HDAC5 Inhibitors as a Potential Treatment in Breast Cancer Affecting Very Young Women
Abstract
1. Introduction
2. Results
2.1. Clinical-Pathologic Characteristics of Patients
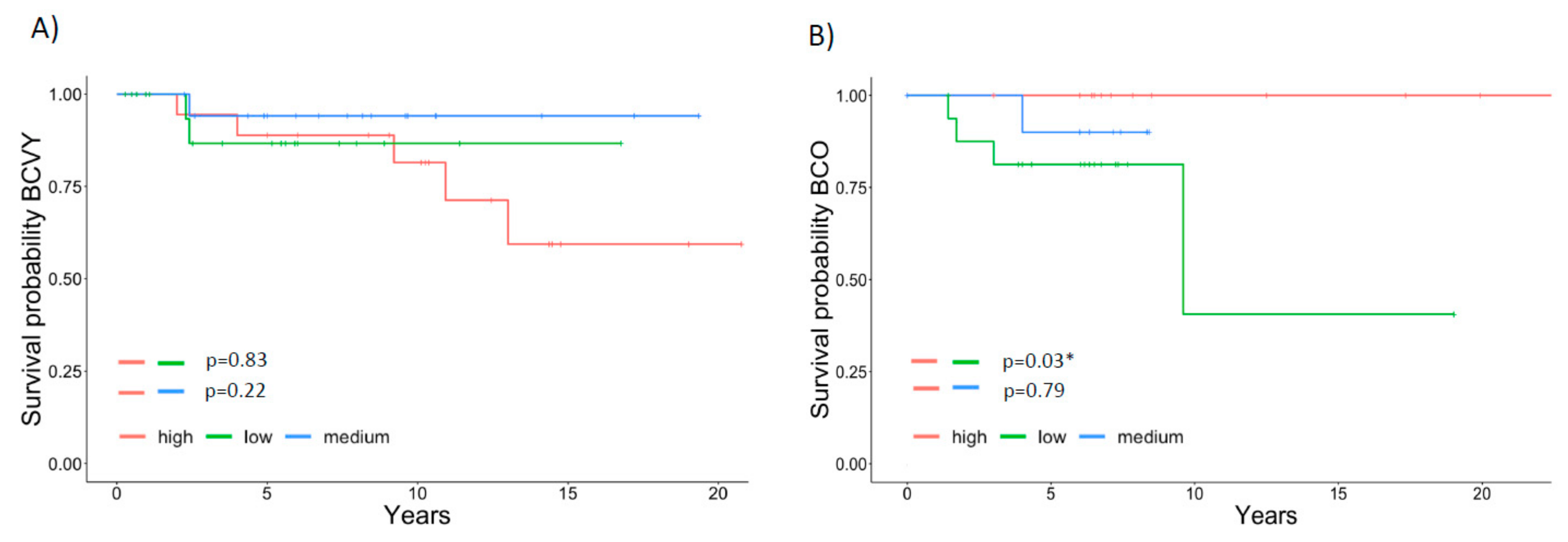
2.2. HDAC5 Overexpression in BCVY Patients Correlates with Poorer Prognosis
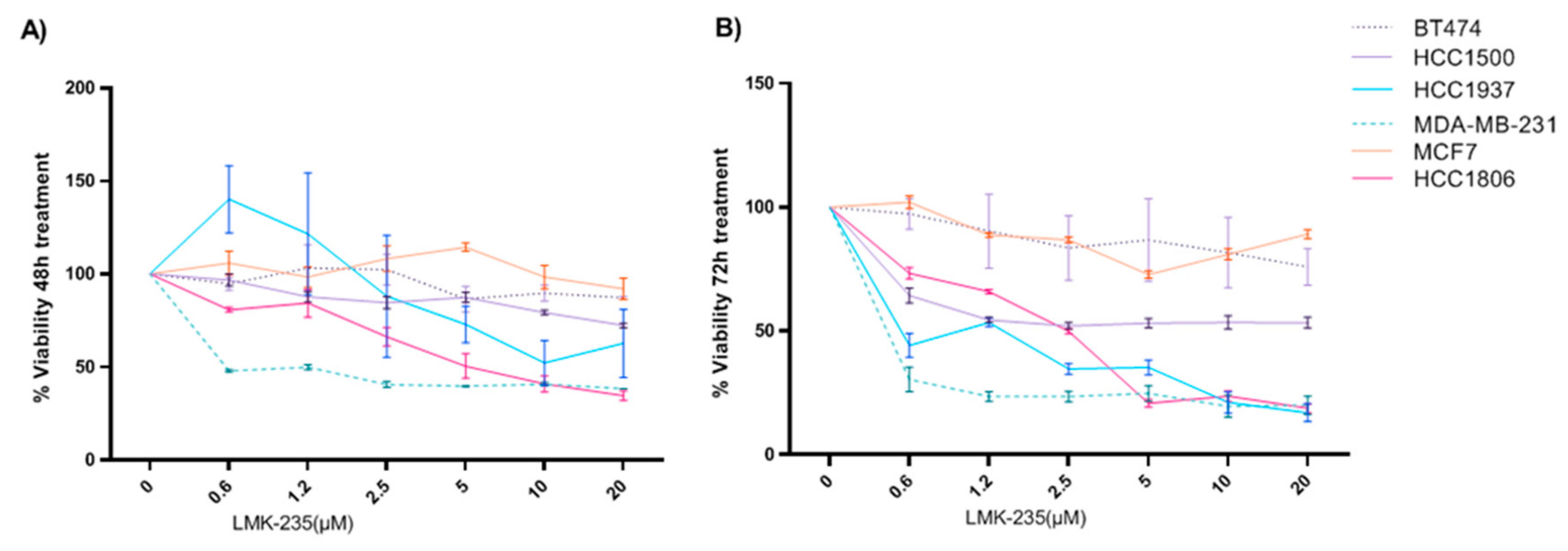
2.3. LMK-235 Inhibitor Reduces Proliferation in BC Cell Lines
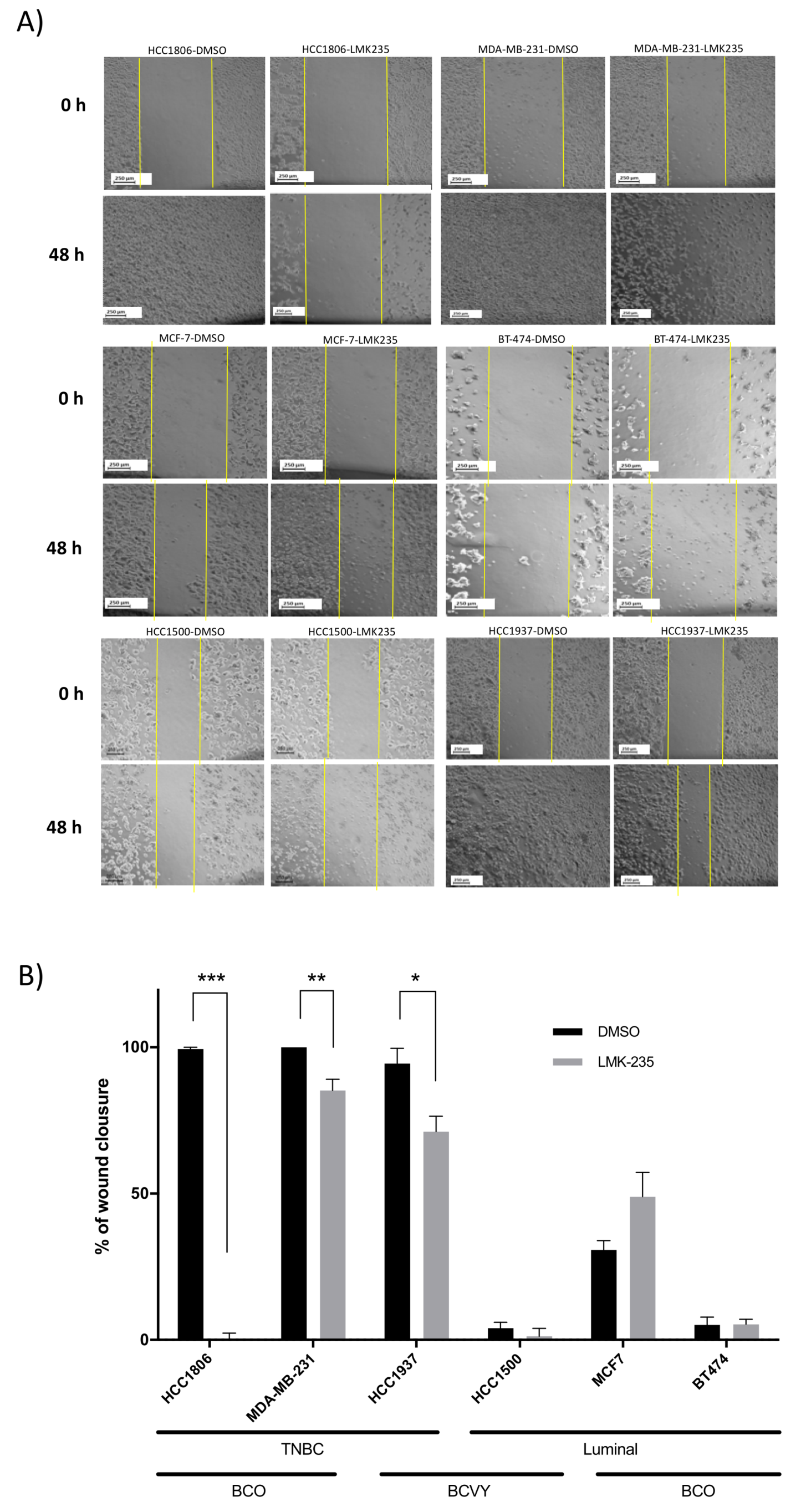
2.4. Reduced Migration of Breast Cancer Cell Lines Treated with LMK-235 Measured by Wound-Healing Assay
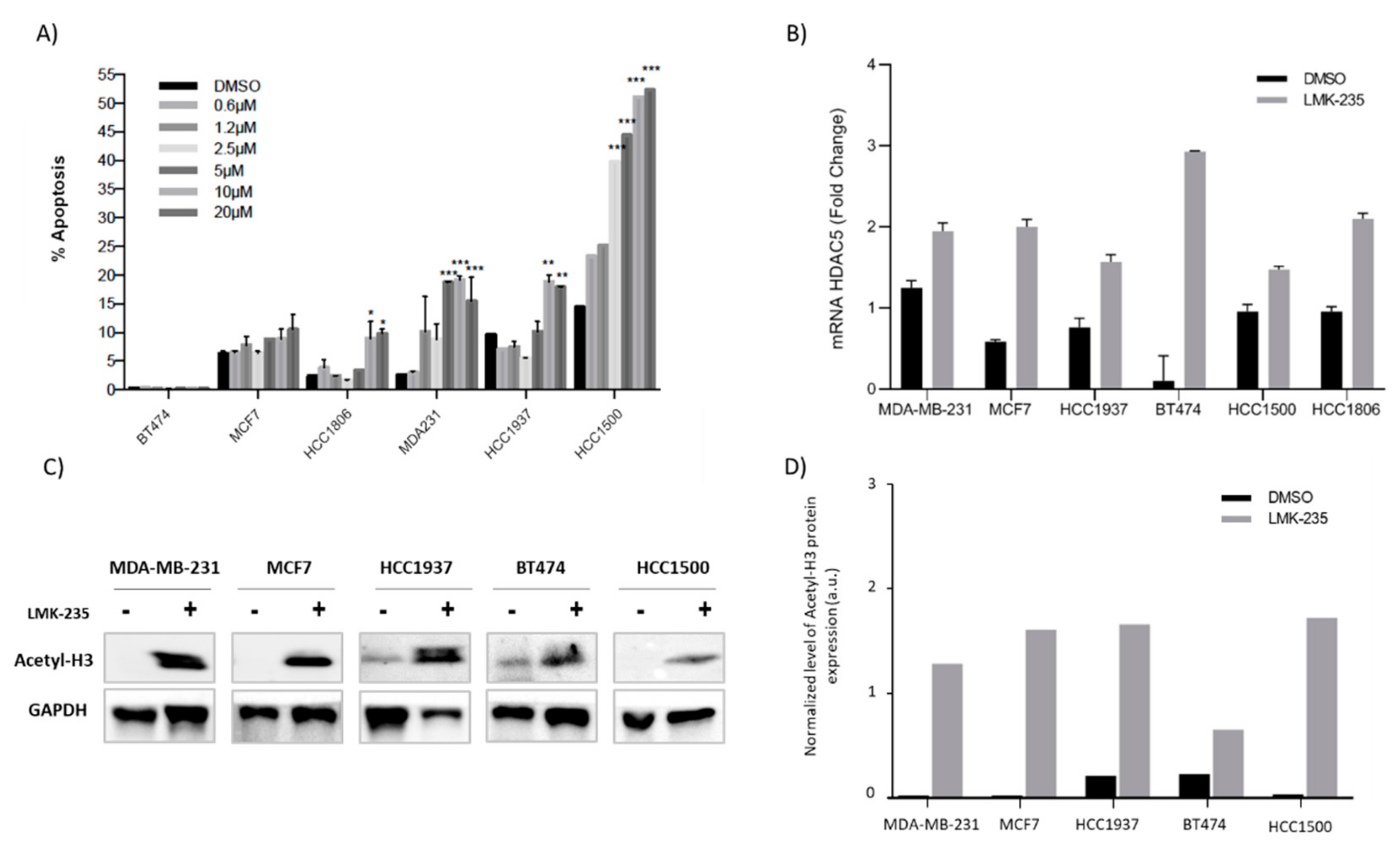
2.5. Apoptosis AfterLMK-235 Treatment
2.6. Accumulation of Acetyl-H3 After LMK-235 Treatment in Breast Cancer Cell Lines
3. Discussion
4. Materials and Methods
4.1. Patient Selection
4.2. Breast Cancer Cell Lines Culture and Treatment
4.3. Cell Proliferation Assay
4.4. Scratch Wound-Healing Assay
4.5. Apoptosis Assay by Flow Cytometry
4.6. Western Blot
4.7. RNA Extraction
4.8. Gene Expression by qRT-PCR
4.9. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Shapira, N. The potential contribution of dietary factors to breast cancer prevention. Eur. J. Cancer Prev. 2017, 26, 385–395. [Google Scholar] [CrossRef] [PubMed]
- Narod, S.A. Breast cancer in young women. Nat. Rev. Clin. Oncol. 2012, 9, 460–470. [Google Scholar] [CrossRef] [PubMed]
- Anastasiadi, Z.; Lianos, G.D.; Ignatiadou, E.; Harissis, H.V.; Mitsis, M. Breast cancer in young women: An overview. Updates Surg. 2017, 69, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Colleoni, M.; Rotmensz, N.; Robertson, C.; Orlando, L.; Viale, G.; Renne, G.; Luini, A.; Veronesi, P.; Intra, M.; Orecchia, R.; et al. Very young women (<35 years) with operable breast cancer: Features of disease at presentation. Ann. Oncol. 