Association of Allostatic Load with All-Cause and Cancer Mortality by Race and Body Mass Index in the REGARDS Cohort
Abstract
1. Introduction
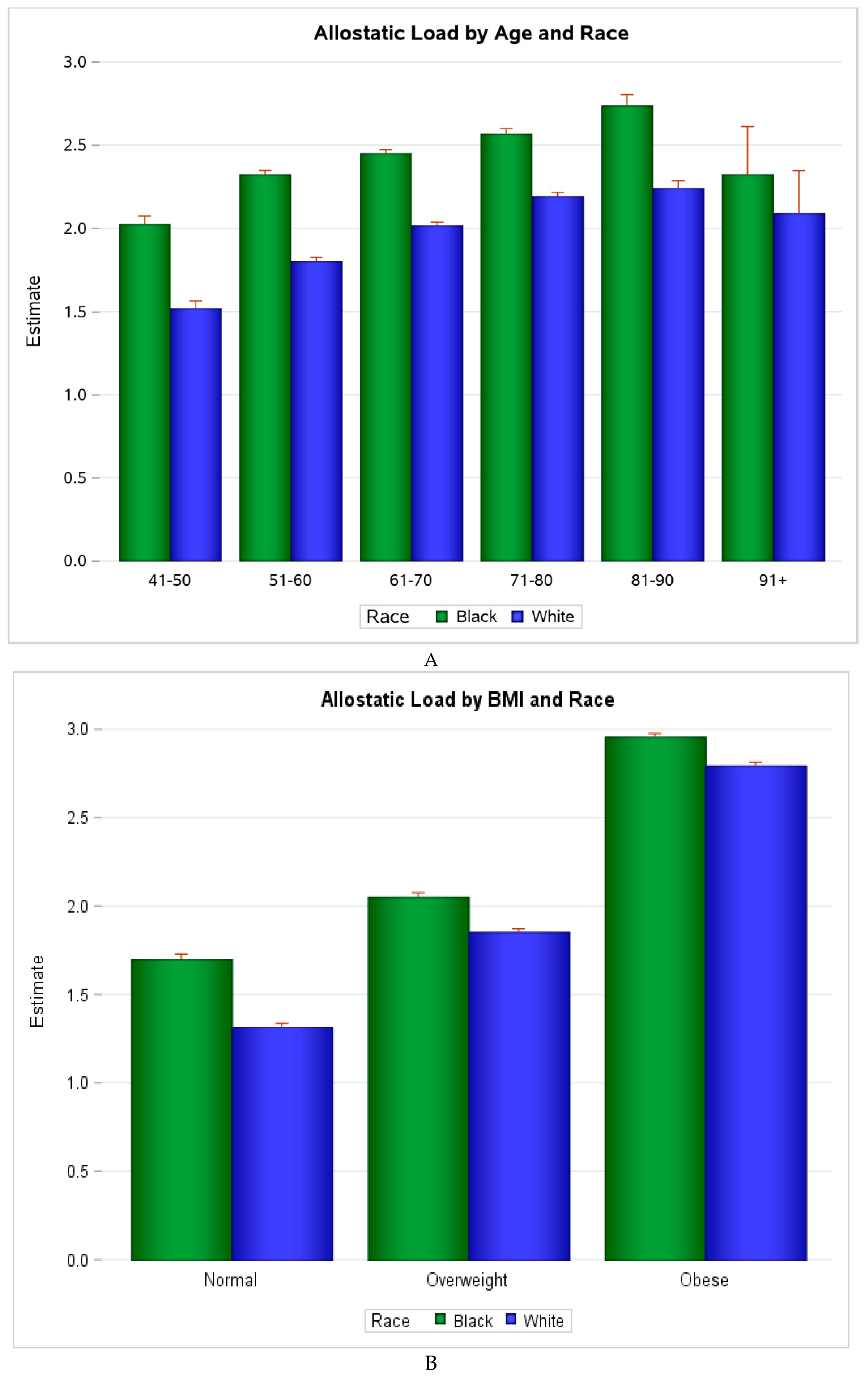
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Subjects
4.2. Exposure
4.3. Outcome
4.4. Covariates
4.5. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- McEwen, B.S.; Gianaros, P.J. Central role of the brain in stress and adaptation: Links to socioeconomic status, health, and disease. Ann. N. Y. Acad. Sci. 2010, 1186, 190–222. [Google Scholar] [CrossRef]
- McEwen, B.; Lasley, E.N. Allostatic load: When protection gives way to damage. Adv. Mind-Body Med. 2003, 19, 28–33. [Google Scholar]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef]
- Seeman, T.E.; Singer, B.H.; Rowe, J.W.; Horwitz, R.I.; McEwen, B.S. Price of adaptation—Allostatic load and its health consequences. MacArthur studies of successful aging. Arch. Intern. Med. 1997, 157, 2259–2268. [Google Scholar] [CrossRef] [PubMed]
- Seeman, T.E.; McEwen, B.S.; Rowe, J.W.; Singer, B.H. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc. Natl. Acad. Sci. USA 2001, 98, 4770–4775. [Google Scholar] [CrossRef] [PubMed]
- Ko, Y.J.; Kwon, Y.M.; Kim, K.H.; Choi, H.C.; Chun, S.H.; Yoon, H.J.; Goh, E.; Cho, B.; Park, M. High-sensitivity C-reactive protein levels and cancer mortality. Cancer Epidemiol. Biomark. Prev. 2012, 21, 2076–2086. [Google Scholar] [CrossRef]
- Rhee, E.J.; Chang, Y.; Sohn, C.I.; Shin, H.C.; Ryu, S.; Lee, W.Y. Impact of systemic inflammation on the relationship between insulin resistance and all-cause and cancer-related mortality. Metabolism 2018, 81, 52–62. [Google Scholar]
