Author Contributions
Conceptualization: E.S.G., G.O., L.K.; data curation: E.S.G., T.S., K.S., D.K.; formal analysis: E.S.G., G.O., D.P., R.N.; investigation: E.S.G., S.G., M.S.; methodology: E.S.G., G.O., D.P., R.N., D.K.; project administration: E.S.G.; resources: D.K., J.W., W.D., L.K.; software: R.N.; supervision: W.D., L.K.; validation: E.S.G., G.O., D.P., R.N., L.K.; writing—original draft: E.S.G., D.P., S.G., R.N.; writing—review & editing: G.O., S.D.T., J.W., B.T., L.K. All authors have read and agreed to the published version of the manuscript.
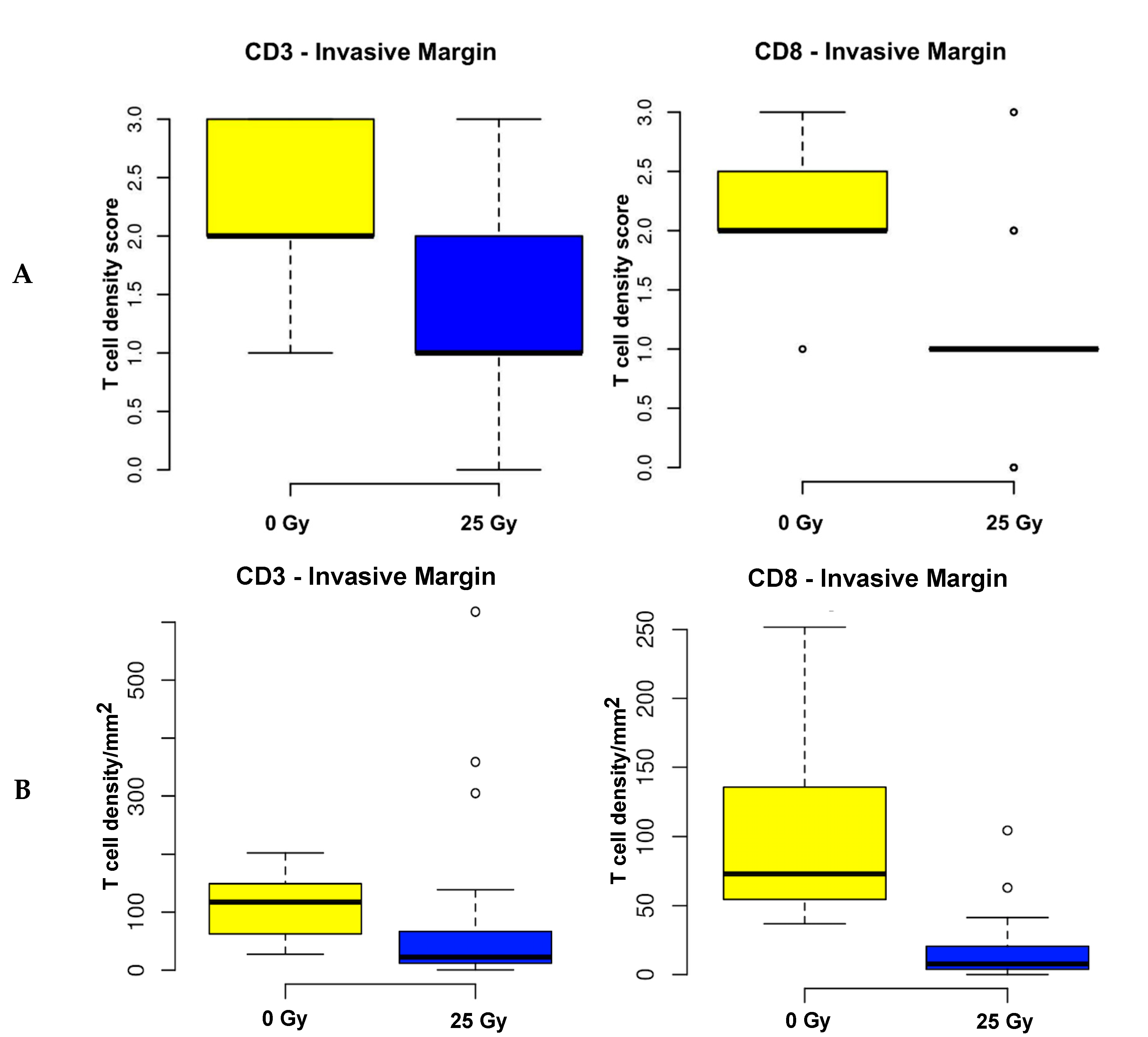
Figure 1.
Correlative analysis of T cell density in preoperatively irradiated vs. treatment-naïve rectal cancer specimens quantified by analogue using full tissue sections (A) and on virtually established tissue microarray (TMA; (B) 2 cores per tumor region and (C) 6 cores per tumor region). A. 25 Gy of preoperative irradiation significantly attenuates marginal density of CD8 positive T cells observed on full tissue sections (p < 0.0001); a trend was shown towards less CD3 density in the IM (p = 0.0970). B. 25 Gy of preoperative irradiation significantly attenuates marginal density of CD3 as well as CD8 positive T cells seen on virtual TMAs using 2 cores (p < 0.0001 each). C. 25 Gy of preoperative irradiation significantly attenuates marginal density of CD3 as well as CD8 T cells seen on virtual TMA using 6 cores (p < 0.0001 each).
Figure 1.
Correlative analysis of T cell density in preoperatively irradiated vs. treatment-naïve rectal cancer specimens quantified by analogue using full tissue sections (A) and on virtually established tissue microarray (TMA; (B) 2 cores per tumor region and (C) 6 cores per tumor region). A. 25 Gy of preoperative irradiation significantly attenuates marginal density of CD8 positive T cells observed on full tissue sections (p < 0.0001); a trend was shown towards less CD3 density in the IM (p = 0.0970). B. 25 Gy of preoperative irradiation significantly attenuates marginal density of CD3 as well as CD8 positive T cells seen on virtual TMAs using 2 cores (p < 0.0001 each). C. 25 Gy of preoperative irradiation significantly attenuates marginal density of CD3 as well as CD8 T cells seen on virtual TMA using 6 cores (p < 0.0001 each).
