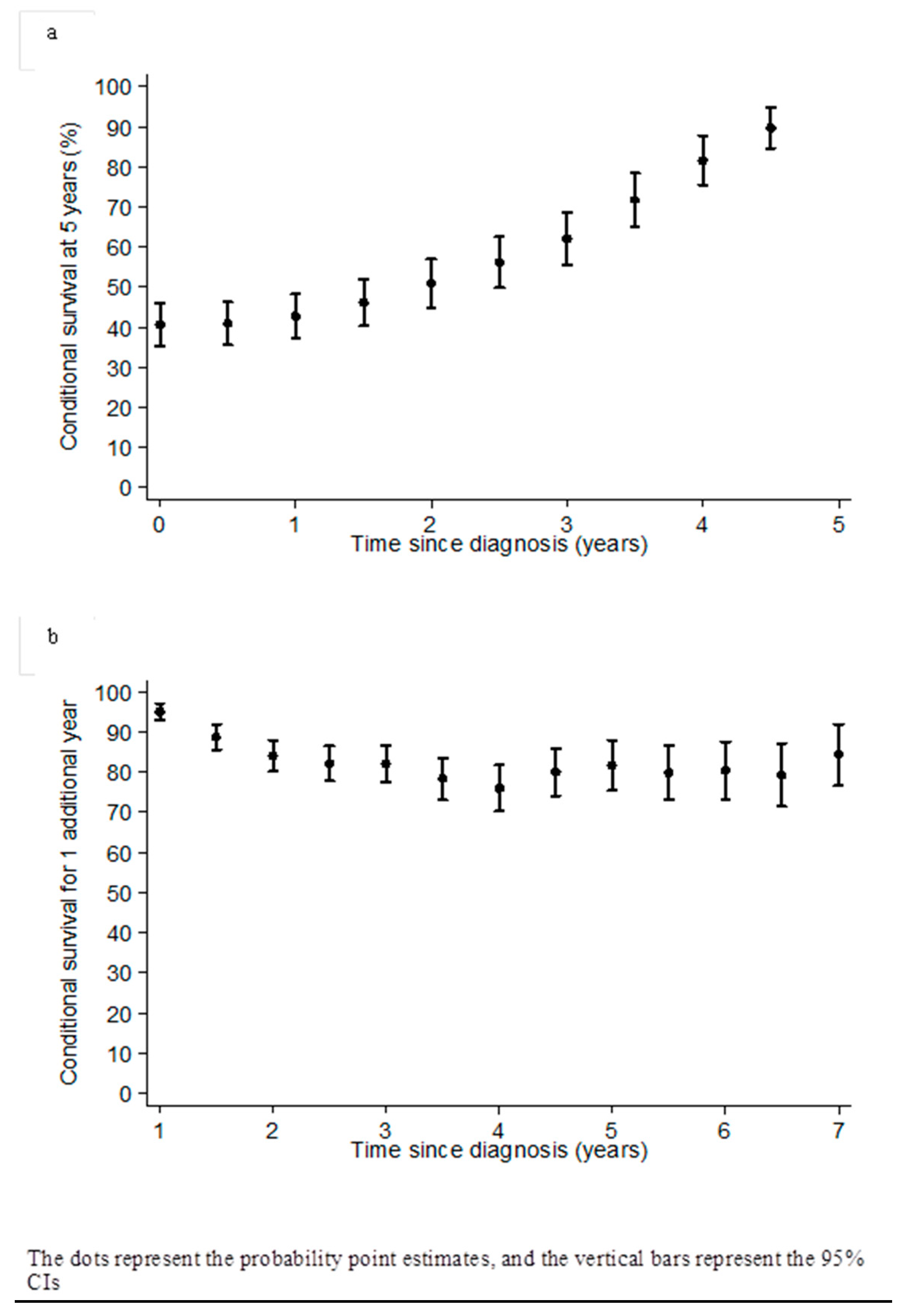
2.3. Survival and Conditional Survival
2.4. Prognostic Factors of Long-Term Survival According to the Five-Year Landmark Analysis
3. Discussion
4. Patients and Methods
4.1. Database
4.2. Study Patients
4.3. Treatment
4.4. Statistical Considerations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Data Sharing Statement
References
- Levanon, K.; Crum, C.; Drapkin, R. New Insights into the Pathogenesis of Serous Ovarian Cancer and Its Clinical Impact. J. Clin. Oncol. 2008, 26, 5284–5293. [Google Scholar] [CrossRef] [PubMed]
- Buys, S.S.; Partridge, E.; Black, A.; Johnson, C.C.; Lamerato, L.; Isaacs, C.; Reding, D.J.; Greenlee, R.T.; Yokochi, L.A.; Kessel, B.; et al. Effect of Screening on Ovarian Cancer Mortality: The Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Randomized Controlled Trial. JAMA 2011, 305, 2295–2303. [Google Scholar] [CrossRef] [PubMed]
- Cannistra, S.A. Cancer of the ovary. N. Engl. J. Med. 2004, 351, 2519–2529. [Google Scholar] [CrossRef] [PubMed]
- Trétarre, B.; Molinié, F.; Woronoff, A.-S.; Bossard, N.; Bessaoud, F.; Marrer, E.; Grosclaude, P.; Guizard, A.-V.; Delafosse, P.; Bara, S.; et al. Ovarian cancer in France: Trends in incidence, mortality and survival, 1980–2012. Gynecol. Oncol. 2015, 139, 324–329. [Google Scholar] [CrossRef]
- Colombo, P.-E.; Mourregot, A.; Fabbro, M.; Gutowski, M.; Saint-Aubert, B.; Quenet, F.; Gourgou, S.; Rouanet, P. Aggressive surgical strategies in advanced ovarian cancer: A monocentric study of 203 stage IIIC and IV patients. Eur. J. Surg. Oncol. 2009, 35, 135–143. [Google Scholar] [CrossRef]
- Du Bois, A.; Lück, H.J.; Meier, W.; Adams, H.P.; Möbus, V.; Costa, S.; Bauknecht, T.; Richter, B.; Warm, M.; Schröder, W. A Randomized Clinical Trial of Cisplatin/Paclitaxel versus Carboplatin/Paclitaxel As First-Line Treatment of Ovarian Cancer. J. Natl. Cancer Inst. 2003, 95, 1320–1329. [Google Scholar] [CrossRef]
- Du Bois, A.; Reuss, A.; Pujade-Lauraine, E.; Harter, P.; Ray-Coquard, I.; Pfisterer, J. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: A combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: By the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe d’Investigateurs Nationaux Pour les Etudes des Cancers de l’Ovaire (GINECO). Cancer 2009, 115, 1234–1244. [Google Scholar]
- Winter, W.E.; Maxwell, G.L.; Tian, C.; Carlson, J.W.; Ozols, R.F.; Rose, P.G.; Markman, M.; Armstrong, D.K.; Muggia, F.; McGuire, W.P. Prognostic Factors for Stage III Epithelial Ovarian Cancer: A Gynecologic Oncology Group Study. J. Clin. Oncol. 2007, 25, 3621–3627. [Google Scholar] [CrossRef]
