Donor Heme Oxygenase-1 Promoter Gene Polymorphism Predicts Survival after Unrelated Bone Marrow Transplantation for High-Risk Patients
Abstract
1. Introduction
2. Results
2.1. The Frequencies of HO-1 Genotypes
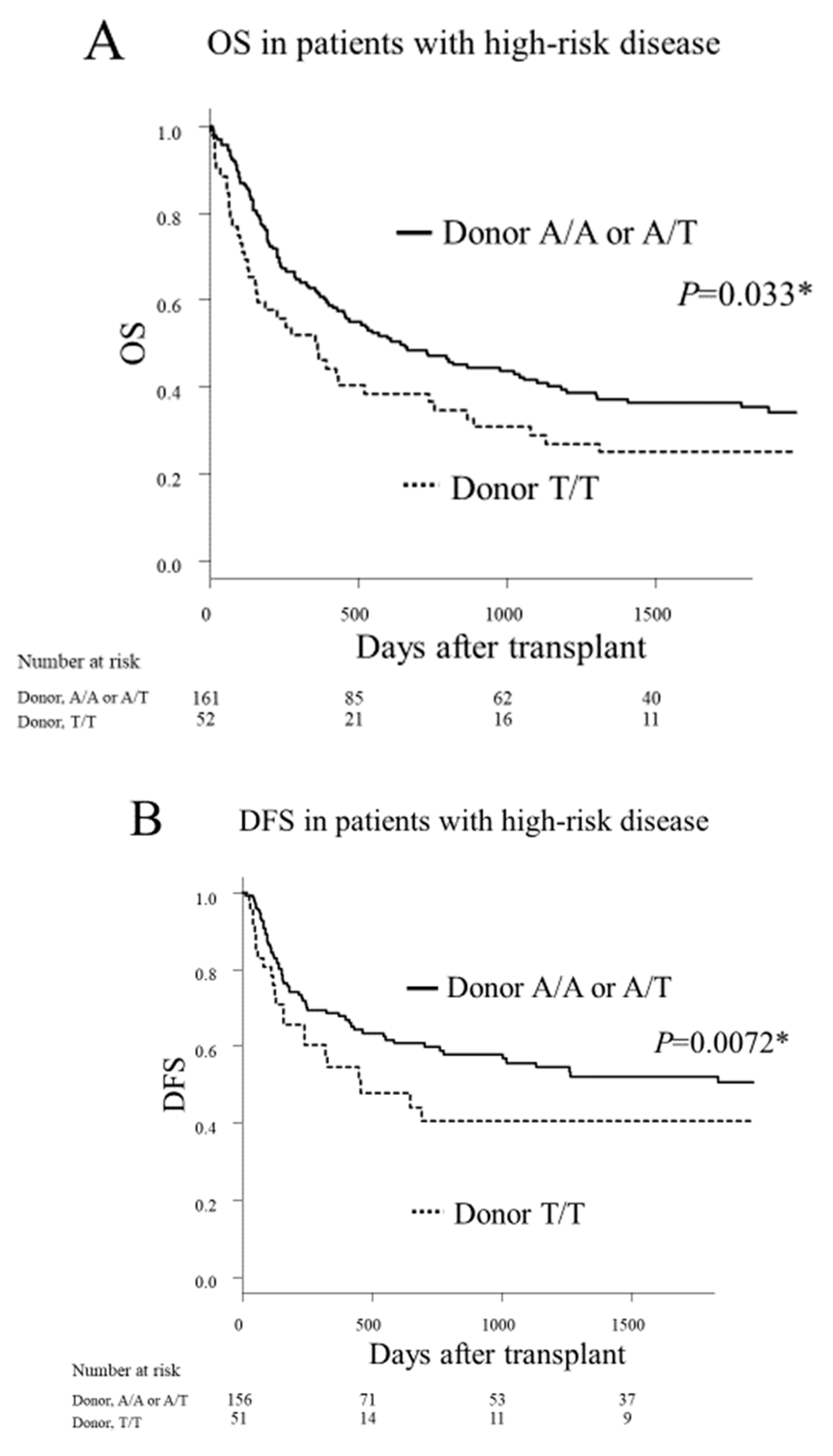
2.2. Transplant Outcomes According to the HO-1 Genotype
2.3. Multivariate Analysis
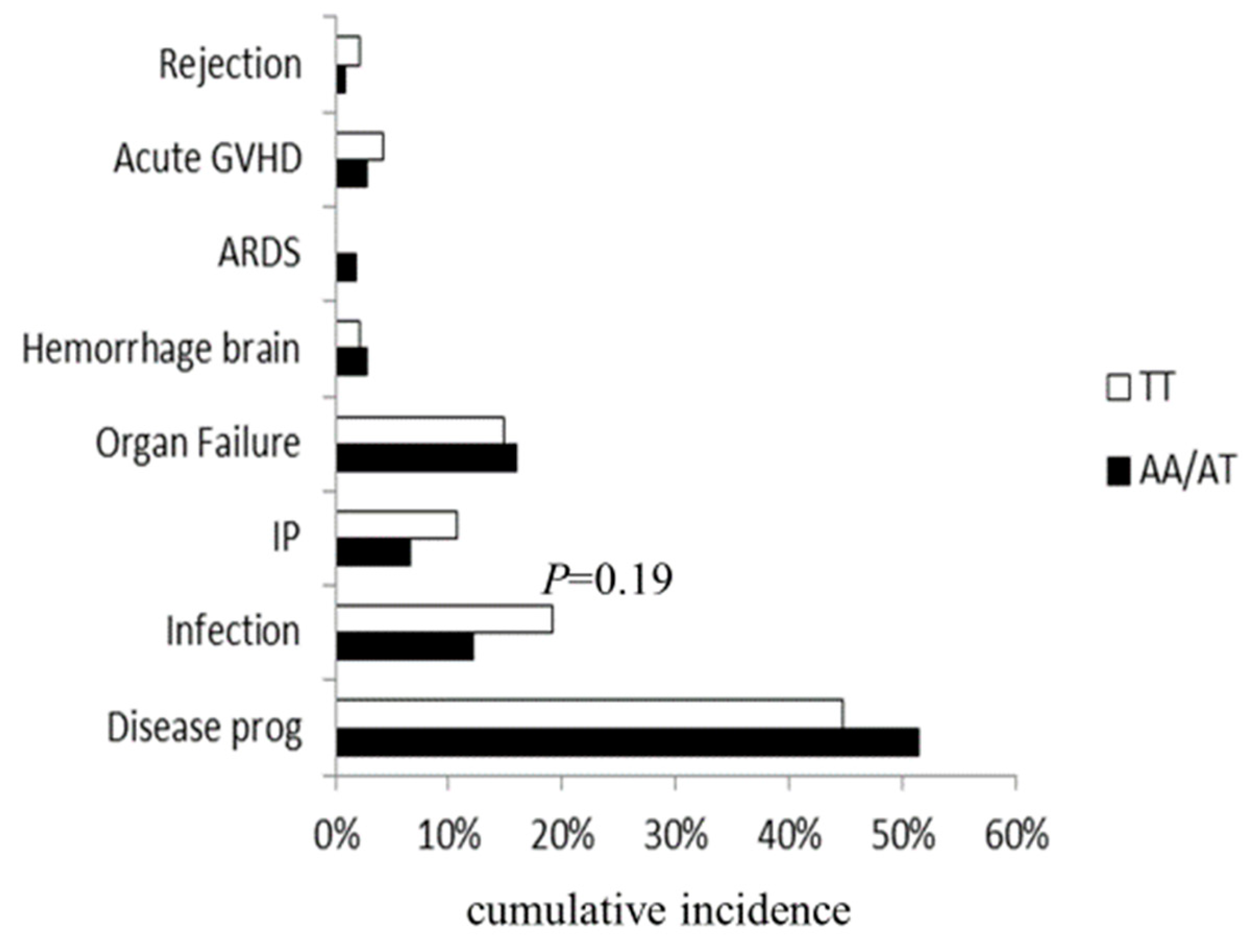
2.4. Main Causes of Death
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. HO-1 Genotyping
4.3. Data Management and Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Biedermann, B.C.; Sahner, S.; Gregor, M.; Tsakiris, D.A.; Jeanneret, C.; Pober, J.S.; Gratwohl, A. Endothelial injury mediated by cytotoxic T lymphocytes and loss of microvessels in chronic graft versus host disease. Lancet 2002, 359, 2078–2083. [Google Scholar] [CrossRef]
- Carreras, E.; Diaz-Ricart, M. The role of the endothelium in the short-term complications of hematopoietic SCT. Bone Marrow Transplant 2011, 46, 1495–1502. [Google Scholar] [CrossRef] [PubMed]
- Cooke, K.R.; Jannin, A.; Ho, V. The contribution of endothelial activation and injury to end-organ toxicity following allogeneic hematopoietic stem cell transplantation. Biol. Blood Marrow Transplant. J. Am. Soc. Blood Marrow Transplant. 2008, 14, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Pagliuca, S.; Michonneau, D.; Sicre de Fontbrune, F.; Sutra Del Galy, A.; Xhaard, A.; Robin, M.; Peffault de Latour, R.; Socie, G. Allogeneic reactivity-mediated endothelial cell complications after HSCT: A plea for consensual definitions. Blood Adv. 2019, 3, 2424–2435. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues-Diez, R.; Gonzalez-Guerrero, C.; Ocana-Salceda, C.; Rodrigues-Diez, R.R.; Egido, J.; Ortiz, A.; Ruiz-Ortega, M.; Ramos, A.M. Calcineurin inhibitors cyclosporine A and tacrolimus induce vascular inflammation and endothelial activation through TLR4 signaling. Sci. Rep. 2016, 6, e27915. [Google Scholar] [CrossRef]
- Schmid, P.M.; Bouazzaoui, A.; Doser, K.; Schmid, K.; Hoffmann, P.; Schroeder, J.A.; Riegger, G.A.; Holler, E.; Endemann, D.H. Endothelial dysfunction and altered mechanical and structural properties of resistance arteries in a murine model of graft-versus-host disease. Biol. Blood Marrow Transplant. J. Am. Soc. Blood Marrow Transplant. 2014, 20, 1493–1500. [Google Scholar] [CrossRef]
- Maines, M.D. Heme oxygenase: Function, multiplicity, regulatory mechanisms, and clinical applications. FASEB J. 1988, 2, 2557–2568. [Google Scholar] [CrossRef]
- Bauer, I.; Raupach, A. The Role of Heme Oxygenase-1 in Remote Ischemic and Anesthetic Organ Conditioning. Antioxidants 2019, 8, 403. [Google Scholar] [CrossRef]
- Willis, D.; Moore, A.R.; Frederick, R.; Willoughby, D.A. Heme oxygenase: A novel target for the modulation of the inflammatory response. Nat. Med. 1996, 2, 87–90. [Google Scholar] [CrossRef]
- Yachie, A.; Niida, Y.; Wada, T.; Igarashi, N.; Kaneda, H.; Toma, T.; Ohta, K.; Kasahara, Y.; Koizumi, S. Oxidative stress causes enhanced endothelial cell injury in human heme oxygenase-1 deficiency. J. Clin. Investig. 1999, 103, 129–135. [Google Scholar] [CrossRef]
