Aptamer-Conjugated Superparamagnetic Ferroarabinogalactan Nanoparticles for Targeted Magnetodynamic Therapy of Cancer
Abstract
1. Introduction
2. Results and Discussion
2.1. Production of Different Compositions of Superparamagnetic FeAG
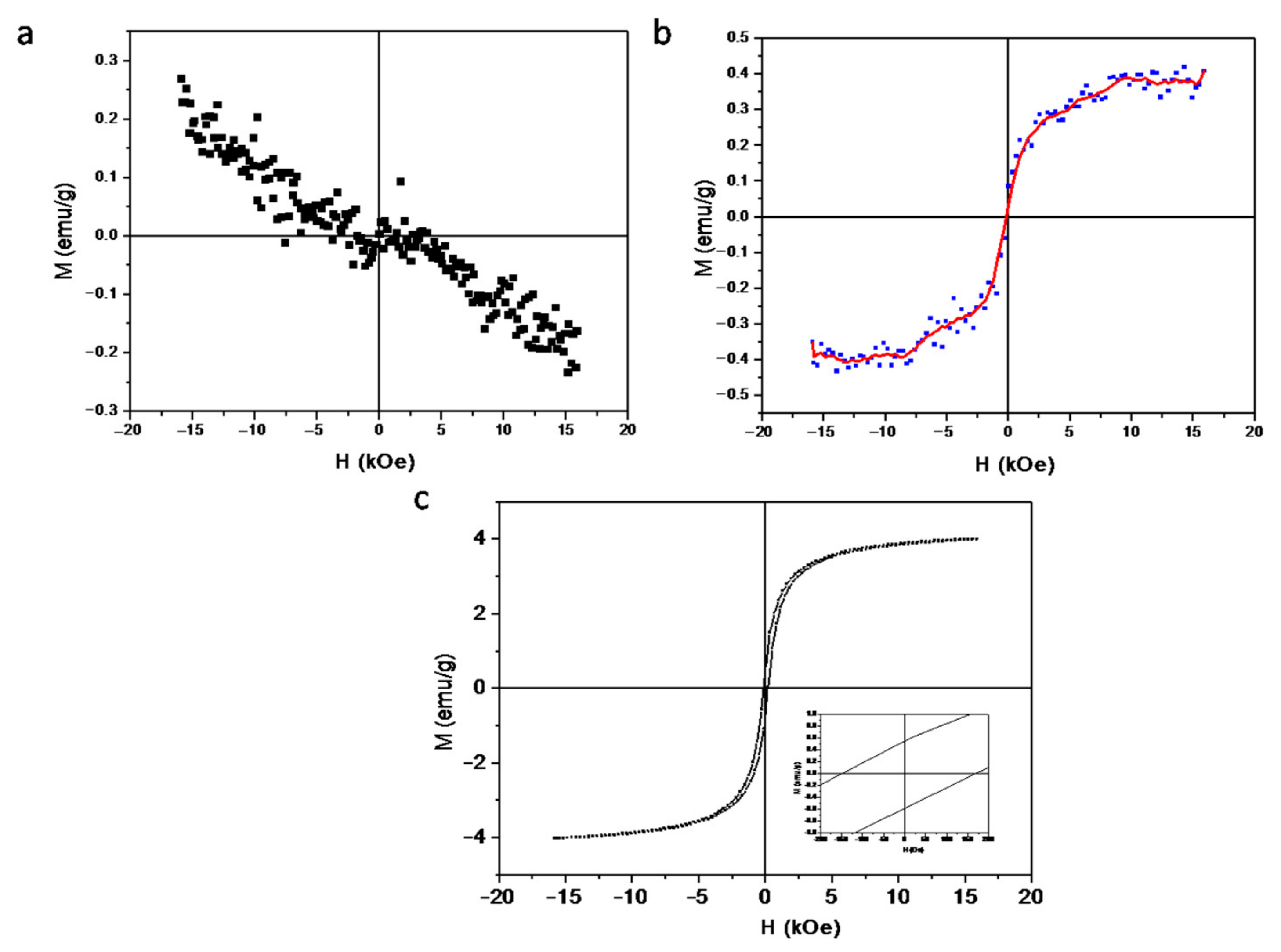
2.2. Magnetic Characteristics of FeAG
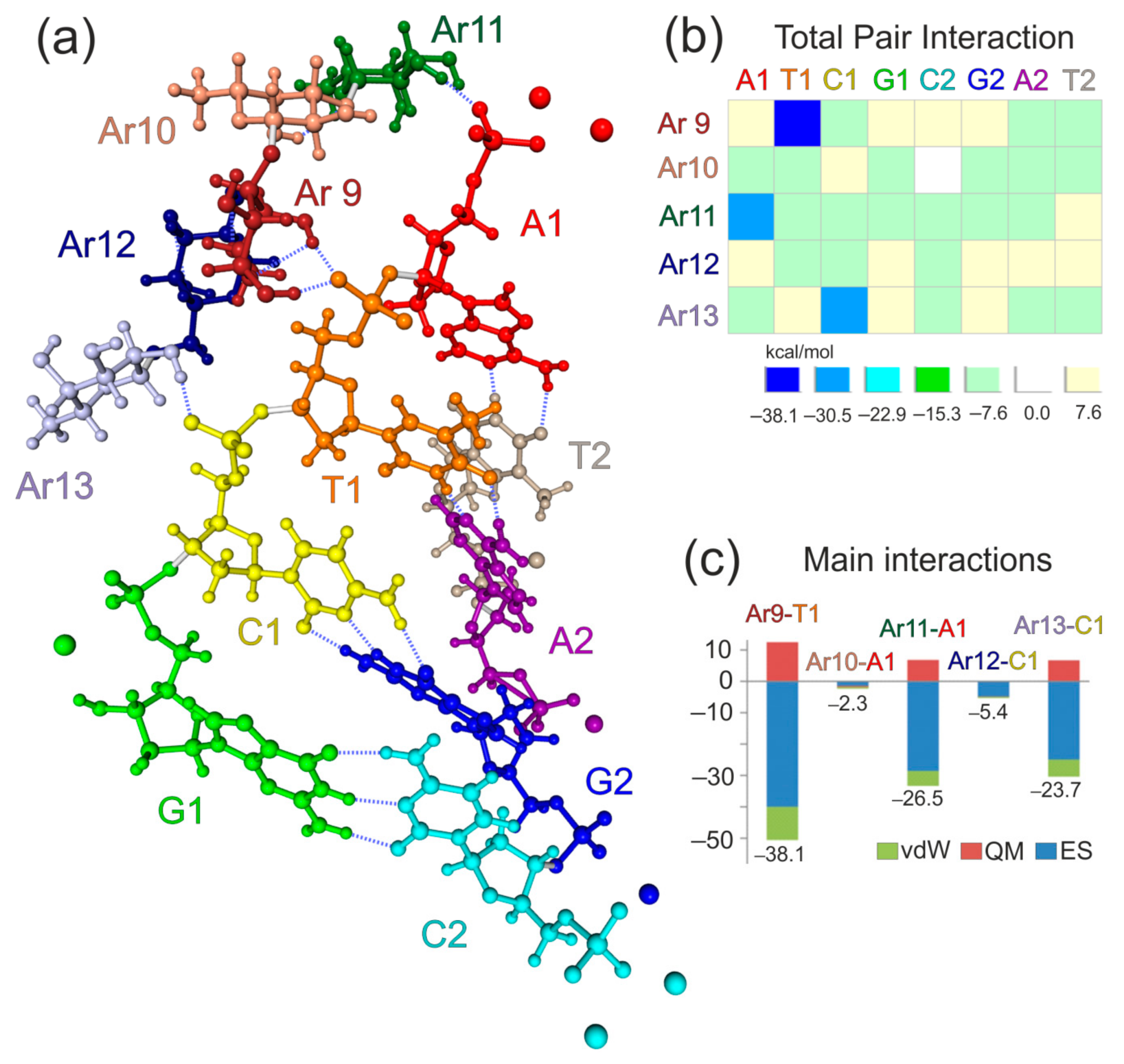
2.3. Conjugation of FeAG with Aptamers
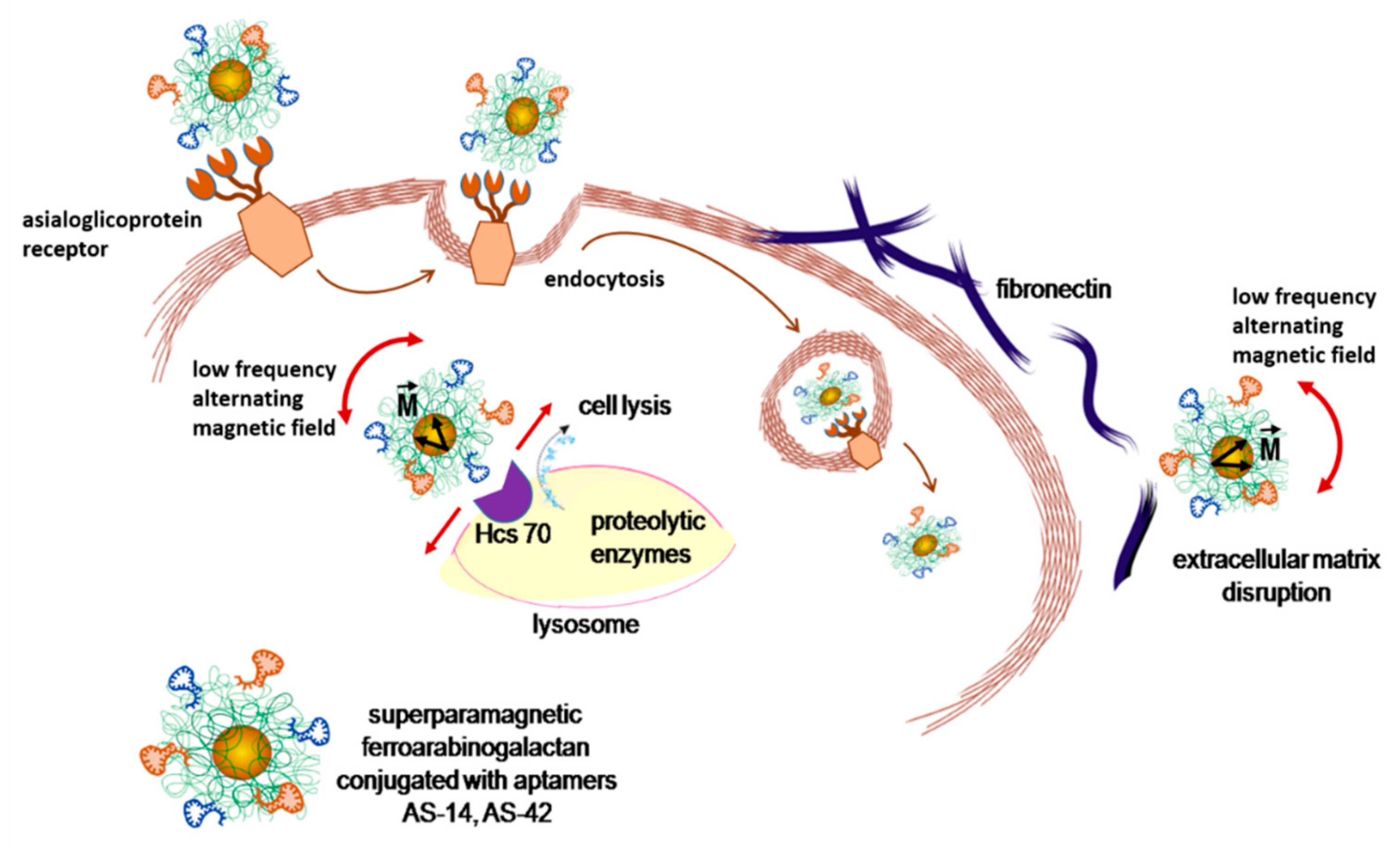
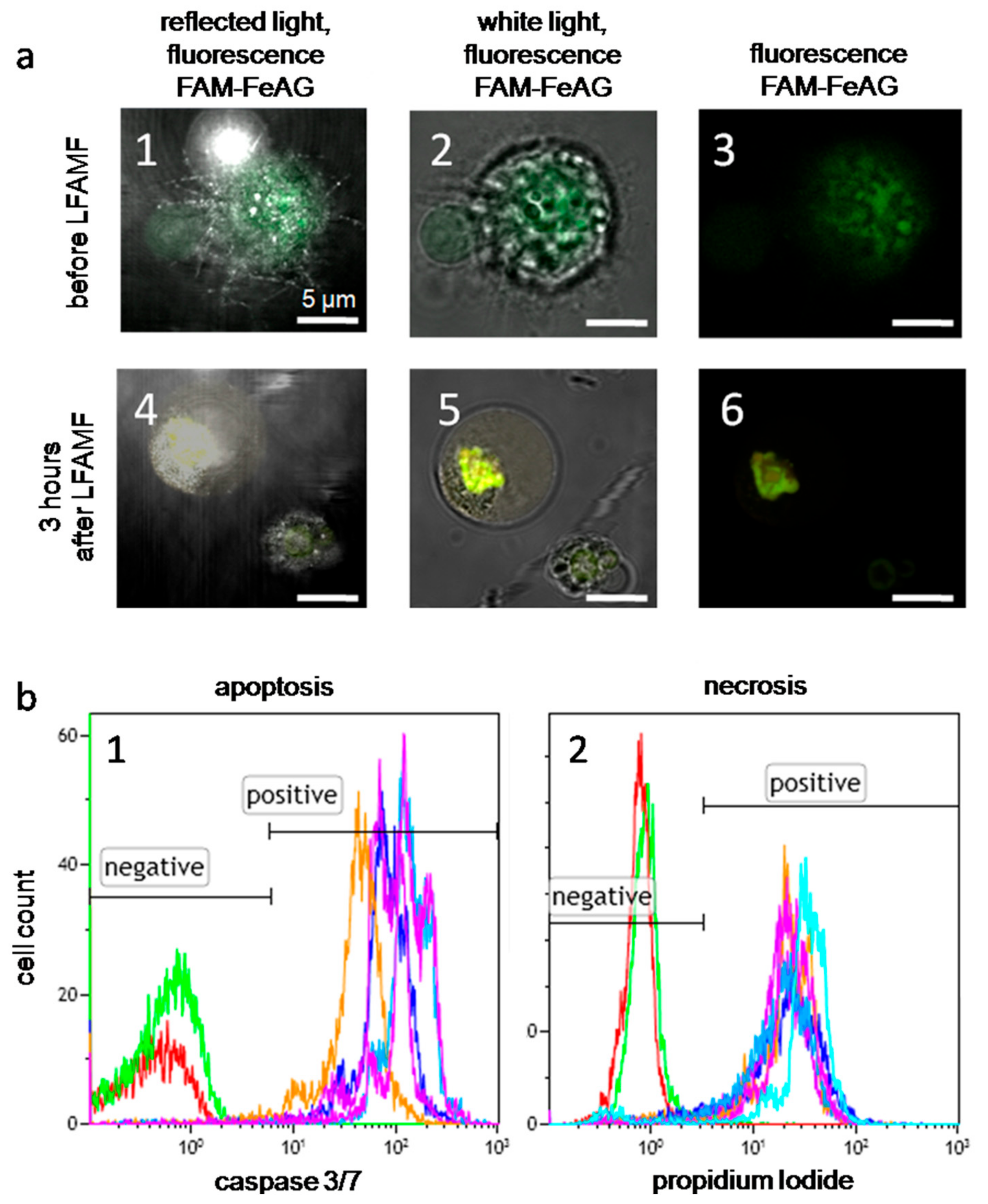
2.4. Effects of AS-FeAG on Carcinoma Cells in Vitro
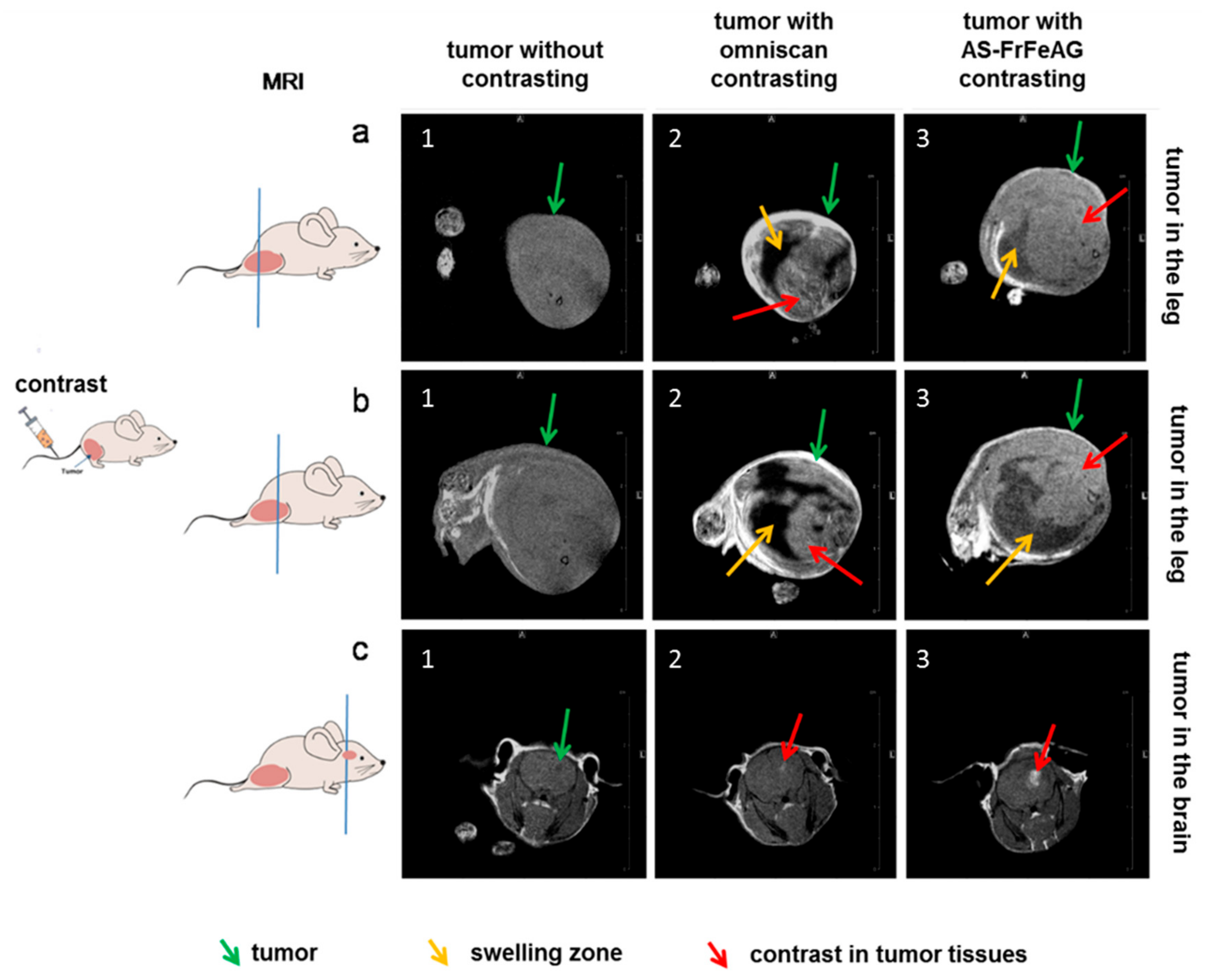
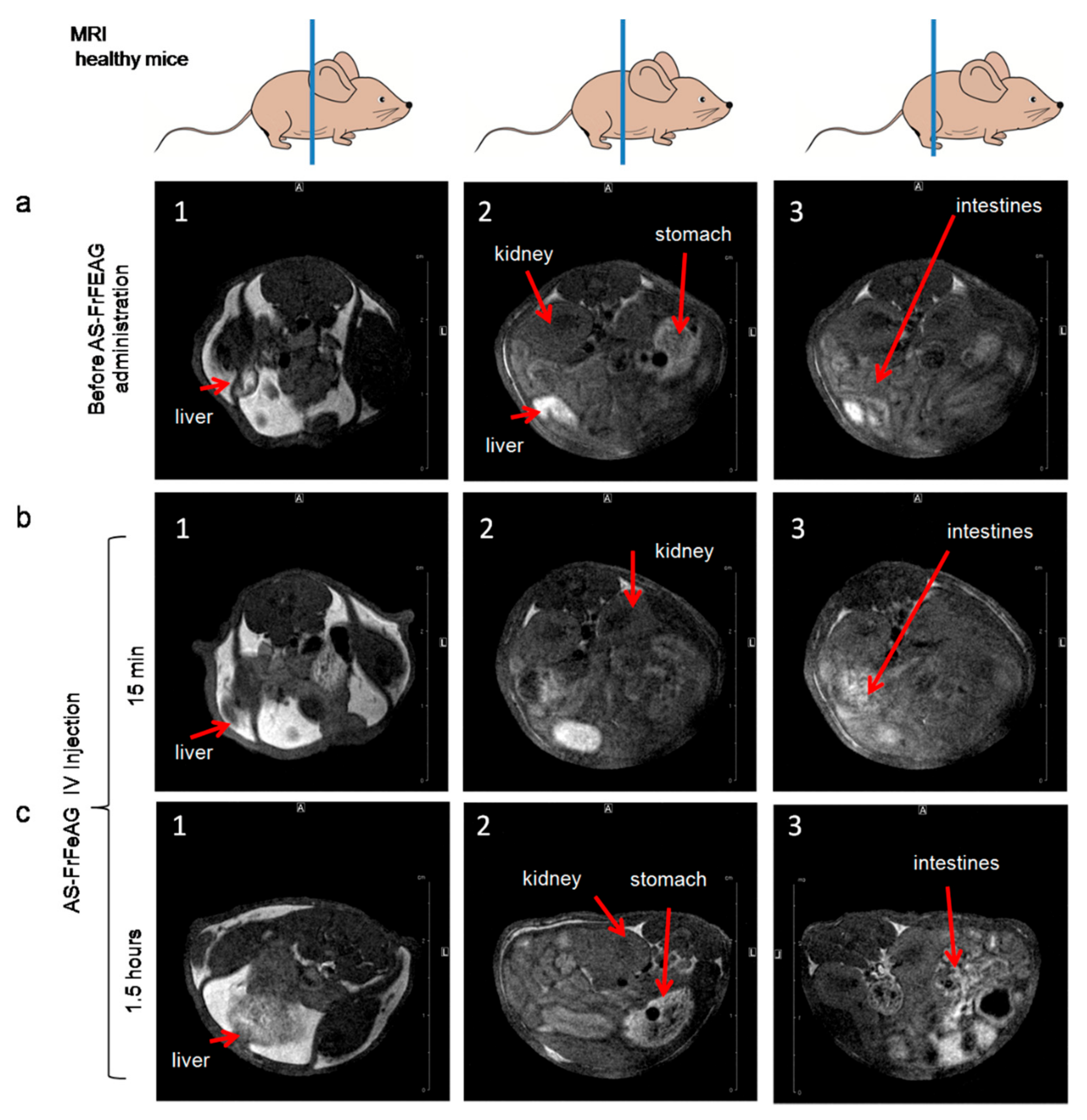
2.5. Magnetic Resonance Imaging of Carcinoma with AS-FeAG In Vivo
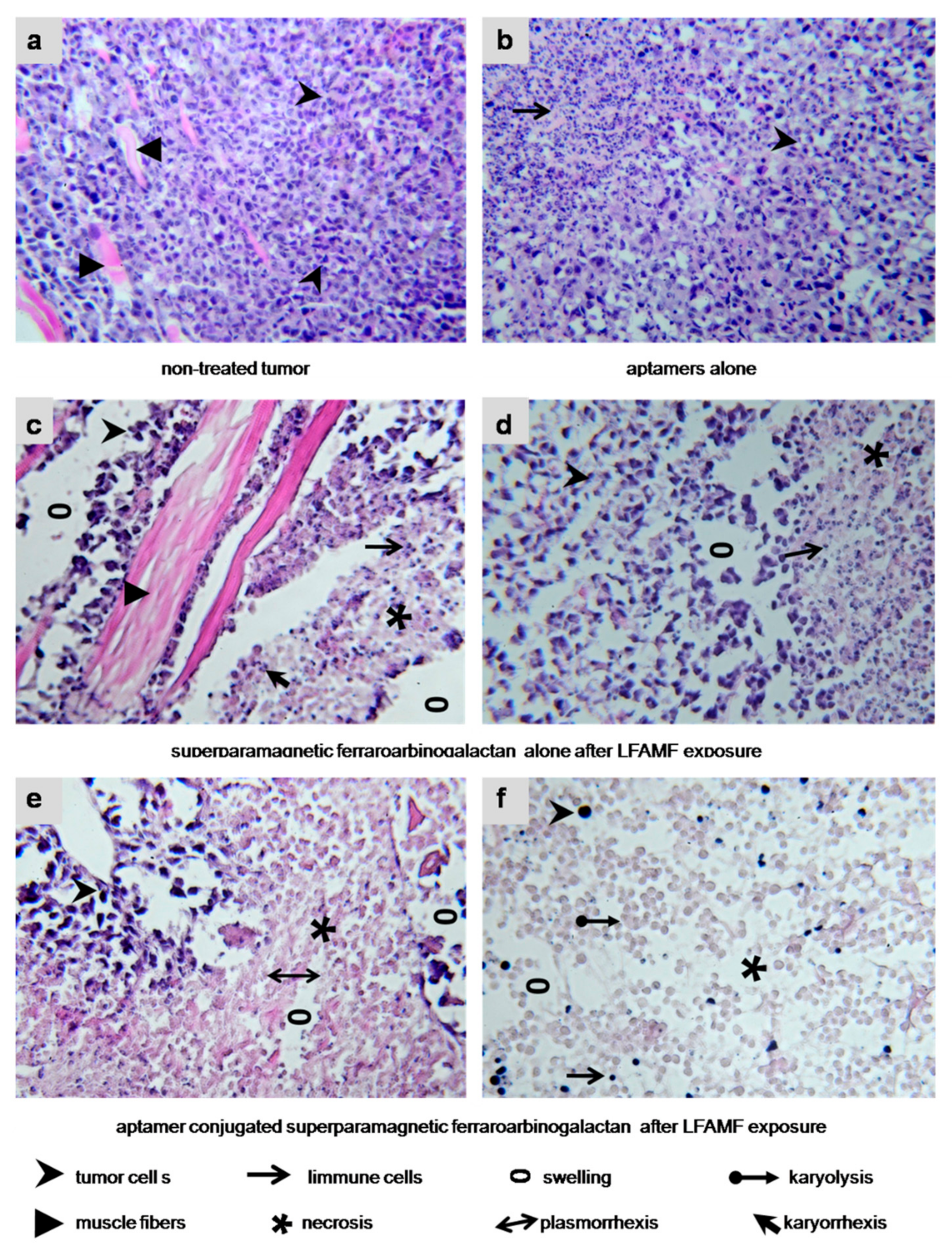
2.6. Effects of AS-FeAG on Carcinoma In Vivo
3. Methods
3.1. Production of Superparamagnetic FeAG
3.2. Conjugating FeAG with Aptamers
3.3. Molecular Modeling of AG Interaction with an Aptamer
3.4. Flow Cytometry Analyses of Cells Treated with AS-FeAG in LFAMF
3.5. Generation of LowFrequency Magnetic Field
3.6. Ethics Committee Approval
3.7. Mice Tumor Models
3.7.1. Solid Tumor in the Leg
3.7.2. Solid Tumor in the Brain
3.8. In Vivo Treatments with AS-FeAG in LFAMF
- Group 1: Untreated control;
- Group 2: Injection of the aptamer mix of AS-14 and AS-42 in 100 μL DPBS (400 μg/kg);
- Group 3: Injection of FrFeAG (6%) in 100 μL DPBS (1.6 μg/kg);
- Group 4: Injection of the aptamer mix (AS-14, AS-42) conjugated with FrFeAG (6%) in 100 μL DPBS (0.8 μg/kg);
3.9. Magnetic Resonance Imaging
3.10. Histological Analysis of Tumor Tissues