- Bristow, R.E.; Puri, I.; Chi, D.S. Cytoreductive surgery for recurrent ovarian cancer: A meta-analysis. Gynecol. Oncol. 2009, 112, 265–274. [Google Scholar] [CrossRef]
- Van Driel, W.J.; Koole, S.N.; Sikorska, K.; Van Leeuwen, J.H.S.; Schreuder, H.W.R.; Hermans, R.H.M.; De Hingh, I.H.J.T.; Van der Velden, J.; Arts, H.J.; Massuger, L.F.A.G.; et al. Hyperthermic Intraperitoneal Chemotherapy in Ovarian Cancer. N. Engl. J. Med. 2018, 378, 230–240. [Google Scholar] [CrossRef]
- Timmermans, M.; Zwakman, N.; Sonke, G.S.; Van de Vijver, K.K.; Duk, M.J.; Van der Aa, M.A.; Kruitwagen, R.F. Perioperative change in CA125 is an independent prognostic factor for improved clinical outcome in advanced ovarian cancer. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 240, 364–369. [Google Scholar] [CrossRef] [PubMed]
- Vencken, P.M.L.H.; Kriege, M.; Hoogwerf, D.; Beugelink, S.; Van der Burg, M.E.L.; Hooning, M.J.; Berns, E.M.; Jager, A.; Collee, M.; Burger, C.W.; et al. Chemosensitivity and outcome of BRCA1- and BRCA2-associated ovarian cancer patients after first-line chemotherapy compared with sporadic ovarian cancer patients. Ann. Oncol. 2011, 22, 1346–1352. [Google Scholar] [CrossRef] [PubMed]
- Kotsopoulos, J.; Rosen, B.; Fan, I.; Moody, J.; McLaughlin, J.R.; Risch, H.; May, T.; Sun, P.; Narod, S.A. Ten-year survival after epithelial ovarian cancer is not associated with BRCA mutation status. Gynecol. Oncol. 2016, 140, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Kurta, M.L.; Edwards, R.P.; Moysich, K.B.; McDonough, K.; Bertolet, M.; Weissfeld, J.L.; Catov, J.M.; Modugno, F.; Bunker, C.H.; Ness, R.B.; et al. Prognosis and Conditional Disease-Free Survival among Patients with Ovarian Cancer. J. Clin. Oncol. 2014, 32, 4102–4112. [Google Scholar] [CrossRef]
- Hoppenot, C.; Eckert, M.A.; Tienda, S.M.; Lengyel, E. Who are the long-term survivors of high grade serous ovarian cancer? Gynecol. Oncol. 2018, 148, 204–212. [Google Scholar] [CrossRef]
- Merrill, R.M.; Henson, D.E.; Barnes, M. Conditional survival among patients with carcinoma of the lung. Chest 1999, 116, 697–703. [Google Scholar] [CrossRef]
- Skuladottir, H.; Olsen, J.H. Conditional survival of patients with the four major histologic subgroups of lung cancer in Denmark. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2003, 21, 3035–3040. [Google Scholar] [CrossRef]
- Chang, G.J.; Hu, C.-Y.; Eng, C.; Skibber, J.M.; Rodriguez-Bigas, M.A. Practical application of a calculator for conditional survival in colon cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2009, 27, 5938–5943. [Google Scholar] [CrossRef]
