Involvement of the Anterior Commissure in Early Glottic Cancer (Tis-T2): A Review of the Literature
Abstract
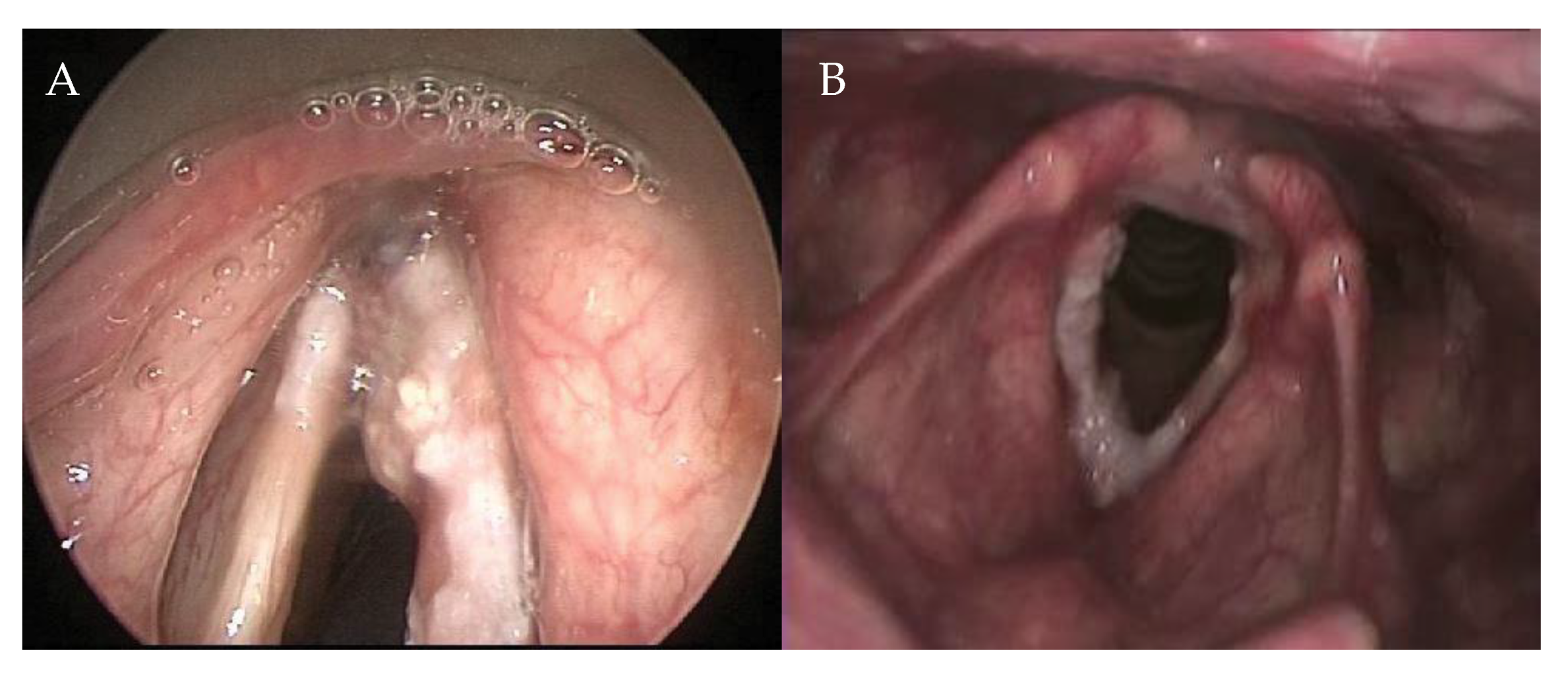
1. Introduction
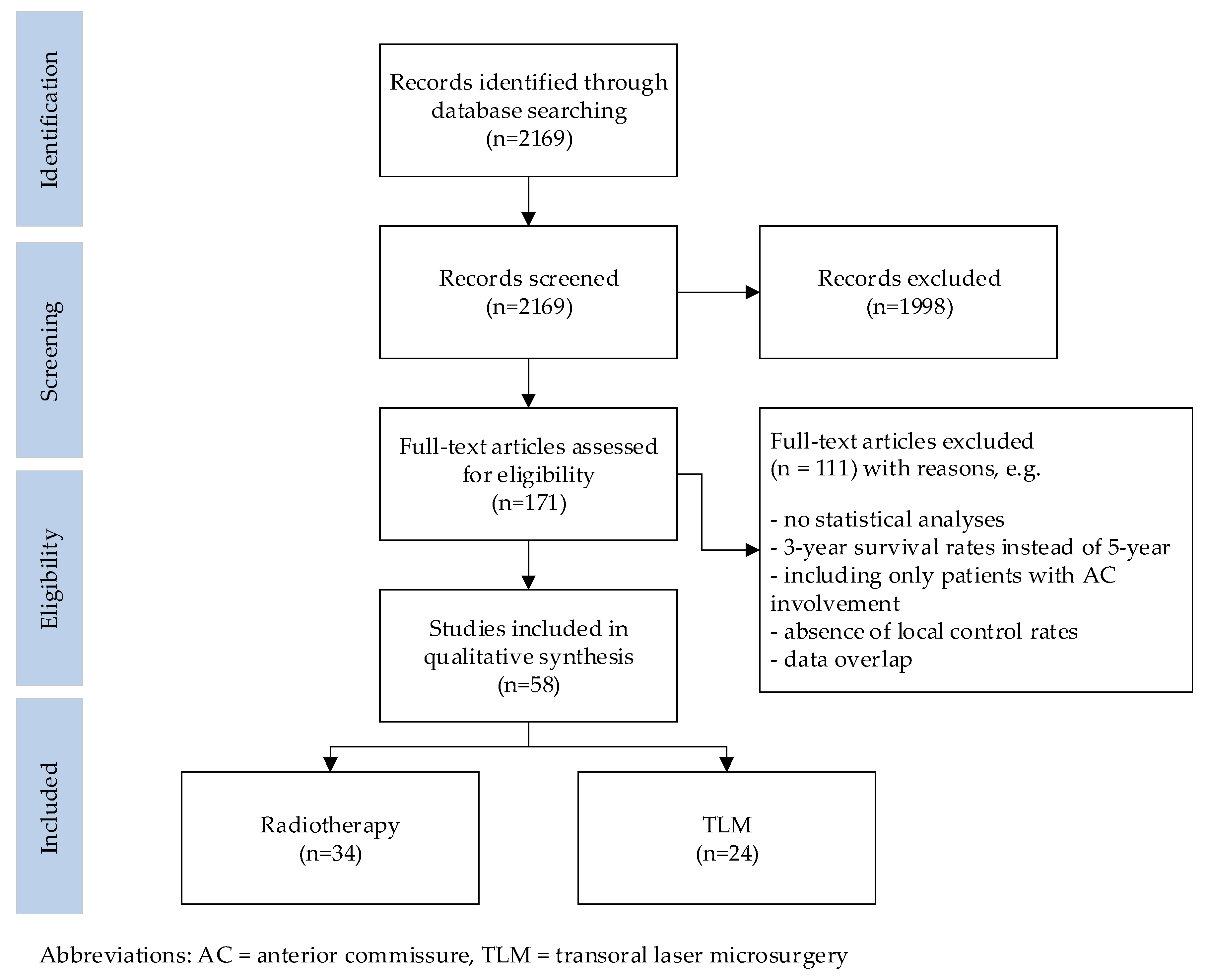
2. Methods
2.1. Search
2.2. Inclusion Criteria and Data Extraction
2.3. Statistical Analyses
3. Results
3.1. Search
3.2. Study Characteristics
3.3. Local Control
3.4. Overall Survival, Disease Specific Survival, and Larynx Preservation
4. Discussion
Limitations
5. Conclusions
Funding
Conflicts of interest
References
- Rucci, L.; Gammarota, L.; Borghi Cirri, M.B. Carcinoma of the anterior commissure of the larynx: I. Embryological and anatomic considerations. Ann. Otol. Rhinol. Laryngol. 1996, 105, 303–308. [Google Scholar] [PubMed]
- Sjögren, E. Transoral Laser Microsurgery in Early Glottic Lesions. Curr. Otorhinolaryngol. Rep. 2017, 5, 56–68. [Google Scholar] [CrossRef] [PubMed]
- Peretti, G.; Piazza, C.; Cocco, D.; De, B.L.; Del, B.F.; Redaelli De Zinis, L.O.; Nicolai, P. Transoral CO2 laser treatment for Tis–T3 glottic cancer: The University of Brescia experience on 595 patients. Head Neck 2010, 32, 977–983. [Google Scholar] [CrossRef] [PubMed]
- Prades, J.M.; Peoc’h, M.; Petcu, C.; Karkas, A.; Dumollard, J.M.; Gavid, M. The anterior commissure of the human larynx revisited. Surg. Radiol. Anat. 2017, 39, 871–876. [Google Scholar] [CrossRef] [PubMed]
- Yamazaki, H.; Nishiyama, K.; Tanaka, E.; Koizumi, M.; Chatani, M. Radiotherapy for early glottic carcinoma (T1N0M0): Results of prospective randomized study of radiation fraction size and overall treatment time. Int. J. Radiat. Oncol. Biol. Phys. 2006, 64, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Siwek, J.; Slawson, D.C.; Health, V.; Shaughnessy, A.F.; D, P.; Family, H.; Residency, P.; Gourlay, M. How to write an evidence–based clinical review article. Am. Fam. Physician 2002, 65, 251–259. [Google Scholar] [PubMed]
- Al–Mamgani, A.; van Rooij, P.H.; Mehilal, R.; Verduijn, G.M.; Tans, L.; Kwa, S.L. Radiotherapy for T1a glottic cancer: The influence of smoking cessation and fractionation schedule of radiotherapy. Eur. Arch. Otorhinolaryngol. 2014, 271, 125–132. [Google Scholar] [CrossRef]
- Berwouts, D.; Swimberghe, M.; Duprez, F.; Boterberg, T.; Bonte, K.; Deron, P.; De, G.W.; De, N.W.; Madani, I. Intensity–modulated radiotherapy for early–stage glottic cancer. Head Neck 2016, 38 (Suppl. 1), E179–E184. [Google Scholar] [CrossRef]
- Raitiola, H.; Wigren, T.; Pukander, J. Radiotherapy outcome and prognostic factors in early glottic carcinoma. Auris Nasus Larynx 2000, 27, 153–159. [Google Scholar] [CrossRef]
- Smee, R.I.; Meagher, N.S.; Williams, J.R.; Broadley, K.; Bridger, G.P. Role of radiotherapy in early glottic carcinoma. Head Neck 2010, 32, 850–859. [Google Scholar] [CrossRef]
- Sommat, K.; Yit, N.L.; Kwok, L.L. Comparison between 4–MV and 6–MV radiotherapy in T1N0 glottic cancer. Laryngoscope 2017, 127, 1061–1067. [Google Scholar] [CrossRef] [PubMed]
- Thariat, J.; Bruchon, Y.; Bonnetain, F.; Barillot, I.; Truc, G.; Peignaux, K.; Horiot, J.C.; Maingon, P. Conservative treatment of early glottic carcinomas with exclusive radiotherapy. Cancer Radiother. 2004, 8, 288–296. [Google Scholar] [CrossRef]
- Bignardi, M.; Antognoni, P.; Sanguineti, G.; Magli, A.; Molteni, M.; Merlotti, A.; Richetti, A.; Tordiglione, M.; Conte, L.; Magno, L. Hyperfractionated radiotherapy for T2N0 glottic carcinoma: A retrospective analysis at 10 years follow-up in a series of 60 consecutive patients. Tumori J. 2004, 90, 317–323. [Google Scholar] [CrossRef]