- Akinyemiju, T.; Moore, J.X.; Pisu, M.; Judd, S.E.; Goodman, M.; Shikany, J.M.; Howard, V.J.; Safford, M.; Gilchrist, S.C. A prospective study of obesity, metabolic health, and cancer mortality. Obesity (Silver Spring) 2018, 26, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Feliciano, E.M.C.; Kroenke, C.H.; Meyerhardt, J.A.; Prado, C.M.; Bradshaw, P.T.; Dannenberg, A.J.; Kwan, M.L.; Xiao, J.; Quesenberry, C.; Weltzien, E.K.; et al. Dysfunction, obesity, and survival among patients with early-stage colorectal cancer. J. Clin. Oncol. 2016, 34, 3664–3671. [Google Scholar] [CrossRef] [PubMed]
- Borrell, L.N.; Dallo, F.J.; Nguyen, N. Racial/ethnic disparities in all-cause mortality in U.S. adults: The effect of allostatic load. Public Health Rep. 2010, 125, 810–816. [Google Scholar] [CrossRef]
- Castagné, R.; Garès, V.; Karimi, M.; Chadeau-Hyam, M.; Vineis, P.; Delpierre, C.; Kelly-Irving, M.; Consortium, L. Allostatic load and subsequent all-cause mortality: Which biological markers drive the relationship? Findings from a UK birth cohort. Eur. J. Epidemiol. 2018, 33, 441–458. [Google Scholar] [CrossRef] [PubMed]
- Duru, O.K.; Harawa, N.T.; Kermah, D.; Norris, K.C. Allostatic load burden and racial disparities in mortality. J. Natl. Med. Assoc. 2012, 104, 89–95. [Google Scholar] [CrossRef]
- Karlamangla, A.S.; Singer, B.H.; Seeman, T.E. Reduction in allostatic load in older adults is associated with lower all-cause mortality risk: Macarthur studies of successful aging. Psychosom. Med. 2006, 68, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Levine, M.E.; Crimmins, E.M. A comparison of methods for assessing mortality risk. Am. J. Hum. Biol. Off. J. Hum. Biol. Counc. 2014, 26, 768–776. [Google Scholar] [CrossRef]
- Robertson, T.; Beveridge, G.; Bromley, C. Allostatic load as a predictor of all-cause and cause-specific mortality in the general population: Evidence from the Scottish Health Survey. PLoS ONE 2017, 12, e0183297. [Google Scholar] [CrossRef] [PubMed]
- Organization WH. Obesity and Overweight. Available online: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 22 September 2019).