- Nathan, H.; De Jong, M.C.; Pulitano, C.; Ribero, D.; Strub, J.; Mentha, G.; Gigot, J.-F.; Schulick, R.D.; Choti, M.A.; Aldrighetti, L.; et al. Conditional survival after surgical resection of colorectal liver metastasis: An international multi-institutional analysis of 949 patients. J. Am. Coll. Surg. 2010, 210, 755–766. [Google Scholar] [CrossRef]
- Wang, S.J.; Fuller, C.D.; Emery, R.; Thomas, C.R. Conditional Survival in Rectal Cancer: A SEER Database Analysis. Gastrointest. Cancer Res. GCR 2007, 1, 84–89. [Google Scholar]
- Polley, M.-Y.C.; Lamborn, K.R.; Chang, S.M.; Butowski, N.; Clarke, J.L.; Prados, M. Conditional probability of survival in patients with newly diagnosed glioblastoma. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2011, 29, 4175–4180. [Google Scholar] [CrossRef] [PubMed]
- Fuller, C.D.; Wang, S.J.; Thomas, C.R.; Hoffman, H.T.; Weber, R.S.; Rosenthal, D.I. Conditional survival in head and neck squamous cell carcinoma: Results from the SEER dataset 1973–1998. Cancer 2007, 109, 1331–1343. [Google Scholar] [CrossRef] [PubMed]
- Rueth, N.M.; Groth, S.S.; Tuttle, T.M.; Virnig, B.A.; Al-Refaie, W.B.; Habermann, E.B. Conditional survival after surgical treatment of melanoma: An analysis of the Surveillance, Epidemiology, and End Results database. Ann. Surg. Oncol. 2010, 17, 1662–1668. [Google Scholar] [CrossRef] [PubMed]
- Xing, Y.; Chang, G.J.; Hu, C.-Y.; Askew, R.L.; Ross, M.I.; Gershenwald, J.E.; Lee, J.E.; Mansfield, P.F.; Lucci, A.; Cormier, J.N. Conditional survival estimates improve over time for patients with advanced melanoma: Results from a population-based analysis. Cancer 2010, 116, 2234–2241. [Google Scholar] [CrossRef]
- Choi, M.; Fuller, C.D.; Thomas, C.R.J.; Wang, S.J. Conditional survival in ovarian cancer: Results from the SEER dataset 1988–2001. Gynecol. Oncol. 2008, 109, 203–209. [Google Scholar] [CrossRef]
- Gloeckler Ries, L.A.; Reichman, M.E.; Lewis, D.R.; Hankey, B.F.; Edwards, B.K. Cancer survival and incidence from the Surveillance, Epidemiology, and End Results (SEER) program. Oncologist 2003, 8, 541–552. [Google Scholar] [CrossRef]
- Merrill, R.M.; Hunter, B.D. Conditional Survival among Cancer Patients in the United States. Oncologist 2010, 15, 873–882. [Google Scholar] [CrossRef]
- Ray-Coquard, I.; Pautier, P.; Pignata, S.; Pérol, D.; González-Martín, A.; Berger, R.; Fujiwara, K.; Vergote, I.; Colombo, N.; Mäenpää, J.; et al. Olaparib Plus Bevacizumab As First-Line Maintenance in Ovarian Cancer. N. Engl. J. Med. 2019, 381, 2416–2428. [Google Scholar] [CrossRef]
