Germline Variants in Phosphodiesterase Genes and Genetic Predisposition to Pediatric Adrenocortical Tumors
Abstract
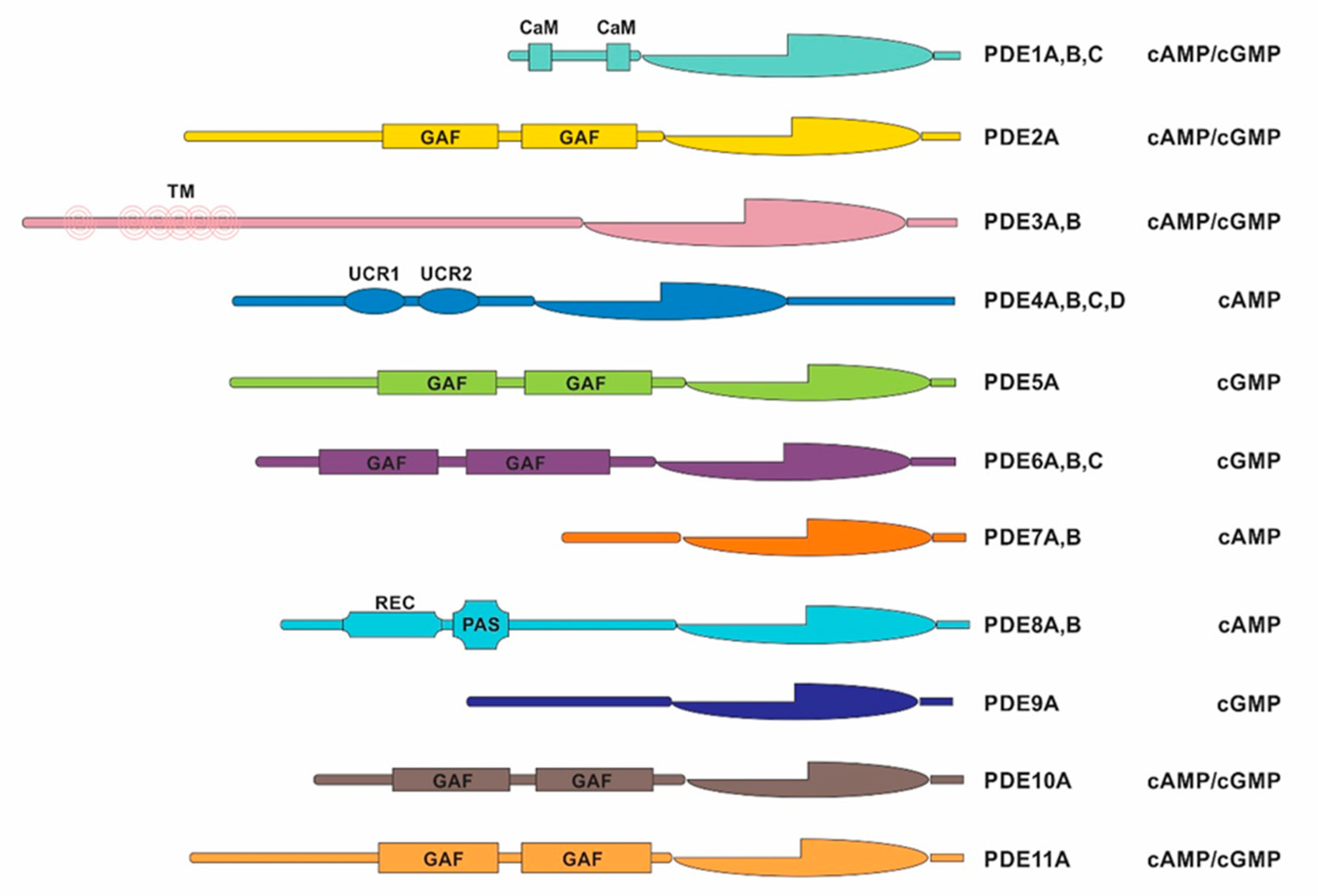
1. Introduction
2. Results
2.1. Discovery Cohort of Pediatric ACT Patients Harboring PDE Variants
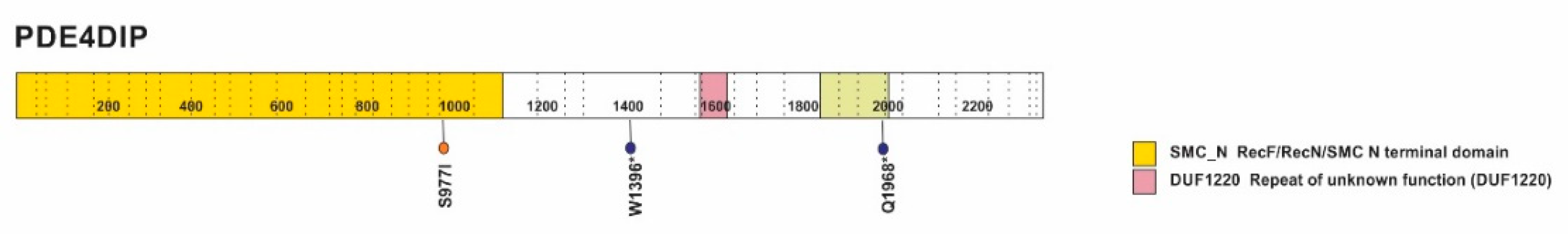
2.2. PDE Variants Identified in the Discovery Cohort
2.3. Transcriptome Profiling of PDEs in the Discovery Cohort
2.4. Germline PDE Variants Identified in Pediatric ACTs Associated with the Founder TP53 p.R337H Variant
3. Discussion
4. Materials and Methods
4.1. Phosphodiesterase Variants in the Discovery Cohort
4.2. Transcriptome Profiling
4.3. Whole Exome Sequencing of an Independent Cohort of Pediatric ACTs Harboring the Germline TP53 p.R337H Variant
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Azevedo, M.F.; Faucz, F.R.; Bimpaki, E.; Horvath, A.; Levy, I.; de Alexandre, R.B.; Ahmad, F.; Manganiello, V.; Stratakis, C.A. Clinical and molecular genetics of the phosphodiesterases (PDEs). Endocr. Rev. 2014, 35, 195–233. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.L.; Whelan, F.; Deloukas, P.; Whittaker, P.; Delgado, M.; Cantor, R.M.; McCann, S.M.; Licino, J. Phosphodiesterase genes are associated with susceptibility to major depression and antidepressant treatment response. Proc. Natl. Acad. Sci. USA 2006, 103, 15124–15129. [Google Scholar] [CrossRef] [PubMed]
- Francis, S.H.; Blount, M.A.; Corbin, J.D. Mammalian cyclic nucleotide phosphodiesterases: Molecular mechanisms and physiological functions. Physiol. Rev. 2011, 91, 651–690. [Google Scholar] [CrossRef] [PubMed]
- Baillie, G.S.; Tejeda, G.S.; Kelly, M.P. Therapeutic targeting of 3’,5’-cyclic nucleotide phosphodiesterases: Inhibition and beyond. Nat. Rev. Drug Discov. 2019, 18, 770–796. [Google Scholar] [CrossRef]
- Fajardo, A.M.; Piazza, G.A.; Tinsley, H.N. The Role of Cyclic Nucleotide Signaling Pathways in Cancer: Targets for Prevention and Treatment. Cancers 2014, 6, 436–458. [Google Scholar] [CrossRef]