- Ogden, C.L.; Carroll, M.D. Prevalence of Overweight, Obesity, and Extreme Obesity Among Adults: United States, Trends 1960–1962 through 2007–2008; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2010. [Google Scholar]
- Geronimus, A.T.; Hicken, M.; Keene, D.; Bound, J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am. J. Public Health 2006, 96, 826–833. [Google Scholar] [CrossRef]
- Oken, B.S.; Chamine, I.; Wakeland, W. A systems approach to stress, stressors and resilience in humans. Behav. Brain Res. 2015, 282, 144–154. [Google Scholar] [CrossRef]
- Dowd, J.B.; Simanek, A.M.; Aiello, A.E. Socio-economic status, cortisol and allostatic load: A review of the literature. Int. J. Epidemiol. 2009, 38, 1297–1309. [Google Scholar] [CrossRef]
- Graves, K.Y.; Nowakowski, A.C.H. Childhood socioeconomic status and stress in late adulthood: A longitudinal approach to measuring Allostatic load. Glob. Pediatric Health 2017, 4. [Google Scholar] [CrossRef]
- Schulz, A.J.; Mentz, G.; Lachance, L.; Johnson, J.; Gaines, C.; Israel, B.A. Associations between socioeconomic status and Allostatic load: Effects of neighborhood poverty and tests of mediating pathways. Am. J. Public Health 2012, 102, 1706–1714. [Google Scholar] [CrossRef]
- Steptoe, A.; Wardle, J. Cardiovascular stress responsivity, body mass and abdominal adiposity. Int. J. Obes. (Lond.) 2005, 29, 1329–1337. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, J.R.; Bovasso, G.B. Early and chronic stress and their relation to breast cancer. Psychol. Med. 2000, 30, 669–678. [Google Scholar] [CrossRef] [PubMed]
- Mariotti, A. The effects of chronic stress on health: New insights into the molecular mechanisms of brain–body communication. Future Sci. OA 2015, 1. [Google Scholar] [CrossRef] [PubMed]
- Gu, H.F.; Tang, C.K.; Yang, Y.Z. Psychological stress, immune response, and atherosclerosis. Atherosclerosis 2012, 223, 69–77. [Google Scholar] [CrossRef]
- Reiche, E.M.; Nunes, S.O.; Morimoto, H.K. Stress, depression, the immune system, and cancer. Lancet Oncol. 2004, 5, 617–625. [Google Scholar] [CrossRef]
- Flint, M.S.; Baum, A.; Episcopo, B.; Knickelbein, K.Z.; Liegey Dougall, A.J.; Chambers, W.H.; Jenkins, F.J. Chronic exposure to stress hormones promotes transformation and tumorigenicity of 3T3 mouse fibroblasts. Stress 2013, 16, 114–121. [Google Scholar] [CrossRef]
- Freeman, V.L.; Ricardo, A.C.; Campbell, R.T.; Barrett, R.E.; Warnecke, R.B. Association of census tract-level socioeconomic status with disparities in prostate cancer–specific survival. Cancer Epidemiol. Biomark. Prev. 2011, 20, 2150–2159. [Google Scholar] [CrossRef]
- Kelly-Irving, M.; Lepage, B.; Dedieu, D.; Lacey, R.; Cable, N.; Bartley, M.; Blane, D.; Grosclaude, P.; Lang, T.; Delpierre, C. Childhood adversity as a risk for cancer: Findings from the 1958 British birth cohort study. BMC Public Health 2013, 13, 767. [Google Scholar] [CrossRef]