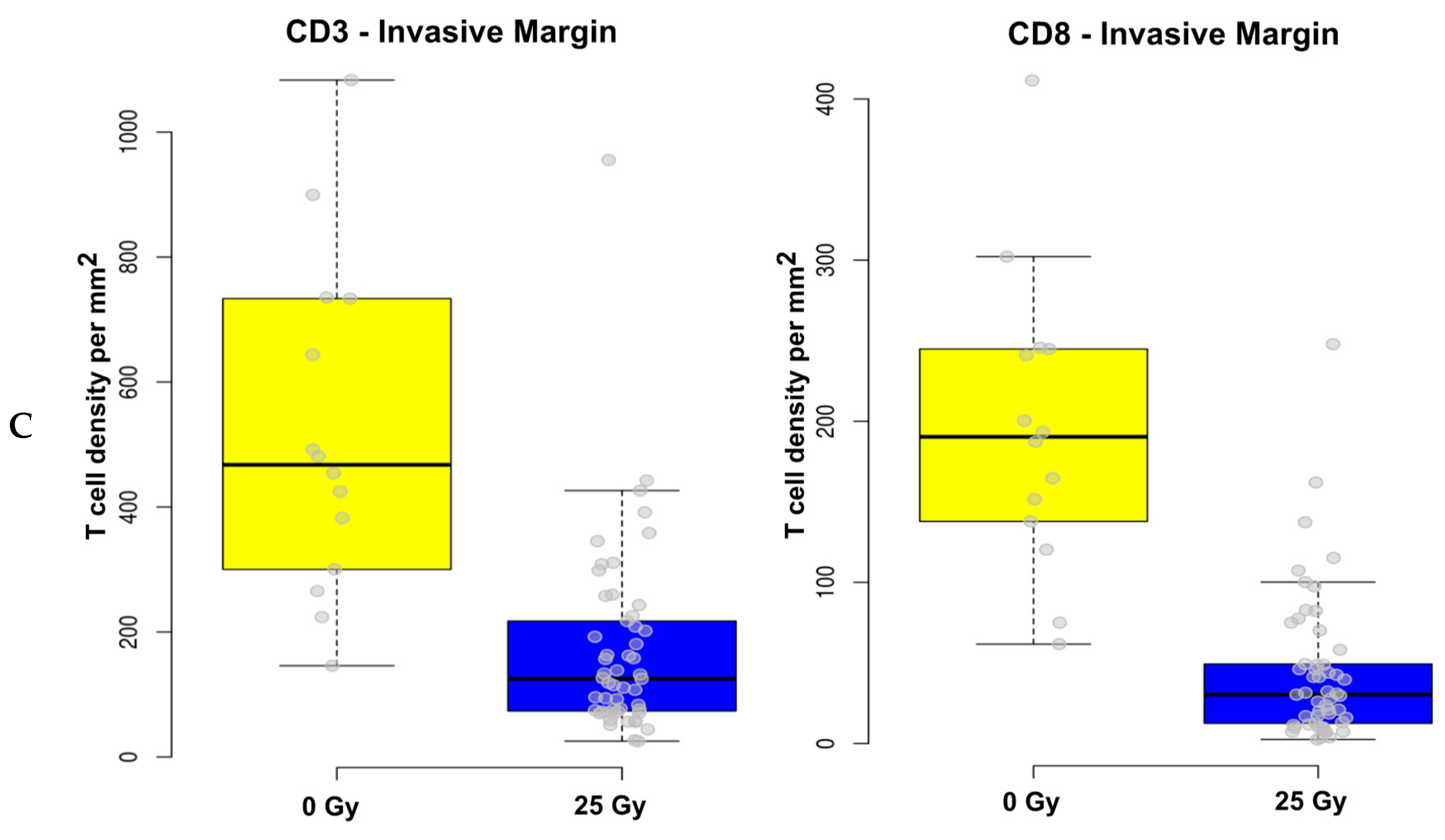
Figure 2.
Virtual TMA establishment on scanned full section slides of rectal cancer (RC) samples using StrataQuestTM®. (Left): Randomly selected virtual cores in the central tumor (2x 0.6mm diameter) and in the invasive margin (2x 1mm diameter) on full section slides of RC samples. (Right): Expansion of virtual core establishment from 2 to a maximum of 6 cores per tumor region taking into account the minimum amount of tumor area available amongst all full section slides. Note. Bar graph = 500 µm.
Figure 2.
Virtual TMA establishment on scanned full section slides of rectal cancer (RC) samples using StrataQuestTM®. (Left): Randomly selected virtual cores in the central tumor (2x 0.6mm diameter) and in the invasive margin (2x 1mm diameter) on full section slides of RC samples. (Right): Expansion of virtual core establishment from 2 to a maximum of 6 cores per tumor region taking into account the minimum amount of tumor area available amongst all full section slides. Note. Bar graph = 500 µm.
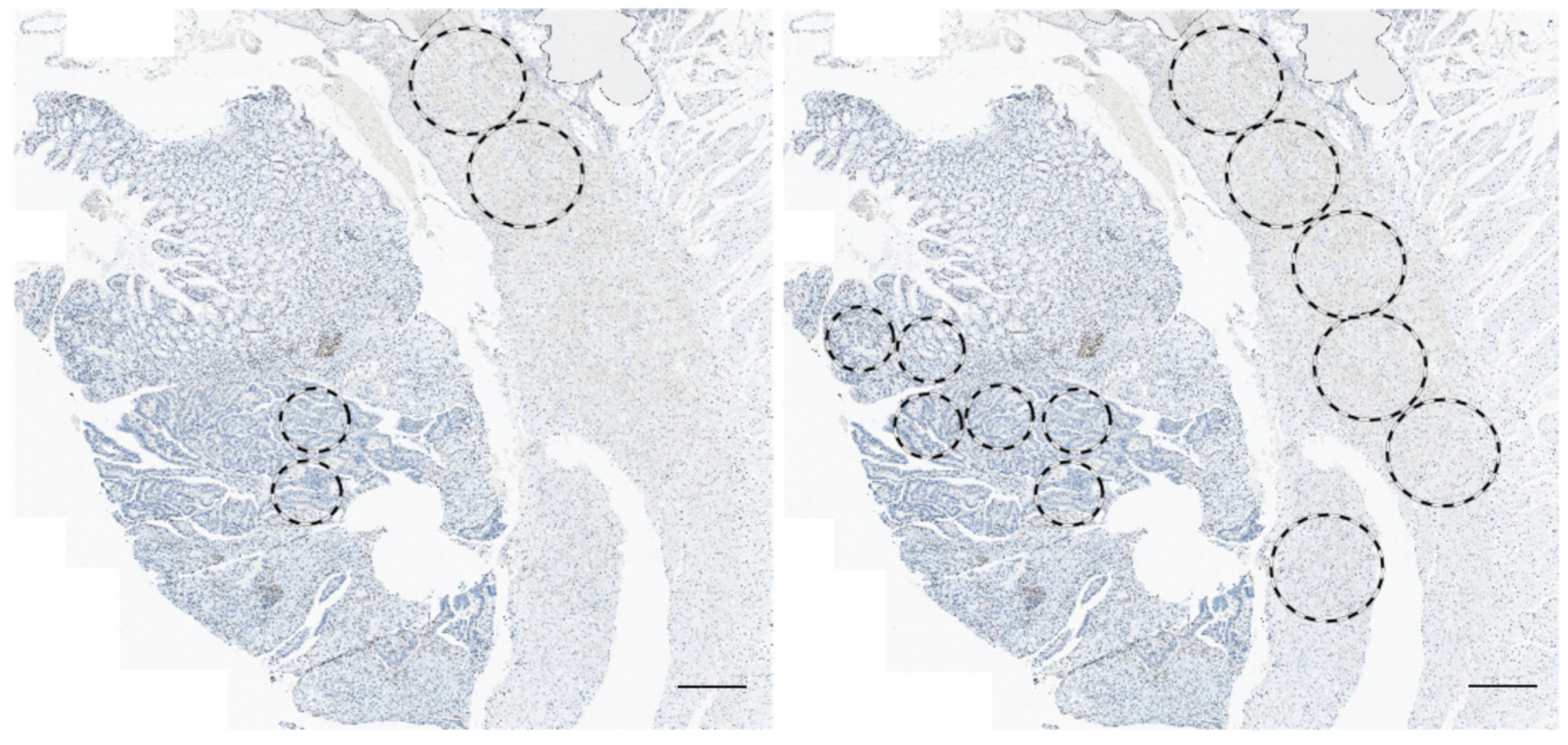
Figure 3.
