Utility of FIB4-T as a Prognostic Factor for Hepatocellular Carcinoma
Abstract
:1. Introduction
2. Patients and Methods
2.1. Patients
2.2. Construction of FIB4-T
2.3. Evaluation of Scores
2.4. Statistics
3. Results
3.1. Patient Characteristics
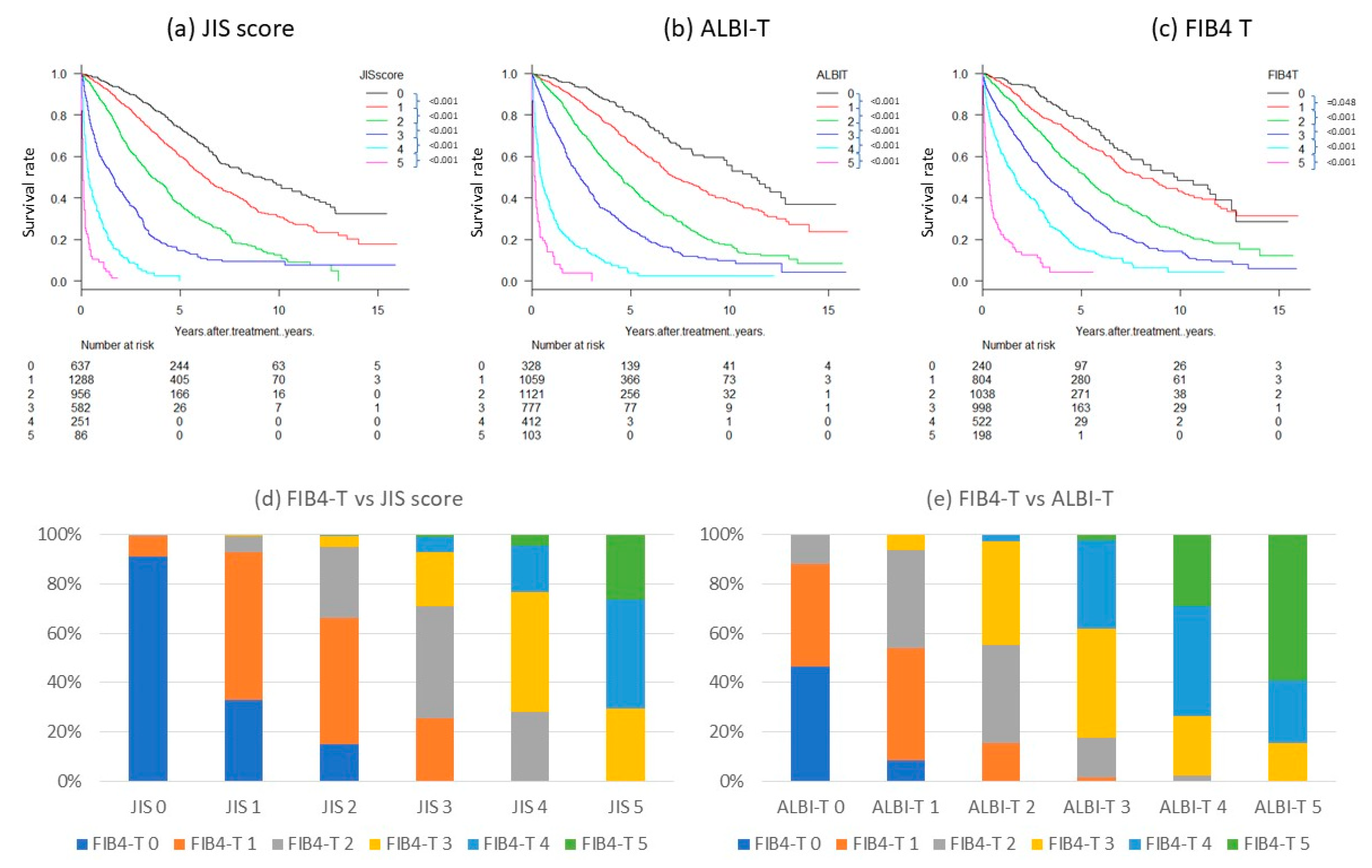
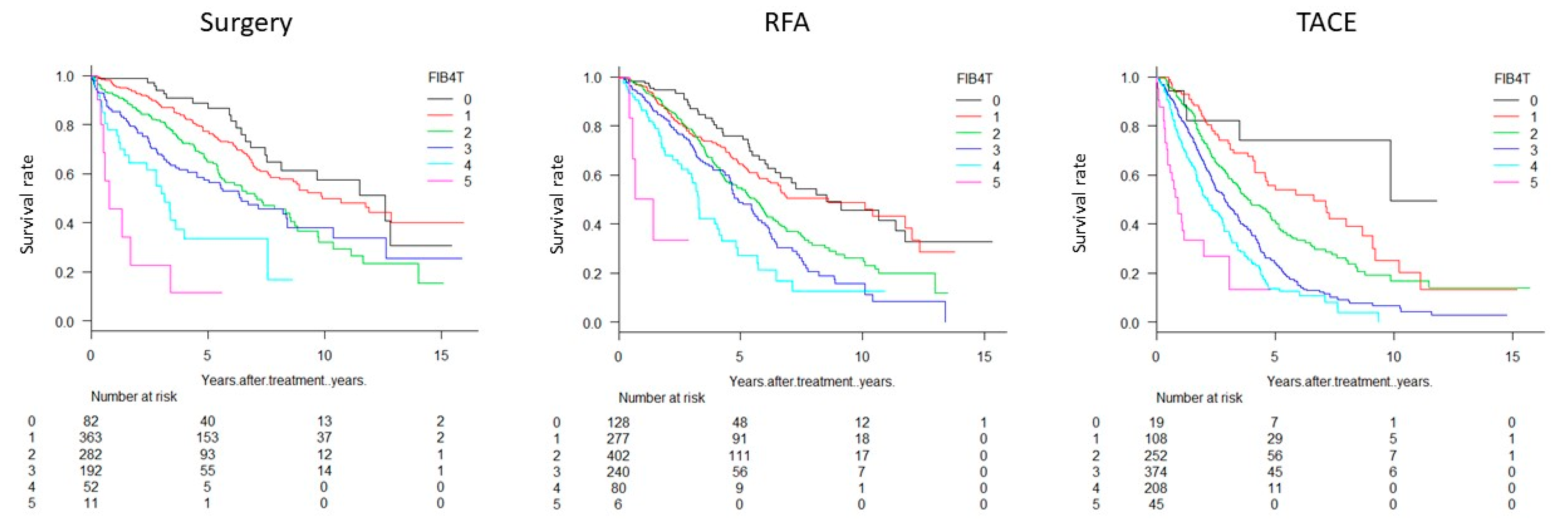
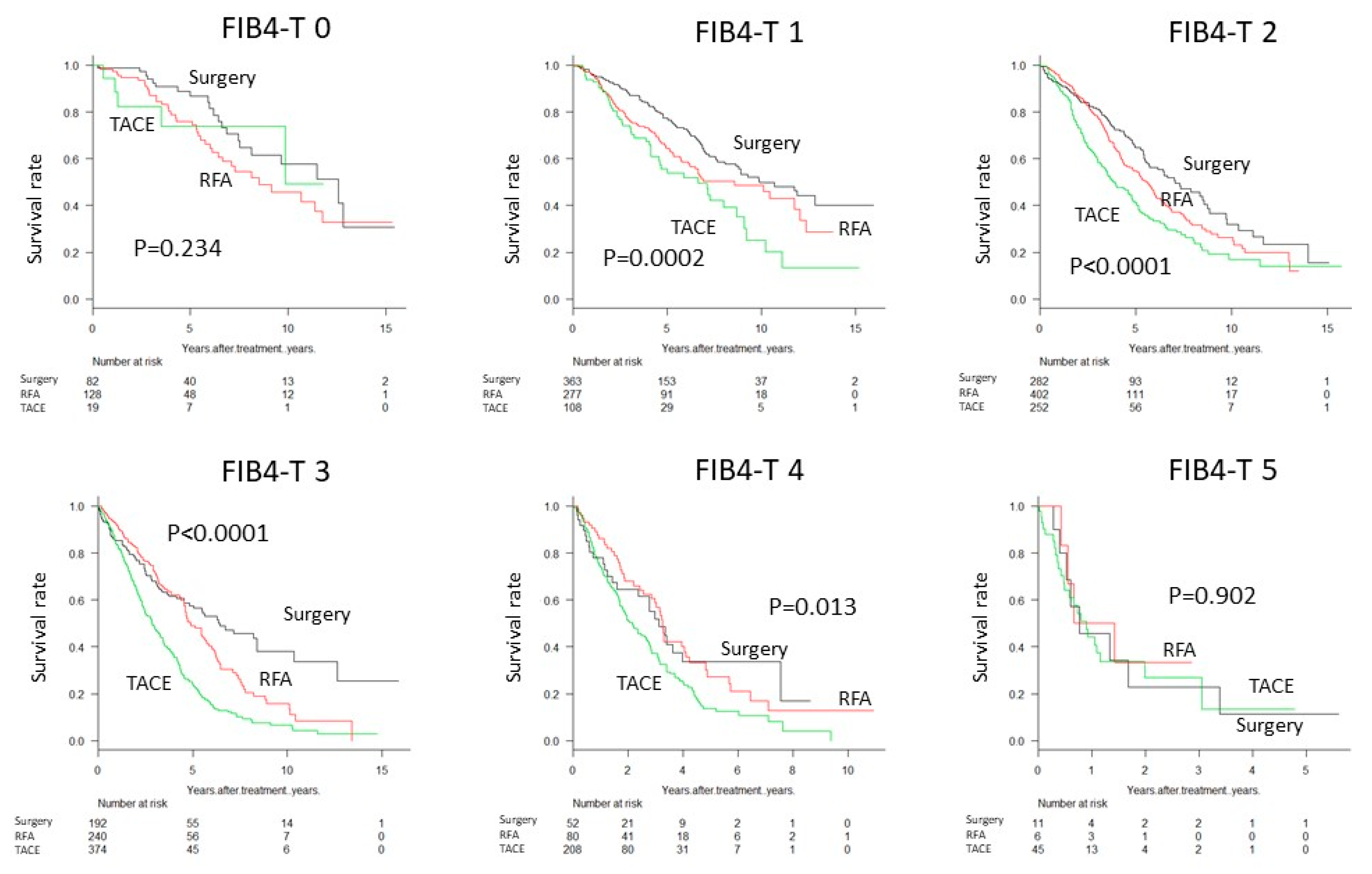
3.2. Patient Survival
3.3. Stratification of FIB4-T Population
3.4. Risk of Mortality Based on FIB4-T
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Global Burden of Disease Cancer Collaboration; Fitzmaurice, C.; Allen, C.; Barber, R.M.; Barregard, L.; Bhutta, Z.A.; Brenner, H.; Dicker, D.J.; Chimed-Orchir, O.; Dandona, R.; et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: A systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2017, 3, 524–548. [Google Scholar] [PubMed]
- Okuda, K.; Ohtsuki, T.; Obata, H.; Tomimatsu, M.; Okazaki, N.; Hasegawa, H.; Nakajima, Y.; Ohnishi, K. Natural history of hepatocellular carcinoma and prognosis in relation to treatment. Study of 850 patients. Cancer 1985, 56, 918–928. [Google Scholar] [CrossRef]
- The Cancer of the Liver Italian Program [CLIP] investigators. A new prognostic system for hepatocellular carcinoma: A retrospective study of 435 patients. Hepatology 1998, 28, 751–755. [Google Scholar] [CrossRef]