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Cole, A.J.; Yang, V.C.; David, A.E. Cancer theranostics: The rise of targeted magnetic nanoparticles. Trends Biotechnol. 2011, 29, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Veiseh, O.; Gunn, J.W.; Zhang, M. Design and fabrication of magnetic nanoparticles for targeted drug delivery and imaging. Adv. Drug Deliv. Rev. 2010, 62, 284–304. [Google Scholar] [CrossRef] [PubMed]
- Chu, X.; Yu, J.; Hou, Y.L. Surface modification of magnetic nanoparticles in biomedicine. Chin. Phys. B 2015, 24. [Google Scholar] [CrossRef]
- Corot, C.; Robert, P.; Idee, J.; Port, M. Recent advances in iron oxide nanocrystal technology for medical imaging. Adv. Drug Deliv. Rev. 2006, 58, 1471–1504. [Google Scholar] [CrossRef] [PubMed]
- Angelakeris, M. Magnetic nanoparticles: A multifunctional vehicle for modern theranostics. Biochim. Biophys. Acta Gen. Subj. 2017, 1861, 1642–1651. [Google Scholar] [CrossRef] [PubMed]
- Gobbo, O.L.; Sjaastad, K.; Radomski, M.W.; Volkov, Y.; Prina-Mello, A. Magnetic Nanoparticles in Cancer Theranostics. Theranostics 2015, 5, 1249–1263. [Google Scholar] [CrossRef] [PubMed]
- Mosayebi, J.; Kiyasatfar, M.; Laurent, S. Synthesis, Functionalization, and Design of Magnetic Nanoparticles for Theranostic Applications. Adv. Healthc. Mater. 2017, 6. [Google Scholar] [CrossRef]
- Feoktistova, L.P.; Sapozhnikov, A.N.; Medvedeva, S.A.; Aleksandrova, G.P.; La, G. Radiographic study of iron-containing arabinogalactan derivatives. J. Appl. Chem. 2002, 75, 1951–1954. [Google Scholar]
- Aleksandrova, G.P.; Grishchenko, L.A.; Medvedeva, S.A.; Tikov, A.V.; Feoktistova, L.P.; Sapozhnikov, A.N.; Vakulskaya, T.I.; Tirsky, V.V.; Semenov, A.L.; Martynovich, B.; et al. Synthesis of nanosized particles with magnetic properties for biomedical purposes. Phys. Mesomech. 2004, 7, 139–142. [Google Scholar]
