Involvement of a Transcription factor, Nfe2, in Breast Cancer Metastasis to Bone
Simple Summary
Abstract
1. Introduction
2. Results
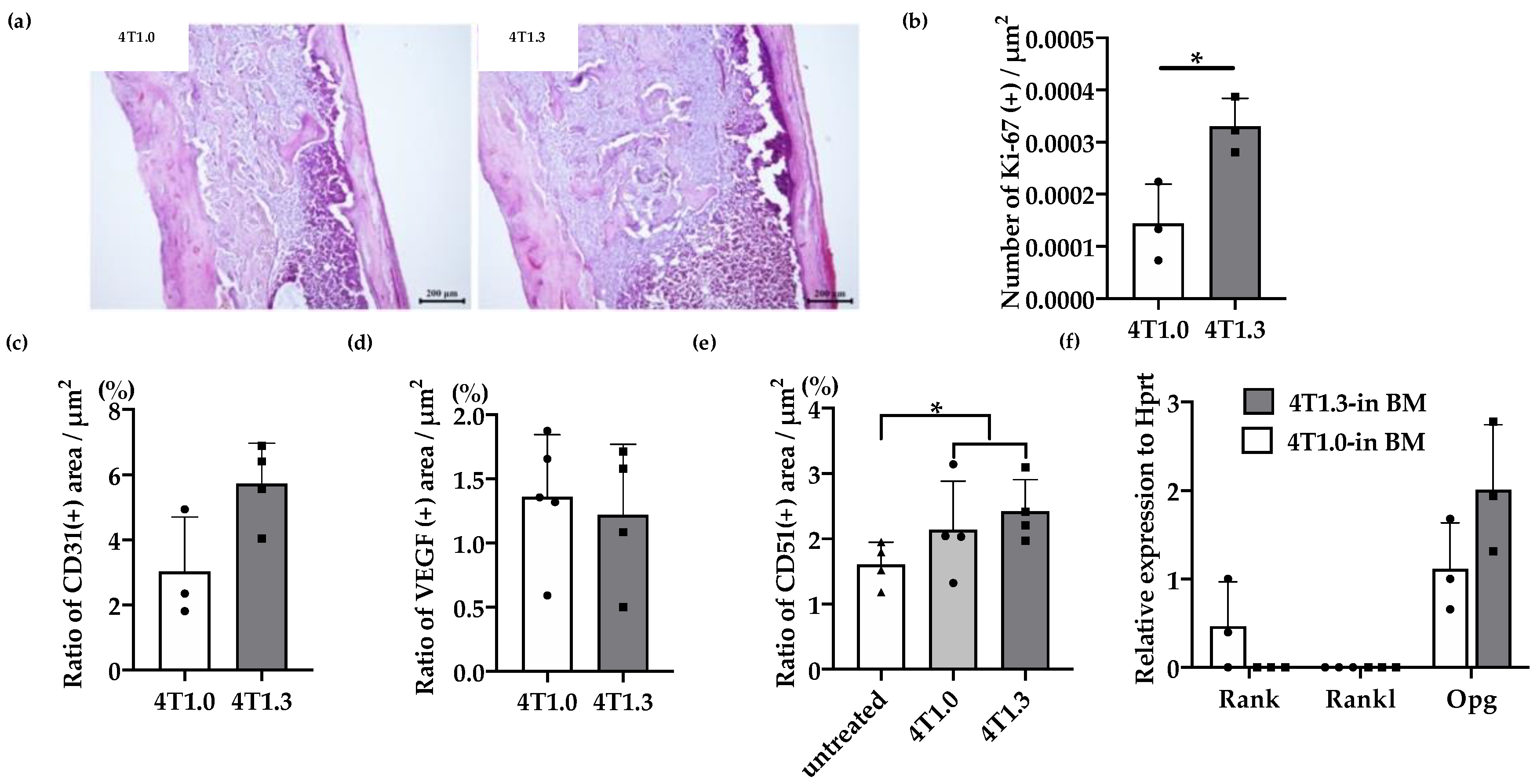
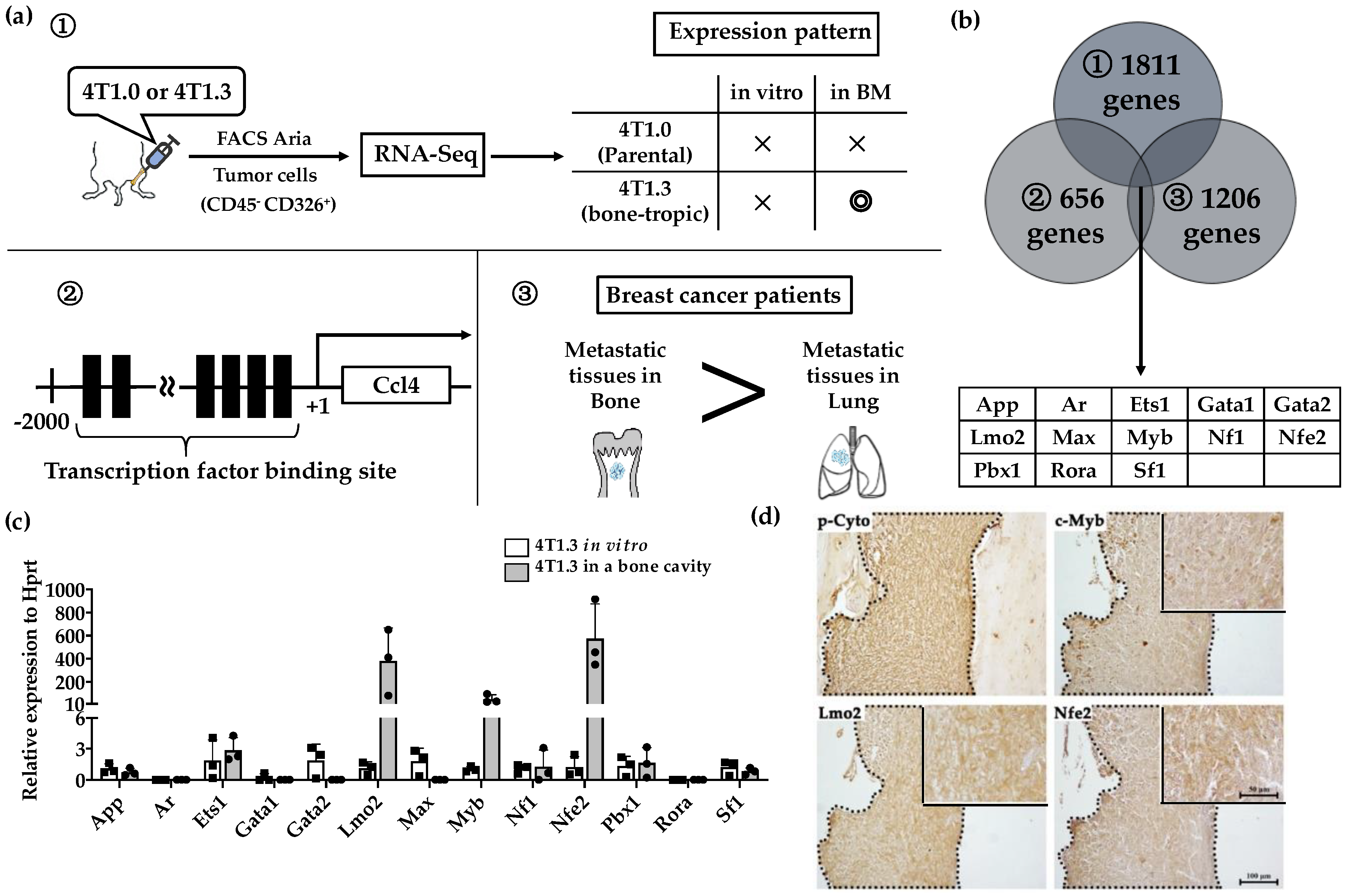
2.1. Transcription Factor Expression in 4T1.3 Grown in a Bone Cavity
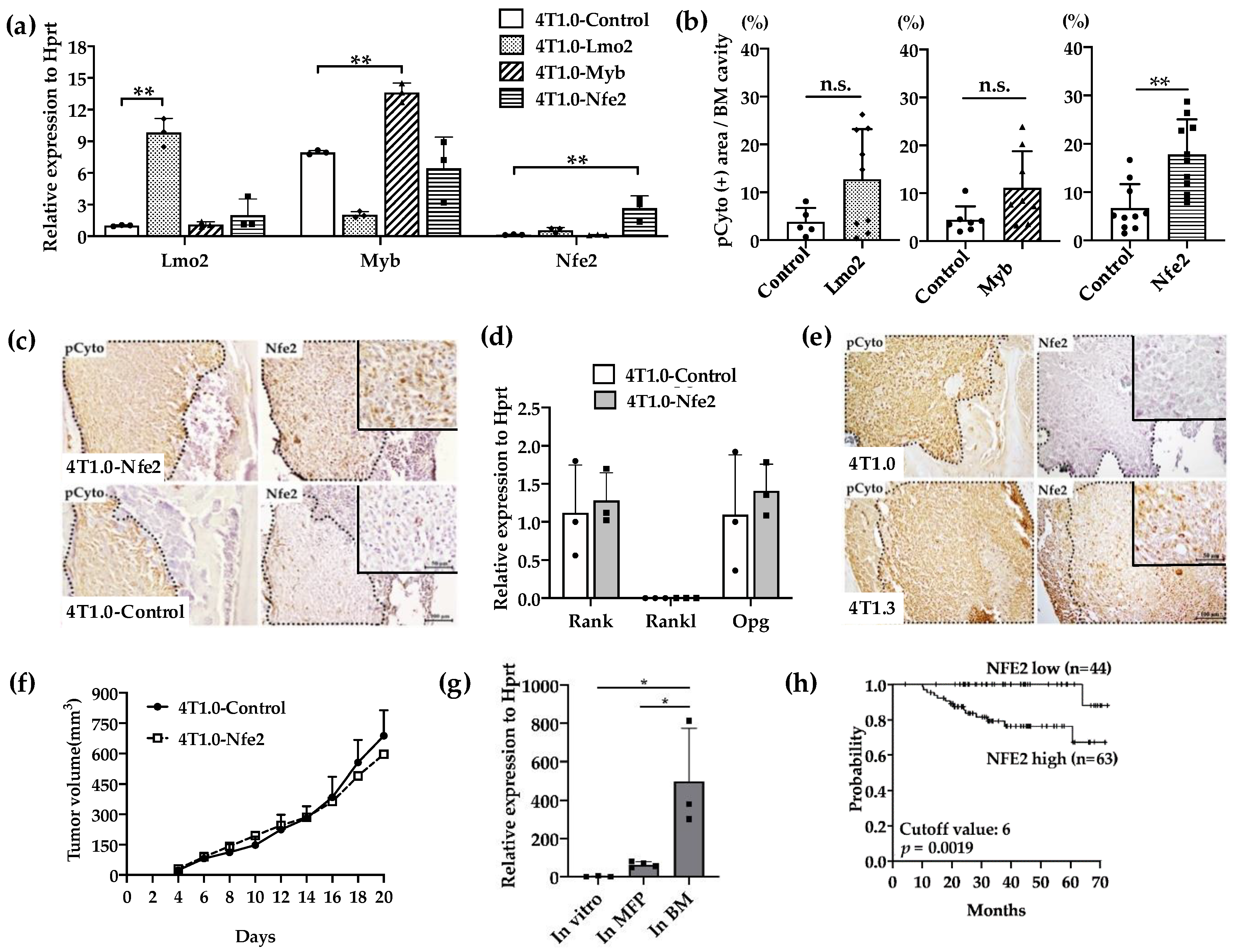
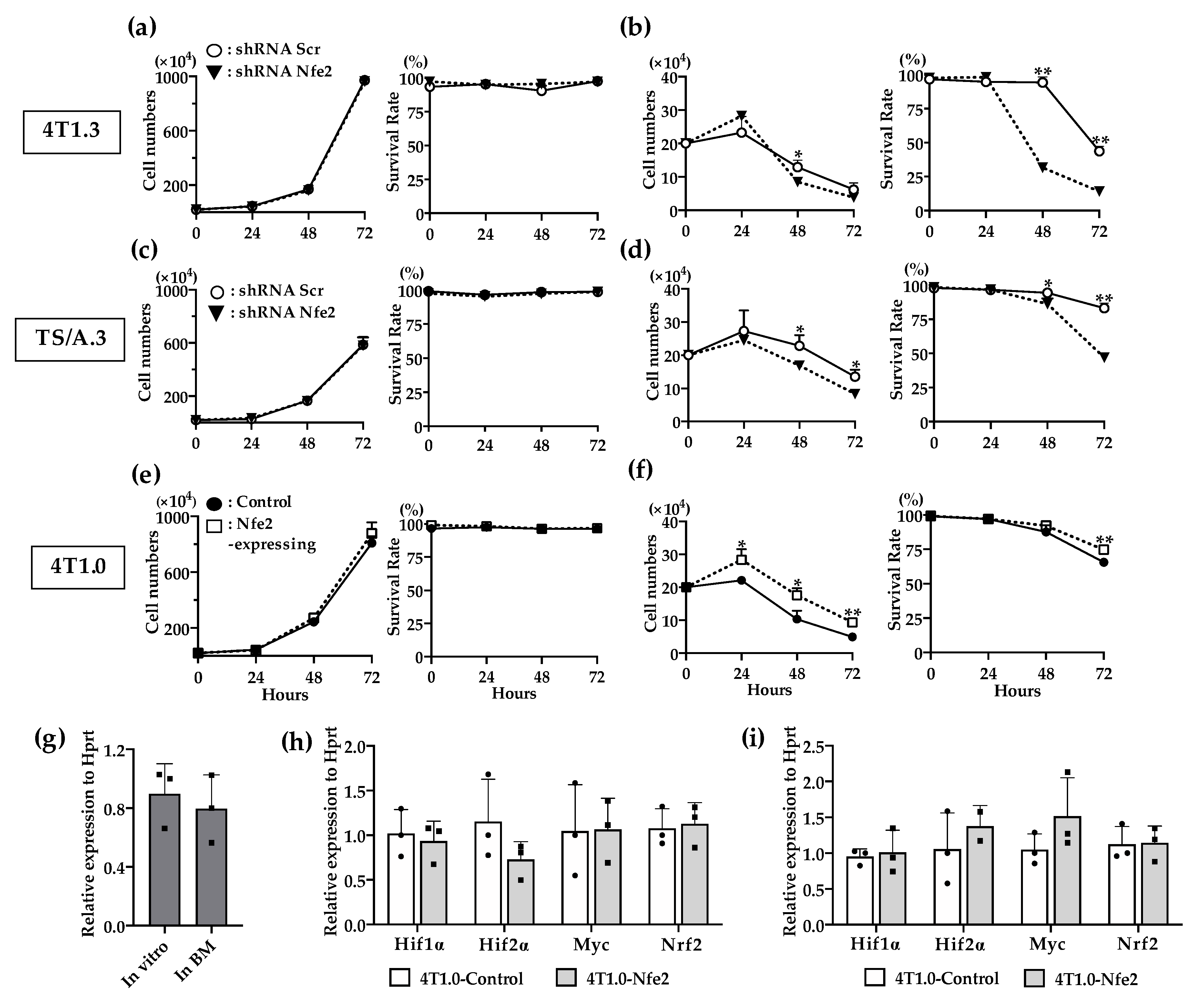
2.2. Enhanced Intraosseous Growth by Nfe2-Expressing Breast Cancer Cells
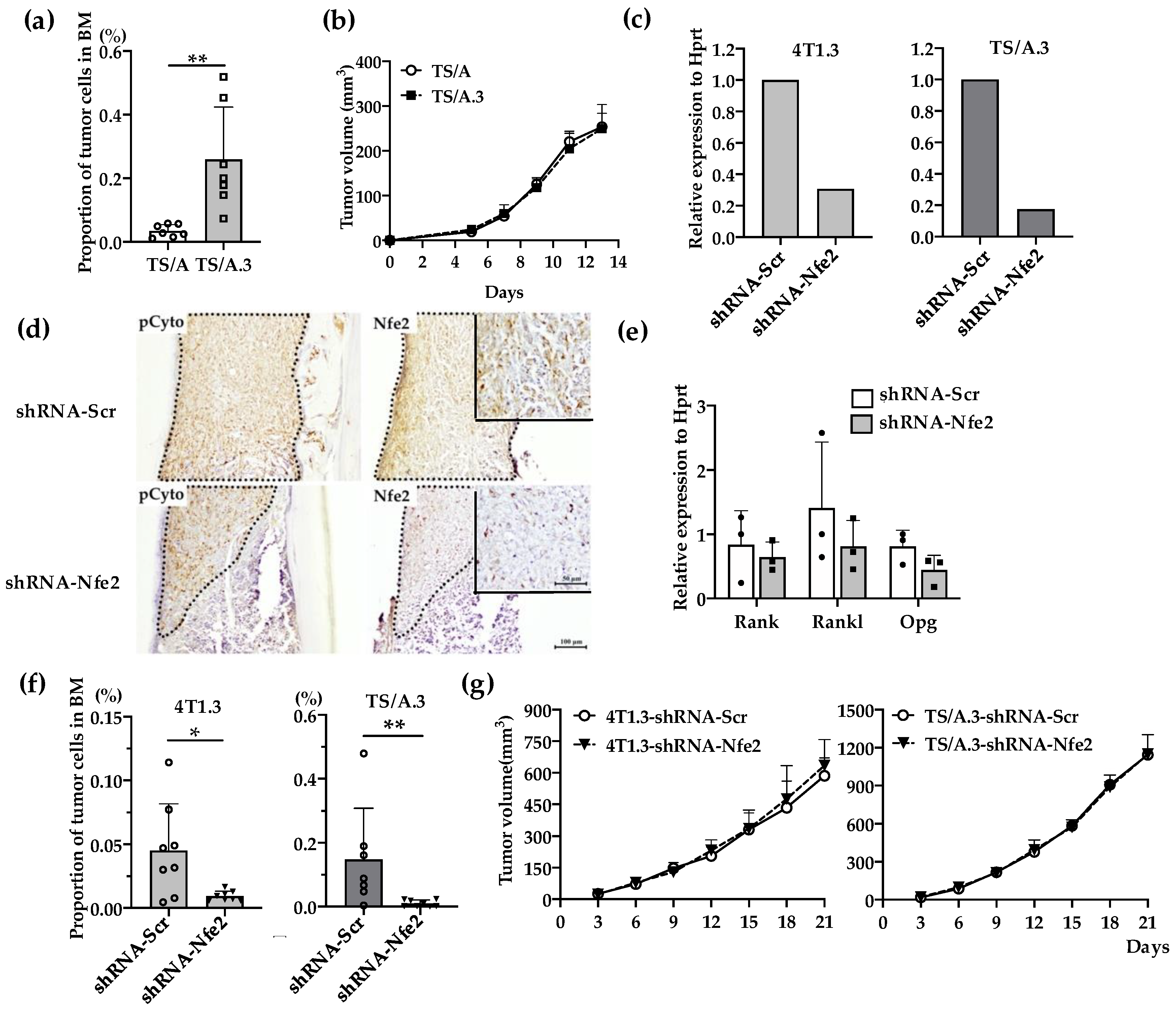
2.3. Reduced Intraosseous Growth of Breast Cancer Cells by Nfe2 Expression Ablation
2.4. Contribution of NFE2 to Breast Cancer Cell Survival under Hypoxic and Anchorage-Independent Conditions
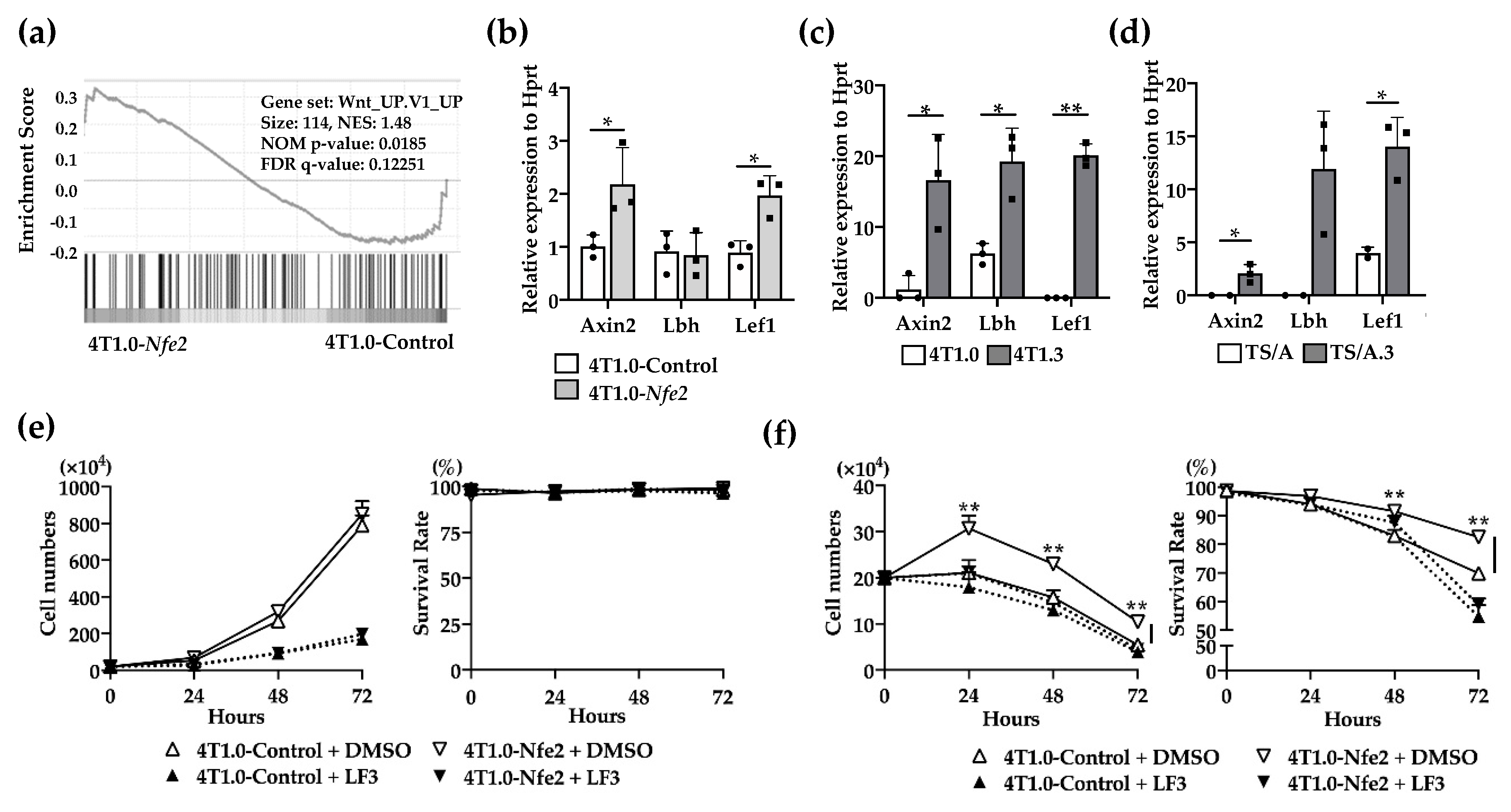
2.5. Wnt Pathway Activation in Nfe2-Mediated Enhanced Intraosseous Tumor Formation
3. Discussion
4. Materials and Methods
4.1. Cell Lines
4.2. Mice
4.3. Antibodies
4.4. RNAseq Analysis
4.5. Procedures to Identify Candidate Transcription Factors
4.6. Establishment of Cell Lines Constitutively-Expressing Transcription Factors
4.7. Establishment of Cell Lines Expressing shRNA
4.8. Intraosseous Injection
4.9. In Vitro Cell Proliferation Assay
4.10. Tumor Growth at the Primary Site
4.11. qRT-PCR Analysis
4.12. Clinical Database Analysis
4.13. Library Construction and Sequencing
4.14. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Gene | Species | Size | Forward Primer (5′-3′) | Reverse Primer (3′-5′) |
|---|---|---|---|---|
| Hprt | mouse | 90 | TCCTCCTCAGACCGCTTTT | CCTGGTTCATCATCGCTAATC |
| Myb | mouse | 79 | GCTGGAGTTGCTCCTGATGT | GCTGCAAGTGTGGTTCTGTG |
| Nfe2 | mouse | 126 | GTACTCAGAGGCAGCGCTCA | CAACCTTTCAGGCACCTGTGG |
| Lmo2 | mouse | 70 | GCAGCTGGATGATTCGCTCT | CCTCCACGCTCAAGGACAGT |
| App | mouse | 167 | CCCAAGGCCTCATCATGTGT | GCTCGTAGATCACACGGAGG |
| Ets1 | mouse | 175 | CGGTCAGCGGGAATTTGAGA | TGATGGTGAGAGTCGGCTTG |
| Sf1 | mouse | 135 | CCATGCAGCACAACCCAAAT | AGGCGTACTTCCCAGGTACT |
| Pbx1 | mouse | 132 | TGTCACAGCCACCAATGTGT | TTGAGTGACTGCACGCTCAT |
| Max | mouse | 142 | GGCTTGTTGTTGTCGGTGAC | AAACCTCGGTTGCTCTTCGT |
