Real-World Data on Thromboprophylaxis in Active Cancer Patients: Where Are We? Are We Getting There?
Abstract
1. Introduction
2. Results
2.1. Baseline Characteristics of Patients
2.2. Risk Assissment for CAT
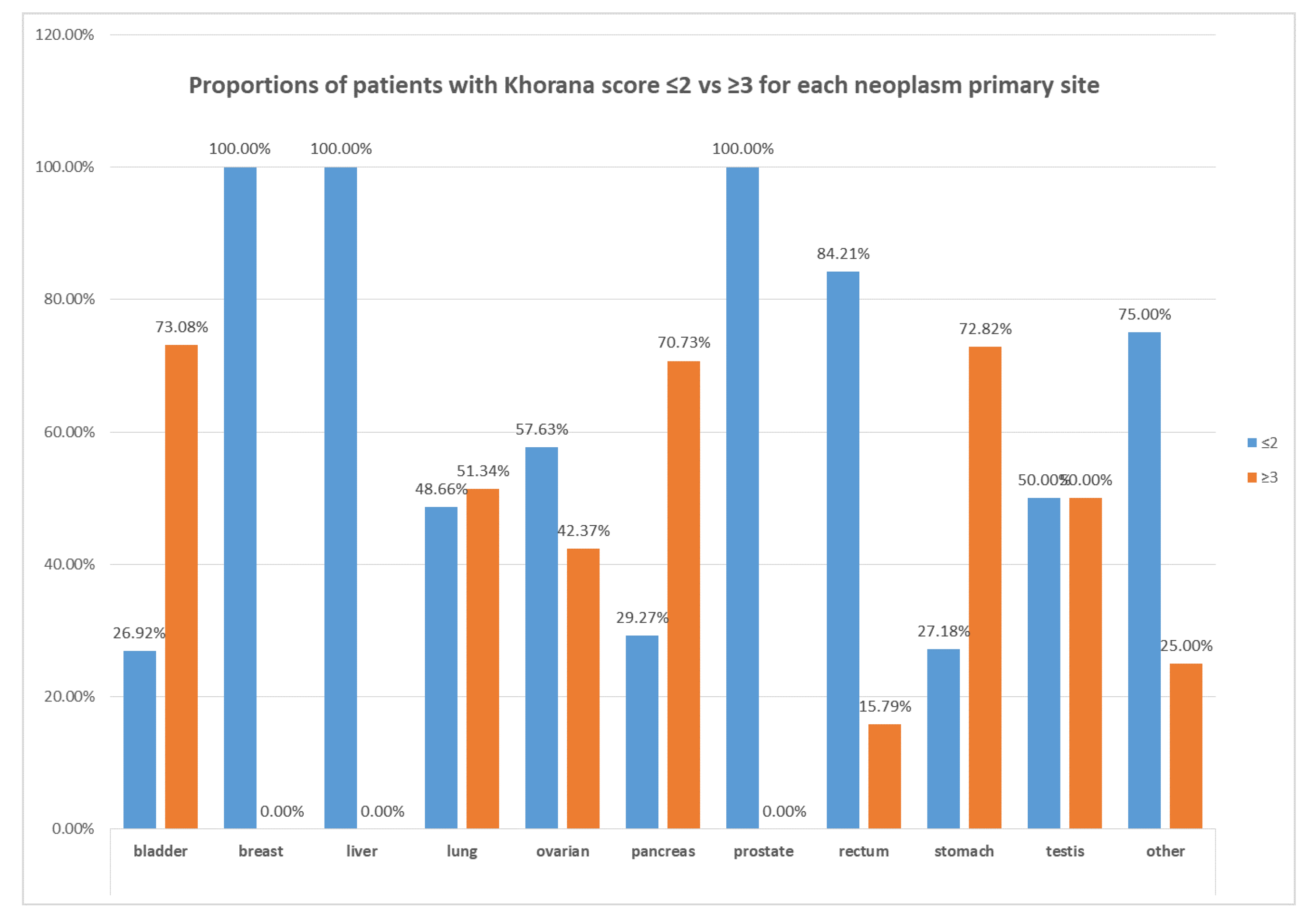
2.3. Stratification of Patients According to the Khorana Score
2.4. Characteristics of Patients with Khorana Score ≤2
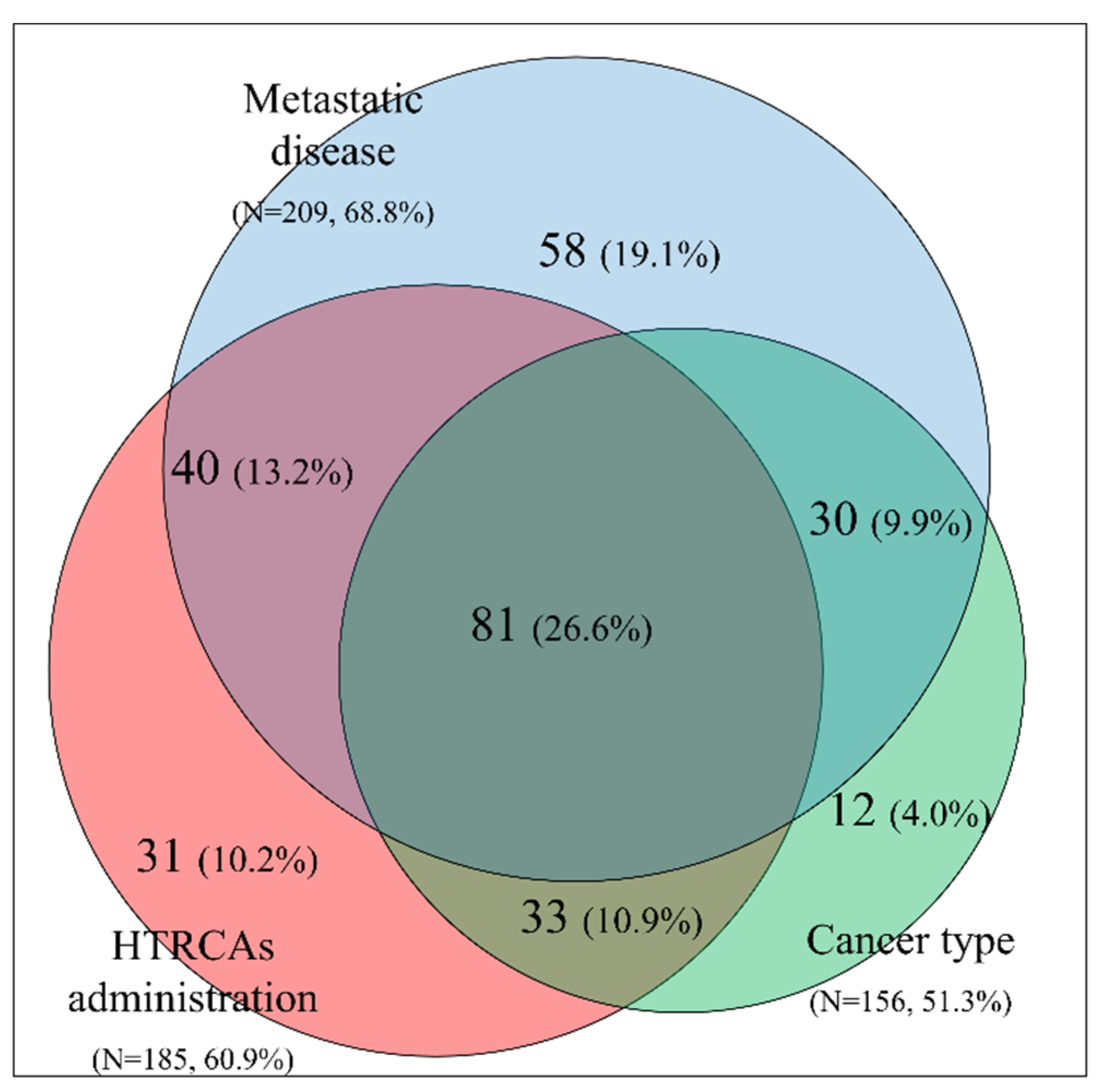
2.5. Clinical Features Influencing the Decision to Administer Thromboprophylaxis for Patients with Khorana Score ≤2
2.6. Thromboprophylaxis Regiments, Doses and Duration
2.7. Thrombotic and Bleeding Events
3. Discussion
4. Materials and Methods
Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Patients Characteristics | Value |
|---|---|
| Number of patients | 304 |
| Male (%) | 50.7% |
| Age (mean ± SD) | 65.5 ± 11.3 |
| Lung | 72 (23.7%) |
| Breast | 37 (12.2%) |
| Colorectal | 30 (9.9%) |
| Ovarian | 25 (8.2%) |
| Pancreas | 24 (7.9%) |
| Stomach | 14 (4.6%) |
| Prostate | 14 (4.6%) |
| Bladder | 12 (4.0%) |
| Testis | 4 (1.3%) |
| Other* | 72 (23.7%) |
| Patients Characteristics | Value |
|---|---|
| BMI (mean ± SD) | 26.1 ± 4.8 |
| BMI ≥ 35 kg/m2 | 3.6% |
| Anemia (Hg <10 g/L) | 12.5% |
| PLT count ≥ 350 × 109/L | 20.6% |
| Leucocytes count > 11 × 109/L | 11.2% |
| Erythropoietin use | 15.6% |
| Metastatic disease | 68.8% |
| HTRCAs | 60.9% |
| Khorana score ≤ 1 | 47.0% |
| Khorana score = 2 | 53.0% |
| Parameter | p-Value | OR | LCL | UCL |
|---|---|---|---|---|
| Gender (Female vs. Male) | 0.5170 | 1.4 | 0.5 | 3.9 |
| Age (<65 years vs higher) | 0.2162 | 0.5 | 0.2 | 1.5 |
| BMI (<35 kg/m2 vs. higher) | 0.0018 | 5.6 | 1.7 | 18.8 |
| Smoking (No vs. Yes) | 0.2014 | 2.1 | 0.7 | 6.6 |
| History of thrombosis (No vs. Yes) | 0.1919 | 3.8 | 0.4 | 33.0 |
| History of trauma (No vs. Yes) | 0.0362 | 4.7 | 0.96 | 23.0 |
| History of surgery (No vs. Yes) | 0.3796 | 1.6 | 0.6 | 4.3 |
| History of comorbidities (No vs. Yes) | 0.7005 | 1.2 | 0.4 | 3.6 |
| Hospitalized Patient (No vs. Yes) | 0.0525 | 3.1 | 0.9 | 10.2 |
| Metastasis (No vs. Yes) | 0.7410 | 0.8 | 0.3 | 2.5 |
| Radiotherapy (No vs. Yes) | 0.3795 | 1.6 | 0.6 | 4.5 |
| HTRCAs (No vs. Yes) | 0.8886 | 1.1 | 0.4 | 3.1 |
| Agents for Erythropoiesis (No vs. Yes) | 0.0682 | Not applicable, one group had zero observations | ||
| Leukocyte Count (pre chemotherapy) (Low vs. High) | 0.4697 | 1.5 | 0.5 | 4.4 |