Correlative analysis of T cell densities quantified on full tissue sections (score 0–3) vs. mean T cell densities of 6 cores. T cell densities of the 2 quantification methods match with respect to correlational strength in the different tumor areas. Top: Tumoral and marginal CD3 positive T cells: R = 0.35 (medium correlation) and R = 0.14 (weak correlation), respectively. Bottom: Tumoral and marginal CD8 positive T cells: R = 0.45 (medium correlation) and R = 0.69 (good correlation), respectively. Note. Score: no (0), low (1), moderate (2) or high (3) protein levels with respect to positive T cells or TILs present; R—Spearman’s correlation coefficient.
Figure 3.
Correlative analysis of T cell densities quantified on full tissue sections (score 0–3) vs. mean T cell densities of 6 cores. T cell densities of the 2 quantification methods match with respect to correlational strength in the different tumor areas. Top: Tumoral and marginal CD3 positive T cells: R = 0.35 (medium correlation) and R = 0.14 (weak correlation), respectively. Bottom: Tumoral and marginal CD8 positive T cells: R = 0.45 (medium correlation) and R = 0.69 (good correlation), respectively. Note. Score: no (0), low (1), moderate (2) or high (3) protein levels with respect to positive T cells or TILs present; R—Spearman’s correlation coefficient.
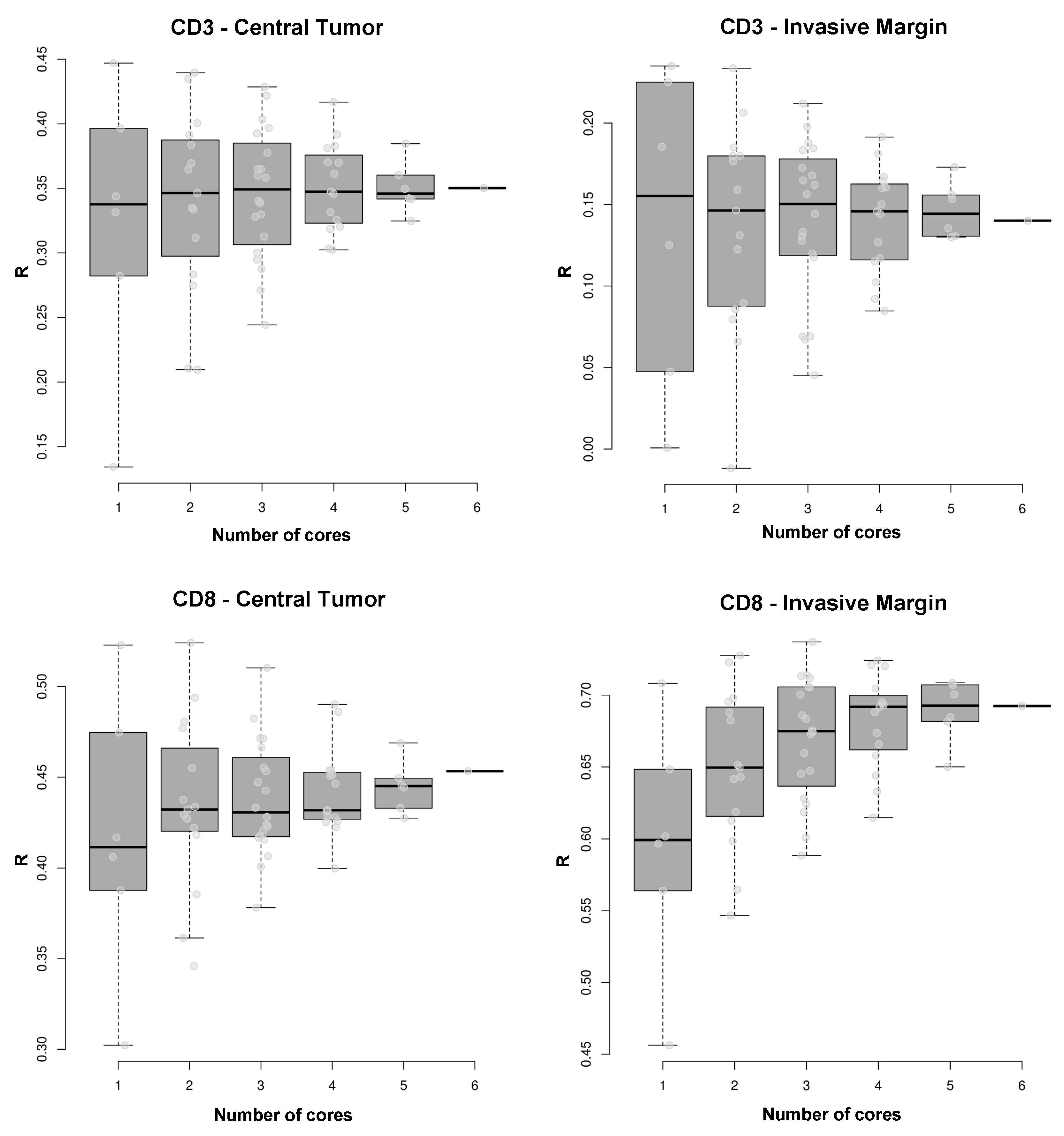
Figure 4.