- Aleksandrova, G.P.; Grishchenko, L.A.; Vakulskaya, T.I.; Sukhov, B.G.; Ovcharenko, V.I.; Trofimov, B.A. Magnetic Activity of Nanostructured Hybrid Composites. Electron. J. Phase Transit. Ordered States New Mater. 2009, 4, 1–2. [Google Scholar]
- Sun, H.; Zhu, X.; Lu, P.Y.; Rosato, R.R.; Tan, W.; Zu, Y. Oligonucleotide aptamers: New tools for targeted cancer therapy. Mol. Ther. Nucleic Acids 2014, 3, e182. [Google Scholar] [CrossRef] [PubMed]
- Kruspe, S.; Mittelberger, F.; Szameit, K.; Hahn, U. Aptamers as Drug Delivery Vehicles. ChemMedChem 2014, 9, 1998–2011. [Google Scholar] [CrossRef] [PubMed]
- Kolovskaya, O.S.; Savitskaya, A.G.; Zamay, T.N.; Reshetneva, I.T.; Zamay, G.S.; Erkaev, E.N.; Wang, X.; Wehbe, M.; Salmina, A.B.; Perianova, O.V.; et al. Development of Bacteriostatic DNA Aptamers for Salmonella. J. Med. Chem. 2013, 56, 1564–1572. [Google Scholar] [CrossRef] [PubMed]
- Muharemagic, D.; Labib, M.; Ghobadloo, S.M.; Zamay, A.S.; Bell, J.C.; Berezovski, M.V. Anti-Fab Aptamers for Shielding Virus from Neutralizing Antibodies. J. Am. Chem. Soc. 2012, 134, 17168–17177. [Google Scholar] [CrossRef] [PubMed]
- Muharemagic, D.; Zamay, A.; Ghobadloo, S.M.; Evgin, L.; Savitskaya, A.; Bell, J.C.; Berezovski, M.V. Aptamer-facilitated Protection of Oncolytic Virus from Neutralizing Antibodies. Mol. Ther. Nucleic Acids 2014, 3, e167. [Google Scholar] [CrossRef]
- Zamay, A.S.; Zamay, T.N. Change in physicochemical parameters of membranes of Ehrlich ascite adenocarcinoma in the course of tumor growth. Dokl. Biochem. Biophys. 2005, 402, 197–199. [Google Scholar] [CrossRef]