- González-Martín, A.; Pothuri, B.; Vergote, I.; DePont Christensen, R.; Graybill, W.; Mirza, M.R.; McCormick, C.; Lorusso, D.; Hoskins, P.; Freyer, G.; et al. Niraparib in Patients with Newly Diagnosed Advanced Ovarian Cancer. N. Engl. J. Med. 2019, 381, 2391–2402. [Google Scholar] [CrossRef]
- Moore, K.; Colombo, N.; Scambia, G.; Kim, B.-G.; Oaknin, A.; Friedlander, M.; Lisyanskaya, A.; Floquet, A.; Leary, A.; Sonke, G.S.; et al. Maintenance Olaparib in Patients with Newly Diagnosed Advanced Ovarian Cancer. N. Engl. J. Med. 2018, 379, 2495–2505. [Google Scholar] [CrossRef]
- Mirza, M.R.; Monk, B.J.; Herrstedt, J.; Oza, A.M.; Mahner, S.; Redondo, A.; Fabbro, M.; Ledermann, J.A.; Lorusso, D.; Vergote, I.; et al. Niraparib Maintenance Therapy in Platinum-Sensitive, Recurrent Ovarian Cancer. N. Engl. J. Med. 2016, 375, 2154–2164. [Google Scholar] [CrossRef] [PubMed]
- Pujade-Lauraine, E.; Ledermann, J.A.; Selle, F.; Gebski, V.; Penson, R.T.; Oza, A.M.; Korach, J.; Huzarski, T.; Poveda, A.; Pignata, S. Olaparib tablets as maintenance therapy in patients with platinum-sensitive, relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT-Ov21): A double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2017, 18, 1274–1284. [Google Scholar] [CrossRef]
- Coleman, R.L.; Oza, A.M.; Lorusso, D.; Aghajanian, C.; Oaknin, A.; Dean, A.; Colombo, N.; Weberpals, J.I.; Clamp, A.; Scambia, G. Rucaparib maintenance treatment for recurrent ovarian carcinoma after response to platinum therapy (ARIEL3): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017, 390, 1949–1961. [Google Scholar] [CrossRef]
- Coleman, R.L.; Fleming, G.F.; Brady, M.F.; Swisher, E.M.; Steffensen, K.D.; Friedlander, M.; Okamoto, A.; Moore, K.N.; Efrat Ben-Baruch, N.; Werner, T.L.; et al. Veliparib with First-Line Chemotherapy and As Maintenance Therapy in Ovarian Cancer. N. Engl. J. Med. 2019, 381, 2403–2415. [Google Scholar] [CrossRef]
- Elzarkaa, A.A.; Shaalan, W.; Elemam, D.; Mansour, H.; Melis, M.; Malik, E.; Soliman, A.A. Peritoneal cancer index as a predictor of survival in advanced stage serous epithelial ovarian cancer: A prospective study. J. Gynecol. Oncol. 2018, 29, e47. [Google Scholar] [CrossRef]
- Pectasides, D.; Papaxoinis, G.; Fountzilas, G.; Aravantinos, G.; Bamias, A.; Pavlidis, N.; Kalofonos, H.P.; Timotheadou, E.; Samantas, E.; Briasoulis, E.; et al. Epithelial ovarian cancer in Greece: A retrospective study of 1791 patients by the Hellenic Cooperative Oncology Group (HeCOG). Anticancer Res. 2009, 29, 745–751. [Google Scholar]
- Colombo, P.E.; Labaki, M.; Fabbro, M.; Bertrand, M.; Mourregot, A.; Gutowski, M.; Saint-Aubert, B.; Quenet, F.; Rouanet, P.; Mollevi, C. Impact of neoadjuvant chemotherapy cycles prior to interval surgery in patients with advanced epithelial ovarian cancer. Gynecol. Oncol. 2014, 135, 223–230. [Google Scholar] [CrossRef]
