Metabolic Parameters Influence Brain Infarction and Outcome after Resection of Brain Metastases
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Anesthesia and Hemodynamic Parameters
2.3. Statistical Data Analysis
2.4. Magnetic Resonance Imaging and Image Analysis
3. Results
3.1. Patient Population
3.2. Postoperative Ischemia
3.3. Correlation between Hemodynamic Parameters and Infarct Volumes
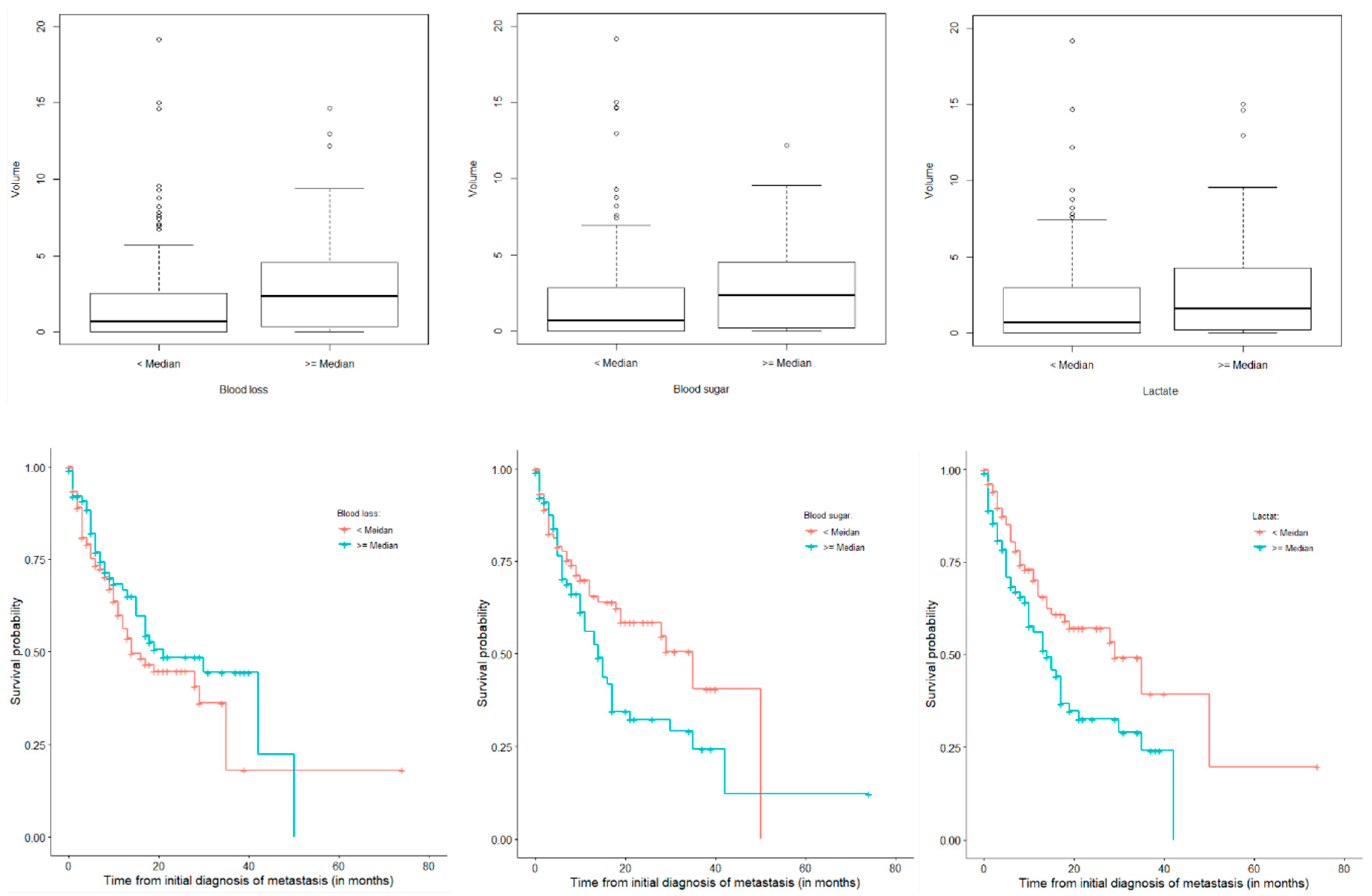
3.4. Overall Survival
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gempt, J.; Förschler, A.; Buchmann, N.; Pape, H.; Ryang, Y.-M.; Krieg, S.M.; Zimmer, C.; Meyer, B.; Ringel, F. Postoperative ischemic changes following resection of newly diagnosed and recurrent gliomas and their clinical relevance. J. Neurosurg. 2013, 118, 801–808. [Google Scholar] [CrossRef] [PubMed]
- Gempt, J.; Gerhardt, J.; Toth, V.; Hüttinger, S.; Ryang, Y.-M.; Wostrack, M.; Krieg, S.M.; Meyer, B.; Förschler, A.; Ringel, F. Postoperative ischemic changes following brain metastasis resection as measured by diffusion-weighted magnetic resonance imaging. J. Neurosurg. 2013, 119, 1395–1400. [Google Scholar] [CrossRef] [PubMed]
- Gempt, J.; Krieg, S.M.; Hüttinger, S.; Buchmann, N.; Ryang, Y.-M.; Shiban, E.; Meyer, B.; Zimmer, C.; Förschler, A.; Ringel, F. Postoperative ischemic changes after glioma resection identified by diffusion-weighted magnetic resonance imaging and their association with intraoperative motor evoked potentials. J. Neurosurg. 2013, 119, 829–836. [Google Scholar] [CrossRef] [PubMed]
- Jakola, A.S.; Berntsen, E.M.; Christensen, P.; Gulati, S.; Unsgård, G.; Kvistad, K.A.; Solheim, O. Surgically acquired deficits and diffusion weighted MRI changes after glioma resection—A matched case-control study with blinded neuroradiological assessment. PLoS ONE 2014, 9, e101805. [Google Scholar] [CrossRef]
- Bette, S.; Wiestler, B.; Kaesmacher, J.; Huber, T.; Gerhardt, J.; Barz, M.; Delbridge, C.; Ryang, Y.-M.; Ringel, F.; Zimmer, C.; et al. Infarct volume after glioblastoma surgery as an independent prognostic factor. Oncotarget 2016, 7, 61945–61954. [Google Scholar] [CrossRef]
- McGirt, M.J.; Mukherjee, D.; Chaichana, K.L.; Than, K.D.; Weingart, J.D.; Quinones-Hinojosa, A. Association of surgically acquired motor and language deficits on overall survival after resection of glioblastoma multiforme. Neurosurgery 2009, 65, 463–469. [Google Scholar] [CrossRef]