2002, 13, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Parker, J.S.; Mullins, M.; Cheang, M.C.; Leung, S.; Voduc, D.; Vickery, T.; Davies, S.; Fauron, C.; He, X.; Hu, Z.; et al. Supervised risk predictor of breast cancer based on intrinsic subtypes. J. Clin. Oncol. 2009, 27, 1160–1167. [Google Scholar] [CrossRef]
- Han, W.; Kim, S.W.; Park, I.A.; Kang, D.; Kim, S.W.; Youn, Y.K.; Oh, S.K.; Choe, K.J.; Noh, D.Y. Young age: An independent risk factor for disease-free survival in women with operable breast cancer. BMC Cancer 2004, 4, 82. [Google Scholar] [CrossRef]
- Anders, C.K.; Fan, C.; Parker, J.S.; Carey, L.A.; Blackwell, K.L.; Klauber-DeMore, N.; Perou, C.M. Breast carcinomas arising at a young age: Unique biology or a surrogate for aggressive intrinsic subtypes? J. Clin. Oncol. 2011, 29, e18. [Google Scholar] [CrossRef]
- Eckschlager, T.; Plch, J.; Stiborova, M.; Hrabeta, J. Histone Deacetylase Inhibitors as Anticancer Drugs. Int. J. Mol. Sci. 2017, 18, 1414. [Google Scholar] [CrossRef]
- Moser, M.A.; Hagelkruys, A.; Seiser, C. Transcription and beyond: The role of mammalian class I lysine deacetylases. Chromosoma 2014, 123, 67–78. [Google Scholar] [CrossRef]
- Nakagawa, M.; Oda, Y.; Eguchi, T.; Aishima, S.; Yao, T.; Hosoi, F.; Basaki, Y.; Ono, M.; Kuwano, M.; Tanaka, M.; et al. Expression profile of class I histone deacetylases in human cancer tissues. Oncol. Rep. 2007, 18, 769–774. [Google Scholar] [CrossRef]
- Montezuma, D.; Henrique, R.M.; Jeronimo, C. Altered expression of histone deacetylases in cancer. Crit. Rev. Oncog. 2015, 20, 19–34. [Google Scholar] [CrossRef]