- Goéré, D.; Souadka, A.; Faron, M.; Cloutier, A.S.; Viana, B.; Honoré, C.; Dumont, F.; Elias, D. Extent of Colorectal Peritoneal Carcinomatosis: Attempt to Define a Threshold above Which HIPEC Does Not Offer Survival Benefit: A Comparative Study. Ann. Surg. Oncol. 2015, 22, 2958–2964. [Google Scholar] [CrossRef]
- Yang, S.Y.C.; Lheureux, S.; Karakasis, K.; Burnier, J.V.; Bruce, J.P.; Clouthier, D.L.; Danesh, A.; Quevedo, R.; Dowar, M.; Hanna, Y.; et al. Landscape of genomic alterations in high-grade serous ovarian cancer from exceptional long- and short-term survivors. Genome Med. 2018, 10, 81. [Google Scholar] [CrossRef]
- Davis, F.G.; McCarthy, B.J.; Freels, S.; Kupelian, V.; Bondy, M.L. The conditional probability of survival of patients with primary malignant brain tumors. Cancer 1999, 85, 485–491. [Google Scholar] [CrossRef]
| Characteristics | Non-Long Survivors n = 284 | Long-Term Survivors n = 120 | Total n = 404 | p-Value | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Age | |||||||
| Median (range) | 62 (20–89) | 57 (21–83) | 61 (20–89) | <0.001 | |||
| <65 | 168 | 59.2 | 91 | 75.8 | 259 | 64.1 | 0.001 |
| ≥65 | 116 | 40.8 | 29 | 24.2 | 145 | 35.9 | |
| WHO Performance status | 0.045 | ||||||
| 0–1 | 227 | 84.7 | 98 | 92.5 | 325 | 86.9 | |
| 2 | 41 | 15.3 | 8 | 7.5 | 49 | 13.1 | |
| Missing | 16 | 14 | 30 | ||||
| CA 125 level | |||||||
| Median (range) | 700 (6–21) | 790 (14–12) | 734 (6–22) | 0.360 | |||
| <70 | 16 | 7.5 | 4 | 4.9 | 20 | 6.8 | 0.434 |
| ≥70 | 197 | 92.5 | 77 | 95.1 | 274 | 93.2 | |
| Missing | 71 | 39 | 110 | ||||
| FIGO stage | 0.168 | ||||||
| III | 230 | 81.0 | 104 | 86.7 | 334 | 82.7 | |
| IV | 54 | 19.0 | 16 | 13.3 | 70 | 17.3 | |
| Metastasis localization (n = 70) | |||||||
| Pleural | 34 | 69.4 | 8 | 61.5 | 42 | 67.7 | |
| Visceral | 15 | 30.6 | 5 | 38.5 | 20 | 32.3 | |
| Missing | 5 | 3 | 8 | ||||
| N stage | 0.431 | ||||||
| N− | 63 | 28.0 | 32 | 32.3 | 95 | 29.3 | |
| N+ | 162 | 72.0 | 67 | 67.7 | 229 | 70.7 | |
| Missing | 59 | 21 | 80 | ||||
| BRCA mutation | 0.768 | ||||||
| Mutated BRCA1 | 12 | 20.7 | 15 | 25.9 | 27 | 23.3 | |
| Mutated BRCA2 | 5 | 8.6 | 6 | 10.3 | 11 | 9.5 | |
| No mutation | 41 | 70.7 | 37 | 63.8 | 78 | 67.2 | |
| Missing | 226 | 62 | 288 | ||||
| Characteristics | Non-Long Survivors n = 284 | Long-Term Survivors n = 120 | Total n = 404 | p-Value | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Surgery type | <0.001 | ||||||
| Primary | 133 | 46.8 | 81 | 67.5 | 214 | 53.0 | |