- Zamay, G.S.; Ivanchenko, T.I.; Zamay, T.N.; Grigorieva, V.L.; Glazyrin, Y.E.; Kolovskaya, O.S.; Garanzha, I.V.; Barinov, A.A.; Krat, A.V.; Mironov, G.G.; et al. DNA Aptamers for the Characterization of Histological Structure of Lung Adenocarcinoma. Mol. Ther. Nucleic Acids 2017, 6, 150–162. [Google Scholar] [CrossRef]
- Zamay, G.S.; Kolovskaya, O.S.; Zamay, T.N.; Glazyrin, Y.E.; Krat, A.V.; Zubkova, O.; Spivak, E.; Wehbe, M.; Gargaun, A.; Muharemagic, D.; et al. Aptamers Selected to Postoperative Lung Adenocarcinoma Detect Circulating Tumor Cells in Human Blood. Mol. Ther. 2015, 23, 1486–1496. [Google Scholar] [CrossRef]
- Kim, D.; Jeong, Y.Y.; Jon, S. A Drug-Loaded Aptamer−Gold Nanoparticle Bioconjugate for Combined CT Imaging and Therapy of Prostate Cancer. ACS Nano 2010, 4, 3689–3696. [Google Scholar] [CrossRef]
- Zhong, Y.N.; Meng, F.H.; Deng, C.; Zhong, Z.Y. Ligand-Directed Active Tumor-Targeting Polymeric Nanoparticles for Cancer Chemotherapy. Biomacromolecules 2014, 15, 1955–1969. [Google Scholar] [CrossRef]
- Engelberg, S.; Modrejewski, J.; Walter, J.G.; Livney, Y.D.; Assaraf, Y.G. Cancer cell-selective, clathrin-mediated endocytosis of aptamer decorated nanoparticles. Oncotarget 2018, 9, 20993–21006. [Google Scholar] [CrossRef] [PubMed]
- Reddy, L.H.; Arias, J.L.; Nicolas, J.; Couvreur, P.; Patrick, C. Magnetic Nanoparticles: Design and Characterization, Toxicity and Biocompatibility, Pharmaceutical and Biomedical Applications. Chem. Rev. 2012, 112, 5818–5878. [Google Scholar] [CrossRef] [PubMed]
- Joshi, M.D.; Patravale, V.B.; Prabhu, R.H. Polymeric nanoparticles for targeted treatment in oncology: Current insights. Int. J. Nanomed. 2015, 10, 1001–1018. [Google Scholar] [CrossRef] [PubMed]
