Novel Quantitative Analysis Using Optical Imaging (VELscope) and Spectroscopy (Raman) Techniques for Oral Cancer Detection
Abstract
Simple Summary
Abstract
1. Introduction
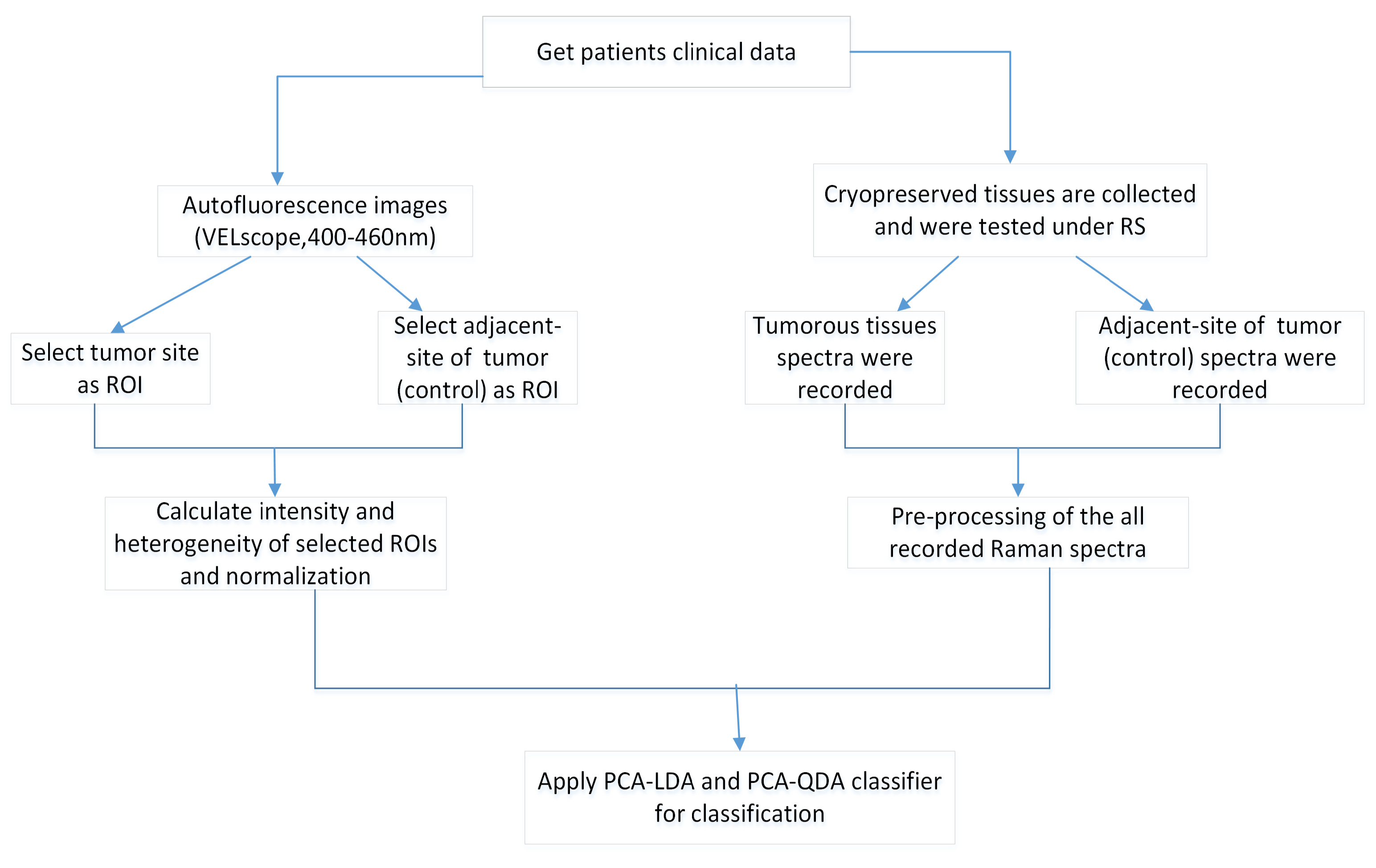
2. Materials and Methods
2.1. Patients and Data Collection
2.2. Preprocessing and Data Analysis Methods
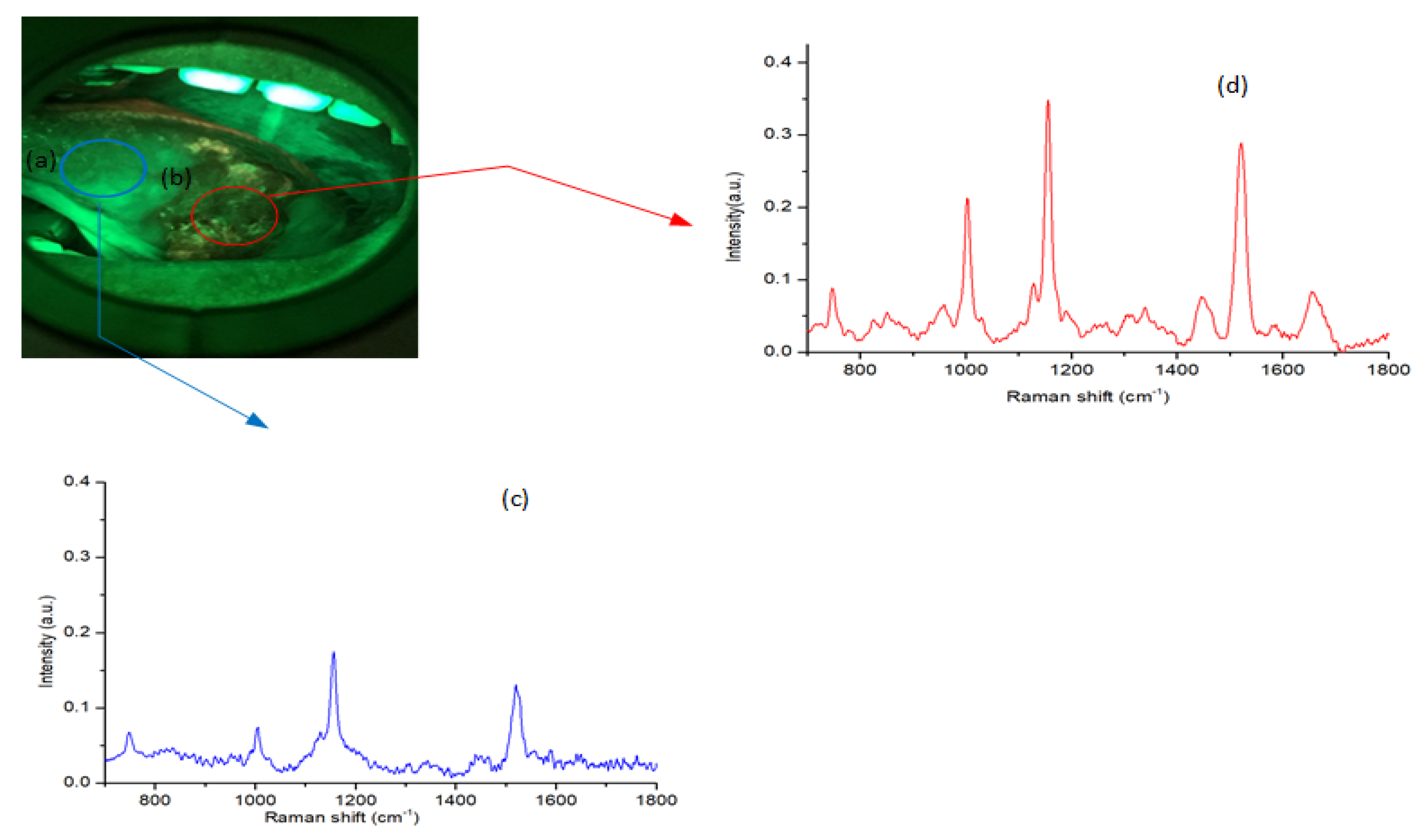
2.3. Raman Spectroscopy (RS)
2.4. VELscope
2.5. Analysis Method
3. Results and Discussion
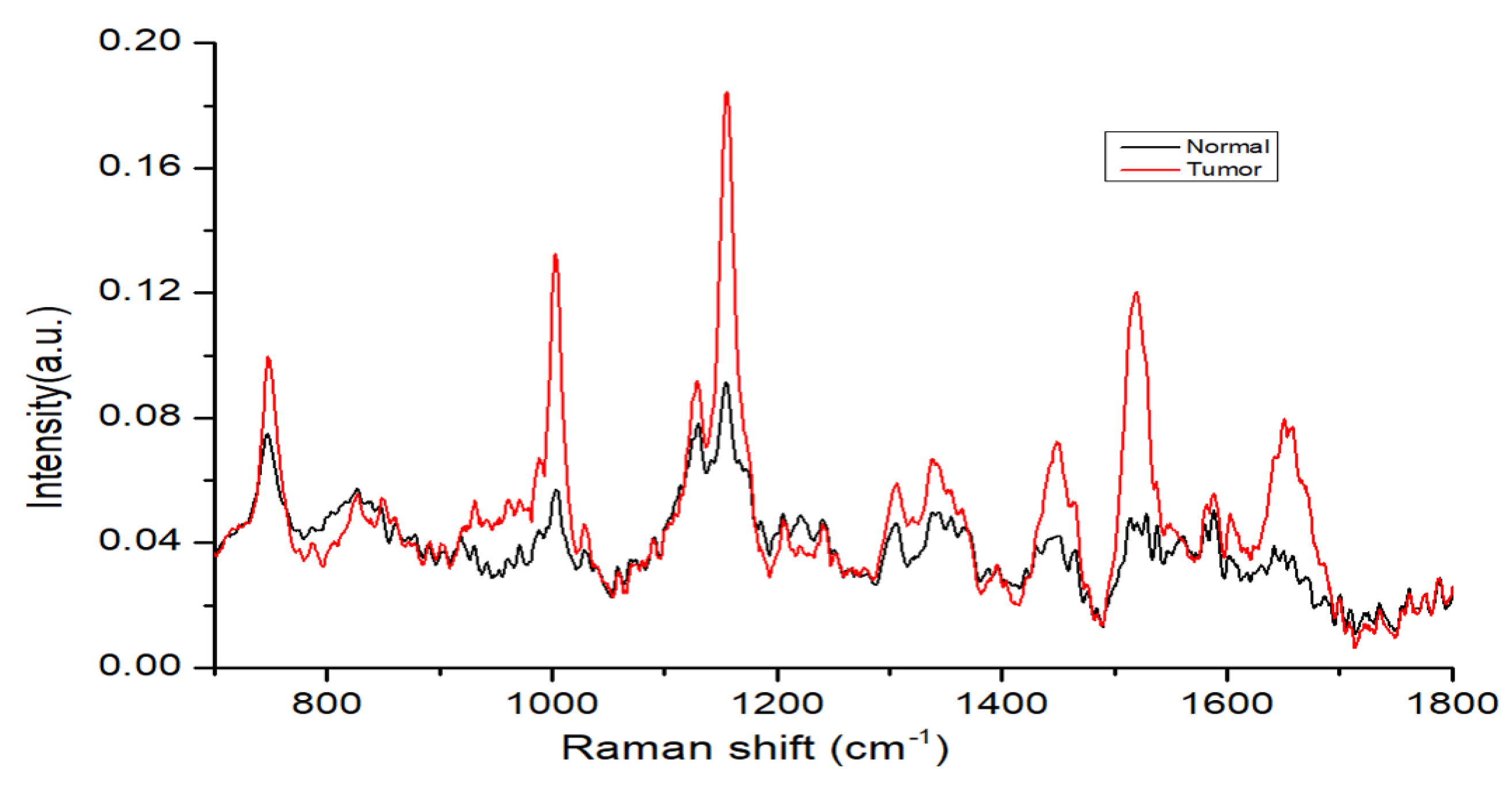
3.1. RS Band Spectral Features
3.2. Tissue Fluorescence Feature
3.3. Autofluorescence Imaging Analysis
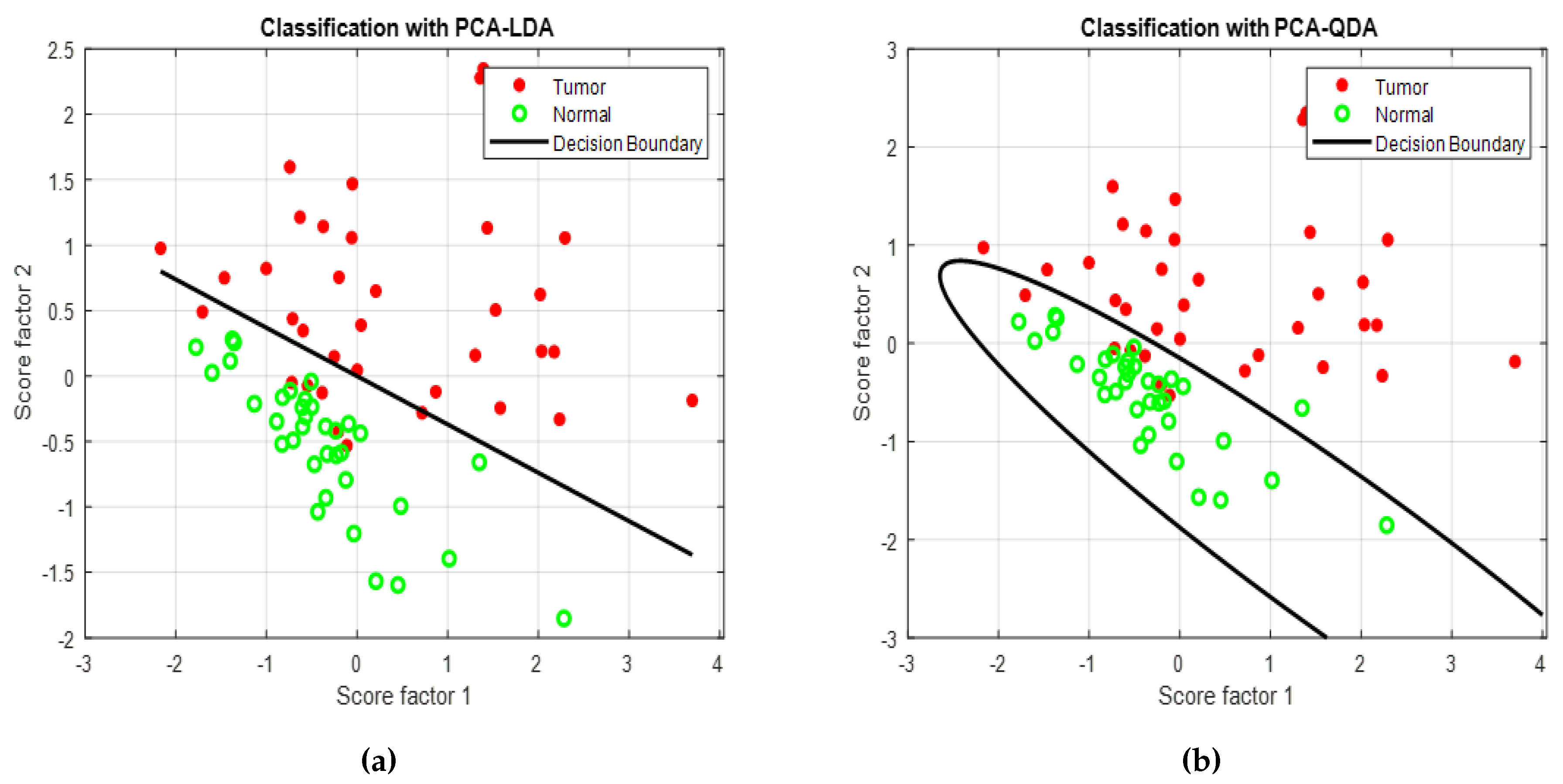
3.4. Raman Spectroscopic Analysis
3.5. Autofluorescence Imaging versus Raman Spectroscopic Analysis
3.6. Discussion
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Reddy, S.S.; Sharma, S.; Mysorekar, V. Expression of Epstein–barr virus among oral potentially malignant disorders and oral squamous cell carcinomas in the South Indian tobacco-chewing population. J. Oral Pathol. Med. 2017, 46, 454–459. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Samal, S.K.; Routray, S.; Dash, R.; Dixit, A. Identification of oral cancer related candidate genes by integrating protein-protein interactions, gene ontology, pathway analysis and immunohistochemistry. Sci. Rep. 2017, 7, 2472. [Google Scholar] [CrossRef] [PubMed]
- Stewart, B.W.; Kleihues, P. World Cancer Report 2014; International Agency for Research on Cancer: Lyon, France, 2014; pp. 16–69. [Google Scholar]
- Hsu, W.L.; Yu, K.J.; Chiang, C.J.; Chen, T.C.; Wang, C.P. Head and neck cancer incidence trends in Taiwan, 1980–2014. Int. J. Head Neck Sci. 2017, 1, 180–189. [Google Scholar]
