Identification of Cardiac Glycosides as Novel Inhibitors of eIF4A1-Mediated Translation in Triple-Negative Breast Cancer Cells
Abstract
1. Introduction
2. Results
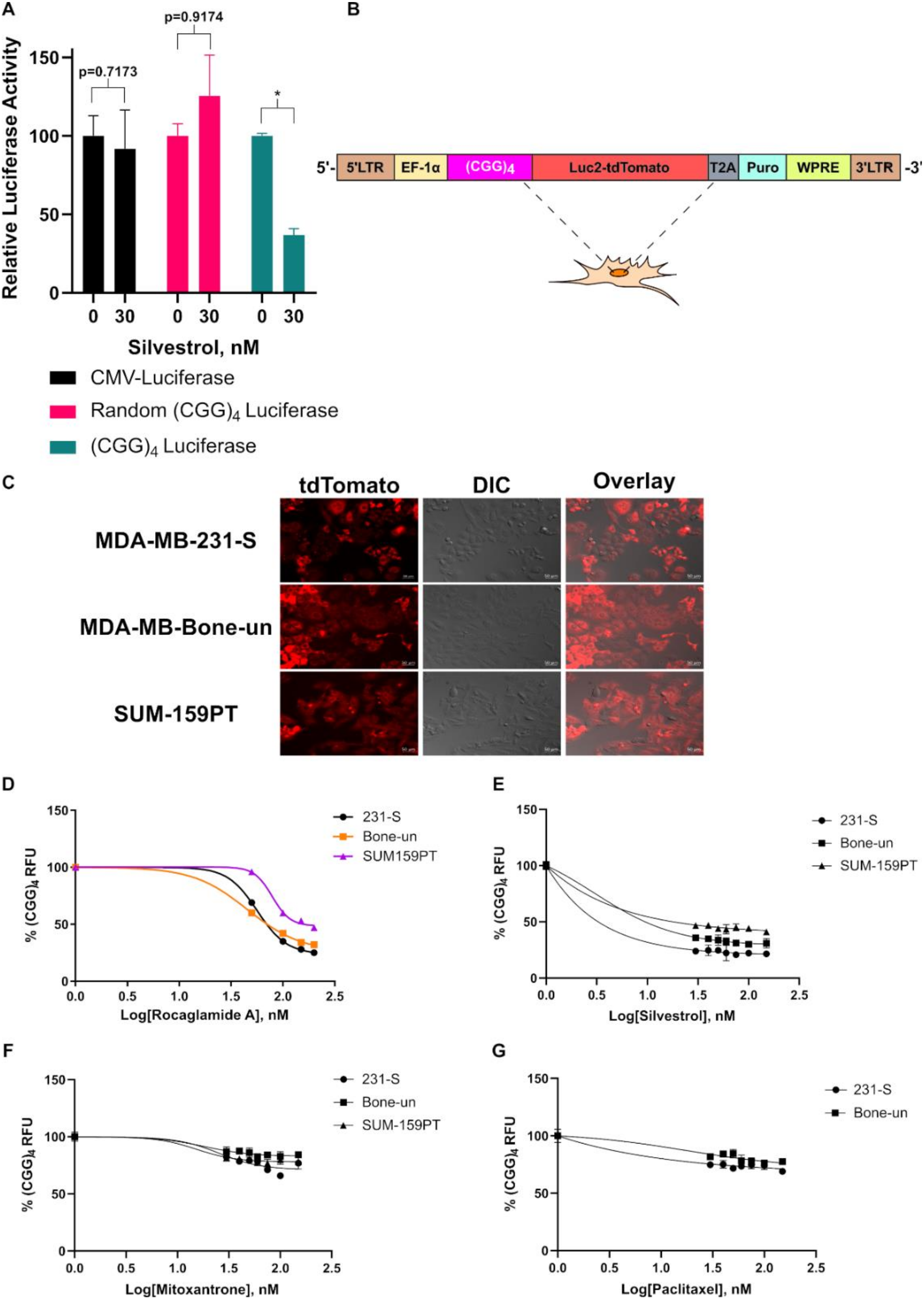
2.1. Establishment of the (CGG)4 Luc2-TdTomato Reporter System
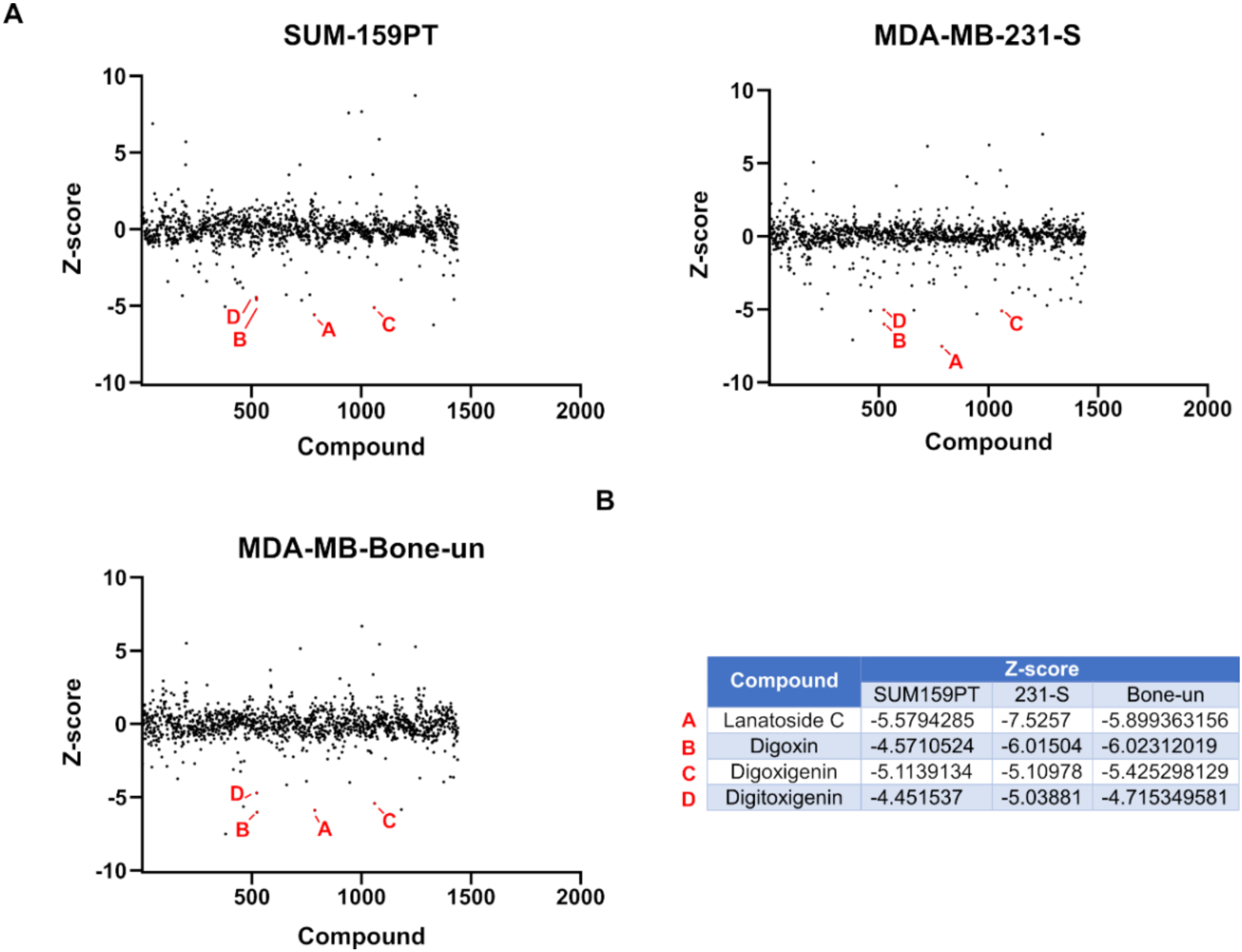
2.2. Prestwick Chemical Library Screen
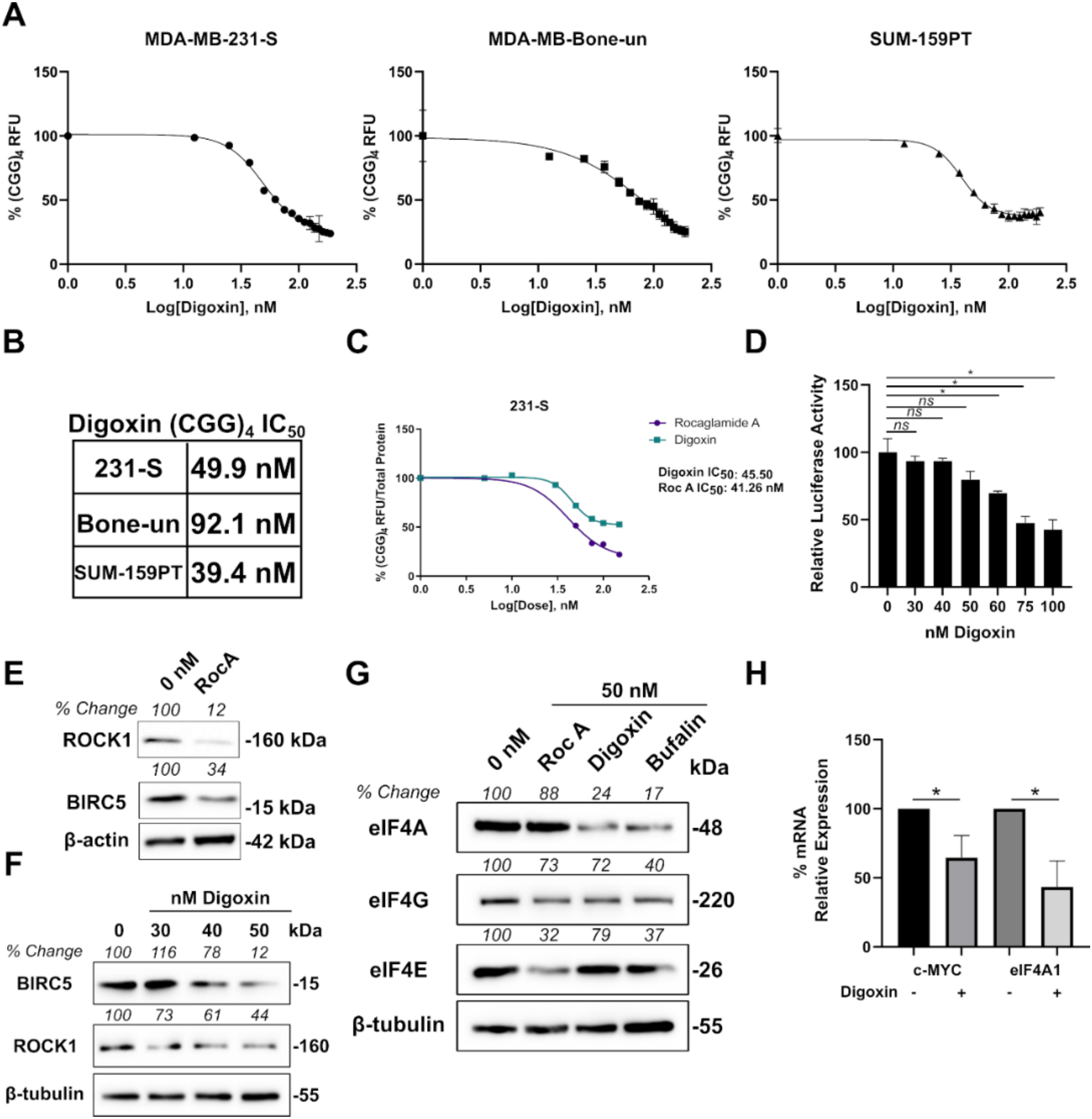
2.3. Cardiac Glycosides Inhibit eIF4A-Mediated Translation in Triple-Negative Breast Cancer Cells
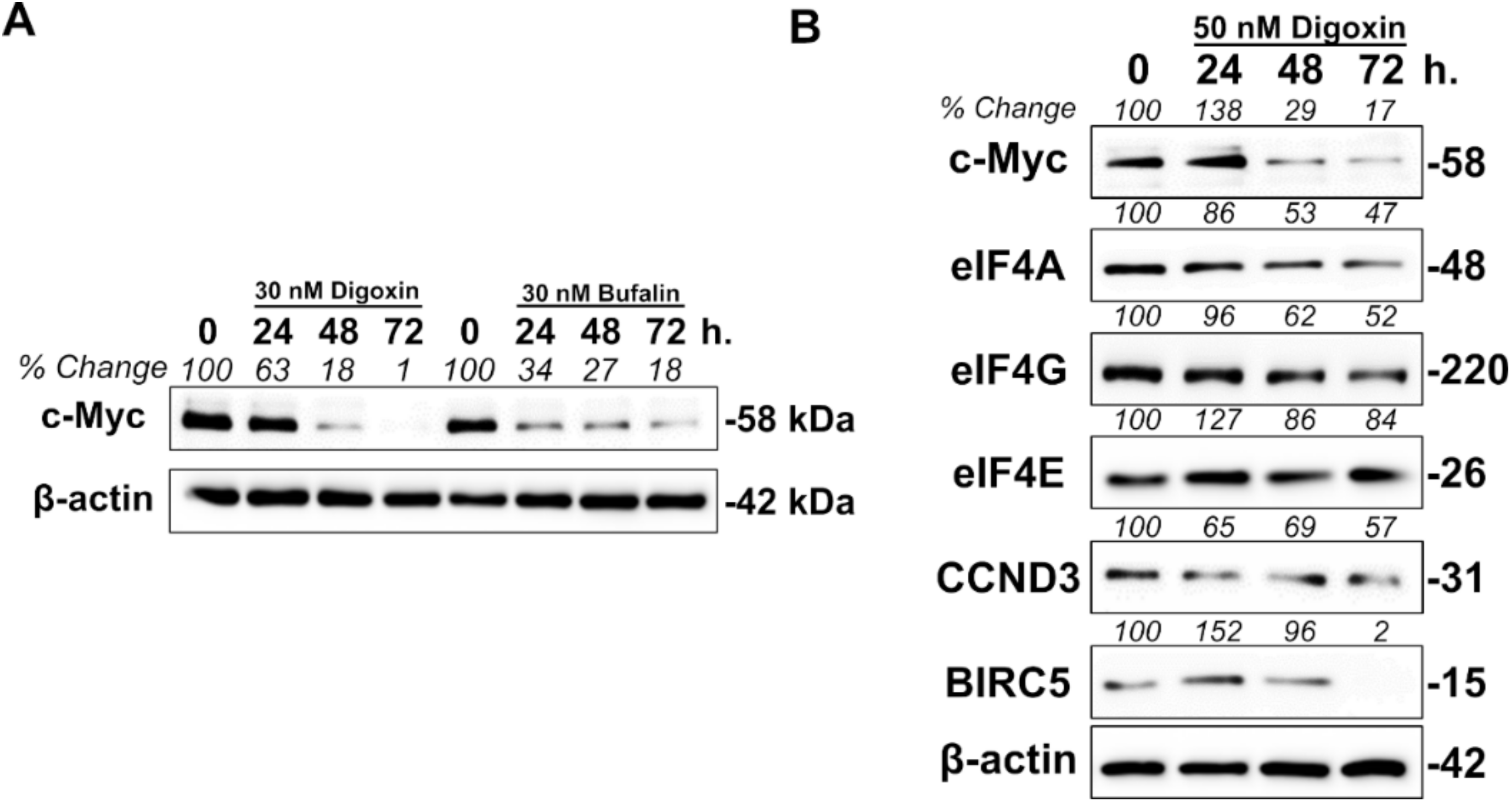
2.4. Cardiac Glycosides Modulate eIF4A1 Expression Levels through c-MYC
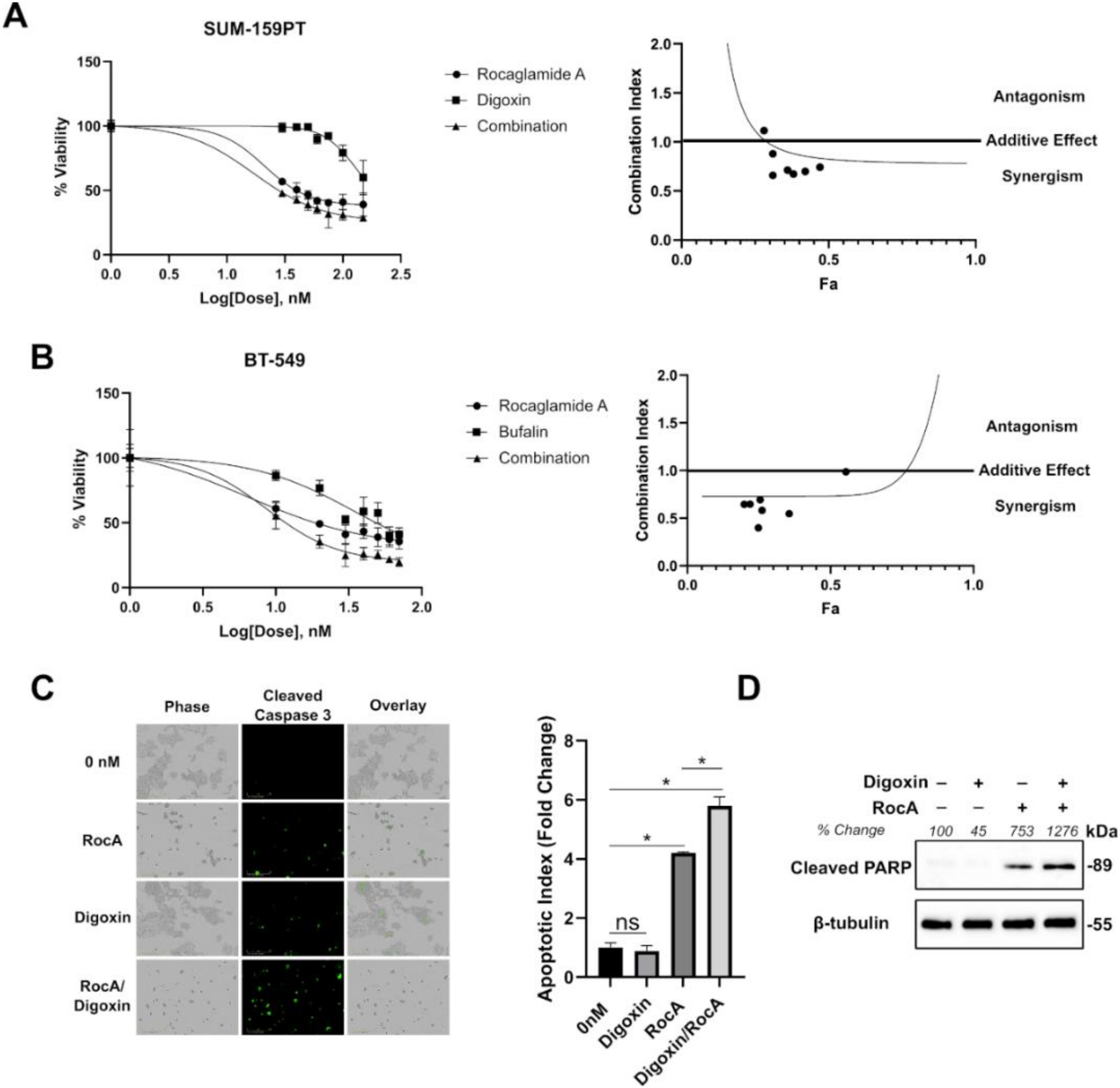
2.5. The Combination of Cardiac Glycosides and Rocaglates are Synergistic in Inhibiting TNBC Cells in Vitro
3. Discussion
4. Materials and Methods
4.1. Cell Culture
4.2. Plasmids
4.3. Compounds and Drug Treatments
4.4. Luciferase Assays
4.5. Generation of (CGG)4 Reporter Cell Lines
4.6. (CGG)4-Luc2-tdTomato and Total Protein Readings
4.7. Prestwick Chemical Library Screen
4.8. Western Blotting
4.9. qPCR
4.10. Promoter Binding Analysis
4.11. iLINCS GSEA
4.12. Rescue Experiments
4.13. Cell Viability
4.14. Synergy Analysis
4.15. Live-cell Cleaved Caspase 3 Staining
4.16. Graph Preparation, Determination of IC50 Values, and Statistical Analysis
4.17. Patents
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Liedtke, C.; Mazouni, C.; Hess, K.R.; André, F.; Tordai, A.; Mejia, J.A.; Symmans, W.F.; Gonzalez-Angulo, A.M.; Hennessy, B.; Green, M.C.; et al. Response to Neoadjuvant Therapy and Long-Term Survival in Patients With Triple-Negative Breast Cancer. J. Clin. Oncol. 2008, 26, 1275–1281. [Google Scholar] [CrossRef] [PubMed]
- Dent, R.; Trudeau, M.E.; Pritchard, K.I.; Hanna, W.; Kahn, H.K.; Sawka, C.A.; Lickley, L.A.; Rawlinson, E.; Sun, P.; Narod, S.A. Triple-Negative Breast Cancer: Clinical Features and Patterns of Recurrence. Clin. Cancer Res. 2007, 13, 4429–4434. [Google Scholar] [CrossRef] [PubMed]
- Dent, R.; Hanna, W.M.; Trudeau, M.; Rawlinson, E.; Sun, P.; Narod, S.A. Pattern of metastatic spread in triple-negative breast cancer. Breast Cancer Res. Treat. 2008, 115, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Di Leo, A.; Desmedt, C.; Bartlett, J.M.S.; Piette, F.; Ejlertsen, B.; Pritchard, K.I.; Larsimont, D.; Poole, C.; Isola, J.; Earl, H.; et al. HER2 and TOP2A as predictive markers for anthracycline-containing chemotherapy regimens as adjuvant treatment of breast cancer: A meta-analysis of individual patient data. Lancet Oncol. 2011, 12, 1134–1142. [Google Scholar] [CrossRef]
- Ellis, P.; Barrett-Lee, P.J.; Johnson, L.; Cameron, D.; Wardley, A.; O’Reilly, S.; Verrill, M.; Smith, I.; Yarnold, J.; Coleman, R.; et al. Sequential docetaxel as adjuvant chemotherapy for early breast cancer (TACT): An open-label, phase III, randomised controlled trial. Lancet 2009, 373, 1681–1692. [Google Scholar] [CrossRef]