- Ridi, F.; Bonini, M.; Baglioni, P. Magneto-responsive nanocomposites: Preparation and integration of magnetic nanoparticles into films, capsules, and gels. Adv. Colloid Interface Sci. 2014, 207, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Wu, Z.H.; Yu, T.; Jiang, C.Z.; Kim, W.S. Recent progress on magnetic iron oxide nanoparticles: Synthesis, surface functional strategies and biomedical applications. Sci. Technol. Adv. Mater. 2015, 16, 23501. [Google Scholar] [CrossRef] [PubMed]
- Zhu, N.; Ji, H.N.; Yu, P.; Niu, J.Q.; Farooq, M.U.; Akram, M.W.; Udego, I.O.; Li, H.D.; Niu, X.B. Surface Modification of Magnetic Iron Oxide Nanoparticles. Nanomaterials 2018, 8, 810. [Google Scholar] [CrossRef]
- Zhi, D.F.; Yang, T.; Yang, J.; Fu, S.; Zhang, S.B. Targeting strategies for superparamagnetic iron oxide nanoparticles in cancer therapy. ActaBiomater. 2019, 102, 13–34. [Google Scholar] [CrossRef]
- Alshaer, W.; Hillaireau, H.; Fattal, E. Aptamer-guided nanomedicines for anticancer drug delivery. Adv. Drug Deliv. Rev. 2018, 134, 122–137. [Google Scholar] [CrossRef]
- Yoon, S.; Rossi, J.J. Targeted Molecular Imaging Using Aptamers in Cancer. Pharmaceuticals 2018, 11, 71. [Google Scholar] [CrossRef]
- Belyanina, I.V.; Zamay, T.N.; Zamay, G.S.; Zamay, S.S.; Kolovskaya, O.S.; Ivanchenko, T.I.; Denisenko, V.V.; Kirichenko, A.K.; Glazyrin, Y.E.; Garanzha, I.V.; et al. In Vivo Cancer Cells Elimination Guided by Aptamer-Functionalized Gold-Coated Magnetic Nanoparticles and Controlled with Low Frequency Alternating Magnetic Field. Theranostics 2017, 7, 3326–3337. [Google Scholar] [CrossRef]