- Chera, B.S.; Amdur, R.J.; Morris, C.G.; Kirwan, J.M.; Mendenhall, W.M. T1N0 to T2N0 squamous cell carcinoma of the glottic larynx treated with definitive radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2010, 78, 461–466. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.Y.; Kim, K.H.; Keum, K.C.; Koh, Y.W.; Kim, S.H.; Choi, E.C.; Lee, C.G. Radiotherapy versus Cordectomy in the Management of Early Glottic Cancer. Cancer Res. Treat 2017. [Google Scholar] [CrossRef] [PubMed]
- Harada, A.; Sasaki, R.; Miyawaki, D.; Yoshida, K.; Nishimura, H.; Ejima, Y.; Kitajima, K.; Saito, M.; Otsuki, N.; Nibu, K. Treatment outcomes of the patients with early glottic cancer treated with initial radiotherapy and salvaged by conservative surgery. Jpn. J. Clin. Oncol. 2015, 45, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.A.; Mendenhall, C.M.; Kirwan, J.; Morris, C.G.; Donnan, A.; Holwerda, S.; Kraus, S.T.; Mann, C.J.; Grant, J.R.; Donnan, B.; et al. Radiation therapy for management of t1–t2 glottic cancer at a private practice. Am. J. Clin. Oncol. 2010, 33, 587–590. [Google Scholar] [CrossRef]
- Khan, M.K.; Koyfman, S.A.; Hunter, G.K.; Reddy, C.A.; Saxton, J.P. Definitive radiotherapy for early (T1–T2) glottic squamous cell carcinoma: A 20 year Cleveland Clinic experience. Radiat. Oncol. 2012, 7, 193. [Google Scholar] [CrossRef]
- Matsumoto, F.; Ohba, S.; Fujimaki, M.; Ikeda, K. The value of insulin–like growth factor–1 receptor for predicting early glottic carcinoma response to radiotherapy. Auris Nasus Larynx 2016, 43, 440–445. [Google Scholar] [CrossRef]
- Mendenhall, W.M.; Amdur, R.J.; Morris, C.G.; Hinerman, R.W. T1–T2N0 squamous cell carcinoma of the glottic larynx treated with radiation therapy. J. Clin. Oncol. 2001, 19, 4029–4036. [Google Scholar] [CrossRef]
- Remacle, M.; Eckel, H.E.; Antonelli, A.; Brasnu, D.; Chevalier, D.; Friedrich, G.; Olofsson, J.; Rudert, H.H.; Thumfart, W.; de Vincentiis, M.; et al. Endoscopic cordectomy. A proposal for a classification by the Working Committee, European Laryngological Society. Eur. Arch. Otorhinolaryngol. 2000, 257, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Remacle, M.; Van Haverbeke, C.; Eckel, H.; Bradley, P.; Chevalier, D.; Djukic, V.; de Vicentiis, M.; Friedrich, G.; Olofsson, J.; Peretti, G.; et al. Proposal for revision of the European Laryngological Society classification of endoscopic cordectomies. Eur. Arch. Otorhinolaryngol. 2007, 264, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Steiner, W.; Ambrosch, P.; Rodel, R.M.; Kron, M. Impact of anterior commissure involvement on local control of early glottic carcinoma treated by laser microresection. Laryngoscope 2004, 114, 1485–1491. [Google Scholar] [CrossRef] [PubMed]
- Wolber, P.; Schwarz, D.; Stange, T.; Ortmann, M.; Balk, M.; Anagiotos, A.; Gostian, A.O. Surgical Treatment for Early Stage Glottic Carcinoma with Involvement of the Anterior Commissure. Otolaryngol. Head Neck Surg. 2018, 158, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Steiner, W.; Ambrosch, P. Endoscopic Laser Surgery of the Upper Aerodigestive Tract, 1st ed.; Thieme: Stuttgart, Germany, 2000; pp. 17–33. [Google Scholar]
- Hakeem, A.H.; Tubachi, J.; Pradhan, S.A. Significance of anterior commissure involvement in early glottic squamous cell carcinoma treated with trans–oral CO2 laser microsurgery. Laryngoscope 2013, 123, 1912–1917. [Google Scholar] [CrossRef] [PubMed]
- Hsin, L.J.; Fang, T.J.; Chang, K.P.; Fang, K.H.; Tsang, N.M.; Chen, Y.L.; Jung, S.M.; Yeh, A.R.; Hao, S.P. Transoral endoscopic CO2 laser microsurgery for early laryngeal cancers. Chang Gung Med. J. 2009, 32, 517–525. [Google Scholar] [PubMed]
- Rodel, R.M.; Steiner, W.; Muller, R.M.; Kron, M.; Matthias, C. Endoscopic laser surgery of early glottic cancer: Involvement of the anterior commissure. Head Neck 2009, 31, 583–592. [Google Scholar] [CrossRef]