Variance of correlations between T cell densities using analogue quantification and T cell densities using any possible combination of 1 to 6 virtual TMA cores to estimate the mean. Ascending numbers of cores resulted in a more precise approximation of correlation to the analogue values in each tumor area, except for marginal CD3 density. Top: Tumoral CD3: 1 core, R = 0.34 vs. 6 cores, R = 0.35 (moderate correlation); marginal CD3: 1 core, R = 0.16 vs. 6 cores, R = 0.14 (weak correlation), respectively. Bottom: Tumoral CD8: 1 core, R = 0.41 vs. 6 cores, R = 0.46 (strong correlation); marginal CD8: 1 core, R = 0.60 vs. 6 cores, R = 0.69 (strong correlation), respectively; however, adding cores for quantification analysis led to a more precise approximation of the correlation between analogue and virtual TMA quantification. Note. R—Spearman’s correlation coefficient.
Figure 4.
Variance of correlations between T cell densities using analogue quantification and T cell densities using any possible combination of 1 to 6 virtual TMA cores to estimate the mean. Ascending numbers of cores resulted in a more precise approximation of correlation to the analogue values in each tumor area, except for marginal CD3 density. Top: Tumoral CD3: 1 core, R = 0.34 vs. 6 cores, R = 0.35 (moderate correlation); marginal CD3: 1 core, R = 0.16 vs. 6 cores, R = 0.14 (weak correlation), respectively. Bottom: Tumoral CD8: 1 core, R = 0.41 vs. 6 cores, R = 0.46 (strong correlation); marginal CD8: 1 core, R = 0.60 vs. 6 cores, R = 0.69 (strong correlation), respectively; however, adding cores for quantification analysis led to a more precise approximation of the correlation between analogue and virtual TMA quantification. Note. R—Spearman’s correlation coefficient.
Figure 5.
Correlation of the mean T cell densities of 6 cores with mean T cell densities of full tissue sections (dashed line) versus ascending sorted mean T cell densities of 1–6 cores. Strength of correlation between T cell densities on full tissue sections and virtual TMA does not depend on the mean T cell density of the cores chosen for correlation. From bottom to top: Tumoral CD3 – low T cell density core, R = 0.35 vs. high density core, Rs = 0.26 (moderate correlation), max. core 3, R = 0.40; marginal CD3 – low T cell density core, R = 0.18 vs. high density core, R = 0.17 (weak correlation), max. core 2, R = 0.19; tumoral CD8 – low T cell density core, R = 0.42 vs. high density core, R = 0.40 (moderate correlation), max. core 2, R = 0.51; marginal CD8 - low T cell density core, R = 0.64 vs. high density core, R = 0.66 (strong correlation); max. core 4, R = 0.70. Note. R—Spearman’s correlation coefficient.
Figure 5.
Correlation of the mean T cell densities of 6 cores with mean T cell densities of full tissue sections (dashed line) versus ascending sorted mean T cell densities of 1–6 cores. Strength of correlation between T cell densities on full tissue sections and virtual TMA does not depend on the mean T cell density of the cores chosen for correlation. From bottom to top: Tumoral CD3 – low T cell density core, R = 0.35 vs. high density core, Rs = 0.26 (moderate correlation), max. core 3, R = 0.40; marginal CD3 – low T cell density core, R = 0.18 vs. high density core, R = 0.17 (weak correlation), max. core 2, R = 0.19; tumoral CD8 – low T cell density core, R = 0.42 vs. high density core, R = 0.40 (moderate correlation), max. core 2, R = 0.51; marginal CD8 - low T cell density core, R = 0.64 vs. high density core, R = 0.66 (strong correlation); max. core 4, R = 0.70. Note. R—Spearman’s correlation coefficient.
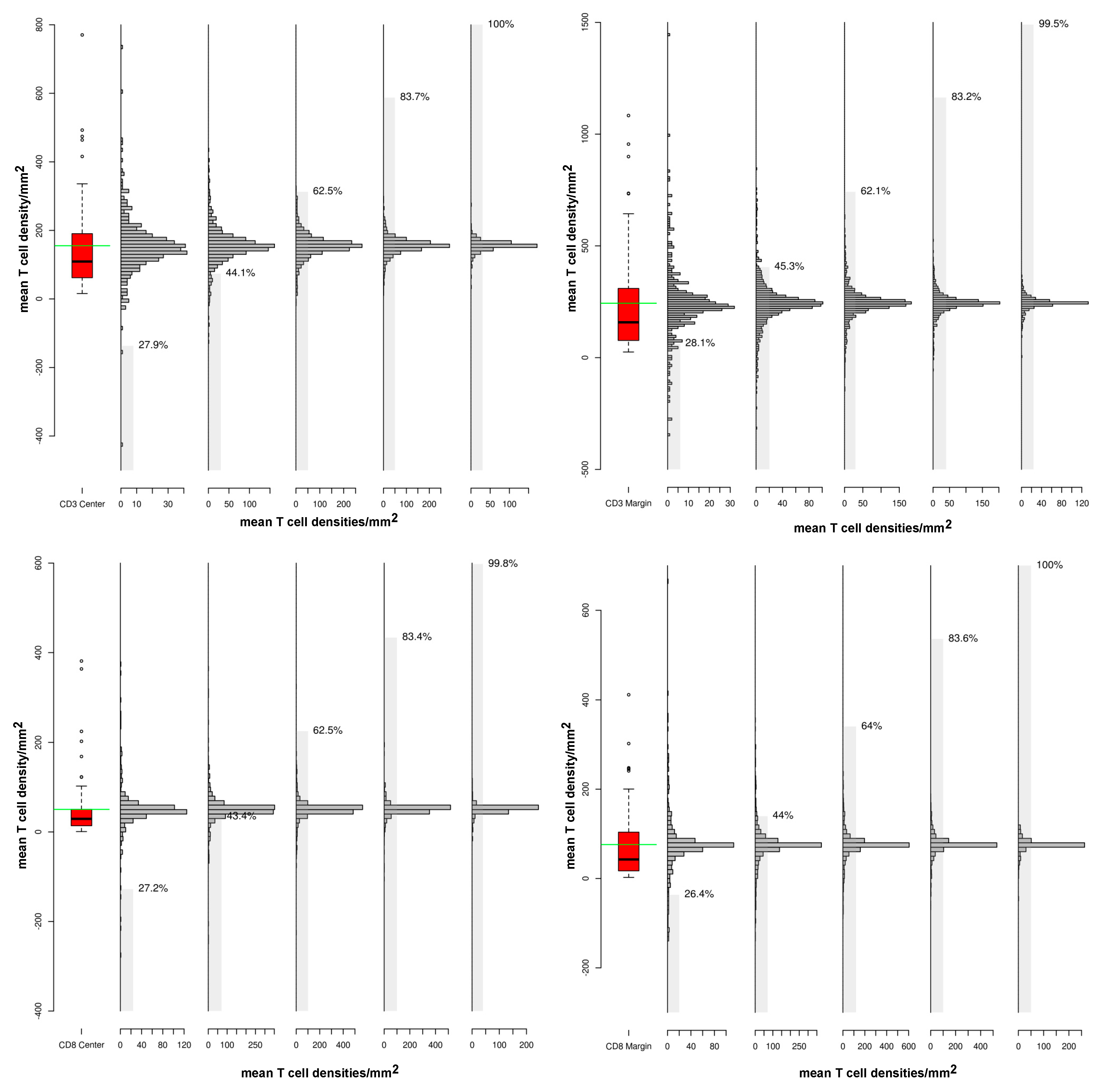
Figure 6.
