Long-Term Outcomes and Prognostic Factors of Endoscopic Submucosal Dissection for Early Gastric Cancer in Patients Aged ≥75 Years
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Patients
2.2. Evaluation of Baseline Patient Characteristics
2.3. Indication and Curability of ESD
2.4. Endoscopic and Histopathologic Evaluation of Lesion Characteristics
2.5. Short-Term Outcomes
2.6. Long-Term Outcomes
2.7. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Lesion Characteristics
3.3. Short-Term Outcomes
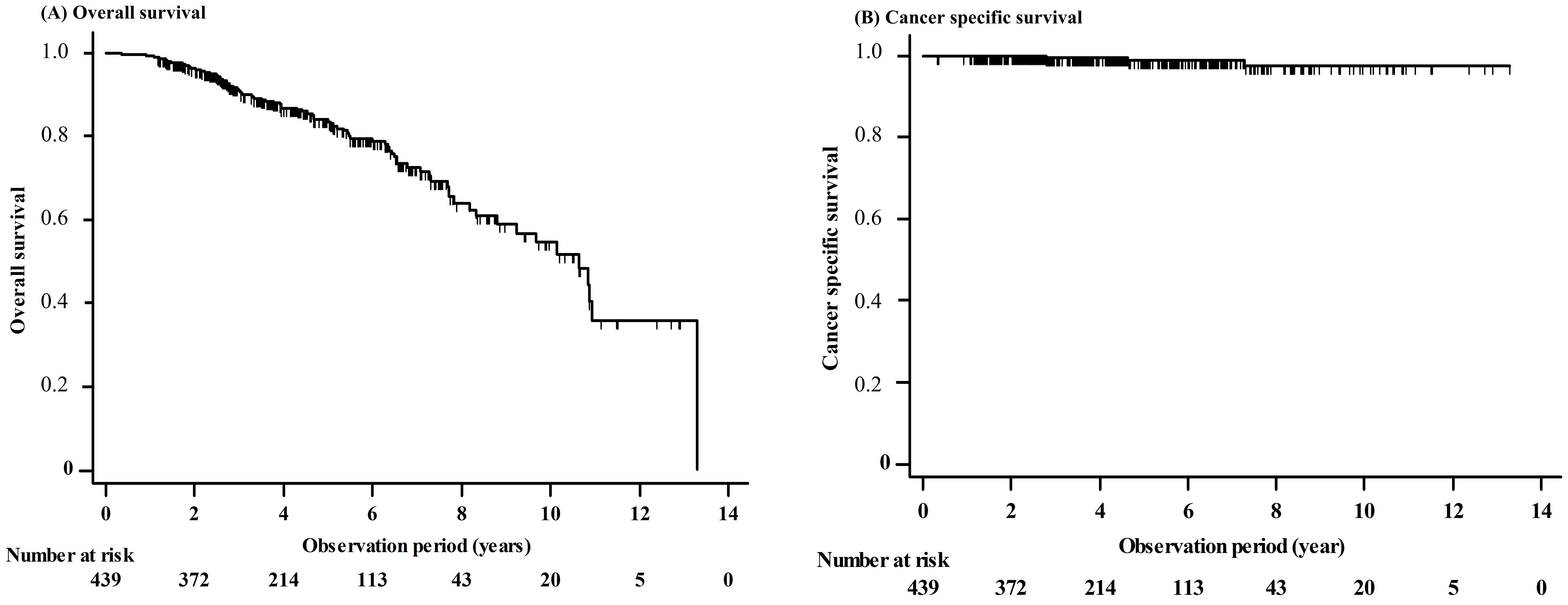
3.4. Long-Term Outcomes
4. Discussion and Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| EGC | early gastric cancer |
| ESD | endoscopic submucosal dissection |
| OS | overall survival |
| NLR | neutrophil-to-lymphocyte ratio |
| PNI | prognostic nutritional index |
| NLR | neutrophil-to-lymphocyte ratio |
| ASA-PS | American Society of Anesthesiologists-performance status |
| CCI | Charlson comorbidity index |
| LVI | lymphovascular invasion |
| CT | computed tomography |
| HR | hazard ratio |
| CI | confidence intervals |
| ROK | Republic of Korea |
References
- Jemal, A.; Bray, F.; Center, M.M.; Ferlay, J.; Ward, E.; Forman, D. Global cancer statistics. CA Cancer J. Clin. 2011, 61, 69–90. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; Bray, F. Global cancer Observatory: Cancer today. Lyon, France: International agency for research on cancer. Cancer Today 2018. Available online: https://gco.iarc.fr/today (accessed on 20 December 2018).