- Gallet, P.; Rumeau, C.; Nguyen, D.T.; Teixeira, P.A.; Baumann, C.; Toussaint, B. “Watchful observation” follow-up scheme after endoscopic CO2 laser treatment for small glottic carcinomas: A retrospective study of 93 cases. Clin. Otolaryngol. 2017, 42, 1193–1199. [Google Scholar] [CrossRef]
- Hartl, D.M.; De Mones, E.; Hans, S.; Janot, F.; Brasnu, D. Treatment of early–stage glottic cancer by transoral laser resection. Ann. Otol. Rhinol. Laryngol. 2007, 116, 832–836. [Google Scholar] [CrossRef]
- Rucci, L.; Romagnoli, P.; Scala, J. CO2 laser therapy in Tis and T1 glottic cancer: Indications and results. Head Neck 2010, 32, 392–398. [Google Scholar]
- Son, H.-J.; Lee, Y.S.; Ku, J.Y.; Roh, J.-L.; Choi, S.-H.; Nam, S.Y.; Kim, S.Y. Radiological tumor thickness as a risk factor for local recurrence in early glottic cancer treated with laser cordectomy. Eur. Arch. Oto-Rhino-Laryngol. 2018, 275, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Mortuaire, G.; Francois, J.; Wiel, E.; Chevalier, D. Local recurrence after CO2 laser cordectomy for early glottic carcinoma. Laryngoscope 2006, 116, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Al–Mamgani, A.; van Rooij, P.H.; Woutersen, D.P.; Mehilal, R.; Tans, L.; Monserez, D.; Baatenburg de Jong, R.J. Radiotherapy for T1–2N0 glottic cancer: A multivariate analysis of predictive factors for the long–term outcome in 1050 patients and a prospective assessment of quality of life and voice handicap index in a subset of 233 patients. Clin. Otolaryngol. 2013, 38, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Bron, L.P.; Soldati, D.; Zouhair, A.; Ozsahin, M.; Brossard, E.; Monnier, P.; Pasche, P. Treatment of early stage squamous–cell carcinoma of the glottic larynx: Endoscopic surgery or cricohyoidoepiglottopexy versus radiotherapy. Head Neck 2001, 23, 823–829. [Google Scholar] [CrossRef] [PubMed]
- Cellai, E.; Frata, P.; Magrini, S.M.; Paiar, F.; Barca, R.; Fondelli, S.; Polli, C.; Livi, L.; Bonetti, B.; Vitali, E.; et al. Radical radiotherapy for early glottic cancer: Results in a series of 1087 patients from two Italian radiation oncology centers. I. The case of T1N0 disease. Int. J. Radiat. Oncol. Biol. Phys. 2005, 63, 1378–1386. [Google Scholar] [CrossRef] [PubMed]
- Cheah, N.L.; Lupton, S.; Marshall, A.; Hartley, A.; Glaholm, J. Outcome of T1N0M0 squamous cell carcinoma of the larynx treated with short-course radiotherapy to a total dose of 50 Gy in 16 fractions: The Birmingham experience. Clin. Oncol. (R. Coll. Radiol.) 2009, 21, 494–501. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.-F.F.; Chang, J.T.-C.; Tsang, N.-M.M.; Liao, C.-T.T.; Chen, W.-C.C. Radiotherapy of early–stage glottic cancer: Analysis of factors affecting prognosis. Ann. Otol. Rhinol. Laryngol. 2003, 112, 904–911. [Google Scholar] [CrossRef] [PubMed]
- Frata, P.; Cellai, E.; Magrini, S.M.; Bonetti, B.; Vitali, E.; Tonoli, S.; Buglione, M.; Paiar, F.; Barca, R.; Fondelli, S.; et al. Radical radiotherapy for early glottic cancer: Results in a series of 1087 patients from two Italian radiation oncology centers. II. The case of T2N0 disease. Int. J. Radiat. Oncol. Biol. Phys. 2005, 63, 1387–1394. [Google Scholar] [CrossRef] [PubMed]
- Garden, A.S.; Forster, K.; Wong, P.F.; Morrison, W.H.; Schechter, N.R.; Ang, K.K. Results of radiotherapy for T2N0 glottic carcinoma: Does the “2” stand for twice–daily treatment? Int. J. Radiat. Oncol. Biol. Phys. 2003, 55, 322–328. [Google Scholar] [CrossRef]
- Gowda, R.V.; Henk, J.M.; Mais, K.L.; Sykes, A.J.; Swindell, R.; Slevin, N.J. Three weeks radiotherapy for T1 glottic cancer: The Christie and Royal Marsden Hospital Experience. Radiother. Oncol. 2003, 68, 105–111. [Google Scholar] [CrossRef]