- Maruyama, K.; Morishita, E.; Yuno, T.; Sekiya, A.; Asakura, H.; Ohtake, S.; Yachie, A. Carbon monoxide (CO)-releasing molecule-derived CO regulates tissue factor and plasminogen activator inhibitor type 1 in human endothelial cells. Thromb. Res. 2012, 130, 188–193. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Otterbein, L.E.; Bach, F.H.; Alam, J.; Soares, M.; Lu, H.T.; Wysk, M.; Davis, R.J.; Flavell, R.A.; Choi, A.M. Carbon monoxide has anti-inflammatory effects involving the mitogen-activated protein kinase pathway. Nat. Med. 2000, 6, e422. [Google Scholar] [CrossRef] [PubMed]
- Brouard, S.; Otterbein, L.E.; Anrather, J.; Tobiasch, E.; Bach, F.H.; Choi, A.M.; Soares, M.P. Carbon monoxide generated by heme oxygenase 1 suppresses endothelial cell apoptosis. J. Exp. Med. 2000, 192, 1015–1026. [Google Scholar] [CrossRef] [PubMed]
- Pan, T.; Qi, J.; You, T.; Han, S.; Yang, L.; Miao, W.; Wu, D.; Ruan, C.; Zhu, L.; Han, Y. Circulating Heme Oxygenase-1 and Complement Activation in Transplant-Associated Thrombotic Microangiopathy. Biol. Blood Marrow Transplant. J. Am. Soc. Blood Marrow Transplant. 2019, 25, 1486–1491. [Google Scholar] [CrossRef] [PubMed]
- Piantadosi, C.A.; Withers, C.M.; Bartz, R.R.; MacGarvey, N.C.; Fu, P.; Sweeney, T.E.; Welty-Wolf, K.E.; Suliman, H.B. Heme oxygenase-1 couples activation of mitochondrial biogenesis to anti-inflammatory cytokine expression. J. Biol. Chem. 2011, 286, 16374–16385. [Google Scholar] [CrossRef]
- Stocker, R.; Yamamoto, Y.; McDonagh, A.F.; Glazer, A.N.; Ames, B.N. Bilirubin is an antioxidant of possible physiological importance. Science 1987, 235, 1043–1046. [Google Scholar] [CrossRef]
- BioGPS. HO-1 (HMOX1) Gene. Available online: http://ds.biogps.org/?dataset=GSE1133&gene=3162 (accessed on 17 October 2019).