- Weichert, W. HDAC expression and clinical prognosis in human malignancies. Cancer Lett. 2009, 280, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Witt, O.; Deubzer, H.E.; Milde, T.; Oehme, I. HDAC family: What are the cancer relevant targets? Cancer Lett. 2009, 277, 8–21. [Google Scholar] [CrossRef] [PubMed]
- Li, A.; Liu, Z.; Li, M.; Zhou, S.; Xu, Y.; Xiao, Y.; Yang, W. HDAC5, a potential therapeutic target and prognostic biomarker, promotes proliferation, invasion and migration in human breast cancer. Oncotarget 2016, 7, 37966–37978. [Google Scholar] [CrossRef]
- Hull, E.E.; Montgomery, M.R.; Leyva, K.J. HDAC Inhibitors as Epigenetic Regulators of the Immune System: Impacts on Cancer Therapy and Inflammatory Diseases. BioMed Res. Int. 2016, 2016, 8797206. [Google Scholar] [CrossRef]
- Thurn, K.T.; Thomas, S.; Moore, A.; Munster, P.N. Rational therapeutic combinations with histone deacetylase inhibitors for the treatment of cancer. Future Oncol. 2011, 7, 263–283. [Google Scholar] [CrossRef]
- Subramanian, S.; Bates, S.E.; Wright, J.J.; Espinoza-Delgado, I.; Piekarz, R.L. Clinical Toxicities of Histone Deacetylase Inhibitors. Pharmaceuticals 2010, 3, 2751–2767. [Google Scholar] [CrossRef]
- Thaler, F.; Minucci, S. Next generation histone deacetylase inhibitors: The answer to the search for optimized epigenetic therapies? Expert Opin. Drug Discov. 2011, 6, 393–404. [Google Scholar] [CrossRef]
- Noureen, N.; Rashid, H.; Kalsoom, S. Identification of type-specific anticancer histone deacetylase inhibitors: Road to success. Cancer Chemother. Pharmacol. 2010, 66, 625–633. [Google Scholar] [CrossRef]