- Adams, S.; Loi, S.; Toppmeyer, D.; Cescon, D.; De Laurentiis, M.; Nanda, R.; Winer, E.; Mukai, H.; Tamura, K.; Armstrong, A.; et al. Pembrolizumab monotherapy for previously untreated, PD-L1-positive, metastatic triple-negative breast cancer: Cohort B of the phase II KEYNOTE-086 study. Ann. Oncol. 2019, 30, 405–411. [Google Scholar] [CrossRef]
- Turner, N.; Telli, M.L.; Rugo, H.S.; Mailliez, A.; Ettl, J.; Grischke, E.-M.; Mina, L.A.; Balmaña, J.; Fasching, P.A.; Hurvitz, S.A.; et al. A Phase II Study of Talazoparib after Platinum or Cytotoxic Nonplatinum Regimens in Patients with Advanced Breast Cancer and Germline BRCA1/2 Mutations (ABRAZO). Clin. Cancer Res. 2018, 25, 2717–2724. [Google Scholar] [CrossRef]
- Pelletier, J.; Sonenberg, N. The Organizing Principles of Eukaryotic Ribosome Recruitment. Annu. Rev. Biochem. 2019, 88, 307–335. [Google Scholar] [CrossRef]
- Svitkin, Y.V.; Pause, A.; Haghighat, A.; Pyronnet, S.; Witherell, G.; Belsham, G.J.; Sonenberg, N. The requirement for eukaryotic initiation factor 4A (eIF4A) in translation is in direct proportion to the degree of mRNA 5′ secondary structure. RNA 2001, 7, 382–394. [Google Scholar] [CrossRef]
- Pelletier, J.; Graff, J.; Ruggero, D.; Sonenberg, N. Targeting the eIF4F translation initiation complex: A critical nexus for cancer development. Cancer Res. 2015, 75, 250–263. [Google Scholar] [CrossRef]
- Graff, J.R.; Konicek, B.W.; Vincent, T.M.; Lynch, R.L.; Monteith, D.; Weir, S.N.; Schwier, P.; Capen, A.; Goode, R.L.; Dowless, M.S.; et al. Therapeutic suppression of translation initiation factor eIF4E expression reduces tumor growth without toxicity. J. Clin. Investig. 2007, 117, 2638–2648. [Google Scholar] [CrossRef] [PubMed]
- Nasr, Z.; Robert, F.; Porco, J.A.; Muller, W.J.; Pelletier, J. eIF4F suppression in breast cancer affects maintenance and progression. Oncogene 2012, 32, 861–871. [Google Scholar] [CrossRef] [PubMed]
- Modelska, A.; Turro, E.; Russell, R.; Beaton, J.; Sbarrato, T.; Spriggs, K.; Miller, J.; Graf, S.; Provenzano, E.; Blows, F.; et al. The malignant phenotype in breast cancer is driven by eIF4A1-mediated changes in the translational landscape. Cell Death Dis. 2015, 6, e1603. [Google Scholar] [CrossRef] [PubMed]
- Sridharan, S.; Robeson, M.; Bastihalli-Tukaramrao, D.; Howard, C.M.; Subramaniyan, B.; Tilley, A.M.C.; Tiwari, A.K.; Raman, D. Targeting of the Eukaryotic Translation Initiation Factor 4A Against Breast Cancer Stemness. Front. Oncol. 2019, 9, 9. [Google Scholar] [CrossRef] [PubMed]