- Ono, K.; Goto, Y.; Takagi, S.; Baba, S.; Tago, N.; Nonogi, H.; Iwai, N. A promoter variant of the heme oxygenase-1 gene may reduce the incidence of ischemic heart disease in Japanese. Atherosclerosis 2004, 173, 315–319. [Google Scholar] [CrossRef]
- Buis, C.I.; van der Steege, G.; Visser, D.S.; Nolte, I.M.; Hepkema, B.G.; Nijsten, M.; Slooff, M.J.; Porte, R.J. Heme oxygenase-1 genotype of the donor is associated with graft survival after liver transplantation. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transpl. Surg. 2008, 8, 377–385. [Google Scholar] [CrossRef]
- Espinoza, J.L.; Takami, A.; Onizuka, M.; Sao, H.; Akiyama, H.; Miyamura, K.; Okamoto, S.; Inoue, M.; Kanda, Y.; Ohtake, S.; et al. NKG2D gene polymorphism has a significant impact on transplant outcomes after HLA-fully-matched unrelated bone marrow transplantation for standard risk hematologic malignancies. Haematologica 2009, 94, 1427–1434. [Google Scholar] [CrossRef]
- Uchino, K.; Mizuno, S.; Sato-Otsubo, A.; Nannya, Y.; Mizutani, M.; Horio, T.; Hanamura, I.; Espinoza, J.L.; Onizuka, M.; Kashiwase, K.; et al. Toll-like receptor genetic variations in bone marrow transplantation. Oncotarget 2017, 8, 45670–45686. [Google Scholar] [CrossRef]
- Nomoto, H.; Takami, A.; Espinoza, J.L.; Onizuka, M.; Kashiwase, K.; Morishima, Y.; Fukuda, T.; Kodera, Y.; Doki, N.; Miyamura, K.; et al. Recipient ADAMTS13 Single-Nucleotide Polymorphism Predicts Relapse after Unrelated Bone Marrow Transplantation for Hematologic Malignancy. Int. J. Mol. Sci. 2019, 20, 214. [Google Scholar] [CrossRef] [PubMed]
- Horio, T.; Mizuno, S.; Uchino, K.; Mizutani, M.; Hanamura, I.; Espinoza, J.L.; Onizuka, M.; Kashiwase, K.; Morishima, Y.; Fukuda, T.; et al. The recipient CCR5 variation predicts survival outcomes after bone marrow transplantation. Transpl. Immunol. 2017, 42, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Uchino, K.; Mizuno, S.; Mizutani, M.; Horio, T.; Hanamura, I.; Espinoza, J.L.; Matsuo, K.; Onizuka, M.; Kashiwase, K.; Morishima, Y.; et al. Toll-like receptor 1 variation increases the risk of transplant-related mortality in hematologic malignancies. Transpl. Immunol. 2016, 38, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Nomoto, H.; Takami, A.; Espinoza, J.L.; Matsuo, K.; Mizuno, S.; Onizuka, M.; Kashiwase, K.; Morishima, Y.; Fukuda, T.; Kodera, Y.; et al. A donor thrombomodulin gene variation predicts graft-versus-host disease development and mortality after bone marrow transplantation. Int. J. Hematol. 2015, 102, 460–470. [Google Scholar] [CrossRef]
- Takami, A. Role of non-HLA gene polymorphisms in graft-versus-host disease. Int. J. Hematol. 2013, 98, 309–318. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Arai, Y.; Kondo, T.; Shigematsu, A.; Tanaka, J.; Ohashi, K.; Fukuda, T.; Kawakita, T.; Mori, T.; Hoshino, T.; Onizuka, M.; et al. Increased non-relapse mortality due to high-dose cytarabine plus CY/TBI in BMT/PBSCT for acute lymphoblastic leukaemia in adults. Br. J. Haematol. 2017, 178, 106–111. [Google Scholar] [CrossRef]
- Kernan, N.A.; Bartsch, G.; Ash, R.C.; Beatty, P.G.; Champlin, R.; Filipovich, A.; Gajewski, J.; Hansen, J.A.; Henslee-Downey, J.; McCullough, J.; et al. Analysis of 462 transplantations from unrelated donors facilitated by the National Marrow Donor Program. N. Engl. J. Med. 1993, 328, 593–602. [Google Scholar] [CrossRef]
- Shimoni, A.; Labopin, M.; Savani, B.; Byrne, M.; Volin, L.; Finke, J.; Niederwieser, D.; Ehninger, G.; Blaise, D.; Beelen, D.; et al. Comparable Long-Term Outcome after Allogeneic Stem Cell Transplantation from Sibling and Matched Unrelated Donors in Patients with Acute Myeloid Leukemia Older Than 50 Years: A Report on Behalf of the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Biol. Blood Marrow Transplant. J. Am. Soc. Blood Marrow Transplant. 2019, 25, 2251–2260. [Google Scholar] [CrossRef]
- HapMap Data of Japanese in rs2071746. Available online: https://www.ncbi.nlm.nih.gov/projects/SNP/snp_ss.cgi?ss=ss8295263 (accessed on 26 January 2020).