| Hemoglobin (High vs. Low) | 0.0403 | All thrombotic cases had high hemoglobin | ||
| PLT Count High (pre chemotherapy) | 0.6221 | 0.8 | 0.3 | 2.2 |
| Khorana Score (≤2 vs. ≥3) | 0.7428 | 0.8 | 0.3 | 2.6 |
| Agent for anticoagulation (prophylactic vs. higher dose) | 0.0413 | 0.3 | 0.1 | 1.0 |
| Parameter | p-Value | OR | LCL | UCL |
|---|---|---|---|---|
| Gender (Femalevs. Male) | 0.1544 | 0.2 | 0.1 | 2.0 |
| Age (<65 years vs. higher) | 0.0353 | 7.3 | 0.8 | 62.9 |
| BMI (<35 kg/m2 vs. higher) | 0.2957 | 0.3 | 0.04 | 2.99 |
| Smoking (Novs. Yes) | 0.2332 | 0.3 | 0.03 | 1.39 |
| History of thrombosis (No vs. Yes) | 0.0075 | 0.1 | 0.01 | 0.9 |
| History of trauma (No vs. Yes) | 0.6481 | Not applicable, one group had zero observations | ||
| History of surgery (No vs. Yes) | 0.5461 | 1.7 | 0.3 | 9.3 |
| History of comorbidities (No vs. Yes) | 0.2027 | 0.4 | 0.1 | 1.8 |
| History of renal Insufficiency (No vs. Yes) | 0.1271 | 0.2 | 0.02 | 1.9 |
| History of bleeding (No vs. Yes) | 0.8655 | Not applicable, one group had zero observations | ||
| Hospitalized Patient (No vs. Yes) | 0.3804 | Not applicable, one group had zero observations | ||
| Metastasis (No vs. Yes) | 0.5452 | 0.5 | 0.1 | 4.5 |
| Radiotherapy (No vs. Yes) | 0.5383 | 1.9 | 0.2 | 16.8 |
| HTRCAs (No vs. Yes) | 0.3681 | 2.1 | 0.4 | 10.4 |
| Use of Agents for Erythropoiesis (No vs. Yes) | 0.2699 | Not applicable, one group had zero observations | ||
| Leukocyte Count (pre chemotherapy) (Low vs. High) | 0.0127 | 0.2 | 0.03 | 0.8 |
| Hemoglobin (High vs. Low) | 0.2147 | Not Applicable | ||
| PLT Count High (pre chemotherapy) | 0.1309 | 0.3 | 0.05 | 1.6 |
| Khorana Score (≤2 vs. ≥3) | 0.0028 | 0.1 | 0.01 | 0.7 |
| Agent for anticoagulation (prophylactic vs. higher dose) | 0.0248 | Not applicable, one group had zero observations | ||
References
- Trousseau, A. Phlegmatia Alba Dolens, 2nd ed.; J.-B. Baillière et fils: Paris, France, 1865; Volume 3. [Google Scholar]
- Agnelli, G.; Verso, M. Management of venous thromboembolism in patients with cancer. J. Thromb. Haemost. 2011, 9, 316–324. [Google Scholar] [CrossRef]
- Elyamany, G.; Alzahrani, A.M.; Bukhary, E. Cancer-associated thrombosis: An overview. Clin. Med. Insights Oncol. 2014, 8, 129–137. [Google Scholar] [CrossRef]