| Interval surgery | 151 | 53.2 | 39 | 32.5 | 190 | 47.0 | |
| Digestive resection | <0.001 | ||||||
| 0 | 87 | 43.1 | 66 | 60.0 | 153 | 49.0 | |
| >1 | 115 | 56.9 | 44 | 40.0 | 159 | 51.0 | |
| Missing | 82 | 10 | 92 | ||||
| Splenectomy | 0.241 | ||||||
| No | 128 | 96.2 | 75 | 92.6 | 203 | 94.9 | |
| Yes | 5 | 3.8 | 6 | 7.4 | 11 | 5.1 | |
| Missing | 151 | 39 | 190 | ||||
| Primary or interval surgery | 0.192 | ||||||
| Complete (Gross total resection) | 160 | 56.3 | 76 | 63.3 | 236 | 58.4 | |
| Incomplete (Macroscopic residual disease) | 124 | 43.7 | 44 | 36.7 | 168 | 41.6 | |
| Initial PCI | |||||||
| Median (range) | 14 (0–33) | 11 (0–24) | 13 (0–33) | <0.001 | |||
| <17 | 165 | 63.0 | 87 | 82.1 | 252 | 68.5 | <0.001 |
| ≥17 | 97 | 37.0 | 19 | 17.9 | 116 | 31.5 | |
| Missing | 22 | 14 | 36 | ||||
| Chemotherapy | |||||||
| Neoadjuvant CT | 147 | 51.9 | 37 | 31.1 | 184 | 45.8 | <0.001 |
| Missing | 1 | 1 | 2 | ||||
| 1st CT line regimen | 0.793 | ||||||
| Platinum salts/Paclitaxel | 223 | 79.7 | 97 | 82.2 | 320 | 80.4 | |
| Platinum salts/Exoxan | 30 | 10.7 | 12 | 10.2 | 42 | 10.6 | |
| Others | 27 | 9.6 | 9 | 7.6 | 36 | 9.0 | |
| Missing | 4 | 2 | 6 | ||||
| Number of cycles | 0.946 | ||||||
| Median (range) | 6 (1–14) | 6 (3–12) | 6 (1–14) | ||||
| Missing | 6 | 1 | 7 | ||||
| Sensibility to 1st CT line | 0.001 | ||||||
| Refractory/Resistant | 85 | 31.8 | 6 | 5.0 | 91 | 23.5 | |
| Sensible | 181 | 68.2 | 114 | 95.0 | 295 | 76.5 | |
| Missing | 18 | 0 | 18 | ||||
| Treatment-free Interval (months) | <0.001 | ||||||
| Median (range) | 8.5 (0.4–47.2) | 23.9 (0.7–121.6) | 11 (0.4–121.6) | ||||
| <18 | 149 | 85.6 | 35 | 42.2 | 184 | 71.6 | |
| ≥18 | 25 | 14.4 | 48 | 57.8 | 73 | 28.4 | |
| Missing/No 2nd CT line | 110 | 37 | 147 | ||||
| Progression-free Interval (months) | <0.001 | ||||||
| Median (range) | 14.5 (0.4–56.6) | 43.4 (2.3–248.2) | 17.4 (0.4–248.2) | ||||
| <18 | 187 | 66.6 | 17 | 14.2 | 204 | 50.9 | |
| ≥18 | 94 | 33.5 | 103 | 85.8 | 197 | 49.1 | |
| Missing | 3 | 0 | 3 | ||||
| n = 404 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Time | Overall Survival Rate | Conditional Probability of Survival | |||||||||
| 2 Years | 3 Years | 4 Years | 5 Years | ||||||||
| % | 95% CI | No. at risk | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| 1 year | 95.0 | (92.4; 96.7) | 373 | 84.0 | (80.2; 87.8) | 68.9 | (64.0; 73.8) | 52.4 | (46.9; 57.8) | 42.8 | (37.3; 48.3) |
| 2 years | 79.8 | (75.4; 83.5) | 279 | 82.0 | (77.4; 86.6) | 62.3 | (56.5; 68.2) | 50.9 | (44.8; 57.0) | ||
| 3 years | 65.5 | (60.3; 70.1) | 219 | 76.0 | (70.2; 81.7) | 62.0 | (55.4; 68.7) | ||||