- Marek, L.; Hamacher, A.; Hansen, F.K.; Kuna, K.; Gohlke, H.; Kassack, M.U.; Kurz, T. Histone deacetylase (HDAC) inhibitors with a novel connecting unit linker region reveal a selectivity profile for HDAC4 and HDAC5 with improved activity against chemoresistant cancer cells. J. Med. Chem. 2013, 56, 427–436. [Google Scholar] [CrossRef]
- Pena-Chilet, M.; Martinez, M.T.; Perez-Fidalgo, J.A.; Peiro-Chova, L.; Oltra, S.S.; Tormo, E.; Alonso-Yuste, E.; Martinez-Delgado, B.; Eroles, P.; Climent, J.; et al. MicroRNA profile in very young women with breast cancer. BMC Cancer 2014, 14, 529. [Google Scholar] [CrossRef] [PubMed]
- Oltra, S.S.; Pena-Chilet, M.; Vidal-Tomas, V.; Flower, K.; Martinez, M.T.; Alonso, E.; Burgues, O.; Lluch, A.; Flanagan, J.M.; Ribas, G. Methylation deregulation of miRNA promoters identifies miR124-2 as a survival biomarker in Breast Cancer in very young women. Sci. Rep. 2018, 8, 14373. [Google Scholar] [CrossRef] [PubMed]
- Oltra, S.S.; Peña-Chilet, M.; Flower, K.; Martinez, M.T.; Alonso, E.; Burgues, O.; Lluch, A.; Flanagan, J.M.; Ribas, G. Acceleration in the DNA methylation age in breast cancer tumours from very young women. Sci. Rep. 2019, 9, 14991. [Google Scholar] [CrossRef] [PubMed]
- Kaletsch, A.; Pinkerneil, M.; Hoffmann, M.J.; Jaguva Vasudevan, A.A.; Wang, C.; Hansen, F.K.; Wiek, C.; Hanenberg, H.; Gertzen, C.; Gohlke, H.; et al. Effects of novel HDAC inhibitors on urothelial carcinoma cells. Clin. Epigenetics 2018, 10, 100. [Google Scholar] [CrossRef] [PubMed]
- Haberland, M.; Montgomery, R.L.; Olson, E.N. The many roles of histone deacetylases in development and physiology: Implications for disease and therapy. Nat. Rev. Genet. 2009, 10, 32–42. [Google Scholar] [CrossRef]