- Kovtunovych, G.; Ghosh, M.C.; Ollivierre, W.; Weitzel, R.P.; Eckhaus, M.A.; Tisdale, J.F.; Yachie, A.; Rouault, T.A. Wild-type macrophages reverse disease in heme oxygenase 1-deficient mice. Blood 2014, 124, 1522–1530. [Google Scholar] [CrossRef]
- Calay, D.; Mason, J.C. The multifunctional role and therapeutic potential of HO-1 in the vascular endothelium. Antioxid. Redox Signal. 2014, 20, 1789–1809. [Google Scholar] [CrossRef]
- Gerbitz, A.; Ewing, P.; Wilke, A.; Schubert, T.; Eissner, G.; Dietl, B.; Andreesen, R.; Cooke, K.R.; Holler, E. Induction of heme oxygenase-1 before conditioning results in improved survival and reduced graft-versus-host disease after experimental allogeneic bone marrow transplantation. Biol. Blood Marrow Transplant. J. Am. Soc. Blood Marrow Transplant. 2004, 10, 461–472. [Google Scholar] [CrossRef] [PubMed]
- Askenazi, D.J.; Halloran, B.; Patil, N.; Keeling, S.; Saeidi, B.; Koralkar, R.; Ambalavanan, N. Genetic polymorphisms of heme-oxygenase 1 (HO-1) may impact on acute kidney injury, bronchopulmonary dysplasia, and mortality in premature infants. Pediatric Res. 2015, 77, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Nitti, M.; Piras, S.; Marinari, U.M.; Moretta, L.; Pronzato, M.A.; Furfaro, A.L. HO-1 Induction in Cancer Progression: A Matter of Cell Adaptation. Antioxidants 2017, 6, 29. [Google Scholar] [CrossRef] [PubMed]
- Salerno, L.; Romeo, G.; Modica, M.N.; Amata, E.; Sorrenti, V.; Barbagallo, I.; Pittala, V. Heme oxygenase-1: A new druggable target in the management of chronic and acute myeloid leukemia. Eur. J. Med. Chem. 2017, 142, 163–178. [Google Scholar] [CrossRef] [PubMed]
- Wei, S.; Wang, Y.; Chai, Q.; Fang, Q.; Zhang, Y.; Lu, Y.; Wang, J. Over-expression of heme oxygenase-1 in peripheral blood predicts the progression and relapse risk of chronic myeloid leukemia. Chin. Med. J. 2014, 127, 2795–2801. [Google Scholar]
- Bernasconi, P.; Borsani, O. Immune Escape after Hematopoietic Stem Cell Transplantation (HSCT): From Mechanisms to Novel Therapies. Cancers 2019, 12, 69. [Google Scholar] [CrossRef]
- Kollgaard, T.; Kornblit, B.; Petersen, J.; Klausen, T.W.; Mortensen, B.K.; Braendstrup, P.; Sengelov, H.; Hogdall, E.; Muller, K.; Vindelov, L.; et al. (GT)n Repeat Polymorphism in Heme Oxygenase-1 (HO-1) Correlates with Clinical Outcome after Myeloablative or Nonmyeloablative Allogeneic Hematopoietic Cell Transplantation. PLoS ONE 2016, 11, e0168210. [Google Scholar] [CrossRef]
- Narita, M.; Hatano, E.; Ikai, I.; Miyagawa-Hayashino, A.; Yanagida, A.; Nagata, H.; Asechi, H.; Taura, K.; Uemoto, S. A phosphodiesterase III inhibitor protects rat liver from sinusoidal obstruction syndrome through heme oxygenase-1 induction. Ann. Surg. 2009, 249, 806–813. [Google Scholar] [CrossRef]
- Yu, M.; Wang, J.; Fang, Q.; Liu, P.; Chen, S.; Zhe, N.; Lin, X.; Zhang, Y.; Zhao, J.; Zhou, Z. High expression of heme oxygenase-1 in target organs may attenuate acute graft-versus-host disease through regulation of immune balance of TH17/Treg. Transpl. Immunol. 2016, 37, 10–17. [Google Scholar] [CrossRef]
- Yakushijin, K.; Atsuta, Y.; Doki, N.; Yokota, A.; Kanamori, H.; Miyamoto, T.; Ohwada, C.; Miyamura, K.; Nawa, Y.; Kurokawa, M.; et al. Sinusoidal obstruction syndrome after allogeneic hematopoietic stem cell transplantation: Incidence, risk factors and outcomes. Bone Marrow Transplant. 2016, 51, 403–409. [Google Scholar] [CrossRef]