- Gultekin, M.; Ozyar, E.; Cengiz, M.; Ozyigit, G.; Hayran, M.; Hosal, S.; Akyol, F. High daily fraction dose external radiotherapy for T1 glottic carcinoma: Treatment results and prognostic factors. Head Neck 2012, 34, 1009–1014. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.; Liao, Z.; Gao, L.; Huang, X.; Xu, G. Analysis of prognostic factors for T(1)N(0)M(0) glottic cancer treated with definitive radiotherapy alone: Experience of the cancer hospital of Peking Union Medical College and the Chinese Academy Of Medical Sciences. Int. J. Radiat. Oncol. Biol. Phys. 2002, 54, 471–478. [Google Scholar] [CrossRef]
- Laskar, S.G.; Baijal, G.; Murthy, V.; Chilukuri, S.; Budrukkar, A.; Gupta, T.; Agarwal, J.P. Hypofractionated Radiotherapy for T1N0M0 Glottic Cancer: Retrospective Analysis of Two Different Cohorts of Dose–fractionation Schedules from a Single Institution. Clin. Oncol. 2012, 24, e180–e186. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.J.; Wu, H.G.; Kwon, T.K.; Hah, J.H.; Sung, M.W.; Kim, K.H.; Park, C.I. Long–Term Outcome of Definitive Radiotherapy for Early Glottic Cancer: Prognostic Factors and Patterns of Local Failure. Cancer Res. Treat. 2015, 47, 862–870. [Google Scholar] [CrossRef] [PubMed]
- Murakami, R.; Nishimura, R.; Baba, Y.; Furusawa, M.; Ogata, N.; Yumoto, E.; Yamashita, Y. Prognostic factors of glottic carcinomas treated with radiation therapy: Value of the adjacent sign on radiological examinations in the sixth edition of the UICC TNM staging system. Int. J. Radiat. Oncol. Biol. Phys. 2005, 61, 471–475. [Google Scholar] [CrossRef] [PubMed]
- Nozaki, M.; Furuta, M.; Murakami, Y.; Izawa, Y.; Iwasaki, N.; Takahashi, H.; Watanabe, K. Radiation therapy for T1 glottic cancer: Involvement of the anterior commissure. Anticancer Res. 2000, 20, 1121–1124. [Google Scholar] [PubMed]
- Robert, A.; Pointreau, Y.; Janoray, G.; Bardet, E.; Fesneau, M.; Garaud, P.; Chapet, S.; Lafond, C.; Dupuis, O.; Calais, G. A large French multicenter retrospective series of T1–T2N0 vocal cords carcinomas treated with exclusive irradiation Une grande serie retrospective francaise de carcinomes des cordes vocales de stade T1–T2N0 traites par irradiation exclusive. Cancer/Radiotherapie 2017, 21, 286–290. [Google Scholar] [CrossRef] [PubMed]
- Sjogren, E.V.; Wiggenraad, R.G.; Le, C.S.; Snijder, S.; Pomp, J.; Baatenburg de Jong, R.J. Outcome of radiotherapy in T1 glottic carcinoma: A population–based study. Eur. Arch. Otorhinolaryngol. 2009, 266, 735–744. [Google Scholar] [CrossRef][Green Version]
- Tong, C.C.; Au, K.H.; Ngan, R.K.; Chow, S.M.; Cheung, F.Y.; Fu, Y.T.; Au, J.S.; Law, S.C. Impact and relationship of anterior commissure and time–dose factor on the local control of T1N0 glottic cancer treated by 6 MV photons. Radiat. Oncol. 2011, 6, 53. [Google Scholar] [CrossRef]
- Warde, P.; O’Sullivan, B.; Bristow, R.G.; Panzarella, T.; Keane, T.J.; Gullane, P.J.; Witterick, I.P.; Payne, D.; Liu, F.F.; McLean, M.; et al. T1/T2 glottic cancer managed by external beam radiotherapy: The influence of pretreatment hemoglobin on local control. Int. J. Radiat. Oncol. Biol. Phys. 1998, 41, 347–353. [Google Scholar] [CrossRef]
- Zouhair, A.; Azria, D.; Coucke, P.; Matzinger, O.; Bron, L.; Moeckli, R.; Do, H.P.; Mirimanoff, R.O.; Ozsahin, M. Decreased local control following radiation therapy alone in early–stage glottic carcinoma with anterior commissure extension. Strahlenther. Onkol. 2004, 180, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Ansarin, M.; Cattaneo, A.; De, B.L.; Zorzi, S.; Lombardi, F.; Alterio, D.; Rocca, M.C.; Scelsi, D.; Preda, L.; Chiesa, F.; et al. Retrospective analysis of factors influencing oncologic outcome in 590 patients with early–intermediate glottic cancer treated by transoral laser microsurgery. Head Neck 2017, 39, 71–81. [Google Scholar] [CrossRef] [PubMed]