- Cohen, L.; Cole, S.W.; Sood, A.K.; Prinsloo, S.; Kirschbaum, C.; Arevalo, J.M.; Jennings, N.B.; Scott, S.; Vence, L.; Wei, Q.; et al. Depressive Symptoms and Cortisol Rhythmicity Predict Survival in Patients with Renal Cell Carcinoma: Role of Inflammatory Signaling. PLoS ONE 2012, 7, e42324. [Google Scholar] [CrossRef]
- Nielsen, N.R.; Kristensen, T.S.; Schnohr, P.; Grønbæk, M. Perceived stress and cause-specific mortality among men and women: Results from a prospective cohort study. Am. J. Epidemiol. 2008, 168, 481–491. [Google Scholar] [CrossRef]
- Steptoe, A.; Hiltl, T.J.; Dowd, J.B.; Hamer, M. Socioeconomic status and central adiposity as determinants of stress-related biological responses relevant to cardiovascular disease risk. Brain Behav. Immun. 2018. [Google Scholar] [CrossRef] [PubMed]
- Wardle, J.; Chida, Y.; Gibson, E.L.; Whitaker, K.L.; Steptoe, A. Stress and adiposity: A meta-analysis of longitudinal studies. Obesity (Silver Spring) 2011, 19, 771–778. [Google Scholar] [CrossRef] [PubMed]
- Kartheuser, A.H.; Leonard, D.F.; Penninckx, F.; Paterson, H.M.; Brandt, D.; Remue, C.; Bugli, C.; Dozois, E.; Mortensen, N.; Ris, F.; et al. Waist circumference and waist/hip ratio are better predictive risk factors for mortality and morbidity after colorectal surgery than body mass index and body surface area. Ann. Surg. 2013, 258, 722–730. [Google Scholar] [CrossRef] [PubMed]
- Streng, K.W.; Voors, A.A.; Hillege, H.L.; Anker, S.D.; Cleland, J.G.; Dickstein, K.; Filippatos, G.; Metra, M.; Ng, L.L.; Ponikowski, P.; et al. Waist-to-hip ratio and mortality in heart failure. Eur. J. Heart Fail. 2018, 20, 1269–1277. [Google Scholar] [CrossRef] [PubMed]
- Czernichow, S.; Kengne, A.P.; Stamatakis, E.; Hamer, M.; Batty, G.D. Body mass index, waist circumference and waist-hip ratio: Which is the better discriminator of cardiovascular disease mortality risk?: Evidence from an individual-participant meta-analysis of 82,864 participants from nine cohort studies. Obes. Rev. 2011, 12, 680–687. [Google Scholar] [CrossRef] [PubMed]
- Howard, V.J.; Cushman, M.; Pulley, L.; Gomez, C.R.; Go, R.C.; Prineas, R.J.; Graham, A.; Moy, C.S.; Howard, G. The reasons for geographic and racial differences in stroke study: Objectives and design. Neuroepidemiology 2005, 25, 135–143. [Google Scholar] [CrossRef]
- Halanych, J.H.; Shuaib, F.; Parmar, G.; Tanikella, R.; Howard, V.J.; Roth, D.L.; Prineas, R.J.; Safford, M.M. Agreement on cause of death between proxies, death certificates, and clinician adjudicators in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. Am. J. Epidemiol. 2011, 173, 1319–1326. [Google Scholar] [CrossRef]