- Rawla, P.; Barsouk, A. Epidemiology of gastric cancer: Global trends, risk factors and prevention. Prz. Gastroenterol. 2019, 14, 26–38. [Google Scholar] [CrossRef] [PubMed]
- Jung, K.W.; Won, Y.J.; Oh, C.M.; Kong, H.J.; Cho, H.; Lee, D.H.; Lee, K.M. Prediction of cancer incidence and mortality in Korea, 2015. Cancer Res. Treat. 2015, 47, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Lim, D.; Ha, M.; Song, I. Trends in the leading causes of death in Korea, 1983–2012. J. Korean Med. Sci. 2014, 29, 1597–1603. [Google Scholar] [CrossRef]
- Oda, I.; Gotoda, T.; Hamanaka, H.; Eguchi, T.; Saito, Y.; Matsuda, T.; Bhandari, P.; Emura, F.; Saito, D.; Ono, H. Endoscopic submucosal dissection for early gastric cancer: Technical feasibility, operation time and complications from a large consecutive series. Dig. Endosc. 2005, 17, 54–58. [Google Scholar] [CrossRef]
- Abe, N.; Gotoda, T.; Hirasawa, T.; Hoteya, S.; Ishido, K.; Ida, Y.; Imaeda, H.; Ishii, E.; Kokawa, A.; Kusano, C.; et al. Multicenter study of the long-term outcomes of endoscopic submucosal dissection for early gastric cancer in patients 80 years of age or older. Gastric Cancer 2012, 15, 70–75. [Google Scholar] [CrossRef]
- Goto, O.; Fujishiro, M.; Kodashima, S.; Ono, S.; Omata, M. Outcomes of endoscopic submucosal dissection for early gastric cancer with special reference to validation for curability criteria. Endoscopy 2009, 41, 118–122. [Google Scholar] [CrossRef]
- Isomoto, H.; Shikuwa, S.; Yamaguchi, N.; Fukuda, E.; Ikeda, K.; Nishiyama, H.; Ohnita, K.; Mizuta, Y.; Shiozawa, J.; Kohno, S. Endoscopic submucosal dissection for early gastric cancer: A large-scale feasibility study. Gut 2009, 58, 331–336. [Google Scholar] [CrossRef]
- Park, C.H.; Lee, H.; Kim, D.W.; Chung, H.; Park, J.C.; Shin, S.K.; Hyung, W.J.; Lee, S.K.; Lee, Y.C.; Noh, S.H. Clinical safety of endoscopic submucosal dissection compared with surgery in elderly patients with early gastric cancer: A propensity-matched analysis. Gastrointest. Endosc. 2014, 80, 599–609. [Google Scholar] [CrossRef]
- Suzuki, H.; Oda, I.; Abe, S.; Sekiguchi, M.; Mori, G.; Nonaka, S.; Yoshinaga, S.; Saito, Y. High rate of 5-year survival among patients with early gastric cancer undergoing curative endoscopic submucosal dissection. Gastric Cancer 2016, 19, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Sekiguchi, M.; Oda, I.; Suzuki, H.; Abe, S.; Nonaka, S.; Yoshinaga, S.; Taniguchi, H.; Sekine, S.; Saito, Y. Clinical outcomes and prognostic factors in gastric cancer patients aged ≥85 years undergoing endoscopic submucosal dissection. Gastrointest. Endosc. 2017, 85, 963–972. [Google Scholar] [CrossRef] [PubMed]