- Thiepold, A.L.; Luger, S.; Wagner, M.; Filmann, N.; Ronellenfitsch, M.W.; Harter, P.N.; Braczynski, A.K.; Dützmann, S.; Hattingen, E.; Steinbach, J.P.; et al. Perioperative cerebral ischemia promote infiltrative recurrence in glioblastoma. Oncotarget 2015, 6, 14537–14544. [Google Scholar] [CrossRef]
- Wigerup, C.; Pahlman, S.; Bexell, D. Therapeutic targeting of hypoxia and hypoxia-inducible factors in cancer. Pharmacol. Ther. 2016, 164, 152–169. [Google Scholar] [CrossRef]
- Colwell, N.; Larion, M.; Giles, A.J.; Seldomridge, A.N.; Sizdahkhani, S.; Gilbert, M.R.; Park, D.M. Hypoxia in the glioblastoma microenvironment: Shaping the phenotype of cancer stem-like cells. Neuro-Oncology 2017, 19, 887–896. [Google Scholar] [CrossRef]
- Bette, S.; Wiestler, B.; Wiedenmann, F.; Kaesmacher, J.; Bretschneider, M.; Barz, M.; Huber, T.; Ryang, Y.-M.; Kochs, E.; Zimmer, C.; et al. Safe Brain Tumor Resection Does not Depend on Surgery Alone—Role of Hemodynamics. Sci. Rep. 2017, 7, 5585. [Google Scholar] [CrossRef]
- Sivasanker, M.; Madhugiri, V.S.; Moiyadi, A.V.; Shetty, P.; Subi, T.S. Surgery for brain metastases: An analysis of outcomes and factors affecting survival. Clin. Neurol. Neurosurg. 2018, 168, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Gould, J. Breaking down the epidemiology of brain cancer. Nature 2018, 561, S40–S41. [Google Scholar] [CrossRef]
- Li, Y.; Lu, B.; Sheng, L.; Zhu, Z.; Sun, H.; Zhou, Y.; Yang, Y.; Xue, D.; Chen, W.; Tian, X.; et al. Hexokinase 2-dependent hyperglycolysis driving microglial activation contributes to ischemic brain injury. J. Neurochem. 2018, 144, 186–200. [Google Scholar] [CrossRef] [PubMed]
- Mazighi, M.; Labreuche, J.; Amarenco, P. Glucose level and brain infarction: A prospective case-control study and prospective study. Int. J. Stroke Off. J. Int. Stroke Soc. 2009, 4, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Brallier, J.W.; Dalal, P.J.; McCormick, P.J.; Lin, H.M.; Deiner, S.G. Elevated Intraoperative Serum Lactate during Craniotomy Is Associated with New Neurological Deficit and Longer Length of Stay. J. Neurosurg. Anesthesiol. 2017, 29, 388–392. [Google Scholar] [CrossRef]
- Freire Jorge, P.; Wieringa, N.; de Felice, E.; van der Horst, I.C.C.; Oude Lansink, A.; Nijsten, M.W. The association of early combined lactate and glucose levels with subsequent renal and liver dysfunction and hospital mortality in critically ill patients. Crit. Care (Lond. Engl.) 2017, 21, 218. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Bi, J.; Zhang, J.; Du, Z.; Ren, Y.; Wei, S.; Ren, F.; Wu, Z.; Lv, Y.; Wu, R. The Impact of Serum Glucose on the Predictive Value of Serum Lactate for Hospital Mortality in Critically Ill Surgical Patients. Dis. Mark. 2019, 2019, 1578502. [Google Scholar] [CrossRef] [PubMed]