- Carta, F.; Bandino, F.; Olla, A.M.; Chuchueva, N.; Gerosa, C.; Puxeddu, R. Prognostic value of age, subglottic, and anterior commissure involvement for early glottic carcinoma treated with CO2 laser transoral microsurgery: A retrospective, single–center cohort study of 261 patients. Eur. Arch. Otorhinolaryngol. 2018, 275, 1199–1210. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.F.; Chu, P.Y. Predictors of local recurrence of glottic cancer in patients after transoral laser microsurgery. J. Chin. Med. Assoc. 2017, 80, 452–457. [Google Scholar] [CrossRef] [PubMed]
- Chone, C.T.; Yonehara, E.; Martins, J.E.F.; Altemani, A.; Crespo, A.N. Importance of anterior commissure in recurrence of early glottic cancer after laser endoscopic resection. Arch. Otolaryngol. Head Neck Surg. 2007, 133, 882–887. [Google Scholar] [CrossRef] [PubMed]
- Fang, T.J.; Courey, M.S.; Liao, C.T.; Yen, T.C.; Li, H.Y. Frozen margin analysis as a prognosis predictor in early glottic cancer by laser cordectomy. Laryngoscope 2013, 123, 1490–1495. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, C.; Hans, S.; Sadoughi, B.; Brasnu, D. Identifying outcome predictors of transoral laser cordectomy for early glottic cancer. Head Neck 2016, 38, E411. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, C.; Cornu, N.; Hans, S.; Sadoughi, B.; Badoual, C.; Brasnu, D. Early glottic cancer involving the anterior commissure treated by transoral laser cordectomy. Laryngoscope 2016, 126, 1817–1822. [Google Scholar] [CrossRef]
- Ledda, G.P.; Grover, N.; Pundir, V.; Masala, E.; Puxeddu, R. Functional outcomes after CO2 laser treatment of early glottic carcinoma. Laryngoscope 2006, 116, 1007–1011. [Google Scholar] [CrossRef]
- Lee, H.S.; Chun, B.G.; Kim, S.W.; Kim, S.T.; Oh, J.H.; Hong, J.C.; Lee, K.D. Transoral laser microsurgery for early glottic cancer as one–stage single–modality therapy. Laryngoscope 2013, 123, 2670–2674. [Google Scholar] [CrossRef]
- Peretti, G.; Nicolai, P.; Redaelli De Zinis, L.O.; Berlucchi, M.; Bazzana, T.; Bertoni, F.; Antonelli, A.R. Endoscopic CO2 laser excision for tis, T1, and T2 glottic carcinomas: Cure rate and prognostic factors. Otolaryngol. Head Neck Surg. 2000, 123, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Peretti, G.; Nicolai, P.; Piazza, C.; Redaelli De Zinis, L.O.; Valentini, S.; Antonelli, A.R. Oncological results of endoscopic resections of Tis and T1 glottic carcinomas by carbon dioxide laser. Ann. Otol. Rhinol. Laryngol. 2001, 110, 820–826. [Google Scholar] [CrossRef] [PubMed]
- Peretti, G.; Piazza, C.; Del, B.F.; Mora, R.; Grazioli, P.; Barbieri, D.; Mangili, S.; Nicolai, P. Function preservation using transoral laser surgery for T2–T3 glottic cancer: Oncologic, vocal, and swallowing outcomes. Eur. Arch. Otorhinolaryngol. 2013, 270, 2275–2281. [Google Scholar] [CrossRef] [PubMed]
- Sachse, F.; Stoll, W.; Rudack, C. Evaluation of treatment results with regard to initial anterior commissure involvement in early glottic carcinoma treated by external partial surgery or transoral laser microresection. Head Neck 2009, 31, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Brierley, J.D.; Gospodarowicz,, M.K.; Wittekind, C. TNM Classification of Malignant Tumours, 8th ed.; John Wiley and Sons Ltd.: Hoboken, NJ, USA, 2017; pp. 9–11. [Google Scholar]
- Rucci, L.; Gammarota, L.; Gallo, O. Carcinoma of the anterior commissure of the larynx: II. Proposal of a new staging system. Ann. Otol. Rhinol. Laryngol. 1996, 105, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Piazza, C.; Filauro, M.; Paderno, A.; Marchi, F.; Perotti, P.; Morello, R.; Taboni, S.; Parrinello, G.; Incandela, F.; Iandelli, A.; et al. Three-Dimensional Map of Isoprognostic Zones in Glottic Cancer Treated by Transoral Laser Microsurgery as a Unimodal Treatment Strategy. Front. Oncol. 2018, 8, 175. [Google Scholar] [CrossRef] [PubMed]