| Nf1 | mouse | 199 | CTTCTTCCTGCGACTGCGTT | TCTGCGACAGACGTCAACAT |
| Gata1 | mouse | 72 | TTGGGATCACCCTGAACTCG | GGTTGAACCTGGGCTTGTTG |
| Gata2 | mouse | 176 | ACCCCTATCCCGTGAATCCG | CCACCTCCATGGTCCACTAC |
| Ar | mouse | 105 | GCTCACCAAGCTCCTGGATT | TCAGGAAAGTCCACGCTCAC |
| Rora | mouse | 170 | GCCGAGGTATCTCAGTCACG | AGGACAGGAGTAGGTGGCAT |
| Axin2 | mouse | 184 | AGCCTGTTTATCCCATCACG | TGAGGCTTCACGTGCATTAG |
| Lbh | mouse | 125 | GATCGGCTGAGATGACCGAG | GCAGCAACGGTCAAAGTCTG |
| Lef1 | mouse | 165 | CGGGAAGAGCAGGCCAAATA | AGCTGTCATTCTGGGACCTG |
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Dafni, U.; Tsourti, Z.; Alatsathianos, I. Breast cancer statistics in the european union: Incidence and survival across european countries. Breast Care 2019, 14, 344–353. [Google Scholar] [CrossRef]
- Body, J.J.; Quinn, G.; Talbot, S.; Booth, E.; Demonty, G.; Taylor, A.; Amelio, J. Systematic review and meta-analysis on the proportion of patients with breast cancer who develop bone metastases. Crit. Rev. Oncol. Hematol. 2017, 115, 67–80. [Google Scholar] [CrossRef] [PubMed]
- Maurizi, A.; Rucci, N. The Osteoclast in Bone Metastasis: Player and Target. Cancers 2018, 10. [Google Scholar] [CrossRef] [PubMed]
- Coleman, R.; Gnant, M.; Morgan, G.; Clezardin, P. Effects of bone-targeted agents on cancer progression and mortality. J. Natl. Cancer Inst. 2012, 104, 1059–1067. [Google Scholar] [CrossRef] [PubMed]
- Fidler, I.J.; Ellis, L.M. The implications of angiogenesis for the biology and therapy of cancer metastasis. Cell 1994, 79, 185–188. [Google Scholar] [CrossRef]
- Langley, R.R.; Fidler, I.J. The seed and soil hypothesis revisited--the role of tumor-stroma interactions in metastasis to different organs. Int. J. Cancer. J. Int. Du Cancer 2011, 128, 2527–2535. [Google Scholar] [CrossRef]
- Kang, Y.; Siegel, P.M.; Shu, W.; Drobnjak, M.; Kakonen, S.M.; Cordón-Cardo, C.; Guise, T.A.; Massagué, J. A multigenic program mediating breast cancer metastasis to bone. Cancer Cell 2003, 3, 537–549. [Google Scholar] [CrossRef]