- Shimoni, A.; Yeshurun, M.; Hardan, I.; Avigdor, A.; Ben-Bassat, I.; Nagler, A. Thrombotic microangiopathy after allogeneic stem cell transplantation in the era of reduced-intensity conditioning: The incidence is not reduced. Biol. Blood Marrow Transplant. J. Am. Soc. Blood Marrow Transplant. 2004, 10, 484–493. [Google Scholar] [CrossRef] [PubMed]
- Tatekawa, S.; Kohno, A.; Ozeki, K.; Watamoto, K.; Ueda, N.; Yamaguchi, Y.; Kobayashi, T.; Yokota, I.; Teramukai, S.; Taniwaki, M.; et al. A Novel Diagnostic and Prognostic Biomarker Panel for Endothelial Cell Damage-Related Complications in Allogeneic Transplantation. Biol. Blood Marrow Transplant. J. Am. Soc. Blood Marrow Transplant. 2016, 22, 1573–1581. [Google Scholar] [CrossRef] [PubMed]
- Kawase, T.; Morishima, Y.; Matsuo, K.; Kashiwase, K.; Inoko, H.; Saji, H.; Kato, S.; Juji, T.; Kodera, Y.; Sasazuki, T.; et al. High-risk HLA allele mismatch combinations responsible for severe acute graft-versus-host disease and implication for its molecular mechanism. Blood 2007, 110, 2235–2241. [Google Scholar] [CrossRef]
- Sasazuki, T.; Juji, T.; Morishima, Y.; Kinukawa, N.; Kashiwabara, H.; Inoko, H.; Yoshida, T.; Kimura, A.; Akaza, T.; Kamikawaji, N.; et al. Effect of matching of class I HLA alleles on clinical outcome after transplantation of hematopoietic stem cells from an unrelated donor. Japan Marrow Donor Program. N. Engl. J. Med. 1998, 339, 1177–1185. [Google Scholar] [CrossRef] [PubMed]
- Morishima, Y.; Yabe, T.; Matsuo, K.; Kashiwase, K.; Inoko, H.; Saji, H.; Yamamoto, K.; Maruya, E.; Akatsuka, Y.; Onizuka, M.; et al. Effects of HLA allele and killer immunoglobulin-like receptor ligand matching on clinical outcome in leukemia patients undergoing transplantation with T-cell-replete marrow from an unrelated donor. Biol. Blood Marrow Transplant. J. Am. Soc. Blood Marrow Transplant. 2007, 13, 315–328. [Google Scholar] [CrossRef]
- Atsuta, Y. Introduction of Transplant Registry Unified Management Program 2 (TRUMP2): Scripts for TRUMP data analyses, part I (variables other than HLA-related data). Int. J. Hematol. 2016, 103, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Kanda, J. Scripts for TRUMP data analyses. Part II (HLA-related data): Statistical analyses specific for hematopoietic stem cell transplantation. Int. J. Hematol. 2016, 103, 11–19. [Google Scholar] [CrossRef]
- Przepiorka, D.; Weisdorf, D.; Martin, P.; Klingemann, H.G.; Beatty, P.; Hows, J.; Thomas, E.D. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant. 1995, 15, 825–828. [Google Scholar]
- Shulman, H.M.; Sullivan, K.M.; Weiden, P.L.; McDonald, G.B.; Striker, G.E.; Sale, G.E.; Hackman, R.; Tsoi, M.S.; Storb, R.; Thomas, E.D. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am. J. Med. 1980, 69, 204–217. [Google Scholar] [CrossRef]
- Filipovich, A.H.; Weisdorf, D.; Pavletic, S.; Socie, G.; Wingard, J.R.; Lee, S.J.; Martin, P.; Chien, J.; Przepiorka, D.; Couriel, D.; et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol. Blood Marrow Transplant. J. Am. Soc. Blood Marrow Transplant. 2005, 11, 945–956. [Google Scholar] [CrossRef]
- Rowlings, P.A.; Przepiorka, D.; Klein, J.P.; Gale, R.P.; Passweg, J.R.; Henslee-Downey, P.J.; Cahn, J.Y.; Calderwood, S.; Gratwohl, A.; Socie, G.; et al. IBMTR Severity Index for grading acute graft-versus-host disease: Retrospective comparison with Glucksberg grade. Br. J. Haematol. 1997, 97, 855–864. [Google Scholar] [CrossRef] [PubMed]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Gooley, T.A.; Leisenring, W.; Crowley, J.; Storer, B.E. Estimation of failure probabilities in the presence of competing risks: New representations of old estimators. Stat. Med. 1999, 18, 695–706. [Google Scholar] [CrossRef]