- Kolovskaya, O.S.; Zamay, T.N.; Belyanina, I.V.; Karlova, E.; Garanzha, I.; Aleksandrovsky, A.S.; Kirichenko, A.; Dubynina, A.V.; Sokolov, A.E.; Zamay, G.S.; et al. Aptamer-Targeted PlasmonicPhotothermal Therapy of Cancer. Mol. Ther. Nucleic Acids 2017, 9, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Zamay, T.N.; Kolovskaya, O.S.; Glazyrin, Y.E.; Zamay, G.S.; Kuznetsova, S.A.; Spivak, E.A.; Wehbe, M.; Savitskaya, A.G.; Zubkova, O.A.; Kadkina, A.; et al. DNA-Aptamer Targeting Vimentin for Tumor Therapy In Vivo. Nucleic Acid Ther. 2014, 24, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Fedorov, D.G.; Kitaura, K. Extending the Power of Quantum Chemistry to Large Systems with the Fragment Molecular Orbital Method. J. Phys. Chem. A 2007, 111, 6904–6914. [Google Scholar] [CrossRef] [PubMed]
- Majeski, A.E.; Dice, J.F. Mechanisms of chaperone-mediated autophagy. Int. J. Biochem. Cell Biol. 2004, 36, 2435–2444. [Google Scholar] [CrossRef] [PubMed]
- Xie, W.; Zhang, L.; Jiao, H.F.; Guan, L.; Zha, J.M.; Li, X.T.; Wu, M.; Wang, Z.X.; Han, J.H.; You, H. Chaperone-mediated autophagy prevents apoptosis by degrading BBC3/PUMA. Autophagy 2015, 11, 1623–1635. [Google Scholar] [CrossRef] [PubMed]
- Groman, E.V.; Enriquez, P.M.; Jung, C.; Josephson, L. Arabinogalactan for Hepatic Drug Delivery. Bioconjug. Chem. 1994, 5, 547–556. [Google Scholar] [CrossRef]
- Ponder, G.R.; Richards, G.N. Arabinogalactan from Western Larch, Part II.; A Reversible Order-Disorder Transition. J. Carbohydr. Chem. 1997, 16, 195–211. [Google Scholar] [CrossRef]
- Josephson, L.; Groman, E.V.; Jung, C.; Lewis, J.M. Targeting of Therapeutic Agents Using Polysaccharides. U.S. Patent 5,336,506, 9 August 1994. [Google Scholar]
- Fedorov, D.G. The fragment molecular orbital method: Theoretical development, implementation in GAMESS, and applications. Wiley Interdiscip. Rev. Comput. Mol. Sci. 2017, 7, e1322. [Google Scholar] [CrossRef]