- Allen, C.T.; Law, J.H.; Dunn, G.P.; Uppaluri, R. Emerging insights into head and neck cancer metastasis. Head Neck 2013, 35, 1669–1678. [Google Scholar] [CrossRef] [PubMed]
- Mortazavi, H.; Baharvand, M.; Mehdipour, M. Oral potentially malignant disorders: An overview of more than 20 entities. J. Dent. Res. Dent. Clin. Dent. Prospects 2014, 8, 6. [Google Scholar] [PubMed]
- Liu, D.; Zhao, X.; Zeng, X.; Dan, H.; Chen, Q. Non-invasive techniques for detection and diagnosis of oral potentially malignant disorders. Tohoku J. Exp. Med. 2016, 238, 165–177. [Google Scholar] [CrossRef] [PubMed]
- Lingen, M.W.; Tampi, M.P.; Urquhart, O.; Abt, E.; Agrawal, N.; Chaturvedi, A.K.; Cohen, E.; D’Souza, G.; Gurenlian, J.; Kalmar, J.R.; et al. Adjuncts for the evaluation of potentially malignant disorders in the oral cavity: Diagnostic test accuracy systematic review and meta-analysis—A report of the American Dental Association. J. Am. Dent. Assoc. 2017, 148, 797–813. [Google Scholar] [CrossRef]
- Jeng, M.J.; Sharma, M.; Chao, T.Y.; Li, Y.C.; Huang, S.F.; Chang, L.B.; Chow, L. Multiclass classification of autofluorescence images of oral cavity lesions based on quantitative analysis. PLoS ONE 2020, 15, e0228132. [Google Scholar] [CrossRef]
- Cordero, E.; Latka, I.; Matthäus, C.; Schie, I.W.; Popp, J. In-vivo Raman spectroscopy: From basics to applications. J. Biomed. Opt. 2018, 23, 071210. [Google Scholar] [CrossRef]
- Vašková, H. A powerful tool for material identification: Raman spectroscopy. Int. J. Math. Models Methods Appl. Sci. 2011, 5, 1205–1212. [Google Scholar]