- Lerner, A.; Epstein, P.M. Cyclic nucleotide phosphodiesterases as targets for treatment of haematological malignancies. Biochem. J. 2006, 393, 21–41. [Google Scholar] [CrossRef]
- Chawla, R.K.; Shlaer, S.M.; Lawson, D.H.; Murray, T.G.; Schmidt, F.; Shoji, M.; Nixon, D.W.; Richmond, A.; Rudman, D. Elevated plasma and urinary guanosine 3’:5’-monophosphate and increased production rate in patients with neoplastic diseases. Cancer Res. 1980, 40, 3915–3920. [Google Scholar]
- Pertuit, M.; Barlier, A.; Enjalbert, A.; Gérard, C. Signalling pathway alterations in pituitary adenomas: Involvement of Gsalpha, cAMP and mitogen-activated protein kinases. J. Neuroendocrinol. 2009, 21, 869–877. [Google Scholar] [CrossRef]
- DeRubertis, F.R.; Craven, P.A. Sequential alterations in the hepatic content and metabolism of cyclic AMP and cyclic GMP induced by DL-ethionine: Evidence for malignant transformation of liver with a sustained increase in cyclic AMP. Metabolism 1976, 25, 1611–1625. [Google Scholar] [CrossRef]
- Aleksijevic, A.; Lugnier, C.; Giron, C.; Mayer, S.; Stoclet, J.C.; Lang, J.M. Cyclic AMP and cyclic GMP phosphodiesterase activities in Hodgkin’s disease lymphocytes. Int. J. Immunopharmacol. 1987, 9, 525–531. [Google Scholar] [CrossRef]
- Zhang, L.; Murray, F.; Zahno, A.; Kanter, J.R.; Chou, D.; Suda, R.; Fenlon, M.; Rassenti, L.; Cottam, H.; Kipps, T.J.; et al. Cyclic nucleotide phosphodiesterase profiling reveals increased expression of phosphodiesterase 7B in chronic lymphocytic leukemia. Proc. Natl. Acad. Sci. USA 2008, 105, 19532–19537. [Google Scholar] [CrossRef] [PubMed]
- Cesarini, V.; Martini, M.; Vitiani, L.R.; Gravina, G.L.; DiAgostino, S.; Graziana, G.; D’Aessandris, Q.G.; Pallini, R.; Larocca, L.M.; Rossi, P.; et al. Type 5 phosphodiesterase regulates glioblastoma multiforme aggressiveness and clinical outcome. Oncotarget 2017, 8, 13223–13239. [Google Scholar] [CrossRef] [PubMed]