- Xia, T.S.; Wang, J.; Yin, H.; Ding, Q.; Zhang, Y.F.; Yang, H.W.; Liu, X.A.; Dong, M.; Du, Q.; Ling, L.J.; et al. Human tissue-specific microenvironment: An essential requirement for mouse models of breast cancer. Oncol. Rep. 2010, 24, 203–211. [Google Scholar] [CrossRef]
- Sasaki, S.; Baba, T.; Nishimura, T.; Hayakawa, Y.; Hashimoto, S.; Gotoh, N.; Mukaida, N. Essential roles of the interaction between cancer cell-derived chemokine, CCL4, and intra-bone CCR5-expressing fibroblasts in breast cancer bone metastasis. Cancer Lett. 2016, 378, 23–32. [Google Scholar] [CrossRef]
- Vishal, M.; Swetha, R.; Thejaswini, G.; Arumugam, B.; Selvamurugan, N. Role of Runx2 in breast cancer-mediated bone metastasis. Int. J. Biol. Macromol. 2017, 99, 608–614. [Google Scholar] [CrossRef] [PubMed]
- Davudian, S.; Mansoori, B.; Shajari, N.; Mohammadi, A.; Baradaran, B. BACH1, the master regulator gene: A novel candidate target for cancer therapy. Gene 2016, 588, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Gasiorek, J.J.; Blank, V. Regulation and function of the NFE2 transcription factor in hematopoietic and non-hematopoietic cells. Cell. Mol. Life Sci. 2015, 72, 2323–2335. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, K.B.; Grunder, A.; Hadlich, T.; Wehrle, J.; Gothwal, M.; Bogeska, R.; Seeger, T.S.; Kayser, S.; Pham, K.B.; Jutzi, J.S.; et al. A novel murine model of myeloproliferative disorders generated by overexpression of the transcription factor NF-E2. J. Exp. Med. 2012, 209, 35–50. [Google Scholar] [CrossRef]
- Jutzi, J.S.; Bogeska, R.; Nikoloski, G.; Schmid, C.A.; Seeger, T.S.; Stegelmann, F.; Schwemmers, S.; Grunder, A.; Peeken, J.C.; Gothwal, M.; et al. MPN patients harbor recurrent truncating mutations in transcription factor NF-E2. J. Exp. Med. 2013, 210, 1003–1019. [Google Scholar] [CrossRef]
- Peeken, J.C.; Jutzi, J.S.; Wehrle, J.; Koellerer, C.; Staehle, H.F.; Becker, H.; Schoenwandt, E.; Seeger, T.S.; Schanne, D.H.; Gothwal, M.; et al. Epigenetic regulation of NFE2 overexpression in myeloproliferative neoplasms. Blood 2018, 131, 2065–2073. [Google Scholar] [CrossRef]