- Pence, I.; Mahadevan-Jansen, A. Clinical instrumentation and applications of Raman spectroscopy. Chem. Soc. Rev. 2016, 45, 1958–1979. [Google Scholar] [CrossRef] [PubMed]
- Cui, S.; Zhang, S.; Yue, S. Raman Spectroscopy and Imaging for Cancer Diagnosis. J. Healthc. Eng. 2018, 2018. [Google Scholar] [CrossRef] [PubMed]
- Notingher, I. Raman spectroscopy cell-based biosensors. Sensors 2007, 7, 1343–1358. [Google Scholar] [CrossRef]
- Malini, R.; Venkatakrishna, K.; Kurien, J.; Pai, K.M.; Rao, L.; Kartha, V.; Krishna, C.M. Discrimination of normal, inflammatory, premalignant, and malignant oral tissue: A Raman spectroscopy study. Biopolym. Orig. Res. Biomol. 2006, 81, 179–193. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Deshmukh, A.; Chaturvedi, P.; Krishna, C.M. In vivo Raman spectroscopic identification of premalignant lesions in oral buccal mucosa. J. Biomed. Opt. 2012, 17, 105002. [Google Scholar] [CrossRef] [PubMed]
- Dai, W.Y.; Lee, S.; Hsu, Y.C. Discrimination between oral cancer and healthy cells based on the adenine signature detected by using Raman spectroscopy. J. Raman Spectrosc. 2018, 49, 336–342. [Google Scholar] [CrossRef]
- Chen, P.H.; Shimada, R.; Yabumoto, S.; Okajima, H.; Ando, M.; Chang, C.T.; Lee, L.T.; Wong, Y.K.; Chiou, A.; Hamaguchi, H.O. Automatic and objective oral cancer diagnosis by Raman spectroscopic detection of keratin with multivariate curve resolution analysis. Sci. Rep. 2016, 6, 20097. [Google Scholar] [CrossRef]
- Cals, F.L.; Bakker Schut, T.C.; Koljenović, S.; Puppels, G.J.; de Jong, R.J.B. Method development: Raman spectroscopy-based histopathology of oral mucosa. J. Raman Spectrosc. 2013, 44, 963–972. [Google Scholar] [CrossRef]