- McEwan, D.G.; Brunton, V.G.; Baillie, G.S.; Leslie, N.R.; Houslay, M.D.; Frame, M.C. Chemoresistant KM12C colon cancer cells are addicted to low cyclic AMP levels in a phosphodiesterase 4-regulated compartment via effects on phosphoinositide 3-kinase. Cancer Res. 2007, 67, 5248–5257. [Google Scholar] [CrossRef] [PubMed]
- Goldhoff, P.; Warrington, N.M.; Limbrick DDJr Hope, A.; Woerner, B.M.; Jackson, E.; Perry, A.; Piwnica-Worms, D.; Rubin, J.B. Targeted inhibition of cyclic AMP phosphodiesterase-4 promotes brain tumor regression. Clin. Cancer Res. 2008, 14, 7717–7725. [Google Scholar] [CrossRef] [PubMed]
- Vigone, G.; Shuhaibar, L.C.; Egbert, J.R.; Uliasz, T.F.; Movsesian, M.A.; Jaffe, L.A. Multiple cAMP Phosphodiesterases Act Together to Prevent Premature Oocyte Meiosis and Ovulation. Endocrinology 2018, 159, 2142–2152. [Google Scholar] [CrossRef] [PubMed]
- Drobnis, E.Z.; Nangia, A.K. Phosphodiesterase Inhibitors (PDE Inhibitors) and Male Reproduction. Adv. Exp. Med. Biol. 2017, 1034, 29–38. [Google Scholar] [CrossRef]
- Szarek, E.; Stratakis, C.A. Phosphodiesterases and adrenal Cushing in mice and humans. Horm. Metab. Res. 2014, 46, 863–868. [Google Scholar] [CrossRef]
- Rothenbuhler, A.; Horvath, A.; Libé, R.; Faucz, F.R.; Fratticci, A.; Raffin Sanson, M.L.; Vezzosi, D.; Azevedo, M.; Levy, I.; Almeida, M.Q.; et al. Identification of novel genetic variants in phosphodiesterase 8B (PDE8B), a cAMP-specific phosphodiesterase highly expressed in the adrenal cortex, in a cohort of patients with adrenal tumours. Clin. Endocrinol. 2012, 77, 195–199. [Google Scholar] [CrossRef]
- Libé, R.; Fratticci, A.; Coste, J.; Tissier, F.; Horvath, A.; Ragazzon, B.; Rene-Corail, F.; Groussin, L.; Bertagna, X.; Raffin-Sanson, M.L.; et al. Phosphodiesterase 11A (PDE11A) and genetic predisposition to adrenocortical tumors. Clin. Cancer Res. 2008, 14, 4016–4024. [Google Scholar] [CrossRef]
- Zheng, S.; Cherniack, A.D.; Dewal, N.; Moffitt, R.A.; Danilova, L.; Murray, B.A.; Lerario, A.M.; Else, T.; Knijnenburg, T.A.; Ciriello, G.; et al. Comprehensive Pan-Genomic Characterization of Adrenocortical Carcinoma. Cancer Cell 2016, 29, 723–736. [Google Scholar] [CrossRef]