- Moerke, N.J.; Aktas, H.; Chen, H.; Cantel, S.; Reibarkh, M.J.; Fahmy, A.; Gross, J.D.; Degterev, A.; Yuan, J.; Chorev, M.; et al. Small-Molecule Inhibition of the Interaction between the Translation Initiation Factors eIF4E and eIF4G. Cell 2007, 128, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Bordeleau, M.-E.; Matthews, J.; Wojnar, J.M.; Lindqvist, L.; Novac, O.; Jankowsky, E.; Sonenberg, N.; Northcote, P.; Teesdale-Spittle, P.; Pelletier, J. Stimulation of mammalian translation initiation factor eIF4A activity by a small molecule inhibitor of eukaryotic translation. Proc. Natl. Acad. Sci. USA 2005, 102, 10460–10465. [Google Scholar] [CrossRef]
- Bordeleau, M.-E.; Mori, A.; Oberer, M.; Lindqvist, L.; Chard, L.S.; Higa, T.; Belsham, G.J.; Wagner, G.; Tanaka, J.; Pelletier, J. Functional characterization of IRESes by an inhibitor of the RNA helicase eIF4A. Nat. Chem. Biol. 2006, 2, 213–220. [Google Scholar] [CrossRef]
- Iwasaki, S.; Floor, S.N.; Ingolia, N.T. Rocaglates convert DEAD-box protein eIF4A into a sequence-selective translational repressor. Nature 2016, 534, 558–561. [Google Scholar] [CrossRef]
- Iwasaki, S.; Iwasaki, W.; Takahashi, M.; Sakamoto, A.; Watanabe, C.; Shichino, Y.; Floor, S.; Fujiwara, K.; Mito, M.; Dodo, K.; et al. The Translation Inhibitor Rocaglamide Targets a Bimolecular Cavity between eIF4A and Polypurine RNA. Mol. Cell 2019, 73, 738–748. [Google Scholar] [CrossRef]
- Cencic, R.; Carrier, M.; Galicia-Vázquez, G.; Bordeleau, M.-E.; Sukarieh, R.; Bourdeau, A.; Brem, B.; Teodoro, J.G.; Greger, H.; Tremblay, M.L.; et al. Antitumor Activity and Mechanism of Action of the Cyclopenta[b]benzofuran, Silvestrol. PLoS ONE 2009, 4, e5223. [Google Scholar] [CrossRef]
- Müller, D.; Shin, S.; De Rugy, T.G.; Samain, R.; Baer, R.; Strehaiano, M.; Masvidal-Sanz, L.; Guillermet-Guibert, J.; Jean, C.; Tsukumo, Y.; et al. eIF4A inhibition circumvents uncontrolled DNA replication mediated by 4E-BP1 loss in pancreatic cancer. JCI Insight 2019, 4. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Chu, J.; Cyr, A.M.; Yueh, H.; Brown, L.E.; Wang, T.T.; Pelletier, J.; Porco, J.A. Intercepted Retro-Nazarov Reaction: Syntheses of Amidino-Rocaglate Derivatives and Their Biological Evaluation as eIF4A Inhibitors. J. Am. Chem. Soc. 2019, 141, 12891–12900. [Google Scholar] [CrossRef] [PubMed]
- Chu, J.; Zhang, W.; Cencic, R.; Devine, W.G.; Beglov, D.; Henkel, T.; Brown, L.E.; Vajda, S.; Porco, J.A.; Pelletier, J. Amidino-Rocaglates: A Potent Class of eIF4A Inhibitors. Cell Chem. Boil. 2019, 26, 1586–1593. [Google Scholar] [CrossRef] [PubMed]
- Ernst, J.T.; Thompson, P.A.; Nilewski, C.; Sprengeler, P.A.; Sperry, S.; Packard, G.; Michels, T.; Xiang, A.; Tran, C.; Wegerski, C.J.; et al. Design of Development Candidate eFT226, a First in Class Inhibitor of Eukaryotic Initiation Factor 4A RNA Helicase. J. Med. Chem. 2020, 63, 5879–5955. [Google Scholar] [CrossRef] [PubMed]