- Guze, K.; Pawluk, H.C.; Short, M.; Zeng, H.; Lorch, J.; Norris, C.; Sonis, S. Pilot study: Raman spectroscopy in differentiating premalignant and malignant oral lesions from normal mucosa and benign lesions in humans. Head Neck 2015, 37, 511–517. [Google Scholar] [CrossRef]
- Knipfer, C.; Motz, J.; Adler, W.; Brunner, K.; Gebrekidan, M.T.; Hankel, R.; Agaimy, A.; Will, S.; Braeuer, A.; Neukam, F.W.; et al. Raman difference spectroscopy: A non-invasive method for identification of oral squamous cell carcinoma. Biomed. Opt. Express 2014, 5, 3252–3265. [Google Scholar] [CrossRef]
- Jeng, M.J.; Sharma, M.; Sharma, L.; Chao, T.Y.; Huang, S.F.; Chang, L.B.; Wu, S.L.; Chow, L. Raman Spectroscopy Analysis for Optical Diagnosis of Oral Cancer Detection. J. Clin. Med. 2019, 8, 1313. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.T.; Diggins, K.E.; Walsh, A.J.; Irish, J.M.; Skala, M.C. In vivo autofluorescence imaging of tumor heterogeneity in response to treatment. Neoplasia 2015, 17, 862–870. [Google Scholar] [CrossRef] [PubMed]
- Mirabet, V.; Carda, C.; Solves, P.; Novella-Maestre, E.; Carbonell-Uberos, F.; Caffarena, J.; Hornero, F.; Montero, J.; Roig, R. Long-term storage in liquid nitrogen does not affect cell viability in cardiac valve allografts. Cryobiology 2008, 57, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Sahu, A.; Sawant, S.; Talathi-Desai, S.; Murali Krishna, C. Raman spectroscopy of serum: A study on oral cancers. Biomed. Spectrosc. Imaging 2015, 4, 171–187. [Google Scholar] [CrossRef]