- Jutzi, J.S.; Basu, T.; Pellmann, M.; Kaiser, S.; Steinemann, D.; Sanders, M.A.; Hinai, A.S.A.; Zeilemaker, A.; Bojtine Kovacs, S.; Koellerer, C.; et al. Altered NFE2 activity predisposes to leukemic transformation and myelosarcoma with AML-specific aberrations. Blood 2019, 133, 1766–1777. [Google Scholar] [CrossRef]
- Spencer, J.A.; Ferraro, F.; Roussakis, E.; Klein, A.; Wu, J.; Runnels, J.M.; Zaher, W.; Mortensen, L.J.; Alt, C.; Turcotte, R.; et al. Direct measurement of local oxygen concentration in the bone marrow of live animals. Nature 2014, 508, 269–273. [Google Scholar] [CrossRef]
- Weilbaecher, K.N.; Guise, T.A.; McCauley, L.K. Cancer to bone: A fatal attraction. Nat. Rev. Cancer 2011, 11, 411–425. [Google Scholar] [CrossRef]
- Li, X.Q.; Lu, J.T.; Tan, C.C.; Wang, Q.S.; Feng, Y.M. RUNX2 promotes breast cancer bone metastasis by increasing integrin α5-mediated colonization. Cancer Lett. 2016, 380, 78–86. [Google Scholar] [CrossRef]
- Kim, B.; Kim, H.; Jung, S.; Moon, A.; Noh, D.Y.; Lee, Z.H.; Kim, H.J.; Kim, H.H. A CTGF-RUNX2-RANKL Axis in Breast and Prostate Cancer Cells Promotes Tumor Progression in Bone. J. Bone Miner. Res. 2020, 35, 155–166. [Google Scholar] [CrossRef] [PubMed]
- Mignotte, V.; Wall, L.; Deboer, E.; Grosveld, F.; Romeo, P.H. Two tissue-specific factors bind the erythroid promoter of the human porphobilinogen deaminase gene. Nucleic Acids Res. 1989, 17, 37–54. [Google Scholar] [CrossRef] [PubMed]
- Andrews, N.C.; Kotkow, K.J.; Ney, P.A.; Erdjument-Bromage, H.; Tempst, P.; Orkin, S.H. The ubiquitous subunit of erythroid transcription factor NF-E2 is a small basic-leucine zipper protein related to the v-maf oncogene. Proc. Natl. Acad. Sci. USA 1993, 90, 11488–11492. [Google Scholar] [CrossRef] [PubMed]
- Andrews, N.C.; Erdjument-Bromage, H.; Davidson, M.B.; Tempst, P.; Orkin, S.H. Erythroid transcription factor NF-E2 is a haematopoietic-specific basic-leucine zipper protein. Nature 1993, 362, 722–728. [Google Scholar] [CrossRef]