- Dawson, M.A.; Kouzarides, T. Cancer epigenetics: From mechanism to therapy. Cell 2012, 150, 12–27. [Google Scholar] [CrossRef]
- Li, A.; Liu, Z.; Li, M.; Zhou, S.; Xu, Y.; Xiao, Y.; Yang, W. Correction: HDAC5, a potential therapeutic target and prognostic biomarker, promotes proliferation, invasion and migration in human breast cancer. Oncotarget 2017, 8, 30619–30620. [Google Scholar] [CrossRef]
- Klieser, E.; Urbas, R.; Stattner, S.; Primavesi, F.; Jager, T.; Dinnewitzer, A.; Mayr, C.; Kiesslich, T.; Holzmann, K.; Di Fazio, P.; et al. Comprehensive immunohistochemical analysis of histone deacetylases in pancreatic neuroendocrine tumors: HDAC5 as a predictor of poor clinical outcome. Hum. Pathol. 2017, 65, 41–52. [Google Scholar] [CrossRef]
- Vasilatos, S.N.; Katz, T.A.; Oesterreich, S.; Wan, Y.; Davidson, N.E.; Huang, Y. Crosstalk between lysine-specific demethylase 1 (LSD1) and histone deacetylases mediates antineoplastic efficacy of HDAC inhibitors in human breast cancer cells. Carcinogenesis 2013, 34, 1196–1207. [Google Scholar] [CrossRef]
- Dawson, S.J.; Rueda, O.M.; Aparicio, S.; Caldas, C. A new genome-driven integrated classification of breast cancer and its implications. EMBO J. 2013, 32, 617–628. [Google Scholar] [CrossRef]
- Curtis, C.; Shah, S.P.; Chin, S.F.; Turashvili, G.; Rueda, O.M.; Dunning, M.J.; Speed, D.; Lynch, A.G.; Samarajiwa, S.; Yuan, Y.; et al. The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature 2012, 486, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Ohguchi, H.; Hideshima, T.; Anderson, K.C. The biological significance of histone modifiers in multiple myeloma: Clinical applications. Blood Cancer J. 2018, 8, 83. [Google Scholar] [CrossRef] [PubMed]