- Siqueira, L.F.; Júnior, R.F.A.; de Araújo, A.A.; Morais, C.L.; Lima, K.M. LDA vs. QDA for FT-MIR prostate cancer tissue classification. Chemom. Intell. Lab. Syst. 2017, 162, 123–129. [Google Scholar] [CrossRef]
- Xie, J.; Qiu, Z. The effect of imbalanced data sets on LDA: A theoretical and empirical analysis. Pattern Recognit. 2007, 40, 557–562. [Google Scholar] [CrossRef]
- Eisenbeis, R.A. Pitfalls in the application of discriminant analysis in business, finance, and economics. J. Financ. 1977, 32, 875–900. [Google Scholar] [CrossRef]
- Ďurčeková, T.; Mocák, J.; Balla, J.; Gromanová, G.; Boronová, K. Relationship between administration of statins and blood serum levels of selected biochemical parameters. Trnava 2009, 2009, 83. [Google Scholar]
- Xue, J.H.; Titterington, D.M. Do unbalanced data have a negative effect on LDA? Pattern Recognit. 2008, 41, 1558–1571. [Google Scholar] [CrossRef]
- Parker, F.S. Applications of Infrared, Raman, and Resonance Raman Spectroscopy in Biochemistry; Springer Science & Business Media: New York, NY, USA, 1983. [Google Scholar]
- Movasaghi, Z.; Rehman, S.; Rehman, I.U. Raman spectroscopy of biological tissues. Appl. Spectrosc. Rev. 2007, 42, 493–541. [Google Scholar] [CrossRef]
- Carvalho, L.F.C.; Nogueira, M.S.; Bhattacharjee, T.; Neto, L.P.; Daun, L.; Mendes, T.O.; Rajasekaran, R.; Chagas, M.; Martin, A.A.; Soares, L.E.S. In vivo Raman spectroscopic characteristics of different sites of the oral mucosa in healthy volunteers. Clin. Oral Investig. 2019, 23, 3021–3031. [Google Scholar] [CrossRef] [PubMed]
- Cals, F.L.; Schut, T.C.B.; Hardillo, J.A.; De Jong, R.J.B.; Koljenović, S.; Puppels, G.J. Investigation of the potential of Raman spectroscopy for oral cancer detection in surgical margins. Lab. Investig. 2015, 95, 1186. [Google Scholar] [CrossRef] [PubMed]