- Peretti, G.; Piazza, C.; Mora, F.; Garofolo, S.; Guastini, L. Reasonable limits for transoral laser microsurgery in laryngeal cancer. Curr. Opin. Otolaryngol. Head Neck Surg. 2016, 24, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Blanch, J.L.; Vilaseca, I.; Caballero, M.; Moragas, M.; Berenguer, J.; Bernal–Sprekelsen, M. Outcome of transoral laser microsurgery for T2–T3 tumors growing in the laryngeal anterior commissure. Head Neck 2011, 33, 1252–1259. [Google Scholar] [CrossRef]
- Vilaseca, I.; Nogués-Sabaté, A.; Avilés-Jurado, F.X.; Berenguer, J.; Grau, J.J.; Verger, E.; Nadal, A.; Muxí, A.; Bernal–Sprekelsen, M.; Blanch, J.L. Factors of local recurrence and organ preservation with transoral laser microsurgery in laryngeal carcinomas; CHAID decision–tree analysis. Head Neck 2019, 41, 756–764. [Google Scholar] [CrossRef]
| First Author and Year | Treatment Period | Treatment Details | Tumor | Patients | Follow-up (in Months) | 5-Year Local Control (%) | 5-Year Overall Survival (%) | 5-Year Disease Specific Survival (%) | 5-Year Laryngeal Preservation (%) |
|---|---|---|---|---|---|---|---|---|---|
| Al-Mamgani 2014 [7] | 1985–2011 | Intended dose 66 Gy <’97 conventional >’98 accelerated | T1 | AC+ 214 AC− 335 | Median 93 | OR = 1.1 p = 0.646 | |||
| Al–Mamgani 2013 [34] | 1985–2011 | Intended dose 66 Gy <’97 conventional >’98 accelerated | T1–T2 | AC+ 553 AC− 497 | Median 90 | AC+ 84 AC− 86 OR 1.1 p = 0.091 | |||
| Berwouts 2016 [8] | 2007–2011 | IMRT: T1: 63 Gy T2: 67.5 Gy Conv RT T1: 66 Gy T2: 70 Gy | T1–T2 | IMRT AC+ 7 AC− 33 Conv RT AC+ 11 AC− 70 | IMRT: Median 45.6 Conv RT: Median 108 | IMRT: p = 0.22 Conv RT: p = 0.62 | IMRT: p = 0.60 Conv RT: p = 0.98 | IMRT: p = 0.64 Conv RT: p = 0.27 | |
| Bignardi 2004 [13] | 1980–1988 | 63 Gy hyperfractionated | T2 | AC+ 33 AC− 27 | Median 117.6 | HR 0.48 p = 0.12 | |||
| Bron 2001 [35] | 1983–1996 | Median 70 Gy | T1–T2 | AC+ 43 AC− 38 | Median 59 | AC+ 66 AC− 90 p = 0.009 | AC+ 88 AC− 100 p = NS | ||
| Cellai 2005 [36] | 1970–1999 | <61 Gy 82 61–65 Gy 352 >65 Gy 397 | T1 | AC+ 282 AC− 549 | Mean 111.6 | AC+ 78 AC− 87 p = 0.001 | |||
| Cheah 2009 [37] | 1993–2001 | 50 Gy | T1 | AC+ 22 AC− 77 | Median 84 | AC+ 78 AC− 90 HR 2.17 | |||
| Chen 2003 [38] | 1983–2001 | T1: median 66 Gy T2: median 70 Gy | T1–T2 | T1 AC+ 33 T1 AC− 55 T2 AC+ 29 T2 AC–17 | Range 12–120 | T1: 55 vs. 90 p = 0.0035 T2: 54 vs. 70 p = 0.74 MVA: RR 3.8 p = 0.020 | T1 p = 0.0366 | ||
| Chera 2010 [14] | 1964–2006 | Median 63 Gy | T1–T2 | AC+ 369 AC− 216 | Median 147 | p = 0.342 | |||
| Chung 2017 [15] | 2006–2012 | Median 65.25 Gy | Tis–T2 | AC+ 52 AC− 112 | Median 77.7 | HR 1.67 p = 0.197 | |||
| Frata 2005 [39] | 1970–1999 | <61 Gy 33 61–65 Gy 83 >65 Gy 140 | T2 | AC+ 145 AC− 111 | Mean 90 | AC+ 69 AC–77 p = 0.1 | |||
| Garden 2003 [40] | 1970–1998 | Median 70 Gy | T2 | AC+ 156 AC− 74 | Median 82 | AC+ 70 AC− 75 p = 0.59 | |||
| Gowda 2003 [41] | 1989–1997 | Total dose 50–52.5 Gy | T1 | AC+ 50 AC− 150 | Median 70 | AC+ 89 AC− 94 p = 0.47 | |||
| Gultekin 2012 [42] | 1998–2007 | Median 64.4 Gy | T1 | AC+ 31 AC− 152 | Median 63 | AC+ 79 AC− 82 p = 0.65 | AC+ 78 AC− 92 p = 0.16 | AC+ 81 AC− 92 p = 0.16 | |
| Harada 2015 [16] | 1999–2010 | Hyperfractionated T1a: median 66 Gy T1b: median 70 Gy | T1–T2 | AC+ 50 AC− 65 | Median 61 | UVA p = 0.25 | |||
| Jin 2002 [43] | 1958–1994 | Median 68.0 Gy | T1 | AC+ 70 AC− 168 | Median 127 | AC+ 70.5 AC− 87.1 p = 0.003 HR 2.00 p = 0.024 | AC+ 79.4 AC− 86.0 p = 0.32 | ||