- Van Es, N.; Le Gal, G.; Otten, H.M.; Robin, P.; Piccioli, A.; Lecumberri, R.; Jara-Palomares, L.; Religa, P.; Rieu, V.; Rondina, M.; et al. Screening for Occult Cancer in Patients With Unprovoked Venous Thromboembolism: A Systematic Review and Meta-analysis of Individual Patient Data. Ann. Intern. Med. 2017, 167, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Carrier, M.; Lazo-Langner, A.; Shivakumar, S.; Tagalakis, V.; Zarychanski, R.; Solymoss, S.; Routhier, N.; Douketis, J.; Danovitch, K.; Lee, A.Y.; et al. Screening for Occult Cancer in Unprovoked Venous Thromboembolism. N. Engl. J. Med. 2015, 373, 697–704. [Google Scholar] [CrossRef]
- Falanga, A.; Marchetti, M.; Russo, L. The mechanisms of cancer-associated thrombosis. Thromb. Res. 2015, 135, S8–S11. [Google Scholar] [CrossRef]
- Falanga, A.; Russo, L.; Milesi, V.; Vignoli, A. Mechanisms and risk factors of thrombosis in cancer. Crit. Rev. Oncol./Hematol. 2017, 118, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Abdol Razak, N.B.; Jones, G.; Bhandari, M.; Berndt, M.C.; Metharom, P. Cancer-Associated Thrombosis: An Overview of Mechanisms, Risk Factors, and Treatment. Cancers 2018, 10, 380. [Google Scholar] [CrossRef]
- Previtali, E.; Bucciarelli, P.; Passamonti, S.M.; Martinelli, I. Risk factors for venous and arterial thrombosis. Blood Transfus. 2011, 9, 120–138. [Google Scholar] [CrossRef]
- Lowe, G.D. Common risk factors for both arterial and venous thrombosis. Br. J. Haematol. 2008, 140, 488–495. [Google Scholar] [CrossRef] [PubMed]
- Haddad, T.C.; Greeno, E.W. Chemotherapy-induced thrombosis. Thromb. Res. 2006, 118, 555–568. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Zhou, B.P. Inflammation: A driving force speeds cancer metastasis. Cell Cycle 2009, 8, 3267–3273. [Google Scholar] [CrossRef] [PubMed]
- Sethi, G.; Shanmugam, M.K.; Ramachandran, L.; Kumar, A.P.; Tergaonkar, V. Multifaceted link between cancer and inflammation. Biosci. Rep. 2012, 32, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Piazza, G.; Ridker, P.M. Is venous thromboembolism a chronic inflammatory disease? Clin. Chem. 2015, 61, 313–316. [Google Scholar] [CrossRef] [PubMed]
- Franco, A.T.; Corken, A.; Ware, J. Platelets at the interface of thrombosis, inflammation, and cancer. Blood 2015, 126, 582–588. [Google Scholar] [CrossRef] [PubMed]
- Morrell, C.N.; Hilt, Z.T.; Pariser, D.N.; Maurya, P. PAD4 and von Willebrand Factor Link Inflammation and Thrombosis. Circ. Res. 2019, 125, 520–522. [Google Scholar] [CrossRef]
- Chen, J.; Chung, D.W. Inflammation, von Willebrand factor, and ADAMTS13. Blood 2018, 132, 141–147. [Google Scholar] [CrossRef]