- De Cremoux, P.; Dalvai, M.; N’Doye, O.; Moutahir, F.; Rolland, G.; Chouchane-Mlik, O.; Assayag, F.; Lehmann-Che, J.; Kraus-Berthie, L.; Nicolas, A.; et al. HDAC inhibition does not induce estrogen receptor in human triple-negative breast cancer cell lines and patient-derived xenografts. Breast Cancer Res. Treat. 2015, 149, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Jang, E.R.; Lim, S.J.; Lee, E.S.; Jeong, G.; Kim, T.Y.; Bang, Y.J.; Lee, J.S. The histone deacetylase inhibitor trichostatin A sensitizes estrogen receptor alpha-negative breast cancer cells to tamoxifen. Oncogene 2004, 23, 1724–1736. [Google Scholar] [CrossRef]
- Raha, P.; Thomas, S.; Thurn, K.T.; Park, J.; Munster, P.N. Combined histone deacetylase inhibition and tamoxifen induces apoptosis in tamoxifen-resistant breast cancer models, by reversing Bcl-2 overexpression. Breast Cancer Res. 2015, 17, 26. [Google Scholar] [CrossRef]
- Thomas, S.; Thurn, K.T.; Raha, P.; Chen, S.; Munster, P.N. Efficacy of histone deacetylase and estrogen receptor inhibition in breast cancer cells due to concerted down regulation of Akt. PLoS ONE 2013, 8, e68973. [Google Scholar] [CrossRef]
- AJCC. Cancer Staging Manual Form Supplement, 8th ed.; American Joint Committee On Cancer (AJCC): Chicago, IL, USA; Available online: https://cancerstaging.org/About/news/Pages/AJCC-8th-Edition-Cancer-Staging-Form-and-Histology-and-Topography-Supplements-Available-Now.aspx (accessed on 5 June 2018).

| BCVY | p-Value (HDAC5 ~ CP) | BCO | p-Value (HDAC5 ~ CP) | |