Variations in T cell densities based on the number of cores chosen for quantification by virtual tissue microarray. Quantification of mean T cell densities using 5 cores for each patient (bar graph) shows a higher range of variation compared to mean T cell densities using 6 cores from all patients (boxplot). Top: Tumoral CD3 density: range 0–350 (boxplot); 1 core: 0–40 (SE = 28.1%) vs. 5 cores: 0–150 (SE = 99.5%); marginal CD3 density: range 0–650 (boxplot); 1 core: 0–30 (SE = 27.9%) vs. 5 cores 0–120 (SE = 100%). Bottom: Marginal CD8 density: range 0–100 (boxplot); 1 core: 0–120 (SE = 27.2%) vs. 5 cores 0-200 (SE = 99.8%); tumoral CD8 density: range 0–200 (boxplot); 1 core: 0–100 (SE = 26.4%) vs. 5 cores: 0-250 (SE = 100%). Note. Range - range of variation in T cell density; SE—standard error.
Figure 6.
Variations in T cell densities based on the number of cores chosen for quantification by virtual tissue microarray. Quantification of mean T cell densities using 5 cores for each patient (bar graph) shows a higher range of variation compared to mean T cell densities using 6 cores from all patients (boxplot). Top: Tumoral CD3 density: range 0–350 (boxplot); 1 core: 0–40 (SE = 28.1%) vs. 5 cores: 0–150 (SE = 99.5%); marginal CD3 density: range 0–650 (boxplot); 1 core: 0–30 (SE = 27.9%) vs. 5 cores 0–120 (SE = 100%). Bottom: Marginal CD8 density: range 0–100 (boxplot); 1 core: 0–120 (SE = 27.2%) vs. 5 cores 0-200 (SE = 99.8%); tumoral CD8 density: range 0–200 (boxplot); 1 core: 0–100 (SE = 26.4%) vs. 5 cores: 0-250 (SE = 100%). Note. Range - range of variation in T cell density; SE—standard error.
Table 1.
Patient and tumor characteristics in relation to the level of CD3 T cell expression determined analogously on full tissue sections.
Table 1.
Patient and tumor characteristics in relation to the level of CD3 T cell expression determined analogously on full tissue sections.
| | CD3 – central tumor | CD3 – invasive margin |
|---|
| Factor | No. of patients (%) | 0 | 1 | 2 | 3 | 0 | 1 | 2 | 3 |
|---|
| | 75 (100.0%) | 9 (12.0%) | 34 (45.7%) | 19 (25.3%) | 13 (17.3%) | 8 (10.7%) | 28 (37.3%) | 28 (37.3%) | 1 (14.7%) |
| Median age (range) | 77 (51–94) | n.s.* | n.s.* |
| Sex | n.s.** | n.s.** |
| female | 31 (41.3%) | 3 (4.0%) | 16 (21.3%) | 7 (9.3%) | 5 (6.7%) | 3 (4.0%) | 12 (16.0%) | 13 (17.3%) | 3 (4.0%) |
| male | 44 (58.7%) | 6 (8.0%) | 18 (24.0%) | 12 (16.0%) | 8 (19.7%) | 5 (6.7%) | 16 (21.3%) | 15 (20.0%) | 8 (10.7%) |
| Preoperative RTx | n.s.** | p = 0.006** |
| Yes | 60 (80.0%) | 26 (34.7%) | 9 (12.0%) | 26 (34.7%) | 9 (12.0%) | 26 (34.7%) | 9 (12.0%) | 26 (34.7%) | 3 (4.0%) |
| No | 15 (20.0%) | 8 (10.7%) | 0 (0.0%) | 8 (10.7%) | 0 (0.0%) | 8 (10.7%) | 0 (0.0%) | 8 (10.7%) | 4 (5.3%) |
| Tumor grading (G) | n.s.* | n.s.* |
| Good (G1) | 1 (1.3%) | 0 (0.0%) | 0 (0.0%) | 1 (1.3%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (1.3%) | 0 (0.0%) |
| Moderate (G2) | 63 (84.0%) | 8 (10.7%) | 25 (37.3%) | 15 (20.0%) | 12 (16.0%) | 8 (10.7%) | 22 (29.3%) | 25 (33.3%) | 8 (10.7%) |
| Poor (G3) | 11 (14.7%) | 1 (1.3%) | 6 (8.0%) | 3 (4.0%) | 1 (1.3%) | 0 (0.0%) | 6 (8.0%) | 2 (2.7%) | 3 (4.0%) |
| Dukes stage | n.s.* | n.s.* |
| Stage A | 21 (28.0%) | 2 (2.7%) | 7 (9.3%) | 6 (8.0%) | 6 (8.0%) | 2 (2.7%) | 6 (8.0%) | 12 (16.0%) | 1 (1.3%) |
| Stage B | 25 (33.3%) | 3 (4.0%) | 14 (18.7%) | 4 (5.3%) | 4 (5.3%) | 2 (2.7%) | 11 (14.7%) | 9 (12.0%) | 3 (4.0%) |
| Stage C | 24 (32.0%) | 2 (2.7%) | 12 (16.0%) | 8 (10.7%) | 2 (2.7%) | 3 (4.0%) | 11 (14.7%) | 3 (4.0%) | 7 (9.3%) |
| Stage D | 5 (6.7%) | 2 (2.6%) | 1 (1.3%) | 1 (1.3%) | 1 (1.3%) | 1 (1.3%) | 0 (0.0%) | 4 (5.3%) | 0 (0.0%) |
Table 2.