- Mandala, M.; Reni, M.; Cascinu, S.; Barni, S.; Floriani, I.; Cereda, S.; Berardi, R.; Mosconi, S.; Torri, V.; Labianca, R. Venous thromboembolism predicts poor prognosis in irresectable pancreatic cancer patients. Ann. Oncol. Off. J. Eur. Soc. Med Oncol. ESMO 2007, 18, 1660–1665. [Google Scholar] [CrossRef]
- Khorana, A.A.; Kuderer, N.M.; Culakova, E.; Lyman, G.H.; Francis, C.W. Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 2008, 111, 4902–4907. [Google Scholar] [CrossRef]
- Key, N.S.; Khorana, A.A.; Kuderer, N.M.; Bohlke, K.; Lee, A.Y.Y.; Arcelus, J.I.; Wong, S.L.; Balaban, E.P.; Flowers, C.R.; Francis, C.W.; et al. Venous Thromboembolism Prophylaxis and Treatment in Patients With Cancer: ASCO Clinical Practice Guideline Update. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2020, 38, 496–520. [Google Scholar] [CrossRef]
- Oppelt, P.; Betbadal, A.; Nayak, L. Approach to chemotherapy-associated thrombosis. Vasc. Med. 2015, 20, 153–161. [Google Scholar] [CrossRef]
- Qi, W.X.; Lin, F.; Sun, Y.J.; Tang, L.N.; Shen, Z.; Yao, Y. Risk of venous and arterial thromboembolic events in cancer patients treated with gemcitabine: A systematic review and meta-analysis. Br. J. Clin. Pharmacol. 2013, 76, 338–347. [Google Scholar] [CrossRef]
- Ay, C.; Pabinger, I.; Cohen, A.T. Cancer-associated venous thromboembolism: Burden, mechanisms, and management. Thromb. Haemost. 2017, 117, 219–230. [Google Scholar] [CrossRef]
- Kuderer, N.M.; Culakova, E.; Lyman, G.H.; Francis, C.; Falanga, A.; Khorana, A.A. A Validated Risk Score for Venous Thromboembolism Is Predictive of Cancer Progression and Mortality. Oncologist 2016, 21, 861–867. [Google Scholar] [CrossRef] [PubMed]
- Ay, C.; Dunkler, D.; Marosi, C.; Chiriac, A.L.; Vormittag, R.; Simanek, R.; Quehenberger, P.; Zielinski, C.; Pabinger, I. Prediction of venous thromboembolism in cancer patients. Blood 2010, 116, 5377–5382. [Google Scholar] [CrossRef]
- Mulder, F.I.; Candeloro, M.; Kamphuisen, P.W.; Di Nisio, M.; Bossuyt, P.M.; Guman, N.; Smit, K.; Buller, H.R.; van Es, N. The Khorana score for prediction of venous thromboembolism in cancer patients: A systematic review and meta-analysis. Haematologica 2019, 104, 1277–1287. [Google Scholar] [CrossRef]
- Van Es, N.; Franke, V.F.; Middeldorp, S.; Wilmink, J.W.; Buller, H.R. The Khorana score for the prediction of venous thromboembolism in patients with pancreatic cancer. Thromb. Res. 2017, 150, 30–32. [Google Scholar] [CrossRef] [PubMed]