- Graham, J.W.; Olchowski, A.E.; Gilreath, T.D. How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prev. Sci. 2007, 8, 206–213. [Google Scholar] [CrossRef]
| Characteristics § | Black ‡ | White ‡ | p | |
|---|---|---|---|---|
| Age, years, mean (SD) | 64.1 (9.2) | 65.4 (9.5) | <0.001 | |
| Comorbidity score, mean (SD) | 2.02(1.36) | 1.79(1.4) | <0.001 | |
| Allostatic load, mean (SD) * | 2.42 (1.50) | 1.99 (1.39) | <0.001 | |
| High allostatic load, % (SE) † | 44.6 (0.4) | 33.4 (0.3) | <0.001 | |
| Allostatic load, mean (SD) by patient characteristics | ||||
| Sex | Female | 2.49 (1.46) | 1.88 (1.35) | <0.001 |
| Male | 2.29 (1.56) | 2.09 (1.42) | ||
| Region | Stroke Belt | 2.44 (1.49) | 2.01 (1.40) | 0.028 |
| Stroke Buckle | 2.34 (1.48) | 1.99 (1.37) | ||
| Non-Belt | 2.43 (1.51) | 1.97 (1.38) | ||
| Annual Income | ≥USD 75,000 | 1.98 (1.42) | 1.63 (1.30) | <0.001 |
| USD 35,000 to USD 74,000 | 2.18 (1.45) | 1.95 (1.36) | ||
| USD 20,000 to USD 34,000 | 2.47 (1.49) | 2.21 (1.41) | ||
| <USD 20,000 | 2.68 (1.51) | 2.38 (1.43) | ||
| Refused | 2.52 (1.52) | 1.89 (1.37) | ||
| Education | College + | 2.18 (1.48) | 1.78 (1.34) | 0.035 |
| Some college | 2.35 (1.45) | 2.05 (1.39) | ||
| High school | 2.47 (1.51) | 2.12 (1.39) | ||
| <High School | 2.74 (1.51) | 2.47 (1.44) | ||
| Alcohol | None | 2.50 (1.51) | 2.14 (1.41) | 0.724 |
| Moderate | 2.20 (1.47) | 1.81 (1.34) | ||
| Heavy | 2.08 (1.33) | 1.66 (1.32) | ||
| Physical activity | None | 2.68 (1.54) | 2.28 (1.43) | 0.19 |
| 1–3 times/week | 2.34 (1.46) | 1.91 (1.36) | ||
| ≥4 times /week | 2.15 (1.44) | 1.78 (1.33) | ||
| Smoking | Never | 2.39 (1.50) | 1.87 (1.35) | 0.087 |
| Past | 2.46 (1.50) | 2.08 (1.40) | ||
| Current | 2.41 (1.49) | 2.12 (1.43) | ||
| Diabetes | Yes | 2.94 (1.51) | 2.79 (1.41) | <0.001 |
| No | 2.20 (1.44) | 1.84 (1.33) | ||
| BMI | Normal | 1.60 (1.35) | 1.28 (1.13) | 0.379 |
| Overweight/obese | 2.60 (1.47) | 2.28 (1.38) | ||
| Biomarkers comprising AL score calculation | ||||
| BUN, mg/dL, median (IQR) | 15.0 (12.0–19.0) | 16.9 (13.6–20.0) | <0.001 | |
| Albumin, g/dL, mean (SD) | 4.11(0.33) | 4.21(0.32) | <0.001 | |
| CRP, mg/L, median (IQR) | 3.1 (1.2–7.2) | 1.9 (0.8–4.6) | <0.001 | |
| Creatinine, mg/dL, median (IQR) | 0.9 (0.7–1.1) | 0.8 (0.7–0.9) | <0.001 | |
| DBP, mmHg, mean (SD) | 78.44(10.08) | 75.16(9.19) | <0.001 | |
| SBP, mmHg, mean (SD) | 130.77(17.35) | 125.37(15.8) | <0.001 | |
| HDL, mg/dL, median (IQR) | 51.0 (42.0–62.0) | 48.0 (39.0–60.0) | <0.001 | |
| Characteristics‡ | High AL (≥3) * (N = 11,280) | Low AL (<3) (N = 18,421) | p | |
|---|---|---|---|---|
| Age, years, mean (SD) | 66.0 (9.3) | 64.2 (9.4) | <0.001 | |
| Sex (% female) | 6274 (55.6) | 10,088(54.7) | 0.149 | |
| Race (% Black) | 5454 (48.3) | 6770 (36.7) | <0.001 | |
| Region | Stroke Belt | 3980 (35.2) | 6308 (34.2) | 0.009 |