- Ashburn, T.T.; Thor, K.B. Drug repositioning: Identifying and developing new uses for existing drugs. Nat. Rev. Drug Discov. 2004, 3, 673–683. [Google Scholar] [CrossRef]
- Holmes, M.D.; Chen, W.Y. Hiding in plain view: The potential for commonly used drugs to reduce breast cancer mortality. Breast Cancer Res. 2012, 14, 216. [Google Scholar] [CrossRef]
- Wolfe, A.L.; Singh, K.; Zhong, Y.; Drewe, P.; Rajasekhar, V.K.; Sanghvi, V.R.; Mavrakis, K.J.; Jiang, M.; Roderick, J.E.; Van Der Meulen, J.; et al. RNA G-quadruplexes cause eIF4A-dependent oncogene translation in cancer. Nature 2014, 513, 65–70. [Google Scholar] [CrossRef]
- Waldron, J.A.; Raza, F.; Le Quesne, J. eIF4A alleviates the translational repression mediated by classical secondary structures more than by G-quadruplexes. Nucleic Acids Res. 2018, 46, 3075–3087. [Google Scholar] [CrossRef]
- Waldron, J.A.; Tack, D.C.; Ritchey, L.E.; Gillen, S.L.; Wilczynska, A.; Turro, E.; Bevilacqua, P.C.; Assmann, S.M.; Bushell, M.; Le Quesne, J. mRNA structural elements immediately upstream of the start codon dictate dependence upon eIF4A helicase activity. Genome Boil. 2019, 20, 300–323. [Google Scholar] [CrossRef]
- Prassas, I.; Diamandis, E.P. Novel therapeutic applications of cardiac glycosides. Nat. Rev. Drug Discov. 2008, 7, 926–935. [Google Scholar] [CrossRef]
- Samanta, D.; Gilkes, D.M.; Chaturvedi, P.; Xiang, L.; Semenza, G.L. Hypoxia-inducible factors are required for chemotherapy resistance of breast cancer stem cells. Proc. Natl. Acad. Sci. USA 2014, 111, E5429–E5438. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Lonard, D.M.; Yu, Y.; Chow, D.-C.; Palzkill, T.G.; Wang, J.; Qi, R.; Matzuk, A.J.; Song, X.; Madoux, F.; et al. Bufalin is a potent small-molecule inhibitor of the steroid receptor coactivators SRC-3 and SRC-1. Cancer Res. 2014, 74, 1506–1517. [Google Scholar] [CrossRef] [PubMed]
- Xie, C.-M.; Lin, X.-T.; Wu, D.; Tan, Y.; Cheng, C.; Zhang, J. Cardiac glycoside bufalin blocks cancer cell growth by inhibition of Aurora A and Aurora B activation via PI3K-Akt pathway. Oncotarget 2018, 9, 13783–13795. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Perne, A.; Muellner, M.K.; Steinrueck, M.; Craig-Mueller, N.; Mayerhofer, J.; Schwarzinger, I.; Sloane, M.; Uras, I.Z.; Hoermann, G.; Nijman, S.M.B.; et al. Cardiac Glycosides Induce Cell Death in Human Cells by Inhibiting General Protein Synthesis. PLoS ONE 2009, 4, e8292. [Google Scholar] [CrossRef]
- Ouyang, X.; Han, S.N.; Zhang, J.Y.; Dioletis, E.; Nemeth, B.T.; Pacher, P.; Feng, D.; Bataller, R.; Cabezas, J.; Starkel, P.; et al. Digoxin Suppresses Pyruvate Kinase M2-Promoted HIF-1alpha Transactivation in Steatohepatitis. Cell Metab. 2018, 27, 339–350. [Google Scholar] [CrossRef]