|---|---|---|---|---|
| N | 60 | 47 | ||
| Age mean (years ± SD) | 32.1 ± 3.3 | 69.8 ± 9.3 | ||
| Histological subtypes (%) | 0.46 | 0.40 | ||
| Luminal A | 16.6 | 27.6 | ||
| Luminal B | 23.3 | 31.9 | ||
| TNBC | 23.3 | 17.0 | ||
| Luminal/HER2 | 21.6 | 10.6 | ||
| HER2 | 11.6 | 10.6 | ||
| Unknown | 3.6 | 2.3 | ||
| ER status (%) | ||||
| ER+ | 60.0 | 0.43 | 74.4 | 0.92 |
| ER- | 33.3 | 21.3 | ||
| Unknown | 6.7 | 4.3 | ||
| PR status (%) | ||||
| PR+ | 50.0 | 0.44 | 57.4 | 0.44 |
| PR- | 43.3 | 38.3 | ||
| Unknown | 6.7 | 4.3 | ||
| HER2 (%) | ||||
| HER2+ | 31.6 | 0.97 | 21.3 | 0.93 |
| HER2- | 61.6 | 74.5 | ||
| Unknown | 6.8 | 4.2 | ||
| KI67 (%) | 0.56 | 0.07 | ||
| <15% | 16.6 | 27.7 | ||
| 15–30% | 28.3 | 32.0 | ||
| >30% | 38.3 | 27.7 | ||
| Unknown | 16.8 | 12.6 | ||
| Grade (%) | 0.16 | 2.8 × 10−3 ** | ||
| I | 13.2 | 23.3 | ||
| II | 49.1 | 41.9 | ** | |
| III | 37.7 | 34.9 | * | |
| Unknown | ||||
| Tumour Size (%) | 0.16 | 0.02 * | ||
| <2 cm | 35.0 | 59.6 | ||
| 2–5 cm | 40.0 | 23.4 | ||
| >5 cm | 20.0 | 8.5 | ||
| Unknown | 5.0 | 8.5 | ||
| Axillary Affection (%) | 0.98 | 0.17 | ||
| POS | 38.3 | 29.8 | ||
| NEG | 56.6 | 63.8 | ||
| Unknown | 5.1 | 6.4 | ||
| Exitus (%) | 13.8 | 0.12 | 13.3 | 0.19 |
| Relapse (%) | 25.0 | 0.27 | 21.0 | 0.15 |
| Cell Line | Subtype | Receptor Expression | Tumor Type | Age | Culture Medium | Conditions | Supplements |
|---|---|---|---|---|---|---|---|
| HCC 1500 | Luminal | ER, PR | IDC | 32 | RPMI | 5% CO2 37 °C | 1% L-glu 10% FBS |
| HCC1937 | Basal | EGP2 | IDC | 24 | RPMI | 5% CO2 37 °C | 1% L-glu 10% FBS |
| MDA-MB-231 | Basal | EGFR, TGF-β | Carcinoma | 51 | RPMI | 5% CO2 37 °C | 1% L-glu 10% FBS |