| Stroke Buckle | 2261 (20.0) | 3956 (21.4) | ||
| Non-Belt | 5039 (44.6) | 8157 (44.2) | ||
| Annual Income | ≥USD 75,000 | 1161 (10.3) | 3537 (19.23) | <0.001 |
| USD 35,000 to USD 74,000 | 3040 (26.9) | 5772 (31.3) | ||
| USD 20,000 to USD 34,000 | 3054 (27.1) | 4123 (22.4) | ||
| <USD 20,000 | 2631 (23.3) | 2715 (14.7) | ||
| Refused | 1394 (12.4) | 2274 (12.3) | ||
| Education | College + | 3180 (28.2) | 7165 (38.9) | <0.001 |
| Some college | 3012 (26.7) | 4965 (26.9) | ||
| High school | 3175 (28.1) | 4494 (24.4) | ||
| <High School | 1913 (16.9) | 1797 (9.7) | ||
| Alcohol | None | 7927 (70.3) | 10,902 (59.2) | <0.001 |
| Moderate | 3022 (26.8) | 6673 (36.2) | ||
| Heavy | 331 (2.9) | 846 (4.6) | ||
| Physical activity | None | 4685 (41.5) | 5385 (29.2) | <0.001 |
| 1–3 times/week | 3900 (34.6) | 7079 (38.4) | ||
| ≥4 times/week | 2695 (23.9) | 5957 (32.3) | ||
| Smoking | Never | 4811 (42.6) | 8690 (47.2) | <0.001 |
| Past | 4689 (41.6) | 7226 (39.2) | ||
| Current | 1780 (15.8) | 2505 (13.6) | ||
| Diabetes (% yes) | 3630 (32.2) | 2664 (14.5) | <0.001 | |
| BMI | Normal | 1363 (12.1) | 6150 (33.4) | <0.001 |
| Overweight/obese | 9917 (87.9) | 12,271 (66.6) | ||
| BUN, mg/dL, median (IQR) | 19.0 (14.6–23.0) | 15.0 (12.0–18.0) | <0.001 | |
| Comorbid score, mean (SD) | 2.5 (1.4) | 1.5 (1.3) | <0.001 | |
| Albumin, g/dL, mean (SD) | 4.1 (0.4) | 4.2 (0.3) | <0.001 | |
| CRP, mg/L, median (IQR) | 4.8 (2.5–9.0) | 1.6 (0.8–3.2) | <0.001 | |
| Creatinine, mg/dL, median (IQR) | 0.9 (0.8–1.2) | 0.8 (0.7–1.0) | <0.001 | |
| DBP, mmHg, mean (SD) | 79.5 (11.0) | 74.7 (8.4) | <0.001 | |
| SBP, mmHg, mean (SD) | 135.1 (18.3) | 123.0 (13.7) | <0.001 | |
| HDL, mg/dL, median (IQR) | 44.0 (36.0–56.0) | 52.0 (43.9–64.0) | <0.001 | |
| Models | Overall (N = 29,701) †‡ | Black (N = 12,224) †‡ | White (N = 17,476) †‡ | |||
|---|---|---|---|---|---|---|
| Allostatic Load | All-Cause Mortality ‡ | Cancer mortality ‡ | All-Cause mortality ‡ | Cancer Mortality ‡ | All-Cause mortality ‡ | Cancer mortality ‡ |
| Deaths | 4622 | 1237 | 2055 | 513 | 2607 | 724 |
| Crude * | 1.35 (1.33, 1.38) | 1.15 (1.11, 1.19) | 1.32 (1.28, 1.36) | 1.09 (1.03, 1.16) | 1.37 (1.34, 1.41) | 1.20 (1.14, 1.26) |
| Model 1 * | 1.32 (1.29, 1.34) | 1.11 (1.07, 1.16) | 1.29 (1.25, 1.33) | 1.06 (1.00, 1.13) | 1.31 (1.28, 1.35) | 1.14 (1.09, 1.21) |
| Model 2 * | 1.30 (1.28, 1.33) | 1.11 (1.06, 1.15) | - | - | - | - |
| Model 3 * | 1.27 (1.24, 1.30) | 1.08 (1.04, 1.13) | 1.33 (1.29, 1.37) | 1.11 (1.04, 1.18) | 1.31 (1.28, 1.35) | 1.15 (1.09, 1.22) |
| Model 4 * | 1.24 (1.22,1.27) | 1.07 (1.03,1.12) | 1.26 (1.22,1.30) | 1.06 (0.99,1.13) | 1.23 (1.20,1.27) | 1.08 (1.03,1.14) |
| Race Ω | ||||||
| Black | 1.05 (0.99, 1.12) | 1.03 (0.92,1.17) | - | - | - | |
| White (Ref) | - | - | - | |||