Patient and tumor characteristics in relation to the level of CD8 T cell expression determined analogously on full tissue sections.
Table 2.
Patient and tumor characteristics in relation to the level of CD8 T cell expression determined analogously on full tissue sections.
| | CD8 – central tumor | CD8 – invasive margin |
|---|
| Factor | No. of patients (%) | 0 | 1 | 2 | 3 | 0 | 1 | 2 | 3 |
|---|
| | 75 (100.0%) | 15 (20.0%) | 46 (61.3%) | 10 (13.3%) | 4 (5.3%) | 12 (16.0%) | 37 (49.3%) | 19 (25.3%) | 7 (9.3%) |
| Median age (range) | 77 (51–94) | n.s.* | n.s.* |
| Sex | n.s.** | n.s.** |
| female | 31 (41.3%) | 7 (9.3%) | 19 (25.3%) | 3 (4.0%) | 2 (2.7%) | 4 (5.3%) | 17 (22.7%) | 7 (9.3%) | 3 (4.0%) |
| male | 44 (58.7%) | 8 (10.7%) | 27 (36.0%) | 7 (9.3%) | 2 (2.7%) | 8 (10.7%) | 20 (26.7%) | 12 (16.0%) | 4 (5.3%) |
| Preoperative RTx | p = 0.017** | p = 0.001** |
| Yes | 60 (80.0%) | 15 (20.0%) | 36 (48.0%) | 7 (9.3%) | 2 (2.7%) | 12 (16.0%) | 35 (46.7%) | 10 (13.3%) | 3 (4.0%) |
| No | 15 (20.0%) | 0 (0.0%) | 10 (13.3%) | 3 (4.0%) | 2 (2.7%) | 0 (0.0%) | 2 (2.7%) | 9 (12.0%) | 4 (5.3%) |
| Tumor grading (G) | n.s.* | n.s.* |
| Good (G1) | 1 (1.3%) | 0 (0.0%) | 1 (1.3%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (1.3%) | 0 (0.0%) | 0 (0.0%) |
| Moderate (G2) | 63 (84.0%) | 13 (17.3%) | 37 (49.3%) | 10 (13.3%) | 3 4.0%) | 10 (13.3%) | 30 (40.0%) | 17 (22.7%) | 6 (8.0%) |
| Poor (G3) | 11 (14.7%) | 2 (2.7%) | 8 (10.7%) | 0 (0.0%) | 1 (1.3%) | 2 (2.7%) | 6 (8.0%) | 2 (2.7%) | 1 (1.3%) |
| Dukes stage | n.s.* | n.s.* |
| Stage A | 21 (28.0%) | 4 (5.3%) | 11 (14.7%) | 6 (8.0%) | 0 (0.0%) | 2 (2.7%) | 12 (16.0%) | 7 (9.3%) | 0 (0.0%) |
| Stage B | 25 (33.3%) | 6 (8.0%) | 15 (20.0%) | 2 (2.7%) | 2 (2.7%) | 5 (6.7%) | 12 (16.0%) | 5 (6.7%) | 3 (4.0%) |
| Stage C | 24 (32.0%) | 4 (5.3%) | 17 (22.7%) | 1 (1.3%) | 2 (2.7%) | 5 (6.7%) | 11 (14.7%) | 5 (6.7%) | 3 (4.0%) |
| Stage D | 5 (6.7%) | 1 (2.7%) | 3 (4.0%) | 1 (2.7%) | 0 (0.0%) | 0 (0.0%) | 2 (2.7%) | 2 (2.7%) | 1 (1.3%) |
Table 3.
Patient and tumor characteristics in relation to the level of PD-1 immune checkpoint protein expression determined analogously on full tissue sections.
Table 3.
Patient and tumor characteristics in relation to the level of PD-1 immune checkpoint protein expression determined analogously on full tissue sections.
| | PD-1 – central tumor* | PD-1 – invasive margin* |
|---|
| Factor | No. of patients (%) | 0 | 1 | 2 | 0 | 1 | 2 |
|---|
| | 75 (100%) | 25 (33.3%) | 42 (56.0%) | 8 (10.7%) | 26 (34.7%) | 37 (49.3%) | 12 (16.0%) |
| Median age (range) | 77 (51–94) | n.s.** | n.s.** |
| Sex | n.s.*** | n.s.*** |
| female | 31 (41.3%) | 10 (13.3%) | 19 (25.3%) | 2 (2.7%) | 12 (16.0%) | 13 (17.3%) | 6 (8.0%) |
| male | 44 (58.7%) | 15 (20.0%) | 23 (30.7%) | 6 (8.0%) | 14 (18.7%) | 24 (32.0%) | 6 (8.0%) |
| Preoperative RTx | n.s.*** | p = 0.005*** |
| Yes | 60 (80.0%) | 23 (30.7%) | 31 (41.3%) | 6 (8.0%) | 2 (2.7%) | 7 (9.3%) | 6 (8.0%) |
| No | 15 (20.0%) | 2 (2.7%) | 11 (14.6%) | 2 (2.7%) | 24 (32.0%) | 30 (40.0%) | 6 (8.0%) |
| Tumor grading (G) | n.s.** | n.s.** |
| Good (G1) | 1 (1.3%) | 0 (0.0%) | 1 (1.3%) | 0 (0.0%) | 0 (0.0%) | 1 (1.3%) | 0 (0.0%) |
| Moderate (G2) | 63 (84.0%) | 21 (28.0%) | 35 (46.7%) | 7 (9.3%) | 22 (29.3%) | 31 (41.3%) | 10 (13.3%) |
| Poor (G3) | 11 (14.7%) | 4 (5.3%) | 6 (8.0%) | 1 (1.3%) | 4 (5.3%) | 5 (6.7%) | 2 (2.7%) |
| Dukes stage | n.s.** | n.s.** |
| Stage A | 21 (28.0%) | 4 (5.3%) | 13 (17.4%) | 4 (5.3%) | 3 (4.0%) | 15 (20.0%) | 3 (4.0%) |
| Stage B | 25 (33.3%) | 11 (14.7%) | 11 (14.6%) | 3 (4.0%) | 11 (14.6%) | 10 (13.3%) | 4 (5.3%) |
| Stage C | 24 (32.0%) | 9 (12.0%) | 14 (18.7%) | 1 (1.3%) | 11 (14.6%) | 10 (13.3%) | 3 (4.0%) |
| Stage D | 5 (6.7%) | 1 (1.3%) | 4 (5.3%) | 0 (0.0%) | 1 (1.3%) | 2 (2.7%) | 2 (2.7%) |
Table 4.