| MCF7 | Luminal | ER, IGFBP | IDC | 69 | RPMI | 5% CO2 37 °C | 1% L-glu 10% FBS |
| BT474 | Luminal | ER, PR, HER2 | IDC | 60 | DMEM | 5% CO2 37 °C | 1% L-glu 10% FBS |
| HCC1806 | Basal | EGP2 | Carcinoma | 60 | RPMI | 5% CO2 37 °C | 1% L-glu 10% FBS 10% FBS |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oltra, S.S.; Cejalvo, J.M.; Tormo, E.; Albanell, M.; Ferrer, A.; Nacher, M.; Bermejo, B.; Hernando, C.; Chirivella, I.; Alonso, E.; et al. HDAC5 Inhibitors as a Potential Treatment in Breast Cancer Affecting Very Young Women. Cancers 2020, 12, 412. https://doi.org/10.3390/cancers12020412
Oltra SS, Cejalvo JM, Tormo E, Albanell M, Ferrer A, Nacher M, Bermejo B, Hernando C, Chirivella I, Alonso E, et al. HDAC5 Inhibitors as a Potential Treatment in Breast Cancer Affecting Very Young Women. Cancers. 2020; 12(2):412. https://doi.org/10.3390/cancers12020412
Chicago/Turabian StyleOltra, Sara S., Juan Miguel Cejalvo, Eduardo Tormo, Marta Albanell, Ana Ferrer, Marta Nacher, Begoña Bermejo, Cristina Hernando, Isabel Chirivella, Elisa Alonso, and et al. 2020. "HDAC5 Inhibitors as a Potential Treatment in Breast Cancer Affecting Very Young Women" Cancers 12, no. 2: 412. https://doi.org/10.3390/cancers12020412
APA StyleOltra, S. S., Cejalvo, J. M., Tormo, E., Albanell, M., Ferrer, A., Nacher, M., Bermejo, B., Hernando, C., Chirivella, I., Alonso, E., Burgués, O., Peña-Chilet, M., Eroles, P., Lluch, A., Ribas, G., & Martinez, M. T. (2020). HDAC5 Inhibitors as a Potential Treatment in Breast Cancer Affecting Very Young Women. Cancers, 12(2), 412. https://doi.org/10.3390/cancers12020412