- Mignotte, V.; Eleouet, J.F.; Raich, N.; Romeo, P.H. Cis- and trans-acting elements involved in the regulation of the erythroid promoter of the human porphobilinogen deaminase gene. Proc. Natl. Acad. Sci. USA 1989, 86, 6548–6552. [Google Scholar] [CrossRef]
- Loyd, M.R.; Okamoto, Y.; Randall, M.S.; Ney, P.A. Role of AP1/NFE2 binding sites in endogenous alpha-globin gene transcription. Blood 2003, 102, 4223–4228. [Google Scholar] [CrossRef]
- Onishi, Y.; Kiyama, R. Interaction of NF-E2 in the human β-globin locus control region before chromatin remodeling. J. Biol. Chem. 2003, 278, 8163–8171. [Google Scholar] [CrossRef]
- Shivdasani, R.A.; Orkin, S.H. Erythropoiesis and globin gene expression in mice lacking the transcription factor NF-E2. Proc. Natl. Acad. Sci. USA 1995, 92, 8690–8694. [Google Scholar] [CrossRef]
- Lecine, P.; Villeval, J.L.; Vyas, P.; Swencki, B.; Xu, Y.; Shivdasani, R.A. Mice lacking transcription factor NF-E2 provide in vivo validation of the proplatelet model of thrombocytopoiesis and show a platelet production defect that is intrinsic to megakaryocytes. Blood 1998, 92, 1608–1616. [Google Scholar] [CrossRef]
- Ney, P.A.; Andrews, N.C.; Jane, S.M.; Safer, B.; Purucker, M.E.; Weremowicz, S.; Morton, C.C.; Goff, S.C.; Orkin, S.H.; Nienhuis, A.W. Purification of the human NF-E2 complex: cDNA cloning of the hematopoietic cell-specific subunit and evidence for an associated partner. Mol. Cell Biol. 1993, 13, 5604–5612. [Google Scholar] [CrossRef]
- Toki, T.; Itoh, J.; Arai, K.; Kitazawa, J.; Yokoyama, M.; Igarashi, K.; Yamamoto, M.; Ito, E. Abundant expression of erythroid transcription factor P45 NF-E2 mRNA in human peripheral granurocytes. Biochem. Biophys. Res. Commun. 1996, 219, 760–765. [Google Scholar] [CrossRef]
- Zhong, Z.; Yu, J.; Virshup, D.M.; Madan, B. Wnts and the hallmarks of cancer. Cancer Metastasis Rev. 2020. [Google Scholar] [CrossRef]
- Taguchi, K.; Yamamoto, M. The KEAP1-NRF2 System in Cancer. Front. Oncol. 2017, 7, 85. [Google Scholar] [CrossRef]
- Ohta, T.; Iijima, K.; Miyamoto, M.; Nakahara, I.; Tanaka, H.; Ohtsuji, M.; Suzuki, T.; Kobayashi, A.; Yokota, J.; Sakiyama, T.; et al. Loss of Keap1 function activates Nrf2 and provides advantages for lung cancer cell growth. Cancer Res. 2008, 68, 1303–1309. [Google Scholar] [CrossRef]