- Gaus, M.; Goez, A.; Elstner, M. Parametrization and Benchmark of DFTB3 for Organic Molecules. J. Chem. Theory Comput. 2013, 9, 338–354. [Google Scholar] [CrossRef]
- Nishimoto, Y.; Fedorov, D.G. The fragment molecular orbital method combined with density-functional tight-binding and the polarizable continuum model. Phys. Chem. Chem. Phys. 2016, 18, 22047–22061. [Google Scholar] [CrossRef]
- Fedorov, D.G. Solvent Screening in Zwitterions Analyzed with the Fragment Molecular Orbital Method. J. Chem. Theory Comput. 2019, 15, 5404–5416. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.W.; Baldridge, K.K.; Boatz, J.A.; Elbert, S.T.; Gordon, M.S.; Jensen, J.H.; Koseki, S.; Matsunaga, N.; Nguyen, K.A.; Su, S.; et al. General atomic and molecular electronic structure system. J. Comput. Chem. 1993, 14, 1347–1363. [Google Scholar] [CrossRef]
- Fedorov, D.G.; Kitaura, K. Pair interaction energy decomposition analysis. J. Comput. Chem. 2007, 28, 222–237. [Google Scholar] [CrossRef] [PubMed]
- Lehr, C.M.; Gabor, F. Lectins and glycoconjugates in drug delivery and targeting. Adv. Drug Deliv. Rev. 2004, 56, 419–420. [Google Scholar] [CrossRef]
- Groman, E.V.; Gou, D.M. Development of an immunoassay for larch arabinogalactan and its use in the detection of larch arabinogalactan in rat blood. Carbohydr. Res. 1997, 301, 69–76. [Google Scholar] [CrossRef]

| Sample | Molecular Mass of the Starting AG, Da | Amount of IronSalts, Mmol | Product Yield, % | Fe Content, % |
|---|---|---|---|---|
| FeAG (4.7%) | 16,645 | 0.75 | 81 | 4.7 |
| FrFeAG (4.5%) | 8380 | 0.75 | 82 | 4.5 |
| FeAG (6%) | 16,645 | 0.96 | 80 | 6.0 |