- Sahu, A.; Tawde, S.; Pai, V.; Gera, P.; Chaturvedi, P.; Nair, S.; Krishna, C.M. Raman spectroscopy and cytopathology of oral exfoliated cells for oral cancer diagnosis. Anal. Methods 2015, 7, 7548–7559. [Google Scholar] [CrossRef]
- Huang, Z.; McWilliams, A.; Lui, H.; McLean, D.I.; Lam, S.; Zeng, H. Near-infrared Raman spectroscopy for optical diagnosis of lung cancer. Int. J. Cancer 2003, 107, 1047–1052. [Google Scholar] [CrossRef] [PubMed]
- Laronde, D.M.; Williams, P.M.; Hislop, T.G.; Poh, C.; Ng, S.; Bajdik, C.; Zhang, L.; MacAulay, C.; Rosin, M.P. Influence of fluorescence on screening decisions for oral mucosal lesions in community dental practices. J. Oral Pathol. Med. 2014, 43, 7–13. [Google Scholar] [CrossRef]
- Panta, P. Oral Cancer Detection: Novel Strategies and Clinical Impact; Springer: New York, NY, USA, 2018. [Google Scholar]
- Huang, T.T.; Huang, J.S.; Wang, Y.Y.; Chen, K.C.; Wong, T.Y.; Chen, Y.C.; Wu, C.W.; Chan, L.P.; Lin, Y.C.; Kao, Y.H.; et al. Novel quantitative analysis of autofluorescence images for oral cancer screening. Oral Oncol. 2017, 68, 20–26. [Google Scholar] [CrossRef]
- Wang, H.; Zheng, H. Model Validation, Machine Learning. In Encyclopedia of Systems Biology; Dubitzky, W., Wolkenhauer, O., Cho, K.H., Yokota, H., Eds.; Springer: New York, NY, USA, 2013; pp. 1406–1407. [Google Scholar] [CrossRef]
- Bhatia, N.; Lalla, Y.; Vu, A.N.; Farah, C.S. Advances in optical adjunctive AIDS for visualisation and detection of oral malignant and potentially malignant lesions. Int. J. Dent. 2013, 2013, 194029. [Google Scholar] [CrossRef]