- Moi, P.; Chan, K.; Asunis, I.; Cao, A.; Kan, Y.W. Isolation of NF-E2-related factor 2 (Nrf2), a NF-E2-like basic leucine zipper transcriptional activator that binds to the tandem NF-E2/AP1 repeat of the β-globin locus control region. Proc. Natl. Acad. Sci. USA 1994, 91, 9926–9930. [Google Scholar] [CrossRef]
- Itoh, K.; Chiba, T.; Takahashi, S.; Ishii, T.; Igarashi, K.; Katoh, Y.; Oyake, T.; Hayashi, N.; Satoh, K.; Hatayama, I.; et al. An Nrf2/small Maf heterodimer mediates the induction of phase II detoxifying enzyme genes through antioxidant response elements. Biochem. Biophys. Res. Commun. 1997, 236, 313–322. [Google Scholar] [CrossRef]
- Hirotsu, Y.; Katsuoka, F.; Funayama, R.; Nagashima, T.; Nishida, Y.; Nakayama, K.; Douglas Engel, J.; Yamamoto, M. Nrf2-MafG heterodimers contribute globally to antioxidant and metabolic networks. Nucleic Acids Res. 2012, 40, 10228–10239. [Google Scholar] [CrossRef]
- Gong, X.; Yi, J.; Carmon, K.S.; Crumbley, C.A.; Xiong, W.; Thomas, A.; Fan, X.; Guo, S.; An, Z.; Chang, J.T.; et al. Aberrant RSPO3-LGR4 signaling in Keap1-deficient lung adenocarcinomas promotes tumor aggressiveness. Oncogene 2015, 34, 4692–4701. [Google Scholar] [CrossRef]
- Manigandan, K.; Manimaran, D.; Jayaraj, R.L.; Elangovan, N.; Dhivya, V.; Kaphle, A. Taxifolin curbs NF-κB-mediated Wnt/β-catenin signaling via up-regulating Nrf2 pathway in experimental colon carcinogenesis. Biochimie 2015, 119, 103–112. [Google Scholar] [CrossRef]
- Mignotte, V.; Navarro, S.; Eleouet, J.F.; Zon, L.I.; Romeo, P.H. The extinction of erythroid genes after tetradecanoylphorbol acetate treatment of erythroleukemic cells correlates with down-regulation of the tissue-specific factors NF-E1 and NF-E2. J. Biol. Chem. 1990, 265, 22090–22092. [Google Scholar]
- Cosphiadi, I.; Atmakusumah, T.D.; Siregar, N.C.; Muthalib, A.; Harahap, A.; Mansyur, M. Bone Metastasis in Advanced Breast Cancer: Analysis of Gene Expression Microarray. Clin. Breast Cancer 2018, 18, e1117–e1122. [Google Scholar] [CrossRef]