- Sumiyoshi, T.; Kondo, H.; Fujii, R.; Minagawa, T.; Fujie, S.; Kimura, T.; Ihara, H.; Yoshizaki, N.; Hirayama, M.; Oyamada, Y.; et al. Short- and long-term outcomes of endoscopic submucosal dissection for early gastric cancer in elderly patients aged 75 years and older. Gastric Cancer 2017, 20, 489–495. [Google Scholar] [CrossRef]
- Yang, H.J.; Kim, S.G.; Lim, J.H.; Choi, J.M.; Oh, S.; Park, J.Y.; Han, S.J.; Kim, J.; Chung, H.; Jung, H.C. Surveillance strategy according to age after endoscopic resection of early gastric cancer. Surg. Endosc. 2018, 32, 846–854. [Google Scholar] [CrossRef] [PubMed]
- Jung, D.H.; Lee, Y.C.; Kim, J.H.; Lee, S.K.; Shin, S.K.; Park, J.C.; Chung, H.; Park, J.J.; Youn, Y.H.; Park, H. Additive treatment improves survival in elderly patients after non-curative endoscopic resection for early gastric cancer. Surg. Endosc. 2017, 31, 1376–1382. [Google Scholar] [CrossRef] [PubMed]
- Onodera, T.; Goseki, N.; Kosaki, G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nippon Geka Gakkai Zasshi 1984, 85, 1001–1005. [Google Scholar]
- Yamanaka, T.; Matsumoto, S.; Teramukai, S.; Ishiwata, R.; Nagai, Y.; Fukushima, M. The baseline ratio of neutrophils to lymphocytes is associated with patient prognosis in advanced gastric cancer. Oncology 2008, 73, 215–220. [Google Scholar] [CrossRef]
- Practice guidelines for sedation and analgesia by non-anesthesiologists: An updated report by the American Society of Anesthesiologists task force on sedation and analgesia by non-anesthesiologists. Anesthesiology 2002, 96, 1004–1017. [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer 2020. [Google Scholar] [CrossRef]
- Habibzadeh, F.; Habibzadeh, P.; Yadollahie, M. On determining the most appropriate test cut-off value: The case of tests with continuous results. Biochem. Med. 2016, 26, 297–307. [Google Scholar] [CrossRef]
- Korean Statistical Information Service (KOSIS). Life Expectancy 17 Provinces in Korea [Internet]. 2018. Available online: https://kosis.kr/statisticsList/statisticsListIndex.do?menuId=M_01_01&vwcd=MT_ZTITLE&parmTabId=M_01_01#SelectStatsBoxDiv (accessed on 10 December 2018).
- Yoshifuku, Y.; Oka, S.; Tanaka, S.; Sanomura, Y.; Miwata, T.; Numata, N.; Hiyama, T.; Chayama, K. Long-term prognosis after endoscopic submucosal dissection for early gastric cancer in super-elderly patients. Surg. Endosc. 2016, 30, 4321–4329. [Google Scholar] [CrossRef]
- Watanabe, K.; Hikichi, T.; Nakamura, J. Endo-scopic submucosal dissection for early gastric cancer in very elderly patients age 85 or older. Endosc. Int. Open 2017, 5, E17–E24. [Google Scholar]
- Toya, Y.; Endo, M.; Nakamura, S.; Akasaka, R.; Yanai, S.; Kawasaki, K.; Koeda, K.; Eizuka, M.; Fujita, Y.; Uesugi, N.; et al. Long-term outcomes and prognostic factors with non-curative endoscopic submucosal dissection for gastric cancer in elderly patients aged ≥75 years. Gastric Cancer 2019, 22, 838–844. [Google Scholar] [CrossRef] [PubMed]