- Huang, T.T.; Chen, K.C.; Wong, T.Y.; Chen, C.Y.; Chen, W.C.; Chen, Y.C.; Chang, M.H.; Wu, D.Y.; Huang, T.Y.; Nioka, S.; et al. Two-channel autofluorescence analysis for oral cancer. J. Biomed. Opt. 2018, 24, 051402. [Google Scholar] [CrossRef]


| Characteristics | N(%) |
|---|---|
| Sex | |
| Male | 31 (89) |
| Female | 4 (11) |
| Stage | |
| T1 | 3 (9) |
| T2 | 11 (31) |
| T3 | 10 (29) |
| T4 | 11 (31) |
| Subsites | |
| Tongue | 8 (23) |
| Buccal mucosa | 18 (51) |
| Gingiva | 8 (23) |
| Mouth floor | 1 (3) |
| Data Set | Confusion Table | Performance Parameters | ||||
|---|---|---|---|---|---|---|
| PCA–LDA | Normal | Tumor | Total | Accuracy (%) | Sensitivity (%) | Specificity (%) |
| Normal | 28 | 7 | 35 | 90 | 100 | 80 |
| Tumor | 0 | 35 | 35 | |||
| PCA–QDA | Normal | Tumor | Total | Accuracy (%) | Sensitivity (%) | Specificity (%) |
| Normal | 29 | 6 | 35 | 90 | 97.14 | 82.86 |
| Tumor | 1 | 34 | 35 | |||
| Data Set | Confusion Table | Performance Parameters | ||||
|---|---|---|---|---|---|---|
| PCA–LDA | Normal | Tumor | Total | Accuracy (%) | Sensitivity (%) | Specificity (%) |
| Normal | 28 | 7 | 35 | 82.9 | 80 | 85.71 |
| Tumor | 5 | 30 | 35 | |||
| PCA–QDA | Normal | Tumor | Total | Accuracy (%) | Sensitivity (%) | Specificity (%) |
| Normal | 28 | 7 | 35 | 82.9 | 80 | 85.71 |
| Tumor | 5 | 30 | 35 | |||
| Data Set | Confusion Table | Performance Parameters | ||||
|---|---|---|---|---|---|---|
| PCA–LDA | Normal | Tumor | Total | Accuracy (%) | Sensitivity (%) | Specificity (%) |
| Normal | 33 | 2 | 35 | 97.14 | 100 | 94.3 |