- Elalamy, I.; Canon, J.L.; Bols, A.; Lybaert, W.; Duck, L.; Jochmans, K.; Bosquée, L.; Peeters, M.; Awada, A.H.; Clement, P.; et al. Thrombo-Embolic Events in Cancer Patients with Impaired Renal Function. J. Blood Disord. Transf. 2014, 5, 1–5. [Google Scholar] [CrossRef]
- Maraveyas, A.; Waters, J.; Roy, R.; Fyfe, D.; Propper, D.; Lofts, F.; Sgouros, J.; Gardiner, E.; Wedgwood, K.; Ettelaie, C.; et al. Gemcitabine versus gemcitabine plus dalteparin thromboprophylaxis in pancreatic cancer. Eur. J. Cancer 2012, 48, 1283–1292. [Google Scholar] [CrossRef] [PubMed]
- Pelzer, U.; Opitz, B.; Deutschinoff, G.; Stauch, M.; Reitzig, P.C.; Hahnfeld, S.; Muller, L.; Grunewald, M.; Stieler, J.M.; Sinn, M.; et al. Efficacy of Prophylactic Low-Molecular Weight Heparin for Ambulatory Patients With Advanced Pancreatic Cancer: Outcomes From the CONKO-004 Trial. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2015, 33, 2028–2034. [Google Scholar] [CrossRef]
- Thein, K.Z.; Yeung, S.J.; Oo, T.H. Primary thromboprophylaxis (PTP) in ambulatory patients with lung cancer receiving chemotherapy: A systematic review and meta-analysis of randomized controlled trials (RCTs). Asia-Pac. J. Clin. Oncol. 2018, 14, 210–216. [Google Scholar] [CrossRef]
- Khorana, A.A.; Francis, C.W.; Kuderer, N.M.; Carrier, M.; Ortel, T.L.; Wun, T.; Rubens, D.; Hobbs, S.; Iyer, R.; Peterson, D.; et al. Dalteparin thromboprophylaxis in cancer patients at high risk for venous thromboembolism: A randomized trial. Thromb. Res. 2017, 151, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Agnelli, G.; George, D.J.; Kakkar, A.K.; Fisher, W.; Lassen, M.R.; Mismetti, P.; Mouret, P.; Chaudhari, U.; Lawson, F.; Turpie, A.G.; et al. Semuloparin for thromboprophylaxis in patients receiving chemotherapy for cancer. N. Engl. J. Med. 2012, 366, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Barni, S.; Labianca, R.; Agnelli, G.; Bonizzoni, E.; Verso, M.; Mandala, M.; Brighenti, M.; Petrelli, F.; Bianchini, C.; Perrone, T.; et al. Chemotherapy-associated thromboembolic risk in cancer outpatients and effect of nadroparin thromboprophylaxis: Results of a retrospective analysis of the PROTECHT study. J. Transl. Med. 2011, 9, 179. [Google Scholar] [CrossRef] [PubMed]