- Van Donkelaar, C.E.; Dijkland, S.A.; van den Bergh, W.M.; Bakker, J.; Dippel, D.W.; Nijsten, M.W.; Van Der Jagt, M. Early Circulating Lactate and Glucose Levels after Aneurysmal Subarachnoid Hemorrhage Correlate with Poor Outcome and Delayed Cerebral Ischemia: A Two-Center Cohort Study. Crit. Care Med. 2016, 44, 966–972. [Google Scholar] [CrossRef]
- Veldeman, M.; Hollig, A.; Clusmann, H.; Stevanovic, A.; Rossaint, R.; Coburn, M. Delayed cerebral ischaemia prevention and treatment after aneurysmal subarachnoid haemorrhage: A systematic review. Br. J. Anaesth. 2016, 117, 17–40. [Google Scholar] [CrossRef]
- Aisiku, I.P.; Chen, P.R.; Truong, H.; Monsivais, D.R.; Edlow, J. Admission serum lactate predicts mortality in aneurysmal subarachnoid hemorrhage. Am. J. Emerg. Med. 2016, 34, 708–712. [Google Scholar] [CrossRef]
- Van Leeuwen, A.F.; Evans, R.G.; Ludbrook, J. Haemodynamic responses to acute blood loss: New roles for the heart, brain and endogenous opioids. Anaesth. Intensive Care 1989, 17, 312–319. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, C.E.; Brambrink, A.M.; Aziz, M.F.; Macri, E.; Raines, J.; Multani-Kohol, A.; Hinson, H.; Lutsep, H.L.; Clark, W.M.; Fields, J.D. Association of intraprocedural blood pressure and end tidal carbon dioxide with outcome after acute stroke intervention. Neurocritical Care 2014, 20, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Solaiman, O.; Singh, J.M. Hypocapnia in aneurysmal subarachnoid hemorrhage: Incidence and association with poor clinical outcomes. J. Neurosurg. Anesthesiol. 2013, 25, 254–261. [Google Scholar] [CrossRef] [PubMed]


| Age at Date of Surgery (n = 234) | Mean 61.3 (Range 18–86) Years |
|---|---|
| Age at date of initial diagnosis (n = 213) | Mean 58.1 years |
| Sex, female | 124/234 (53.0%) |
| Recurrent disease | 17/233 (7.3%) |
| KPS preoperative (n = 232) | 80 (20–100) % |
| KPS postoperative (n = 234) | 80 (0–100) % |
| Death during FU | 99/234 (42.3%) |
| Arterial hypertension | 81/228 (35.5%) |
| Diabetes | 24/229 (10.5%) |
| Previous thromboembolic events | 20/229 (8.7%) |
| PAOD | 5/228 (2.2%) |
| Smoker | 71/229 (31.0%) |
| Postoperative infarct volume (n = 213) | Median 1.1 (IQR 0–3–7) cm3 |
| OP Time (n = 225) | Mean 147.1 (SD 62.3) min |
| Blood loss (n = 231) | Mean 363.7 (SD 349.4) mL |
| Tumor Entity | Tumor Entity-Subgroup | No. Patients | % |
|---|---|---|---|