- Karas, K.; Salkowska, A.; Sobalska-Kwapis, M.; Walczak-Drzewiecka, A.; Strapagiel, D.; Dastych, J.; Bachorz, R.A.; Ratajewski, M. Digoxin, an Overlooked Agonist of RORgamma/RORgammaT. Front. Pharmacol. 2018, 9, 1460. [Google Scholar] [CrossRef]
- Didiot, M.-C.; Hewett, J.; Varin, T.; Freuler, F.; Selinger, D.; Nick, H.; Reinhardt, J.; Buckler, A.; Myer, V.; Schuffenhauer, A.; et al. Identification of Cardiac Glycoside Molecules as Inhibitors of c-Myc IRES-Mediated Translation. J. Biomol. Screen. 2013, 18, 407–419. [Google Scholar] [CrossRef]
- Steinberger, J.; Robert, F.; Hallé, M.; Williams, D.E.; Cencic, R.; Sawhney, N.; Pelletier, D.; Williams, P.; Igarashi, Y.; Porco, J.A.; et al. Tracing MYC Expression for Small Molecule Discovery. Cell Chem. Boil. 2019, 26, 699–710. [Google Scholar] [CrossRef]
- Polunovsky, V.A.; Rosenwald, I.B.; Tan, A.T.; White, J.; Chiang, L.; Sonenberg, N.; Bitterman, P.B. Translational control of programmed cell death: Eukaryotic translation initiation factor 4E blocks apoptosis in growth-factor-restricted fibroblasts with physiologically expressed or deregulated Myc. Mol. Cell. Boil. 1996, 16, 6573–6581. [Google Scholar] [CrossRef]
- Ruggero, D.; Montanaro, L.; Ma, L.; Xu, W.; Londei, P.; Cordon-Cardo, C.; Pandolfi, P.P. The translation factor eIF-4E promotes tumor formation and cooperates with c-Myc in lymphomagenesis. Nat. Med. 2004, 10, 484–486. [Google Scholar] [CrossRef]
- Lin, C.-J.; Cencic, R.; Mills, J.R.; Robert, F.; Pelletier, J. c-Myc and eIF4F Are Components of a Feedforward Loop that Links Transcription and Translation. Cancer Res. 2008, 68, 5326–5334. [Google Scholar] [CrossRef] [PubMed]
- Hart, J.R.; Garner, A.L.; Yu, J.; Ito, Y.; Sun, M.; Ueno, L.; Rhee, J.-K.; Baksh, M.M.; Stefan, E.; Hartl, M.; et al. Inhibitor of MYC identified in a Krohnke pyridine library. Proc. Natl. Acad. Sci. USA 2014, 111, 12556–12561. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Liu, H.; Qing, G. Targeting oncogenic Myc as a strategy for cancer treatment. Signal Transduct. Target. Ther. 2018, 3, 5. [Google Scholar] [CrossRef] [PubMed]
- Karasneh, R.A.; Murray, L.J.; McMenamin, Ú.; Hughes, C.M.; Cardwell, C.R. Digoxin use after diagnosis of breast cancer and survival: A population-based cohort study. Breast Cancer Res. Treat. 2015, 151, 661–669. [Google Scholar] [CrossRef] [PubMed]
- Clifford, R.J.; Kaplan, J.H. Human Breast Tumor Cells Are More Resistant to Cardiac Glycoside Toxicity Than Non-Tumorigenic Breast Cells. PLoS ONE 2013, 8, e84306. [Google Scholar] [CrossRef] [PubMed]
- Tan, A.; Bitterman, P.B.; Sonenberg, N.; Peterson, M.; Polunovsky, V. Inhibition of Myc-dependent apoptosis by eukaryotic translation initiation factor 4E requires cyclin D1. Oncogene 2000, 19, 1437–1447. [Google Scholar] [CrossRef][Green Version]