- Bochenek, J.; Puskulluoglu, M.; Krzemieniecki, K. The antineoplastic effect of low-molecular-weight heparins-a literature review. Contemp. Oncol. 2013, 17, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Campello, E.; Ilich, A.; Simioni, P.; Key, N.S. The relationship between pancreatic cancer and hypercoagulability: A comprehensive review on epidemiological and biological issues. Br. J. Cancer 2019, 121, 359–371. [Google Scholar] [CrossRef] [PubMed]
- Young, A.; Chapman, O.; Connor, C.; Poole, C.; Rose, P.; Kakkar, A.K. Thrombosis and cancer. Nat. Rev. Clin. Oncol. 2012, 9, 437–449. [Google Scholar] [CrossRef] [PubMed]
- Grosskopf, I.; Shaish, A.; Ray, A.; Harats, D.; Kamari, Y. Low molecular weight heparin-induced increase in chylomicron-remnants clearance, is associated with decreased plasma TNF-alpha level and increased hepatic lipase activity. Thromb. Res. 2014, 133, 688–692. [Google Scholar] [CrossRef]
- Etulain, J.; Mena, H.A.; Negrotto, S.; Schattner, M. Stimulation of PAR-1 or PAR-4 promotes similar pattern of VEGF and endostatin release and pro-angiogenic responses mediated by human platelets. Platelets 2015, 26, 799–804. [Google Scholar] [CrossRef]
- Khorana, A.A.; Soff, G.A.; Kakkar, A.K.; Vadhan-Raj, S.; Riess, H.; Wun, T.; Streiff, M.B.; Garcia, D.A.; Liebman, H.A.; Belani, C.P.; et al. Rivaroxaban for Thromboprophylaxis in High-Risk Ambulatory Patients with Cancer. N. Engl. J. Med. 2019, 380, 720–728. [Google Scholar] [CrossRef]
- Al-Samkari, H.; Connors, J.M. The Role of Direct Oral Anticoagulants in Treatment of Cancer-Associated Thrombosis. Cancers 2018, 10, 271. [Google Scholar] [CrossRef]
- Kraaijpoel, N.; Carrier, M. How I treat cancer-associated venous thromboembolism. Blood 2019, 133, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Napolitano, M.; Mansueto, M.F.; Raso, S.; Siragusa, S. Quality of Life in Patients With Cancer Under Prolonged Anticoagulation for High-Risk Deep Vein Thrombosis: A Long-Term Follow-Up. Clin. Appl. Thromb./Hemost. Off. J. Int. Acad. Clin. Appl. Thromb./Hemost. 2020, 26, 1076029620918290. [Google Scholar] [CrossRef] [PubMed]
- Patsopoulos, N.A. A pragmatic view on pragmatic trials. Dialogues Clin. Neurosci. 2011, 13, 217–224. [Google Scholar] [PubMed]
- Kaatz, S.; Ahmad, D.; Spyropoulos, A.C.; Schulman, S. Subcommittee on Control of, A. Definition of clinically relevant non-major bleeding in studies of anticoagulants in atrial fibrillation and venous thromboembolic disease in non-surgical patients: Communication from the SSC of the ISTH. J. Thromb. Haemost. 2015, 13, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- Schulman, S.; Kearon, C. Subcommittee on Control of Anticoagulation of the, S.; Standardization Committee of the International Society on, T.; Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J. Thromb. Haemost. 2005, 3, 692–694. [Google Scholar] [CrossRef]