| Allostatic Load | Normal BMI (n = 7299) † | Overweight/Obese (N = 22,401) † | ||
|---|---|---|---|---|
| All-Cause mortality ‡ | Cancer mortality ‡ | All-Cause mortality ‡ | Cancer mortality ‡ | |
| Deaths | 1414 | 407 | 3248 | 830 |
| Crude * | 1.56 (1.50, 1.63) | 1.40 (1.30, 1.50) | 1.41 (1.38, 1.44) | 1.17 (1.11, 1.23) |
| Model 1 * | 1.41 (1.35, 1.47) | 1.29 (1.19, 1.39) | 1.36 (1.33, 1.40) | 1.13 (1.07, 1.18) |
| Model 2 * | 1.38 (1.32, 1.44) | 1.27 (1.17, 1.37) | 1.35 (1.32, 1.39) | 1.12 (1.07, 1.18) |
| Model 3 * | 1.34 (1.28, 1.40) | 1.22 (1.13, 1.33) | 1.32 (1.29, 1.35) | 1.10 (1.05, 1.16) |
| Model 4 * | 1.29 (1.23, 1.35) | 1.17 (1.08, 1.28) | 1.29 (1.26, 1.32) | 1.09 (1.03, 1.14) |
| Race Ω | ||||
| Black | 1.18 (1.05, 1.33) | 1.11 (0.89, 1.38) | 1.09 (1.01, 1.17) | 1.06 (0.91, 1.23) |
| White (Ref) | - | - | - | - |
| Allostatic Load | Age < 65 years (N = 15,008) † | Age ≥65 years (N = 14,692) † | ||
|---|---|---|---|---|
| All-Cause mortality ‡ | Cancer mortality ‡ | All-Cause mortality ‡ | Cancer mortality ‡ | |
| Deaths | 1106 | 320 | 3556 | 917 |
| Crude | 1.47 (1.42, 1.53) | 1.17 (1.09, 1.26) | 1.28 (1.25, 1.31) | 1.11 (1.06, 1.16) |
| Model 1 * | 1.46 (1.40, 1.51) | 1.15 (1.07, 1.24) | 1.27 (1.24, 1.30) | 1.10 (1.05, 1.15) |
| Model 2 * | 1.43 (1.37, 1.49) | 1.13 (1.04, 1.22) | 1.26 (1.23, 1.29) | 1.10 (1.05, 1.15) |
| Model 3 * | 1.36 (1.31,1.42) | 1.07(0.99, 1.16) | 1.24 (1.21, 1.27) | 1.08 (1.03, 1.13) |
| Model 4 * | 1.34 (1.28, 1.39) | 1.06 (0.98, 1.15) | 1.22 (1.19, 1.25) | 1.07 (1.02, 1.12) |
| Allostatic Load Components | Continuous * | High vs. Low *† | Continuous * | High vs. Low *† |
|---|---|---|---|---|
| All-Cause mortality ‡ | Cancer mortality ‡ | |||
| Overall | ||||
| Deaths | 4622 | 4622 | 1237 | 1237 |
| CRP | 1.01 (1.01, 1.02) | 1.50 (1.41, 1.59) | 1.01 (1.01, 1.02) | 1.30 (1.16, 1.46) |
| Albumin | 0.60 (0.53, 0.67) | 1.44 (1.31, 1.59) | 0.80 (0.64, 1.00) | 1.12 (0.90, 1.39) |
| BUN | 1.03 (1.02, 1.04) | 1.46 (1.35, 1.57) | 1.01 (1.00, 1.02) | 1.12 (0.97, 1.28) |
| Total Cholesterol | 1.00 (1.00,1.00) | 1.00 (0.90, 1.11) | 1.00 (1.00, 1.00) | 0.95 (0.78, 1.16) |
| Creatinine | 1.37 (1.30, 1.43) | 2.10 (1.93, 2.28) | 1.14 (1.03, 1.25) | 1.19 (0.98, 1.45) |
| HDL | 1.00 (0.99, 1.00) | 1.13 (1.05, 1.21) | 1.00 (0.99, 1.00) | 1.07 (0.93, 1.23) |
| DBP | 1.00 (1.00, 1.00) | 1.15 (1.03, 1.28) | 0.99 (0.99, 1.00) | 0.82 (0.65, 1.03) |
| SBP | 1.01 (1.00,1.01) | 1.29 (1.21, 1.38) | 1.00 (1.00, 1.00) | 1.02 (0.90, 1.17) |
| WC | 1.01 (1.01, 1.01) | 1.06(0.99,1.14) | 1.00 (1.00, 1.00) | 0.91 (0.80, 1.04) |
| Blacks | ||||
| Deaths | 2055 | 2055 | 513 | 513 |
| CRP | 1.01 (1.01, 1.02) | 1.37 (1.24, 1.50) | 1.01 (1.01, 1.02) | 1.08 (0.90, 1.29) |
| Albumin | 0.52 (0.44, 0.61) | 1.57 (1.38, 1.78) | 0.74 (0.52, 1.05) | 1.12 (0.83, 1.50) |