- Scrucca, L.; Santucci, A.; Aversa, F. Competing risk analysis using R: An easy guide for clinicians. Bone Marrow Transplant. 2007, 40, 381–387. [Google Scholar] [CrossRef]
- Giralt, S.; Ballen, K.; Rizzo, D.; Bacigalupo, A.; Horowitz, M.; Pasquini, M.; Sandmaier, B. Reduced-intensity conditioning regimen workshop: Defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol. Blood Marrow Transplant. J. Am. Soc. Blood Marrow Transplant. 2009, 15, 367–369. [Google Scholar] [CrossRef]
- Kim, D.H.; Jung, H.D.; Lee, N.Y.; Sohn, S.K. Single nucleotide polymorphism of CC chemokine ligand 5 promoter gene in recipients may predict the risk of chronic graft-versus-host disease and its severity after allogeneic transplantation. Transplantation 2007, 84, 917–925. [Google Scholar] [CrossRef]
| Variable | All | High-Risk | Standard-Risk | |
| Value | Value | Value | p | |
| Number of cases | 593 | 232 | 361 | |
| Recipient age, years, median (range) | 33 (1–67) | 34 (1–67) | 34 (1–65) | |
| Donor age, years, median (range) | 34 (20–57) | 34 (21–50) | 34 (20–57) | |
| Year of HSCT, median (range) | 2000 (1993–2007) | 2000 (1993–2007) | 2000 (1993–2007) | |
| Recipient HO-1 genotype, n (%) | 0.03 | |||
| A/A | 125 (21) | 40 (17) | 85 (24) | |
| A/T | 306 (52) | 135 (58) | 171 (47) | |
| T/T | 162 (27) | 57 (25) | 105 (29) | |
| Donor HO-1 genotype, n (%) | 0.96 | |||
| A/A | 134 (23) | 51 (22) | 83 (23) | |
| A/T | 308 (52) | 122 (53) | 186 (52) | |
| T/T | 151 (25) | 59 (25) | 92 (25) | |
| Recipient sex, n (%) | 0.55 | |||
| Male | 352 (59) | 134 (58) | 218 (60) | |
| Female | 241 (41) | 98 (42) | 143 (40) | |
| Donor sex, n (%) | 0.43 | |||
| Male | 374 (63) | 142 (61) | 232 (64) | |
| Female | 218 (37) | 90 (39) | 128 (36) | |
| Recipient/Donor sex match, n (%) | 0.54 | |||
| Sex-matched | 387 (65) | 158 (68) | 229 (64) | |
| Female/Male | 114 (19) | 41 (18) | 73 (20) | |
| Male/Female | 92 (16) | 33 (14) | 59 (16) | |
| Disease, n (%) | 0.01 | |||
| AML | 197 (33) | 112 (48) | 85 (24) | |
| ALL | 145 (24) | 72 (31) | 73 (20) | |
| MDS | 82 (14) | 0 (0) | 82 (23) | |
| ML | 64 (11) | 29 (13) | 35 (9) | |
| CML | 101 (17) | 16 (7) | 85 (24) | |
| MM | 4 (1) | 3 (1) | 1 (0) | |
| ABO matching, n (%) | 0.97 | |||
| ABO-matched | 359 (61) | 137 (59) | 222 (62) | |
| Major mismatch | 115 (19) | 46 (20) | 69 (19) | |
| Minor mismatch | 95 (16) | 40 (17) | 55 (15) | |
| Bidirectional | 16 (3) | 6 (3) | 10 (3) | |
| Missing | 8 (1) | 3 (1) | 5 (1) | |
| Conditioning regimen, n (%) | 0.86 | |||
| Myeloablative | 517 (87) | 204 (88) | 313 (87) | |
| Reduced intensity | 69 (12) | 26 (11) | 43 (12) | |
| Missing | 7 (1) | 2 (1) | 5 (1) | |
| Pretransplantation CMV serostatus, n (%) | 0.23 | |||
| CMV-positive recipient | 373 (63) | 142 (61) | 231 (64) | |
| CMV-negative recipient | 102 (17) | 36 (16) | 66 (18) | |
| Missing | 118 (20) | 54 (23) | 64 (18) | |
| TNC, ×108/kg, median (range) | 7.7 (0.1–259) | 7.7 (0.1–79.1) | 7.7 (0.6–259) |
| Variable | OS | DFS | TRM | Relapse | ||||||||
| HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | |
| High-risk disease | ||||||||||||
| Donor HO-1 genotype, A/T or A/A vs. T/T | 0.72 | 0.50–1.04 | 0.08 | 0.64 | 0.44–0.93 | 0.02 | 0.66 | 0.36–1.19 | 0.16 | 0.83 | 0.51–1.35 | 0.44 |
| Recipient HO-1 genotype, A/T or A/A vs. T/T | 0.91 | 0.62–1.32 | 0.61 | 0.99 | 0.68–1.45 | 0.98 | 1.03 | 0.57–1.85 | 0.92 | 0.99 | 0.60–1.64 | 0.98 |
| Recipient age | 0.99 | 0.97-0.99 | 0.004 | 0.99 | 0.98–1.00 | 0.02 | 0.98 | 0.96–0.99 | 0.006 | |||
| Standard-risk disease | ||||||||||||