- Singh, A.; Venkannagari, S.; Oh, K.H.; Zhang, Y.Q.; Rohde, J.M.; Liu, L.; Nimmagadda, S.; Sudini, K.; Brimacombe, K.R.; Gajghate, S.; et al. Small molecule inhibitor of NRF2 selectively intervenes therapeutic resistance in KEAP1-deficient NSCLC tumors. ACS Chem. Biol. 2016, 11, 3214–3225. [Google Scholar] [CrossRef]
- Pratap, J.; Wixted, J.J.; Gaur, T.; Zaidi, S.K.; Dobson, J.; Gokul, K.D.; Hussain, S.; Van Wijnen, A.J.; Stein, J.L.; Stein, G.S.; et al. Runx2 transcriptional activation of Indian Hedgehog and a downstream bone metastatic pathway in breast cancer cells. Cancer Res. 2008, 68, 7795–7802. [Google Scholar] [CrossRef]
- Glembotsky, A.C.; Bluteau, D.; Espasandin, Y.R.; Goette, N.P.; Marta, R.F.; Marin Oyarzun, C.P.; Korin, L.; Lev, P.R.; Laguens, R.P.; Molinas, F.C.; et al. Mechanisms underlying platelet function defect in a pedigree with familial platelet disorder with a predisposition to acute myelogenous leukemia: Potential role for candidate RUNX1 targets. J. Thromb. Haemost. 2014, 12, 761–772. [Google Scholar] [CrossRef]
- Lee, W.H.; Chung, M.H.; Tsai, Y.H.; Chang, J.L.; Huang, H.M. Interferon-γ suppresses activin A/NF-E2 induction of erythroid gene expression through the NF-κB/c-Jun pathway. Am. J. Physiol. Cell Physiol. 2014, 306, C407–C414. [Google Scholar] [CrossRef]
- Chui, C.M.; Li, K.; Yang, M.; Chuen, C.K.; Fok, T.F.; Li, C.K.; Yuen, P.M. Platelet-derived growth factor up-regulates the expression of transcription factors NF-E2, GATA-1 and c-Fos in megakaryocytic cell lines. Cytokine 2003, 21, 51–64. [Google Scholar] [CrossRef]
- Lollini, P.L.; de Giovanni, C.; Eusebi, V.; Nicoletti, G.; Prodi, G.; Nanni, P. High-metastatic clones selected in vitro from a recent spontaneous BALB/c mammary adenocarcinoma cell line. Clin. Exp. Metastasis 1984, 2, 251–259. [Google Scholar] [CrossRef]
- Mootha, V.K.; Lindgren, C.M.; Eriksson, K.F.; Subramanian, A.; Sihag, S.; Lehar, J.; Puigserver, P.; Carlsson, E.; Ridderstråle, M.; Laurila, E.; et al. PGC-1alpha-responsive genes involved in oxidative phosphorylation are coordinately downregulated in human diabetes. Nat. Genet. 2003, 34, 267–273. [Google Scholar] [CrossRef]