- Juhlin, C.C.; Goh, G.; Healy, J.M.; Fonseca, A.L.; Scholl, U.I.; Stenman, A.; Kunstman, J.W.; Brown, T.C.; Overton, J.D.; Mane, S.M.; et al. Whole-exome Sequencing Characterizes the Landscape of Somatic Mutations and Copy Number Alterations in Adrenocortical Carcinoma. J. Clin. Endocrinol. Metab. 2015, 100, E493–E502. [Google Scholar] [CrossRef] [PubMed]
- Butt, E.; Beltman, J.; Becker, D.E.; Jensen, G.S.; Rybalkin, S.D.; Jastorff, B.; Beavo, J.A. Characterization of cyclic nucleotide phosphodiesterases with cyclic AMP analogs: Topology of the catalytic sites and comparison with other cyclic AMP-binding proteins. Mol. Pharmacol. 1995, 47, 340–347. [Google Scholar] [PubMed]
- Horvath, A.; Boikis, S.; Giatzakis, C.; Robinson-White, A.; Groussin, L.; Griffin, K.J.; Stein, E.; Levine, E.; Delimpasi, G.; Hsiao, H.P.; et al. A genome-wide scan identifies mutations in the gene encoding phosphodiesterase 11A4 (PDE11A) in individuals with adrenocortical hyperplasia. Nat. Genet. 2006, 38, 794–800. [Google Scholar] [CrossRef] [PubMed]
- Sato, Y.; Maekawa, S.; Ishii, R.; Sanada, M.; Morikawa, T.; Shiraishi, Y.; Yoshida, K.; Nagata, Y.; Sato-Otsubo, A.; Yoshizato, T.; et al. Recurrent somatic mutations underlie corticotropin-independent Cushing’s syndrome. Science 2014, 344, 917–920. [Google Scholar] [CrossRef] [PubMed]
- Wieneke, J.A.; Thompson, L.D.R.; Heffess, C.S. Adrenal Cortical Neoplasms in the Pediatric Population: A Clinicopathologic and Immunophenotypic Analysis of 83 Patients. Am. J. Surg. Pathol. 2003, 27, 867–881. [Google Scholar] [CrossRef]
- Pinto, E.M.; Chen, X.; Easton, J.; Finkelstein, D.; Liu, Z.; Pounds, S.; Rodriguez-Galindo, C.; Lund, T.C.; Mardis, E.R.; Wilson, R.K.; et al. Genomic landscape of paediatric adrenocortical tumours. Nat. Commun. 2015. [Google Scholar] [CrossRef]