| lung | 75 | 32.1 | |
| breast | 37 | 15.8 | |
| malignant melanoma | 35 | 15.0 | |
| gastrointestinal | rectum | 8 | 3.4 |
| colon | 6 | 2.6 | |
| AEG | 3 | 1.3 | |
| pancreas | 2 | 0.9 | |
| gastric | 1 | 0.4 | |
| sigma | 1 | 0.4 | |
| urogenital | renal | 8 | 3.4 |
| bladder | 4 | 1.7 | |
| men | prostate | 4 | 1.7 |
| testicle | 7 | 3.0 | |
| women | ovarial | 7 | 3.0 |
| endometric | 1 | 0.4 | |
| hepatocellular | 4 | 1.7 | |
| parotid | 4 | 1.7 | |
| thyroid | 2 | 0.9 | |
| skin | 3 | 1.3 | |
| MPNST | 2 | 0.9 | |
| ewing sarcoma | 1 | 0.4 | |
| choroidal melanoma | 1 | 0.4 | |
| plasmocytoma | 1 | 0.4 | |
| unknown | 17 | 7.3 |
| Parameter | p | (i/m) × q; q = 0.15 | Spearman’s Coefficient with FDR Correction |
|---|---|---|---|
| blood glucose (mg/dL) | 0.00358315 | 0.0046875 | 0.20659276 |
| blood loss (mL) | 0.00587021 | 0.009375 | 0.18951449 |
| lactate mg/dL (mmol/L) | 0.01368411 | 0.0140625 | 0.17630288 |
| PaCO2 (mmHg) | 0.04454785 | 0.01875 | −0.14293733 |
| heart rate SD | 0.07068349 | 0.0234375 | 0.12468846 |
| oxygen saturation SD | 0.07193419 | 0.028125 | 0.12414285 |
| systolic blood pressure, mean | 0.08442738 | 0.0328125 | 0.11907649 |
| heart rate, mean | 0.0937836 | 0.0375 | 0.11566422 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lange, N.; Urich, J.; Barz, M.; Aftahy, K.; Wagner, A.; Albers, L.; Bette, S.; Wiestler, B.; Bretschneider, M.; Meyer, B.; et al. Metabolic Parameters Influence Brain Infarction and Outcome after Resection of Brain Metastases. Cancers 2020, 12, 1127. https://doi.org/10.3390/cancers12051127
Lange N, Urich J, Barz M, Aftahy K, Wagner A, Albers L, Bette S, Wiestler B, Bretschneider M, Meyer B, et al. Metabolic Parameters Influence Brain Infarction and Outcome after Resection of Brain Metastases. Cancers. 2020; 12(5):1127. https://doi.org/10.3390/cancers12051127
Chicago/Turabian StyleLange, Nicole, Julia Urich, Melanie Barz, Kaywan Aftahy, Arthur Wagner, Lucia Albers, Stefanie Bette, Benedikt Wiestler, Martin Bretschneider, Bernhard Meyer, and et al. 2020. "Metabolic Parameters Influence Brain Infarction and Outcome after Resection of Brain Metastases" Cancers 12, no. 5: 1127. https://doi.org/10.3390/cancers12051127
APA StyleLange, N., Urich, J., Barz, M., Aftahy, K., Wagner, A., Albers, L., Bette, S., Wiestler, B., Bretschneider, M., Meyer, B., & Gempt, J. (2020). Metabolic Parameters Influence Brain Infarction and Outcome after Resection of Brain Metastases. Cancers, 12(5), 1127. https://doi.org/10.3390/cancers12051127