| Tumor | 0 | 35 | 35 | |||
| PCA–QDA | Normal | Tumor | Total | Accuracy (%) | Sensitivity (%) | Specificity (%) |
| Normal | 33 | 2 | 35 | 97.14 | 100 | 94.3 |
| Tumor | 0 | 35 | 35 | |||
| Error Rate | PCA–LDA (%) | PCA–QDA (%) | Validation: KFold (%) | Validation: LOOCV (%) |
|---|---|---|---|---|
| Raman analysis | 17.10 | 17.10 | 17.10 | 14.30 |
| VELscope analysis | 10 | 10 | 10 | 10 |
| Raman+VELscope analysis | 3 | 3 | 7 | 9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeng, M.-J.; Sharma, M.; Sharma, L.; Huang, S.-F.; Chang, L.-B.; Wu, S.-L.; Chow, L. Novel Quantitative Analysis Using Optical Imaging (VELscope) and Spectroscopy (Raman) Techniques for Oral Cancer Detection. Cancers 2020, 12, 3364. https://doi.org/10.3390/cancers12113364
Jeng M-J, Sharma M, Sharma L, Huang S-F, Chang L-B, Wu S-L, Chow L. Novel Quantitative Analysis Using Optical Imaging (VELscope) and Spectroscopy (Raman) Techniques for Oral Cancer Detection. Cancers. 2020; 12(11):3364. https://doi.org/10.3390/cancers12113364
Chicago/Turabian StyleJeng, Ming-Jer, Mukta Sharma, Lokesh Sharma, Shiang-Fu Huang, Liann-Be Chang, Shih-Lin Wu, and Lee Chow. 2020. "Novel Quantitative Analysis Using Optical Imaging (VELscope) and Spectroscopy (Raman) Techniques for Oral Cancer Detection" Cancers 12, no. 11: 3364. https://doi.org/10.3390/cancers12113364
APA StyleJeng, M.-J., Sharma, M., Sharma, L., Huang, S.-F., Chang, L.-B., Wu, S.-L., & Chow, L. (2020). Novel Quantitative Analysis Using Optical Imaging (VELscope) and Spectroscopy (Raman) Techniques for Oral Cancer Detection. Cancers, 12(11), 3364. https://doi.org/10.3390/cancers12113364