| BUN | 1.03 (1.02, 1.04) | 1.57 (1.42, 1.75) | 1.01 (1.00, 1.02) | 1.13 (0.92, 1.39) |
| Total Cholesterol | 1.00 (1.00, 1.00) | 1.06 (0.92, 1.23) | 1.00 (1.00, 1.00) | 0.98 (0.73, 1.31) |
| Creatinine | 1.34 (1.27, 1.41) | 2.25 (2.00, 2.52) | 1.15 (1.04, 1.27) | 1.24 (0.95, 1.62) |
| HDL | 1.00 (0.99, 1.00) | 1.15 (1.03, 1.29) | 1.00 (0.99, 1.00) | 1.12 (0.89, 1.40) |
| DBP | 1.00 (1.00, 1.01) | 1.20 (1.05, 1.37) | 0.99 (0.98, 1.00) | 0.88 (0.65, 1.17) |
| SBP | 1.01 (1.01, 1.01) | 1.34 (1.22, 1.47) | 1.00 (1.00, 1.01) | 1.08 (0.89, 1.31) |
| WC | 1.01 (1.01, 1.01) | 0.98 (0.88, 1.08) | 1.00 (0.99, 1.00) | 0.89(0.73, 1.09) |
| Whites | ||||
| Deaths | 2607 | 2607 | 704 | 704 |
| CRP | 1.02 (1.02, 1.03) | 1.61 (1.48, 1.74) | 1.02 (1.01, 1.02) | 1.48 (1.27, 1.72) |
| Albumin | 0.68 (0.58, 0.80) | 1.32 (1.15, 1.53) | 0.84 (0.63, 1.13) | 1.15 (0.86, 1.54) |
| BUN | 1.03 (1.03, 1.04) | 1.37 (1.23, 1.52) | 1.00 (0.99,1.02) | 1.11 (0.93, 1.33) |
| Total Cholesterol | 1.00 (1.00, 1.00) | 0.95 (0.82, 1.09) | 1.00 (1.00, 1.00) | 0.93 (0.71, 1.21) |
| Creatinine | 1.45 (1.34, 1.58) | 1.93 (1.70, 2.19) | 1.08 (0.86, 1.36) | 1.11 (0.83, 1.48) |
| HDL | 1.00 (0.99, 1.00) | 1.11 (1.01, 1.21) | 1.00 (0.99, 1.00) | 1.04 (0.88, 1.24) |
| DBP | 1.00 (0.99, 1.00) | 1.06 (0.88, 1.27) | 0.99 (0.98, 1.00) | 0.74 (0.51, 1.08) |
| SBP | 1.00 (1.00, 1.01) | 1.25 (1.14, 1.37) | 1.00 (0.99, 1.00) | 0.98 (0.81, 1.17) |
| WC | 1.01 (1.01, 1.01) | 1.14 (1.04, 1.26) | 1.00 (1.00, 1.01) | 0.94 (0.79, 1.13) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akinyemiju, T.; Wilson, L.E.; Deveaux, A.; Aslibekyan, S.; Cushman, M.; Gilchrist, S.; Safford, M.; Judd, S.; Howard, V. Association of Allostatic Load with All-Cause and Cancer Mortality by Race and Body Mass Index in the REGARDS Cohort. Cancers 2020, 12, 1695. https://doi.org/10.3390/cancers12061695
Akinyemiju T, Wilson LE, Deveaux A, Aslibekyan S, Cushman M, Gilchrist S, Safford M, Judd S, Howard V. Association of Allostatic Load with All-Cause and Cancer Mortality by Race and Body Mass Index in the REGARDS Cohort. Cancers. 2020; 12(6):1695. https://doi.org/10.3390/cancers12061695
Chicago/Turabian StyleAkinyemiju, Tomi, Lauren E Wilson, April Deveaux, Stella Aslibekyan, Mary Cushman, Susan Gilchrist, Monika Safford, Suzanne Judd, and Virginia Howard. 2020. "Association of Allostatic Load with All-Cause and Cancer Mortality by Race and Body Mass Index in the REGARDS Cohort" Cancers 12, no. 6: 1695. https://doi.org/10.3390/cancers12061695
APA StyleAkinyemiju, T., Wilson, L. E., Deveaux, A., Aslibekyan, S., Cushman, M., Gilchrist, S., Safford, M., Judd, S., & Howard, V. (2020). Association of Allostatic Load with All-Cause and Cancer Mortality by Race and Body Mass Index in the REGARDS Cohort. Cancers, 12(6), 1695. https://doi.org/10.3390/cancers12061695