- Simpson, C.D.; Mawji, I.A.; Anyiwe, K.; Williams, M.A.; Wang, X.; Venugopal, A.L.; Gronda, M.; Hurren, R.; Cheng, S.; Serra, S.; et al. Inhibition of the Sodium Potassium Adenosine Triphosphatase Pump Sensitizes Cancer Cells to Anoikis and Prevents Distant Tumor Formation. Cancer Res. 2009, 69, 2739–2747. [Google Scholar] [CrossRef]
- Lin, S.-Y.; Chang, H.-H.; Lai, Y.-H.; Lin, C.-H.; Chen, M.-H.; Chang, G.-C.; Tsai, M.-F.; Chen, J.J.W. Digoxin Suppresses Tumor Malignancy through Inhibiting Multiple Src-Related Signaling Pathways in Non-Small Cell Lung Cancer. PLoS ONE 2015, 10, e0123305. [Google Scholar] [CrossRef]
- Wang, Z.; Zheng, M.; Li, Z.; Li, R.; Jia, L.; Xiong, X.; Southall, N.; Wang, S.; Xia, M.; Austin, C.P.; et al. Cardiac glycosides inhibit p53 synthesis by a mechanism relieved by Src or MAPK inhibition. Cancer Res. 2009, 69, 6556–6564. [Google Scholar] [CrossRef]
- Triana-Martínez, F.; Picallos-Rabina, P.; Da Silva-Álvarez, S.; Pietrocola, F.; Llanos, S.; Rodilla, V.; Soprano, E.; Pedrosa, P.; Ferreirós, A.; Barradas, M.; et al. Identification and characterization of Cardiac Glycosides as senolytic compounds. Nat. Commun. 2019, 10, 1–12. [Google Scholar] [CrossRef]
- Schito, L.; Rey, S.; Tafani, M.; Zhang, H.; Wong, C.C.-L.; Russo, A.; Russo, M.A.; Semenza, G.L. Hypoxia-inducible factor 1-dependent expression of platelet-derived growth factor B promotes lymphatic metastasis of hypoxic breast cancer cells. Proc. Natl. Acad. Sci. USA 2012, 109, E2707–E2716. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Zhou, Y.; Peng, J.; Xie, B.; Shou, Q.; Wang, J. Silencing c-Myc Enhances the Antitumor Activity of Bufalin by Suppressing the HIF-1α/SDF-1/CXCR4 Pathway in Pancreatic Cancer Cells. Front. Pharmacol. 2020, 11, 495. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, E.V. The role of c-myc in regulation of translation initiation. Oncogene 2004, 23, 3217–3221. [Google Scholar] [CrossRef] [PubMed]
- Stoelzle, T.; Schwarb, P.; Trumpp, A.; Hynes, N.E. c-Myc affects mRNA translation, cell proliferation and progenitor cell function in the mammary gland. BMC Boil. 2009, 7, 63. [Google Scholar] [CrossRef]
- Ruggero, D. The role of Myc-induced protein synthesis in cancer. Cancer Res. 2009, 69, 8839–8843. [Google Scholar] [CrossRef] [PubMed]
- Lazaris-Karatzas, A.; Sonenberg, N. The mRNA 5’ cap-binding protein, eIF-4E, cooperates with v-myc or E1A in the transformation of primary rodent fibroblasts. Mol. Cell. Boil. 1992, 12, 1234–1238. [Google Scholar] [CrossRef]
- Lin, C.-J.; Nasr, Z.; Premsrirut, P.K.; Porco, J.A.; Hippo, Y.; Lowe, S.W.; Pelletier, J. Targeting Synthetic Lethal Interactions between Myc and the eIF4F Complex Impedes Tumorigenesis. Cell Rep. 2012, 1, 325–333. [Google Scholar] [CrossRef]
- Pourdehnad, M.; Truitt, M.L.; Siddiqi, I.N.; Ducker, G.S.; Shokat, K.M.; Ruggero, D. Myc and mTOR converge on a common node in protein synthesis control that confers synthetic lethality in Myc-driven cancers. Proc. Natl. Acad. Sci. USA 2013, 110, 11988–11993. [Google Scholar] [CrossRef]