- Pinto, E.M.; Rodriguez-Galindo, C.; Pounds, S.B.; Wang, L.; Clay, M.R.; Neale, G.; Garfinkle, E.A.R.; Lam, C.G.; Levy, C.F.; Pappo, A.S.; et al. Identification of Clinical and Biologic Correlates Associated With Outcome in Children With Adrenocortical Tumors Without Germline TP53 Mutations: A St Jude Adrenocortical Tumor Registry and Children’s Oncology Group Study. J. Clin. Oncol. 2017, 35, 3956–3963. [Google Scholar] [CrossRef]
- Wasserman, J.D.; Novokmet, A.; Eichler-Jonsson, C.; Ribeiro, R.C.; Rodriguez-Galingo, C.; Zambetti, G.P.; Malkin, D. Prevalence andFunctional Consequence of TP53 Mutations in Pediatric Adrenocortical Carcinoma: A Children’s Oncology Group Study. J. Clin. Oncol. 2015, 33, 602–609. [Google Scholar] [CrossRef]
- Zambetti, G.P. The p53 Mutation “Gradient Effect” and Its Clinical Implications. J. Cell Physiol. 2007, 213, 370–373. [Google Scholar] [CrossRef]
- Libe, R.; Horvath, A.; Vezzosi, D.; Fratticci, A.; Coste, J.; Perlemoine, K.; Ragazzon, B.; Guillaud-Bataille, M.; Groussin, L.; Clauser, E.; et al. Frequend Phosphodiesterase 11A Gene (PDE11A) Defects in Patients With Carney Complex (CNC) Caused by PRKAR1A Mutations: PDE11A May Contribute to Adrenal and Testicular Tumors in CNC as a Modifier of the Phenotype. J. Clin. Endocrinol. Metab. 2011, 96, E208–E214. [Google Scholar] [CrossRef]
- de Alexandre, R.B.; Horvath, A.D.; Szarek, E.; Manning, A.D.; Leal, L.F.; Kardauke, F.; Epstein, J.A.; Carraro, D.M.; Soares, F.A.; Apanasovich, T.V.; et al. Phosphodiesterase sequence variants may predispose to prostate cancer. Endocr. Relat. Cancer 2015, 22, 519–530. [Google Scholar] [CrossRef] [PubMed]
- Saloustros, E.; Salpea, P.; Starost, M.; Liu, S.; Faucz, F.R.; London, E.; Szarek, E.; Song, W.J.; Hussain, M.; Stratakis, C.A. Prkar1a Gene Knockout in the Pancreas Leads to Neuroendocrine Tumorigenesis. Endocr. Relat. Cancer 2017, 24, 31–40. [Google Scholar] [CrossRef]
- Wilkinson, K.; Velloso, E.R.P.; Lopes, L.F.; Lee, C.; Aster, J.C.; Shipp, M.A.; Aguiar, R.C.T. Cloning of the t(1;5)(q23;q33) in a myeloproliferative disorder associated with eosinophilia: Involvement of PDGFRB and response to imatinib. Blood 2003, 102, 4187–4190. [Google Scholar] [CrossRef] [PubMed]