| Patients Characteristics | Value |
|---|---|
| Number of patients | 426 |
| Male (%) | 54.6% |
| Age (mean ± SD) | 65.3 ± 11.2 |
| Lung | 107 (25.1%) |
| Pancreas | 59 (13.9%) |
| Breast | 37 (8.7%) |
| Stomach | 36 (8.5%) |
| Ovarian | 33 (7.8%) |
| Colorectal | 31 (7.3%) |
| Bladder | 24 (5.6%) |
| Prostate | 14 (3.3%) |
| Testis | 6 (1.4%) |
| Other* | 79 (18.5%) |
| Patients Characteristics | Value |
|---|---|
| BMI (mean ± SD) | 26.1 ± 5.1 |
| BMI ≥35 kg/m2 | 6.3% |
| Anemia (Hg < 10 g/L) | 20.2% |
| PLT count ≥ 350 × 109/L | 37.1% |
| Leucocytes count > 11 × 109/L | 23.7% |
| Erythropoietin use | 16.7% |
| Metastatic disease | 69.5% |
| HTRCAs* | 67.1% |
| Khorana score ≤ 1 | 43.9% |
| Khorana score = 2 | 27.5% |
| Khorana score ≥ 3 | 28.6% |
| Cancer | Treatment | Patient | Biomarker | |||||
|---|---|---|---|---|---|---|---|---|
| Primary Site | Patients (N, %) | Metastatic (N, %) | HTRCAs (N, %) | Age (≥65, N, %) | Comorbidities (N, %) | PLT Count (≥350 × 109/L, N, %) | Anemia (Hg < 10 g/L, N, %) | Leucocytes (>11 × 109/L, N, %) |
| Lung | 107 (25.1%) | 80 (74.8%) | 70 (65.4%) | 59 (55.1%) | 27 (25.2%) | 48 (44.9%) | 26 (24.3%) | 35 (32.7%) |
| Pancreas | 59 (13.9%) | 43 (72.9%) | 55 (93.2%) | 35 (59.3%) | 16 (27.1%) | 21 (35.6%) | 11 (18.6%) | 13 (22.0%) |
| Breast | 37 (8.7%) | 25 (67.6%) | 13 (35.1%) | 18 (48.7%) | 5 (13.9%) | 4 (10.8%) | 4 (10.8%) | 1 (2.7%) |
| Stomach | 36 (8.5%) | 29 (80.6%) | 31 (86.1%) | 24 (66.7%) | 9 (25%) | 14 (38.9%) | 9 (25%) | 6 (16.7%) |
| Ovarian | 33 (7.8%) | 19 (57.6%) | 25 (75.8%) | 19 (57.6%) | 9 (27.3%) | 12 (36.4%) | 6 (18.2%) | 5 (15.2%) |
| Colorectal | 31 (7.3%) | 23 (74.2%) | 25 (80.7%) | 18 (58.1%) | 8 (25.8%) | 7 (22.6%) | 7 (22.6%) | 4 (12.9%) |
| Bladder | 24 (5.6%) | 17 (70.8%) | 19 (79.2%) | 17 (70.8%) | 8 (33.3%) | 12 (50%) | 5 (20.8%) | 8 (33.3%) |
| Prostate | 14 (3.3%) | 12 (85.7% | 1 (7.1%) | 10 (71.4%) | 3 (21.4%) | 4 (28.6%) | 4 (28.6%) | |
| Testis | 6 (1.4%) | 2 (33.3%) | 6 (100%) | 1 (16.7%) | 1 (16.7%) | 4 (66.7%) | 0 (0%) | 2 (33.3%) |
| Other | 79 (18.5%) | 47 (59.5%) | 41 (51.9%) | 38 (48.1%) | 29 (36.7%) | 32 (40.5%) | 14 (17.7%) | 27 (34.2%) |