- Xu, Y.; Poggio, M.; Jin, H.Y.; Shi, Z.; Forester, C.M.; Wang, Y.; Stumpf, C.R.; Xue, L.; Devericks, E.; So, L.; et al. Translation control of the immune checkpoint in cancer and its therapeutic targeting. Nat. Med. 2019, 25, 301–311. [Google Scholar] [CrossRef]
- Tameire, F.; Verginadis, I.I.; Leli, N.M.; Polte, C.; Conn, C.S.; Ojha, R.; Salinas, C.S.; Chinga, F.; Monroy, A.M.; Fu, W.; et al. ATF4 couples MYC-dependent translational activity to bioenergetic demands during tumour progression. Nat. Cell. Biol. 2019, 21, 889–899. [Google Scholar] [CrossRef]
- McBryan, J.; Theissen, S.M.; Byrne, C.; Hughes, E.; Cocchiglia, S.; Sande, S.; O’Hara, J.; Tibbitts, P.; Hill, A.D.; Young, L. Metastatic Progression with Resistance to Aromatase Inhibitors Is Driven by the Steroid Receptor Coactivator SRC-1. Cancer Res. 2011, 72, 548–559. [Google Scholar] [CrossRef] [PubMed]
- Osman, M.H.; Farrag, E.; Selim, M.; Hasanine, A.; Selim, A.; Osman, M.S. Cardiac glycosides use and the risk and mortality of cancer; systematic review and meta-analysis of observational studies. PLoS ONE 2017, 12, e0178611. [Google Scholar] [CrossRef] [PubMed]
- Biggar, R.J.; Wohlfahrt, J.; Oudin, A.; Hjuler, T.; Melbye, M. Digoxin Use and the Risk of Breast Cancer in Women. J. Clin. Oncol. 2011, 29, 2165–2170. [Google Scholar] [CrossRef] [PubMed]
- Duvall-Noelle, N.; Karwandyar, A.; Richmond, A.; Raman, D. LASP-1: A nuclear hub for the UHRF1-DNMT1-G9a-Snail1 complex. Oncogene 2015, 35, 1122–1133. [Google Scholar] [CrossRef]
- Johnson, R.W.; Nguyen, M.P.; Padalecki, S.S.; Grubbs, B.G.; Merkel, A.R.; Oyajobi, B.O.; Matrisian, L.M.; Mundy, G.R.; Sterling, J.A. TGF-beta promotion of Gli2-induced expression of parathyroid hormone-related protein, an important osteolytic factor in bone metastasis, is independent of canonical Hedgehog signaling. Cancer Res. 2010, 71, 822–831. [Google Scholar] [CrossRef]
- Howard, C.M.; Bearss, N.; Subramaniyan, B.; Tilley, A.; Sridharan, S.; Villa, N.; Fraser, C.S.; Raman, D. The CXCR4-LASP1-eIF4F Axis Promotes Translation of Oncogenic Proteins in Triple-Negative Breast Cancer Cells. Front. Oncol. 2019, 9, 284. [Google Scholar] [CrossRef]
- Chou, T.-C. Drug Combination Studies and Their Synergy Quantification Using the Chou-Talalay Method. Cancer Res. 2010, 70, 440–446. [Google Scholar] [CrossRef]

| Term | Overlap | p-Value | Adjusted p-Value | Old p-Value | Old Adjusted p-Value | Odds Ratio | Combined Score |
|---|---|---|---|---|---|---|---|
| MYC oe MCF7 human gse101738 RNAseq down | 11/159 | 4.36 × 10−10 | 8.54 × 10−7 | 0 | 0 | 13.83647799 | 298.2241 |
| SREBF2 KD human gse50588 creedsid gene 2823 up | 12/294 | 2.70 × 10−8 | 2.64 × 10−5 | 0 | 0 | 8.163265306 | 142.2611 |