| Jones 2010 [17] | 1987–2006 | T1 median 63 Gy T2 median 74.4 Gy | T1–T2 | AC+ 70 AC− 48 | Median 69.6 | NS | |||
| Khan 2012 [18] | 1986–2006 | Median 68.2 Gy | T1–T2 | AC+ 71 AC− 52 | Mean 67.2 | UVA p = 0.0505 MVA p = 0.094 | |||
| Laskar 2012 [44] | 1975–2000 | Hypofractionated 50–62.5 Gy | T1 | AC+ 228 AC− 414 | Median 62 | AC+ 86.3 AC− 90.3 p = 0.367 | |||
| Lim 2015 [45] | 1981–2010 | Median 66 Gy | T1–T2 | AC+ 56 AC–166 | Mean 85.2 | AC+ 75.7 AC− 91.9 p < 0.001 MVA HR 3.37 p = 0.001 | |||
| Matsumoto 2016 [19] | 2007–2014 | Maximum total dose 63.0–70 Gy | T1–T2 | AC+ 13 AC− 30 | Median 33 | UVA 0.085 MVA HR 4.97 p = 0.023 | |||
| Mendenhall 2001 [20] | 1964–1998 | Median 63 Gy | T1–T2 | AC+ 328 AC− 191 | Median 118.4 | MVA p = 0.350 | p = 0.224 | p = 0.293 | |
| Murakami 2005 [46] | 1989–1998 | T1a 60–66 Gy T1b–T2 64–70 Gy | T1–2 | AC+ 59 AC− 71 | Mean 75 | AC+ 74 AC− 78 p = 0.668 | |||
| Nozaki 2000 [47] | 1985–1997 | Range 60–70 Gy | T1 | AC+ 14 AC− 50 | Not mentioned | AC+ 58 AC− 89 p < 0.05 | |||
| Raitola 2000 [9] | 1970–1991 | Range 45–70 Gy | T1–T2 | AC+ 19 AC− 57 | Median 82.8 | HR 3.8 p = 0.004 MVA = NS | HR 3.0 (0.9–9.9) p = 0.0706 | ||
| Robert 2017 [48] | 1987–2015 | Mean 66.5 Gy | T1–T2 | AC+ 45 AC–213 | Median 50 | AC+ 84 AC− 88 p = 0.382 | |||
| Sjogren 2009 [49] | 1982–1993 | Median 60 Gy | T1 | AC+ 106 AC–210 | Median 70 | AC+ 85 AC− 87 p = 0.38 | |||
| Smee 2010 [10] | 1967–2006 | Median 60 Gy | Tis–T2 | AC+ 127 AC− 395 | Median 91.2 | UVA p = 0.016 MVA p = 0.040 | UVA = 0.019 MVA 0.050 (SE 0.303) | ||
| Sommat 2017 [11] | 2000–2012 | Median 63.0 Gy | T1 | AC+ 62 AC− 37 | Median 58.8 | HR 2.36 p = 0.274 | |||
| Thairat 2004 [12] | 1975–2001 | Median 66 Gy | Tis–T2 | AC+ 37 AC− 118 | Median 66 | HR 1.1 p = 0.73 | |||
| Tong 2011 [50] | 1983–2005 | 55–68 Gy | T1 | AC+ 197 AC− 236 | Median 126 | AC+ 86 AC− 95 p = 0.004 MVA HR 2.34 p = 0.011 | |||
| Warde 1998 [51] | 1981–1989 | 50 Gy | T1–T2 | AC+ 261 AC− 474 | Median 81.6 | AC+ 75 AC− 85 p = 0.0005 MVA NS | |||
| Yamazaki 2006 [5] | 1993–2001 | 56.25–63 Gy | T1 | AC+ 26 AC– 154 | Median 64 | OR 0.25 p = 0.25 | |||
| Zouhair 2004 [52] | 1983–2000 | Median 70 Gy | T1–T2 | AC+ 61 AC− 61 | Median 85 | AC+ 73 AC− 94 p = 0.002 MVA RR 0.42 p = 0.001 |
| First Author and Year | Treatment Period | Treatment Details | Tumor | Patients | Follow-up (in Months) | 5-Year Local Control (%) | 5-Year Overall Survival (%) | 5-Year Disease Specific Survival (%) | 5-Year Laryngeal Preservation (%) |
|---|---|---|---|---|---|---|---|---|---|
| Ansarin 2017 [53] | 1999–2013 | TLM (ELS I–VI) | Tis–T3 | AC+ 102 AC− 483 | Median 72 | AC+ 79.4 AC –86.7 p = 0.04 MVA HR 1.29 p = 0.38 | AC− 96.0 AC+ 87.2 p = 0.004 | p = 0.12 | |
| Carta 2018 [54] | 1993–2005 and 2010–2016 | TLM (ELS I–VI) | Tis–T2 | AC+ 105 AC–156 AC0 156 AC1 31 AC2 65 AC3 9 | Median 51.6 | AC+ 89.7 AC− 93.9 p = 0.205 AC0 93.9 AC1 96.2 AC2 89.3 AC3 74.1 p = 0.044 | AC+ 78.6 AC− 89.5 NS | AC+ 98.4 AC− 100 NS | AC+ 95.3 AC− 99.1 p = 0.08 AC0 99.1 AC1 100 AC2 96.1 AC3 71.1 p < 0.0001 |
| Chang 2017 [55] | 2003–2009 | TLM (ELS I–VI) | Tis–T3 | AC+ 34 AC− 59 | Median 35 | AC+ 74 AC− 95 p = 0.007 MVA NS | |||
| Chone 2007 [56] | 1998–2003 | TLM (ELS I–III) | T1–T2 | AC+ 24 AC− 24 | Mean 44 | AC+ 79 AC− 96 p = 0.08 | AC+ 96 AC− 100 p = 0.50 | ||
| Fang 2013 [57] | 2004–2011 | TLM (ELS I–VI) | T1–T2 | AC+ 45 AC− 28 | Median 33 | AC+ 83 AC− 85 p = 0.906 | |||
| Gallet 2017 [29] | 2001–2010 | TLM (ELS III–IV) | Tis–T2 | AC+ 49 AC− 44 | Median 75.6 | UVA OR 3.4 p = 0.021 MVA = NS | |||
| Hakeem 2013 [26] | 2000–2011 | TLM (nfs) | T1–T2 | AC+ 61 AC− 235 | Mean 49 | p = 0.0001 | AC+ 90.2 AC− 86.4 p = 0.642 | AC+ 95.1 AC− 91.5 p = 0.642 | AC+ 95.01 AC− 93.2 p = 0.287 |
| Hartl 2007 [30] | 1994–2006 | TLM (ELS I–V) | Tis–T1 | AC+ 8 AC− 79 | Median 46 | p = 0.16 | |||