Patient and tumor characteristics in relation to the level of PD-L1 immune checkpoint protein expression determined analogously on full tissue sections.
Table 4.
Patient and tumor characteristics in relation to the level of PD-L1 immune checkpoint protein expression determined analogously on full tissue sections.
| | PD-L1 – central tumor* | PD-L1 – invasive margin* |
|---|
| Factor | No. of patients (%) | 0 | 1 | 2 | 3 | 0 | 1 | 2 | 3 |
|---|
| | 75 (100.0%) | 42 (56.0%) | 15 (20.0%) | 15 (20.0%) | 3 (4.0%) | 47 (62.7%) | 12 (16.0%) | 13 (17.3%) | 3 (4.0%) |
| Median age (range) | 77 (51–94) | n.s.** | n.s.** |
| Sex | n.s.*** | n.s.*** |
| female | 31 (41.3%) | 16 (21.3%) | 7 (9.3%) | 6 (8.0%) | 2 (2.7%) | 20 (26.7%) | 4 (5.3%) | 6 (8.0%) | 1 (1.3%) |
| male | 44 (58.7%) | 26 (34.7%) | 8 (10.7%) | 9 (12.0%) | 1 (1.3%) | 27 (36%) | 8 (10.7%) | 7 (9.3%) | 2 (2.7%) |
| Preoperative RTx | n.s.*** | n.s.*** |
| Yes | 60 (80.0%) | 36 (48.0%) | 10 (13.3%) | 11 (14.7%) | 3 (4.0%) | 40 (53.3%) | 9 (12.0%) | 8 (10.7%) | 3 (4.0%) |
| No | 15 (20.0%) | 6 (8.0%) | 5 (6.7%) | 4 (5.3%) | 0 (0.0%) | 7 (9.3%) | 3 (4.0%) | 5 (6.7%) | 0 (0.0%) |
| Tumor grading (G) | n.s.** | n.s.** |
| Good (G1) | 1 (1.3%) | 0 (0.0%) | 0 (0.0%) | 1 (1.3%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (1.33%) | 0 (0.0%) |
| Moderate (G2) | 63 (84.0%) | 36 (48.0%) | 14 (18.7%) | 10 (13.3%) | 3 (4.0%) | 39 (52.0%) | 11 (14.7%) | 10 (13.3%) | 3 (4.0%) |
| Poor (G3) | 11 (14.7%) | 6 (8.0%) | 1 (1.33%) | 4 (5.3%) | 0 (0.0%) | 8 (10.7%) | 1 (1.3%) | 2 (3.7%) | 0 (0.0%) |
| Dukes stage | R = −0.23, p = 0.046** | R = −0.24, p = 0.041** |
| Stage A | 21 (28.0%) | 10 (13.3%) | 3 (4.0%) | 7 (9.3%) | 1 (1.3%) | 9 (12.0%) | 4 (5.3%) | 6 (8.0%) | 2 (3.7%) |
| Stage B | 25 (33.3%) | 12 (16.0%) | 7 (9.3%) | 4 (5.3%) | 2 (2.7%) | 18 (24.0%) | 3 (4.0%) | 3 (4.0%) | 1 (1.3%) |
| Stage C | 24 (32.0%) | 16 (21.3%) | 4 (5.3%) | 4 (5.3%) | 0 (0.0%) | 16 (21.2%) | 4 (5.4%) | 4 (5.4%) | 0 (0.0%) |
| Stage D | 5 (6.7%) | 4 (5.3%) | 1 (1.3%) | 0 (0.0%) | 0 (0.0%) | 4 (5.3%) | 1 (1.3%) | 0 (0.0%) | 0 (0.0%) |
Table 5.
Univariate (A) and multiple Cox Regression analysis (B) for disease-free survival of rectal cancer patients quantified using analogue quantification for T cell densities (full sections).
Table 5.
Univariate (A) and multiple Cox Regression analysis (B) for disease-free survival of rectal cancer patients quantified using analogue quantification for T cell densities (full sections).
| Table A | Univariate Analysis |
| Factor | HR | CI95 | p-value |
| CD3 (CT) | 0.45 | 0.23–0.88 | 0.018 |
| CD3 (IM) | 0.33 | 0.16–0.65 | 0.002 |
| CD8 (CT) | n.s. |
| CD8 (IM) | 0.48 | 0.23.1.00 | 0.049 |
| PD-1 (CT) | 0.36 | 0.14–0.94 | 0.037 |
| PD-1 (IM) | 0.30 | 0.11–0.79 | 0.016 |
| PD-L1 (CT) | 0.51 | 0.24–1.10 | 0.087 |
| PD-L1 (IM) | 0.42 | 0.16–1.10 | 0.078 |
| Radiation therapy (25 Gy) | n.s. |
| Nodal positive RC | 3.69 | 1.23–11.08 | 0.020 |
| Table B | Multiple Model |
| Factor | HR | CI95 | p-value |
| CD3 (CT)* | n.s. |
| Nodal positive RC | 2.42 | 0.10–5.87 | 0.050 |
| CD3 (IM)* | 0.46 | 0.27–0.79 | 0.004 |
| Nodal positive RC | 2.49 | 1.03–6.05 | 0.043 |
| CD8 (CT)* | n.s. |
| Nodal positive RC | 2.69 | 1.12–6.53 | 0.029 |
| CD8 (IM)* | 0.59 | 0.33–1.05 | 0.074 |
| Nodal positive RC | 2.78 | 1.14–6.74 | 0.024 |
| PD-1 (CT)* | 0.45 | 0.20–0.99 | 0.048 |
| Nodal positive RC | 2.45 | 1.01–5.94 | 0.047 |
| PD-1 (IM)* | 0.48 | 0.23–0.98 | 0.045 |
| Nodal positive RC | 2.50 | 1.03–6.07 | 0.043 |
| PD-L1 (CT)* | 0.54 | 0.28–1.04 | 0.067 |
| Nodal positive RC | 2.13 | 0.87–5.21 | 0.099 |
| PD-L1 (IM)* | 0.47 | 0.22–1.00 | 0.050 |
| Nodal positive RC | 2.38 | 0.98–5.76 | 0.056 |
Table 6.