- Gara, S.K.; Lack, J.; Zhang, L.; Harris, E.; Cam, M.; Electron, K. Metastatic adrenocortical carcinoma displays higher mutation rate and tumor heterogeneity than primary tumors. Nat. Commun. 2018. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, R.C.; Sandrini, F.; Figueiredo, B.; Zambetti, G.P.; Michalkiewicz, E.; Lafferty, A.R.; DeLacerda, L.; Rabin, M.; Cadwell, C.; Sampaio, G.; et al. An inherited p53 mutation that contributes in a tissue-specific manner to pediatric adrenal cortical carcinoma. Proc. Natl. Acad. Sci. USA 2001, 98, 9330–9335. [Google Scholar] [CrossRef] [PubMed]
- Latronico, A.C.; Pinto, E.M.; Domenice, S.; Fragoso, M.C.; Martin, R.M.; Zerbini, M.C.; Lucon, A.M.; Mendonca, B.B. An inherited mutation outside the highly conserved DNA-binding domain of the p53 tumor suppressor protein in children and adults with sporadic adrenocortical tumors. J. Clin. Endocrinol. Metab. 2001, 86, 4970–4973. [Google Scholar] [CrossRef]
- Pinto, E.M.; Billerbeck, A.E.; Villares, M.C.; Domenice, S.; Mendonca, B.B.; Latronico, A.C. Founder effect for the highly prevalent R337H mutation of tumor suppressor p53 in Brazilian patients with adrenocortical tumors. Arq. Bras. Endocrinol. Metabol. 2004, 48, 647–650. [Google Scholar] [CrossRef]
- Yang, Q.; Khoury, M.J.; Friedman, J.M.; Little, J.; Flanders, W.D. How many genes underlie the occurrence of common complex diseases in the population? Int. J. Epidemiol. 2005, 34, 1129–1137. [Google Scholar] [CrossRef]
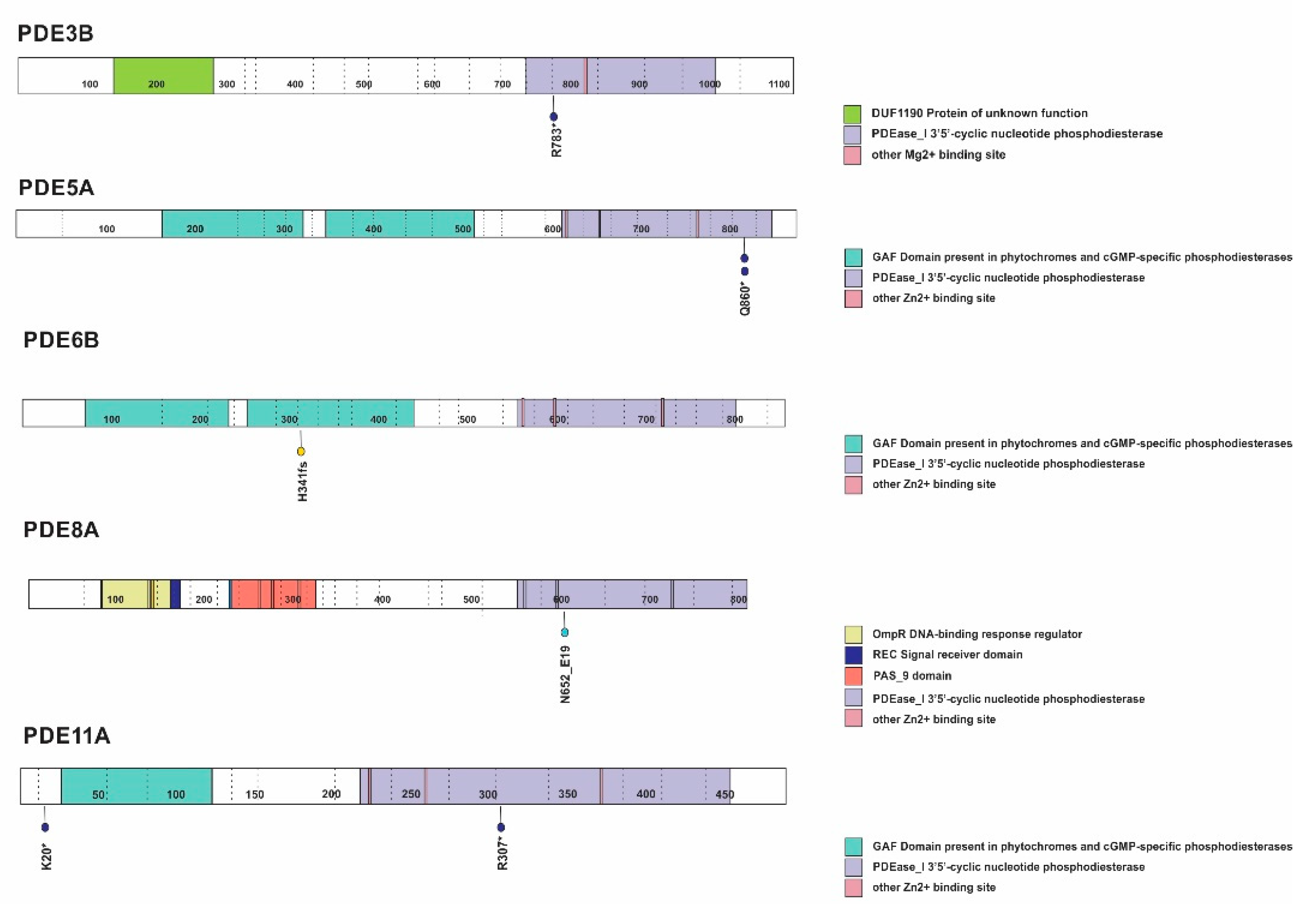

| Case | c-AMP Pathway/ Germline | c-AMP Pathway/ Somatic | TP53 status | Gender | Clinical Presentation | Histology | Age at diagnosis (months) | Tumor weight (g) | Stage | Survival Status |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | p.Q860*-PDE5A | WT | F | V | ACA | 59.8 | 20.5 | I | Alive | |
| 2 | p.Q860*-PDE5A | p.R337H | F | V | ACC | 38.0 | 6 | I | Alive | |
| 3 | p.R307*-PDE11A | p.S977I-PDE4DIP/p.R201H-GNAS | WT/UPD | F | A | Und | 140.6 | 388 | III | Alive |