| Hoffmann 2016a [58] | 2001–2011 | TLM (I–VI) | Tis–T2 | AC+ 75 AC− 126 | Mean 50.82 | AC+ 54.6 AC− 79.8 p = 0.004 | AC+ 76.9 AC− 88.5 p = 0.29 | AC+ 90.8 AC− 99.0 p = 0.03 | AC+ 91.9 AC− 100 p = 0.0003 |
| Hoffmann 2016b [59] | 2001–2013 | TLM (Va–VI) | Tis–T2 | AC1 29 AC2 17 AC3 50 | Mean 44.3 | AC1 71.6 AC2 87.5 AC3 50.8 p–0.04 | NS | NS | NS |
| Hsin 2009 [27] | 1999–2008 | TLM (nfs) | Tis–T2 | AC+ 18 AC− 30 | Median 36.5 | AC+ 74 AC− 71 p = 0.90 | |||
| Ledda 2006 [60] | 1993–2001 | TLM (ELS I–V) | Tis–T2 | AC+ 22 AC− 81 | Mean 70.8 | AC+ 87.5 AC− 96.5 p = 0.6 | |||
| Lee 2013 [61] | 1997–2011 | TLM (ELS I–VI) | T1–T2 | AC+ 33 AC− 85 | Mean 69.4 | AC+ 80.9 AC− 91.1 p= 0.583 | AC+ 88.7 AC− 91.6 p = 0.883 | ||
| Mortuaire 2006 [33] | 1990–2000 | TLM (ELS I–V) | Tis–T2 | AC+ 22 AC− 88 | Median 42 | UVA NS | |||
| Peretti 2000 [62] | 1987–1994 | TLM (I–V) | Tis–T2 | AC+ 40 AC− 98 | Mean 76 | AC + 72 AC− 86 p = 0.2 | |||
| Peretti 2001 [63] | 1995–1997 | TLM (I–V) | Tis–T1 | AC+ 12 AC− 76 | Mean 43 | AC+ 83 AC− 87 p = 0.7 | |||
| Peretti 2010 [3] | 1988–2005 | TLM (ELS I–V) | Tis–T1 | AC+ 84 AC− 391 | Mean 84 | AC+ 100 AC–99.2 p = 0.44 | AC+ 100 AC− 98.9 p = 0.27 | AC+ 98.8 AC− 98.1 p = 0.57 | |
| Peretti 2013 [64] | 2005–2010 | TLM (ELS Type V) | T2–T3 | AC+ 4 AC− 85 | Minimal 18 | AC+ 59 AC− 62 NS | AC+ 96 AC− 75 NS | ||
| Rodel 2009 [28] | 1986–2004 | TLM (nfs) | T1–T2 | T1a AC+ 55 T1a AC− 237 T1b AC+ 34 T1b AC− 16 T2 AC+ 64 T2 AC− 38 | Median 65 | T1a: 73 vs. 89 p = 0.06 T1b: 68 vs. 86 p = 0.32 T2: 76 vs. 76 | T1a: 85 vs. 87 T1b: 93 vs. 72 T2: 80 vs. 59 NS | T1a: 95 vs. 98 T1b: 88 vs. 100 T2: 89 vs. 95 no p–value | |
| Rucci 2010 [31] | 2003–2007 | TLM (ELS I–V) | Tis–T1 | AC0 48 AC1 20 AC2 13 AC3 0 | Mean 24.2 | UVA p =0.0119 MVA OR 5.14 p = 0.036 | |||
| Sachse 2009 [65] | 1995–2005 | TLM (ELS II–Va) | T1 | AC+ 14 AC− 32 | Median 36 | AC+ 42 AC− 87 NS | AC+ 67 AC− 100 | ||
| Son 2018 [32] | 2009–2014 | TLM (ELS I–VI) | T1–T2 | AC+ 25 AC− 48 | Median 44 | HR 3.45 p =0.030 MVA 1.03 p = 0.964 | 1.96 p = 0.412 | ||
| Steiner 2004 [23] | 1986–1996 | TLM (proposal by Steiner) | T1–T2 | T1a AC+ 28 T1a AC− 130 T1b AC+ 16 T1b AC− 14 T2 AC+ 45 T2 AC− 30 | Median 63.9 | T1a: 84 vs. 90 T1b: 73 vs. 92 T2: 79 vs. 74 All p–value > 0.05 | T1a: 87 vs. 86 T1b: 100 vs. 70 T2: 80 vs. 56 no p–value | T1a: 93 vs. 99 T1b: 88 vs. 100 T2: 93 vs. 97 no p–value | |
| Wolber 2017 [24] | 1992–2002 | TLM (proposal by Steiner) | T1–T2 | AC+ 21 AC–28 | Mean 62.0 | AC+ 57.1 AC− 92.9 p < 0.01 | AC+ 90.5 AC− 96.4 p = 0.39 |
| Heading Title | n | T1 | n | T2 | n | T1–T2 | |
|---|---|---|---|---|---|---|---|
| Radiotherapy | AC+ AC– | 1033 2064 | 82.2 89.1 | 330 202 | 68.2 75.7 | 1140 1592 | 78.2 86.8 |
| TLM | AC+ AC– | 147 429 | 70.1 89.1 | 109 68 | 77.2 75.1 | 123 165 | 77.3 91.1 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hendriksma, M.; Sjögren, E.V. Involvement of the Anterior Commissure in Early Glottic Cancer (Tis-T2): A Review of the Literature. Cancers 2019, 11, 1234. https://doi.org/10.3390/cancers11091234
Hendriksma M, Sjögren EV. Involvement of the Anterior Commissure in Early Glottic Cancer (Tis-T2): A Review of the Literature. Cancers. 2019; 11(9):1234. https://doi.org/10.3390/cancers11091234
Chicago/Turabian StyleHendriksma, Martine, and Elisabeth V. Sjögren. 2019. "Involvement of the Anterior Commissure in Early Glottic Cancer (Tis-T2): A Review of the Literature" Cancers 11, no. 9: 1234. https://doi.org/10.3390/cancers11091234
APA StyleHendriksma, M., & Sjögren, E. V. (2019). Involvement of the Anterior Commissure in Early Glottic Cancer (Tis-T2): A Review of the Literature. Cancers, 11(9), 1234. https://doi.org/10.3390/cancers11091234