- Numata, N.; Oka, S.; Tanaka, S.; Higashiyama, M.; Sanomura, Y.; Yoshida, S.; Arihiro, K.; Chayama, K. Clinical outcomes of endoscopic submucosal dissection for early gastric cancer in patients with chronic kidney disease. J. Gastroenterol. Hepatol. 2013, 28, 1632–1637. [Google Scholar] [CrossRef] [PubMed]
- Oda, I.; Saito, D.; Tada, M.; Iishi, H.; Tanabe, S.; Oyama, T.; Doi, T.; Otani, Y.; Fujisaki, J.; Ajioka, Y.; et al. A multicenter retrospective study of endoscopic resection for early gastric cancer. Gastric Cancer 2006, 9, 262–270. [Google Scholar] [CrossRef]
- Ko, B.M. History and Development of Accessories for Endoscopic Submucosal Dissection. Clin. Endosc. 2017, 50, 219–223. [Google Scholar] [CrossRef] [PubMed]
| Variables | Value |
|---|---|
| Demographic variables | |
| Age, years (range) | 78.3 (75–92) |
| Male gender | 302 (68.8) |
| Smoking history | 219 (49.9) |
| Heavy alcoholics | 36 (8.2) |
| Comorbidities (with overlap) | |
| Cardiovascular disease | 74 (16.9) |
| Cerebrovascular disease | 24 (5.5) |
| Cancer of the other organs | 53 (12.1) |
| Kidney disease | 18 (4.1) |
| Diabetes mellitus | 101 (23.0) |
| Hypertension | 255 (58.1) |
| Use of anticoagulants and/or antiplatelet drugs | 143 (32.6) |
| Prognostic factors | |
| Prognostic nutritional index (range) | 50.1 (35.0–115) |
| Neutrophil to lymphocyte ratio (range) | 3.2 (0.5–36.0) |
| ASA-PS score | |
| 1 | 21 (4.8) |
| 2 | 276 (62.9) |
| 3 | 135 (30.8) |
| 4 | 7 (1.6) |
| Charlson comorbidity index | |
| 1 | 1 (0.2) |
| 2 | 260 (59.2) |
| 3 | 136 (31.0) |
| 4 | 33 (7.5) |
| 5 | 7 (1.6) |
| 6 | 2 (0.5) |
| Variables | Value |
|---|---|
| Location | |
| Upper | 41 (9.3) |
| Middle | 100 (22.8) |
| Lower | 313 (71.3) |
| Remnant stomach | 3 (0.7) |
| Number of lesions | |
| 1 | 362 (82.5) |
| 2 | 64 (14.6) |
| 3 | 11 (2.5) |
| 4 | 2 (0.5) |
| Macroscopic type | |
| Elevated | 109 (24.8) |
| Flat | 46 (10.5) |
| Depressed | 44 (10.0) |
| Mixed | 240 (54.7) |
| Tumor size (mm), median | |
| Tumor size | |
| ≤20 mm | 326 (74.3) |
| 21–30 mm | 68 (15.5) |
| >30 mm | 45 (10.2) |
| Tumor depth | |
| Mucosa | 416 (94.8) |
| Submucosa | 23 (5.2) |
| Histologic type | |
| Differentiated | 401 (91.3) |
| Undifferentiated | 38 (8.7) |
| Lymphovascular involvement | |
| Present | 50 (11.4) |
| Absent | 389 (88.6) |
| Perineural involvement | |
| Present | 1 (0.2) |
| Absent | 438 (99.8) |
| Variables | Value |
|---|---|
| En bloc resection | 425 (96.8) |
| R0 resection | 398 (90.7) |
| Curative resection | 332 (75.6) |
| Adverse event (<48 hrs) | |
| Bleeding | 11 (2.5) |
| Perforation | 12 (2.7) |
| Pneumonia | 0 (0.0) |
| Adverse event (>48 hrs) | |
| Bleeding | 10 (2.3) |