| 4 years | 49.7 | (44.3; 54.9) | 158 | 81.7 | (75.5; 87.8) | ||||||
| 5 years | 40.6 | (35.3; 45.9) | 120 | ||||||||
| n = 120 | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | |
| Age | ||||
| <65 | 1 | |||
| ≥65 | 1.60 | (0.95; 2.70) | ||
| p = 0.085 | ||||
| WHO Performance status | ||||
| 0 | 1 | |||
| 1–2 | 1.15 | (0.42; 3.18) | ||
| p = 0.790 | ||||
| FIGO stage | ||||
| III | 1 | |||
| IV | 1.08 | (0.53; 2.19) | ||
| p = 0.830 | ||||
| N stage | ||||
| N− | 1 | |||
| N+ | 1.33 | (0.75; 2.38) | ||
| p = 0.325 | ||||
| BRCA mutation | ||||
| Mutated BRCA1/2 | 1 | |||
| No mutation | 1.02 | (0.43; 2.44) | ||
| p = 0.958 | ||||
| Primary or interval surgery | ||||
| Complete | 1 | |||
| Incomplete | 1.92 | (1.17; 3.14) | ||
| p = 0.011 | ||||
| Initial PCI | ||||
| <17 | 1 | |||
| ≥17 | 1.78 | (0.96; 3.27) | ||
| p = 0.079 | ||||
| Sensibility to 1st CT line | ||||
| Refractory/Resistant | 1 | |||
| Sensitive | 0.47 | (0.19; 1.19) | ||
| p = 0.149 | ||||
| Progression-free interval | ||||
| <18 months | 1 | 1 | ||
| ≥18 months | 0.23 | (0.13; 0.40) | 0.23 | [0.13; 0.40] |
| p < 0.0001 | p < 0.0001 | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fabbro, M.; Colombo, P.-E.; Leaha, C.M.; Rouanet, P.; Carrère, S.; Quenet, F.; Gutowski, M.; Mourregot, A.; D’Hondt, V.; Coupier, I.; et al. Conditional Probability of Survival and Prognostic Factors in Long-Term Survivors of High-Grade Serous Ovarian Cancer. Cancers 2020, 12, 2184. https://doi.org/10.3390/cancers12082184
Fabbro M, Colombo P-E, Leaha CM, Rouanet P, Carrère S, Quenet F, Gutowski M, Mourregot A, D’Hondt V, Coupier I, et al. Conditional Probability of Survival and Prognostic Factors in Long-Term Survivors of High-Grade Serous Ovarian Cancer. Cancers. 2020; 12(8):2184. https://doi.org/10.3390/cancers12082184
Chicago/Turabian StyleFabbro, Michel, Pierre-Emmanuel Colombo, Cristina Marinella Leaha, Philippe Rouanet, Sébastien Carrère, François Quenet, Marian Gutowski, Anne Mourregot, Véronique D’Hondt, Isabelle Coupier, and et al. 2020. "Conditional Probability of Survival and Prognostic Factors in Long-Term Survivors of High-Grade Serous Ovarian Cancer" Cancers 12, no. 8: 2184. https://doi.org/10.3390/cancers12082184
APA StyleFabbro, M., Colombo, P.-E., Leaha, C. M., Rouanet, P., Carrère, S., Quenet, F., Gutowski, M., Mourregot, A., D’Hondt, V., Coupier, I., Vendrell, J., Vilquin, P., Pujol, P., Solassol, J., & Mollevi, C. (2020). Conditional Probability of Survival and Prognostic Factors in Long-Term Survivors of High-Grade Serous Ovarian Cancer. Cancers, 12(8), 2184. https://doi.org/10.3390/cancers12082184