- Reich, M.; Liefeld, T.; Gould, J.; Lerner, J.; Tamayo, P.; Mesirov, J.P. GenePattern 2.0. Nat. Genet. 2006, 38, 500–501. [Google Scholar] [CrossRef]
- Subramanian, A.; Tamayo, P.; Mootha, V.K.; Mukherjee, S.; Ebert, B.L.; Gillette, M.A.; Paulovich, A.; Pomeroy, S.L.; Golub, T.R.; Lander, E.S.; et al. Gene set enrichment analysis: A knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl. Acad. Sci. USA 2005, 102, 15545–15550. [Google Scholar] [CrossRef]
- Baba, T.; Naka, K.; Morishita, S.; Komatsu, N.; Hirao, A.; Mukaida, N. MIP-1alpha/CCL3-mediated maintenance of leukemia-initiating cells in the initiation process of chronic myeloid leukemia. J. Exp. Med. 2013, 210, 2661–2673. [Google Scholar] [CrossRef]
- Sasaki, S.; Baba, T.; Shinagawa, K.; Matsushima, K.; Mukaida, N. Crucial involvement of the CCL3-CCR5 axis-mediated fibroblast accumulation in colitis-associated carcinogenesis in mice. Int. J. Cancer 2014, 135, 1297–1306. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, D.; Iwabuchi, S.; Baba, T.; Hashimoto, S.-i.; Mukaida, N.; Sasaki, S.-i. Involvement of a Transcription factor, Nfe2, in Breast Cancer Metastasis to Bone. Cancers 2020, 12, 3003. https://doi.org/10.3390/cancers12103003
Zhang D, Iwabuchi S, Baba T, Hashimoto S-i, Mukaida N, Sasaki S-i. Involvement of a Transcription factor, Nfe2, in Breast Cancer Metastasis to Bone. Cancers. 2020; 12(10):3003. https://doi.org/10.3390/cancers12103003
Chicago/Turabian StyleZhang, Di, Sadahiro Iwabuchi, Tomohisa Baba, Shin-ichi Hashimoto, Naofumi Mukaida, and So-ichiro Sasaki. 2020. "Involvement of a Transcription factor, Nfe2, in Breast Cancer Metastasis to Bone" Cancers 12, no. 10: 3003. https://doi.org/10.3390/cancers12103003
APA StyleZhang, D., Iwabuchi, S., Baba, T., Hashimoto, S.-i., Mukaida, N., & Sasaki, S.-i. (2020). Involvement of a Transcription factor, Nfe2, in Breast Cancer Metastasis to Bone. Cancers, 12(10), 3003. https://doi.org/10.3390/cancers12103003