| Perforation | 0 (0.0) |
| Pneumonia | 11 (2.5) |
| Procedure time (minutes), median (range) | 30 (5–300) |
| Duration of hospital stay for ESD (days), median (range) | 4 (2–15) |
| Clinicopathologic Features | Number of Patients | 3-Year OS, % (95% CI) | 5-Year OS, % (95% CI) | 10-Year OS, % (95% CI) | p-Value |
|---|---|---|---|---|---|
| Patients characteristics | |||||
| Sex | 0.025 | ||||
| Male | 302 | 88.8 (84.9–92.7) | 82.1 (77.0–87.2) | 48.1 (34.4–61.8) | |
| Female | 137 | 96.6 (93.3–99.9) | 87.2 (79.9–94.5) | 66.2 (51.3–81.1) | |
| Smoking | <0.001 | ||||
| Smoker | 219 | 87.6 (82.9–92.3) | 78.2 (71.5–84.9) | 42.6 (26.3–58.9) | |
| Non-smoker | 220 | 94.6 (91.3–97.9) | 88.8 (83.5–94.1) | 65.0 (51.7–78.3) | |
| Alcohol | 0.006 | ||||
| Heavy | 36 | 79.2 (64.3–94.1) | 53.3 (20.6–86.0) | 53.3 (20.6–86.0) | |
| Non-alcohol, social | 403 | 92.1 (89.2–95.0) | 84.7 (80.4–89.0) | 55.5 (44.9–66.1) | |
| Cardiovascular disease | 0.054 | ||||
| Yes | 74 | 91.4 (84.0–98.8) | 76.4 (62.7–90.1) | 27.5 (0.3–54.7) | |
| No | 365 | 91.1 (88.0–94.2) | 84.6 (80.1–89.1) | 58.0 (46.8–69.2) | |
| Cerebrovascular disease | 0.803 | ||||
| Yes | 24 | 85.4 (70.1–100) | 78.3 (58.9–97.7) | 78.3 (58.9–97.7) | |
| No | 415 | 91.5 (88.6–94.4) | 83.8 (79.5–88.1) | 53.9 (43.1–64.7) | |
| Cancer of the other organs | 0.022 | ||||
| Yes | 53 | 80.7 (68.4–93.0) | 72.4 (56.7–88.1) | 47.3 (24.2–70.4) | |
| No | 386 | 92.4 (89.5–95.3) | 84.8 (80.5–89.1) | 55.6 (44.2–67.0) | |
| Kidney disease | 0.591 | ||||
| Yes | 18 | 75.9 (55.1–96.7) | 75.9 (55.1–96.7) | 75.9 (55.1–96.7) | |
| No | 421 | 91.6 (88.7–94.5) | 83.9 (79.6–88.2) | 54.2 (43.6–64.8) | |
| DM | 0.195 | ||||
| Yes | 101 | 92.8 (89.9–95.7) | 84.8(80.1–89.5) | 51.3 (31.5–71.1) | |
| No | 338 | 85.2 (77.4–93.0) | 79.3 (69.5–89.1) | 55.3 (43.0–67.6) | |
| HTN | 0.749 | ||||
| Yes | 255 | 91.7 (88.0–95.4) | 85.6 (80.3–90.9) | 50.7 (36.2–65.2) | |
| No | 184 | 90.3 (85.6–95.0) | 80.6 (73.5–87.7) | 59.7 (45.2–74.2) | |
| Use of anticoagulants and/or antiplatelet drugs | 0.449 | ||||
| Yes | 143 | 88.0 (81.9–94.1) | 81.6 (73.8–89.4) | 55.6 (35.0–76.2) | |
| No | 296 | 92.7 (89.6–95.8) | 84.5 (79.4–89.6) | 54.7 (42.7–66.7) | |
| PNI | 0.278 | ||||
| ≤52.4 | 306 | 90.9 (87.4–94.4) | 81.4 (75.9–86.9) | 50.9 (33.8–68.0) | |
| >52.4 | 133 | 91.9 (86.8–97.0) | 88.1 (81.6–94.6) | 58.8 (44.1–73.5) | |
| NLR | 0.006 | ||||
| ≤1.6 | 124 | 94.0 (89.3–98.7) | 89.5 (82.8–96.2) | 69.3 (54.0–84.6) | |
| >1.6 | 315 | 90.0 (86.5–93.5) | 81.2 (75.9–86.5) | 47.5 (34.2–60.8) | |
| ASA-PS | 0.753 | ||||
| 1 & 2 | 297 | 90.6 (87.1–94.1) | 83.5 (78.4–88.6) | 54.1 (42.9–65.3) | |
| 3 & 4 | 142 | 92.5 (87.8–97.2) | 83.4 (75.2–91.6) | 49.0 (8.8–89.2) | |
| Charson comorbidity index | 0.002 | ||||
| ≤2 | 261 | 92.7 (89.2–96.2) | 87.1 (82.0–92.2) | 64.9 (51.0–78.8) | |