| FrFeAG (6%) | 8380 | 0.96 | 75 | 6.0 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kolovskaya, O.S.; Zamay, T.N.; Zamay, G.S.; Babkin, V.A.; Medvedeva, E.N.; Neverova, N.A.; Kirichenko, A.K.; Zamay, S.S.; Lapin, I.N.; Morozov, E.V.; et al. Aptamer-Conjugated Superparamagnetic Ferroarabinogalactan Nanoparticles for Targeted Magnetodynamic Therapy of Cancer. Cancers 2020, 12, 216. https://doi.org/10.3390/cancers12010216
Kolovskaya OS, Zamay TN, Zamay GS, Babkin VA, Medvedeva EN, Neverova NA, Kirichenko AK, Zamay SS, Lapin IN, Morozov EV, et al. Aptamer-Conjugated Superparamagnetic Ferroarabinogalactan Nanoparticles for Targeted Magnetodynamic Therapy of Cancer. Cancers. 2020; 12(1):216. https://doi.org/10.3390/cancers12010216
Chicago/Turabian StyleKolovskaya, Olga S., Tatiana N. Zamay, Galina S. Zamay, Vasily A. Babkin, Elena N. Medvedeva, Nadezhda A. Neverova, Andrey K. Kirichenko, Sergey S. Zamay, Ivan N. Lapin, Evgeny V. Morozov, and et al. 2020. "Aptamer-Conjugated Superparamagnetic Ferroarabinogalactan Nanoparticles for Targeted Magnetodynamic Therapy of Cancer" Cancers 12, no. 1: 216. https://doi.org/10.3390/cancers12010216
APA StyleKolovskaya, O. S., Zamay, T. N., Zamay, G. S., Babkin, V. A., Medvedeva, E. N., Neverova, N. A., Kirichenko, A. K., Zamay, S. S., Lapin, I. N., Morozov, E. V., Sokolov, A. E., Narodov, A. A., Fedorov, D. G., Tomilin, F. N., Zabluda, V. N., Alekhina, Y., Lukyanenko, K. A., Glazyrin, Y. E., Svetlichnyi, V. A., ... Kichkailo, A. S. (2020). Aptamer-Conjugated Superparamagnetic Ferroarabinogalactan Nanoparticles for Targeted Magnetodynamic Therapy of Cancer. Cancers, 12(1), 216. https://doi.org/10.3390/cancers12010216