Univariate and multiple Cox Regression analysis for overall survival of rectal cancer patients quantified using analogue quantification for TC densities (full sections).
Table 6.
Univariate and multiple Cox Regression analysis for overall survival of rectal cancer patients quantified using analogue quantification for TC densities (full sections).
| Table A | Univariate Analysis |
| Factor | HR | CI95 | p-value |
| CD3 (CT) | 0.45 | 0.23–0.88 | 0.018 |
| CD3 (IM) | 0.33 | 0.16–0.65 | 0.002 |
| CD8 (CT) | n.s. |
| CD8 (IM) | 0.48 | 0.23–1.00 | 0.049 |
| PD-1 (CT) | 0.36 | 0.14–0.94 | 0.037 |
| PD-1 (IM) | 0.30 | 0.11–0.79 | 0.016 |
| PD-L1 (CT) | 0.51 | 0.24–1.10 | 0.087 |
| PD-L1 (IM) | 0.42 | 0.16–1.10 | 0.078 |
| Radiation therapy (25 Gy) | n.s. |
| Nodal positive RC | 3.69 | 1.23–11.08 | 0.020 |
| Table B | Multiple Models |
| Factor | HR | CI95 | p-value |
| CD3 (CT)* | 0.46 | 0.23–0.89 | 0.021 |
| Nodal positive RC | 3.51 | 1.17–10.53 | 0.025 |
| CD3 (IM)* | 0.35 | 0.18–0.69 | 0.002 |
| Nodal positive RC | 3.44 | 1.14–10.33 | 0.028 |
| CD8 (CT)* | 0.44 | 0.21–0.92 | 0.029 |
| Nodal positive RC | 4.18 | 1.39–12.57 | 0.011 |
| CD8 (IM)* | 0.44 | 0.21–0.92 | 0.029 |
| Nodal positive RC | 4.18 | 1.39–12.57 | 0.011 |
| PD-1 (CT)* | 0.35 | 0.13–0.94 | 0.037 |
| Nodal positive RC | 3.62 | 1.21–10.87 | 0.022 |
| PD-1 (IM)* | 0.30 | 0.11–0.81 | 0.017 |
| Nodal positive RC | 3.60 | 1.20–10.86 | 0.023 |
| PD-L1 (CT) | n.i. |
| Nodal positive RC | 4.26 | 1.41–12.86 | 0.010 |
| Radiation Therapy (25Gy) | n.s. |
| PD-L1 (IM)* | 0.44 | 0.16–1.17 | 0.099 |
| Nodal positive RC | 3.36 | 1.12–10.10 | 0.031 |
Table 7.
Univariate and multiple Cox Regression analysis for disease-free survival of rectal cancer patients using the Immunoscore (2 cores per tumor area, virtual TMA).
Table 7.
Univariate and multiple Cox Regression analysis for disease-free survival of rectal cancer patients using the Immunoscore (2 cores per tumor area, virtual TMA).
| Factor | Univariate Analysis* | Multiple Model* |
|---|
| | HR | CI95 | p-value | HR | CI95 | p-value |
|---|
| Immunoscore | n.s. | n.s. |
| Radiation therapy (25 Gy) | n.s. | n.s. |
| Nodal positive RC | n.s. | n.s. |
Table 8.
Univariate and multiple Cox Regression analysis for overall survival of rectal cancer patients using the Immunoscore (2 cores per tumor area, virtual TMA).
Table 8.
Univariate and multiple Cox Regression analysis for overall survival of rectal cancer patients using the Immunoscore (2 cores per tumor area, virtual TMA).
| Factor | Univariate Analysis* | Multiple Model* |
|---|
| | HR | CI95 | p-value | HR | CI95 | p-value |
|---|
| Immunoscore | n.s. | n.i. |
| Radiation therapy (25 Gy) | n.s. | n.i. |
| Nodal positive RC | n.s. | n.s. |
Table 9.
Univariate and multiple Cox Regression analysis for disease-free survival of rectal cancer patients (6 cores per tumor region, virtual TMA).
Table 9.
Univariate and multiple Cox Regression analysis for disease-free survival of rectal cancer patients (6 cores per tumor region, virtual TMA).
| Table A | Univariate Analysis |
| Factor | HR | CI95 | p-value |
| CD3 (CT) | 0.38 | 0.10–1.20 | 0.093 |
| CD3 (IM) | n.s. |
| CD8 (CT) | n.s. |
| CD8 (IM) | n.s. |
| Radiation therapy (25 Gy) | n.s. |
| Nodal positive RC | n.s. |
| Table B | Multiple Model |
| Factor | HR | CI95 | p-value |
| CD3 (CT)* | 0.34 | 0.10-1.20 | 0.093 |
| Nodal positive RC | n.i. |
| CD3 (IM)* | n.i. |
| Nodal positive RC | n.s. |
| CD8 (CT)* | n.i. |
| Nodal positive RC | n.s. |
| CD8 (IM)* | n.i. |
| Nodal positive RC | n.s. |
Table 10.
Univariate and multiple Cox Regression analysis for overall survival of rectal cancer patients (6 cores per tumor region, virtual TMA).
Table 10.
Univariate and multiple Cox Regression analysis for overall survival of rectal cancer patients (6 cores per tumor region, virtual TMA).
| Table A | Univariate Analysis |
| Factor | HR | CI95 | p-value |
| CD3 (CT) | 0.20 | 0.04-1.01 | 0.052 |
| CD3 (IM) | n.s. |
| CD8 (CT) | n.s. |
| CD8 (IM) | n.s. |
| Radiation therapy (25 Gy) | n.s. |
| Nodal positive RC | 2.88 | 0.90–9.20 | 0.074 |
| Table B | Multiple Model |
| Factor | HR | CI95 | p-value |
| CD3 (CT)* | 0.23 | 0.04–1.22 | 0.084 |
| Nodal positive RC | n.s. |
| CD3 (IM)* | n.i. |
| Nodal positive RC | 2.88 | 0.90–9.20 | 0.074 |
| CD8 (CT)* | n.i. |
| Nodal positive RC | 2.88 | 0.90–9.20 | 0.074 |
| CD8 (IM)* | n.i. |
| Nodal positive RC | 2.88 | 0.90–9.20 | 0.074 |