| STAT3 KD human gse42979 creedsid gene 2148 down | 12/309 | 4.67 × 10−8 | 3.05 × 10−5 | 0 | 0 | 7.766990291 | 131.1075 |
| HEY2 KO mouse gse6526 creedsid gene 1511 up | 9/205 | 8.91 × 10−7 | 3.49 × 10−4 | 0 | 0 | 8.780487805 | 122.3245 |
| HEY2 KO mouse gse6526 creedsid gene 1512 down | 9/205 | 8.91 × 10−7 | 2.91 × 10−4 | 0 | 0 | 8.780487805 | 122.3245 |
| Term | Overlap | p-Value | Adjusted p-Value | Old p-Value | Old Adjusted p-Value | Odds Ratio | Combined Score |
|---|---|---|---|---|---|---|---|
| MYC oe MCF7 human gse101738 RNAseq down | 8/159 | 1.34 × 10−6 | 8.74 × 10−4 | 0 | 0 | 10.0628931 | 136.0840 |
| ZNF143 siRNA MCF7 human gse76453 RNAseq down | 10/233 | 2.63 × 10−7 | 5.15 × 10−4 | 0 | 0 | 8.58369099 | 130.0552 |
| STAT3 deficiency mouse gse6846 creedsid gene 85 down | 10/246 | 4.33 × 10−7 | 4.24 × 10−4 | 0 | 0 | 8.1300813 | 119.1174 |
| FOXO1 KD mouse gse6623 creedsid gene 505 down | 8/195 | 6.12 × 10−6 | 0.001711 | 0 | 0 | 8.20512821 | 98.4977 |
| SREBF2 KD human gse50588 creedsid gene 2823 up | 10/294 | 2.18 × 10−6 | 8.54 × 10−4 | 0 | 0 | 6.80272109 | 88.6777 |
| Gene | Factor Name | Start Position | End Position | Dissimilarity | String | Random Expectation Equally | Random Expectation Query |
|---|---|---|---|---|---|---|---|
| eIF4A | c-MYC (T00140) | ||||||
| 204 | 209 | 0.000000 | CACGTG | 0.14648 | 0.19526 | ||
| eIF4E | |||||||
| 266 | 271 | 0.000000 | CACGTG | 0.14648 | 0.16595 | ||
| 419 | 424 | 0.000000 | CACGTG | 0.14648 | 0.16595 | ||
| eIF4G | |||||||
| 355 | 360 | 0.000000 | CACGTG | 0.14648 | 0.18917 | ||
| 432 | 437 | 0.000000 | CACGTG | 0.14648 | 0.18917 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Howard, C.M.; Estrada, M.; Terrero, D.; Tiwari, A.K.; Raman, D. Identification of Cardiac Glycosides as Novel Inhibitors of eIF4A1-Mediated Translation in Triple-Negative Breast Cancer Cells. Cancers 2020, 12, 2169. https://doi.org/10.3390/cancers12082169
Howard CM, Estrada M, Terrero D, Tiwari AK, Raman D. Identification of Cardiac Glycosides as Novel Inhibitors of eIF4A1-Mediated Translation in Triple-Negative Breast Cancer Cells. Cancers. 2020; 12(8):2169. https://doi.org/10.3390/cancers12082169
Chicago/Turabian StyleHoward, Cory M., Matthew Estrada, David Terrero, Amit K. Tiwari, and Dayanidhi Raman. 2020. "Identification of Cardiac Glycosides as Novel Inhibitors of eIF4A1-Mediated Translation in Triple-Negative Breast Cancer Cells" Cancers 12, no. 8: 2169. https://doi.org/10.3390/cancers12082169
APA StyleHoward, C. M., Estrada, M., Terrero, D., Tiwari, A. K., & Raman, D. (2020). Identification of Cardiac Glycosides as Novel Inhibitors of eIF4A1-Mediated Translation in Triple-Negative Breast Cancer Cells. Cancers, 12(8), 2169. https://doi.org/10.3390/cancers12082169