| 4 | p.K20*-PDE11A | p.T125T | M | V | ACC | 103.0 | 500 | III | Alive | |
| 5 | p.R783*-PDE3B | WT | F | V | Und | 26.2 | 69 | I | Alive | |
| 6 | p.W1396*-PDE4DIP | p.R337H | M | V | ACC | 21.0 | Unk | I | Unk | |
| 7 | p.Q1968*-PDE4DIP | p.R337H | M | V+C | ACC | 24.4 | Unk | I | Died | |
| 8 | p.H341Qfs*23-PDE6B | p.R337H | F | V | ACC | 35.0 | 30 | I | Alive | |
| 9 | c.1953-4A>G -PDE8A | WT/UPD | F | C | ACA | 17.0 | 120 | III | Alive | |
| 10 | PDE4-ERRB4 | p.R273C | F | NF | ACC | 24.0 | Unk | IV | Died | |
| 11 | p.R201C-GNAS | WT | F | V | Und | 83.0 | 255.7 | II | Alive |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pinto, E.M.; Faucz, F.R.; Paza, L.Z.; Wu, G.; Fernandes, E.S.; Bertherat, J.; Stratakis, C.A.; Lalli, E.; Ribeiro, R.C.; Rodriguez-Galindo, C.; et al. Germline Variants in Phosphodiesterase Genes and Genetic Predisposition to Pediatric Adrenocortical Tumors. Cancers 2020, 12, 506. https://doi.org/10.3390/cancers12020506
Pinto EM, Faucz FR, Paza LZ, Wu G, Fernandes ES, Bertherat J, Stratakis CA, Lalli E, Ribeiro RC, Rodriguez-Galindo C, et al. Germline Variants in Phosphodiesterase Genes and Genetic Predisposition to Pediatric Adrenocortical Tumors. Cancers. 2020; 12(2):506. https://doi.org/10.3390/cancers12020506
Chicago/Turabian StylePinto, Emilia Modolo, Fabio R. Faucz, Luana Z. Paza, Gang Wu, Elizabeth S. Fernandes, Jerome Bertherat, Constantine A. Stratakis, Enzo Lalli, Raul C. Ribeiro, Carlos Rodriguez-Galindo, and et al. 2020. "Germline Variants in Phosphodiesterase Genes and Genetic Predisposition to Pediatric Adrenocortical Tumors" Cancers 12, no. 2: 506. https://doi.org/10.3390/cancers12020506
APA StylePinto, E. M., Faucz, F. R., Paza, L. Z., Wu, G., Fernandes, E. S., Bertherat, J., Stratakis, C. A., Lalli, E., Ribeiro, R. C., Rodriguez-Galindo, C., Figueiredo, B. C., & Zambetti, G. P. (2020). Germline Variants in Phosphodiesterase Genes and Genetic Predisposition to Pediatric Adrenocortical Tumors. Cancers, 12(2), 506. https://doi.org/10.3390/cancers12020506