| ≥3 | 178 | 88.0 (82.5–93.5) | 78.2 (70.8–85.6) | 41.2 (26.1–56.3) | |
| Lesion characteristics | |||||
| Tumor size | 0.068 | ||||
| ≤30 | 394 | 90.5 (87.4–93.6) | 82.4 (77.9–86.9) | 52.7 (41.9–63.5) | |
| >30 | 45 | 97.7 (93.4–100) | 88.8 (71.7–100) | 88.8 (71.7–100) | |
| Histologic type | 0.339 | ||||
| Differentiated | 401 | 91.9 (89.0–94.8) | 84.2 (79.7–88.7) | 56.3 (54.3–67.3) | |
| Undifferentiated | 38 | 83.0 (70.5–95.5) | 75.9 (61.2–90.6) | 48.2 (21.3–75.1) | |
| Lymphovascular involvement | <0.001 | ||||
| Present | 50 | 86.2 (75.8–86.6) | 56.4 (37.2–75.6) | 32.3 (2.7–61.9) | |
| Absent | 359 | 91.6 (88.5–94.7) | 86.8 (82.7–90.9) | 56.9 (45.5–68.3) | |
| ESD curability | 0.037 | ||||
| Curative | 332 | 91.0 (87.7–94.3) | 86.9 (82.6–91.2) | 58.3 (45.4–71.2) | |
| Noncurative | 107 | 91.6 (85.9–97.3) | 72.7 (61.5–83.9) | 43.8 (26.2–61.4) | |
| En bloc resection | 0.481 | ||||
| En bloc resection | 425 | 91.3 (88.4–94.2) | 83.7 (79.4–88.0) | 54.4 (43.2–65.6) | |
| Piecemeal | 14 | 85.7 (67.3–100) | 76.2 (52.3–100) | 53.3 (21.4–85.2) |
| Variable | HR | 95% CI | p-Value |
|---|---|---|---|
| Male gender | 0.64 | 0.313–1.298 | 0.214 |
| Smoker | 3.96 | 2.050–7.652 | <0.001 |
| Heavy alcoholics | 1.78 | 0.850–3.740 | 0.126 |
| Cancer of the other organs | 2.42 | 1.296–4.520 | 0.006 |
| Neutrophil to lymphocyte ratio >1.6 | 1.83 | 1.043–3.211 | 0.035 |
| Charlson comorbidity index ≥3 | 2.05 | 1.317–3.195 | 0.001 |
| Lymphovascular involvement | 2.63 | 1.206–5.732 | 0.015 |
| Noncurative resection | 1.42 | 0.746–2.717 | 0.283 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, J.W.; Jung, D.H.; Park, J.C.; Shin, S.K.; Lee, S.K.; Lee, Y.C. Long-Term Outcomes and Prognostic Factors of Endoscopic Submucosal Dissection for Early Gastric Cancer in Patients Aged ≥75 Years. Cancers 2020, 12, 3222. https://doi.org/10.3390/cancers12113222
Chang JW, Jung DH, Park JC, Shin SK, Lee SK, Lee YC. Long-Term Outcomes and Prognostic Factors of Endoscopic Submucosal Dissection for Early Gastric Cancer in Patients Aged ≥75 Years. Cancers. 2020; 12(11):3222. https://doi.org/10.3390/cancers12113222
Chicago/Turabian StyleChang, Jin Won, Da Hyun Jung, Jun Chul Park, Sung Kwan Shin, Sang Kil Lee, and Yong Chan Lee. 2020. "Long-Term Outcomes and Prognostic Factors of Endoscopic Submucosal Dissection for Early Gastric Cancer in Patients Aged ≥75 Years" Cancers 12, no. 11: 3222. https://doi.org/10.3390/cancers12113222
APA StyleChang, J. W., Jung, D. H., Park, J. C., Shin, S. K., Lee, S. K., & Lee, Y. C. (2020). Long-Term Outcomes and Prognostic Factors of Endoscopic Submucosal Dissection for Early Gastric Cancer in Patients Aged ≥75 Years. Cancers, 12(11), 3222. https://doi.org/10.3390/cancers12113222