| Risk Group | Factor |
|---|---|
| Cancer Related | Cancer type has a very high risk for CAT according to the Khorana score |
| Cancer type has a high risk for CAT according to the Khorana score | |
| Cancer type is not included in the Khorana score | |
| Metastatic disease | |
| Treatment Related | Use of HTRCAs during treatment |
| Cancer surgery was performed | |
| Hospitalization of patient | |
| Use of erythropoietin | |
| Use of hormonotherapy (tamoxifen) | |
| Patient Related | BMI ≥35 kg/m2 |
| Age >65 years | |
| Smoking | |
| Co-morbidities | |
| History of trauma or heart failure or thrombosis | |
| Biomarkers | Pre-chemotherapy platelets count ≥350 × 10⁹/L |
| Hemoglobin level <10 g/dL or use of erythropoietin | |
| Pre-chemotherapy leukocytes count >11 × 10⁹/L |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsoukalas, N.; Papakotoulas, P.; Christopoulou, A.; Ardavanis, A.; Koumakis, G.; Papandreou, C.; Papatsimpas, G.; Papakostas, P.; Samelis, G.; Andreadis, C.; et al. Real-World Data on Thromboprophylaxis in Active Cancer Patients: Where Are We? Are We Getting There? Cancers 2020, 12, 1907. https://doi.org/10.3390/cancers12071907
Tsoukalas N, Papakotoulas P, Christopoulou A, Ardavanis A, Koumakis G, Papandreou C, Papatsimpas G, Papakostas P, Samelis G, Andreadis C, et al. Real-World Data on Thromboprophylaxis in Active Cancer Patients: Where Are We? Are We Getting There? Cancers. 2020; 12(7):1907. https://doi.org/10.3390/cancers12071907
Chicago/Turabian StyleTsoukalas, Nikolaos, Pavlos Papakotoulas, Athina Christopoulou, Alexandros Ardavanis, Georgios Koumakis, Christos Papandreou, Georgios Papatsimpas, Pavlos Papakostas, Georgios Samelis, Charalambos Andreadis, and et al. 2020. "Real-World Data on Thromboprophylaxis in Active Cancer Patients: Where Are We? Are We Getting There?" Cancers 12, no. 7: 1907. https://doi.org/10.3390/cancers12071907
APA StyleTsoukalas, N., Papakotoulas, P., Christopoulou, A., Ardavanis, A., Koumakis, G., Papandreou, C., Papatsimpas, G., Papakostas, P., Samelis, G., Andreadis, C., Aravantinos, G., Ziras, N., Kalofonos, C., Samantas, E., Souggleri, M., Makrantonakis, P., Pentheroudakis, G., Athanasiadis, A., Stergiou, H., ... Boukovinas, I. (2020). Real-World Data on Thromboprophylaxis in Active Cancer Patients: Where Are We? Are We Getting There? Cancers, 12(7), 1907. https://doi.org/10.3390/cancers12071907