| Donor HO-1 genotype, A/T or A/A vs. T/T | 1.05 | 0.71–1.54 | 0.80 | 0.91 | 0.56–1.47 | 0.70 | 1.04 | 0.59–1.82 | 0.89 | 0.71 | 0.40–1.22 | 0.20 |
| Recipient HO-1 genotype, A/T or A/A vs. T/T | 1.39 | 0.93–2.08 | 0.10 | 1.30 | 0.79–2.17 | 0.28 | 1.15 | 0.66–2.00 | 0.62 | 1.41 | 0.76–2.63 | 0.28 |
| Recipient age | 0.97 | 0.96–0.98 | <0.001 | 1.00 | 0.97–1.01 | 0.24 | 0.96 | 0.94–0.98 | 0.11 | 0.91 | 0.56–1.47 | 0.70 |
| Donor age | 0.97 | 0.94–1.01 | 0.11 | 1.33 | 0.80–2.22 | 0.27 | ||||||
| CMV-positive recipient | 1.22 | 0.77–1.92 | 0.39 | 0.58 | 0.36–0.94 | 0.03 | 0.47 | 0.26–0.82 | 0.008 | |||
| ABO major mismatch | 1.04 | 0.54–200 | 0.90 | |||||||||
| ABO minor mismatch | 0.59 | 0.39–0.88 | 0.01 | 0.50 | 0.28–0.89 | 0.02 | ||||||
| ABO bidirectional | 13513.5 | 5555.6–33333.3 | <0.001 | |||||||||
| Male donor/female recipient | 1.00 | 0.58–1.75 | 0.99 | |||||||||
| Female donor/male recipient | 2.27 | 1.05–5.00 | 0.04 | 2.22 | 1.03–4.76 | 0.04 |
| Variable | Grades 2–4 acute GVHD | Grades 3–4 acute GVHD | Chronic GVHD | ||||||
| HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | |
| High-risk disease | |||||||||
| Donor HO-1 genotype, A/T or A/A vs. T/T | 1.10 | 0.61–1.96 | 0.76 | 1.03 | 0.41–2.78 | 0.88 | 0.91 | 0.51–1.59 | 0.72 |
| Recipient HO-1 genotype, A/T or A/A vs. T/T | 1.09 | 0.62–1.92 | 0.76 | 1.00 | 0.40–2.50 | 1.00 | 0.63 | 0.37–1.08 | 0.09 |
| Recipient age | |||||||||
| Donor age | |||||||||
| Conditioning regimen, MAC vs. RIC | 3.03 | 0.94–10.0 | 0.06 | ||||||
| TNC | 0.99 | 0.97–1.01 | 0.23 | ||||||
| Year of HSCT | 0.59 | 0.35–0.98 | 0.04 | 0.97 | 0.94–1.00 | 0.10 | |||
| Standard-risk disease | |||||||||
| Donor HO-1 genotype, A/T or A/A vs. T/T | 0.79 | 0.61–1.02 | 0.07 | 1.19 | 0.56–2.50 | 0.66 | 0.98 | 0.68–1.41 | 0.91 |
| Recipient HO-1 genotype, A/T or A/A vs. T/T | 1.09 | 0.80–1.47 | 0.60 | 1.96 | 0.85–4.35 | 0.11 | 1.00 | 0.70–1.41 | 1.00 |
| Recipient age | 0.99 | 0.97–1.00 | 0.02 | ||||||
| CMV-positive recipient | 1.49 | 1.16–1.92 | 0.002 | ||||||
| Year of HSCT | 1.61 | 1.14-2.27 | 0.008 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Horio, T.; Morishita, E.; Mizuno, S.; Uchino, K.; Hanamura, I.; Espinoza, J.L.; Morishima, Y.; Kodera, Y.; Onizuka, M.; Kashiwase, K.; et al. Donor Heme Oxygenase-1 Promoter Gene Polymorphism Predicts Survival after Unrelated Bone Marrow Transplantation for High-Risk Patients. Cancers 2020, 12, 424. https://doi.org/10.3390/cancers12020424
Horio T, Morishita E, Mizuno S, Uchino K, Hanamura I, Espinoza JL, Morishima Y, Kodera Y, Onizuka M, Kashiwase K, et al. Donor Heme Oxygenase-1 Promoter Gene Polymorphism Predicts Survival after Unrelated Bone Marrow Transplantation for High-Risk Patients. Cancers. 2020; 12(2):424. https://doi.org/10.3390/cancers12020424
Chicago/Turabian StyleHorio, Tomohiro, Eriko Morishita, Shohei Mizuno, Kaori Uchino, Ichiro Hanamura, J. Luis Espinoza, Yasuo Morishima, Yoshihisa Kodera, Makoto Onizuka, Koichi Kashiwase, and et al. 2020. "Donor Heme Oxygenase-1 Promoter Gene Polymorphism Predicts Survival after Unrelated Bone Marrow Transplantation for High-Risk Patients" Cancers 12, no. 2: 424. https://doi.org/10.3390/cancers12020424
APA StyleHorio, T., Morishita, E., Mizuno, S., Uchino, K., Hanamura, I., Espinoza, J. L., Morishima, Y., Kodera, Y., Onizuka, M., Kashiwase, K., Fukuda, T., Doki, N., Miyamura, K., Mori, T., Nakao, S., & Takami, A. (2020). Donor Heme Oxygenase-1 Promoter Gene Polymorphism Predicts Survival after Unrelated Bone Marrow Transplantation for High-Risk Patients. Cancers, 12(2), 424. https://doi.org/10.3390/cancers12020424