- Tateishi, R.; Yoshida, H.; Shiina, S.; Imamura, H.; Hasegawa, K.; Teratani, T.; Obi, S.; Sato, S.; Koike, Y.; Fujishima, T.; et al. Proposal of a new prognostic model for hepatocellular carcinoma: An analysis of 403 patients. Gut 2005, 54, 419–425. [Google Scholar] [CrossRef]
- Kudo, M.; Chung, H.; Osaki, Y. Prognostic staging system for hepatocellular carcinoma [CLIP score]: Its value and limitations, and a proposal for a new staging system, the Japan Integrated Staging Score [JIS score]. J. Gastroenterol. 2003, 38, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Hiraoka, A.; Kumada, T.; Kudo, M.; Hirooka, M.; Tsuji, K.; Itobayashi, E.; Kariyama, K.; Ishikawa, T.; Tajiri, K.; Ochi, H.; et al. Albumin-Bilirubin [ALBI] Grade as Part of the Evidence-Based Clinical Practice Guideline for HCC of the Japan Society of Hepatology: A Comparison with the Liver Damage and Child-Pugh Classifications. Liver Cancer 2017, 6, 204–215. [Google Scholar] [CrossRef] [PubMed]
- Nagaoki, Y.; Aikata, H.; Nakano, N.; Shinohara, F.; Nakamura, Y.; Hatooka, M.; Morio, K.; Kan, H.; Fujino, H.; Kobayashi, T.; et al. Development of hepatocellular carcinoma in patients with hepatitis C virus infection who achieved sustained virological response following interferon therapy: A large-scale, long-term cohort study. J. Gastroenterol. Hepatol. 2016, 31, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Sterling, R.K.; Lissen, E.; Clumeck, N.; Sola, R.; Correa, M.C.; Montaner, J.; Sulkowski, M.S.; Torriani, F.J.; Dieterich, D.T.; Thomas, D.L.; et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology 2006, 43, 1317–1325. [Google Scholar] [CrossRef]
- Shah, A.G.; Lydecker, A.; Murray, K.; Tetri, B.N.; Contos, M.J.; Sanyal, A.J.; Nash Clinical Research Network. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin. Gastroenterol. Hepatol. 2009, 7, 1104–1112. [Google Scholar] [CrossRef]
- Bruix, J.; Sherman, M. Management of hepatocellular carcinoma. Hepatology 2005, 42, 1208–1236. [Google Scholar] [CrossRef]
- Kudo, M.; Kitano, M.; Sakurai, T.; Nishida, N. General rules for the clinical and pathological study of primary liver cancer, nationwide follow-up survey and clinical practice guidelines: The outstanding achievements of the Liver Cancer Study Group of Japan. Dig. Dis. 2015, 33, 765–770. [Google Scholar] [CrossRef] [PubMed]
- Liver Cancer Study Group of Japan. The General Rules for the Clinical and Pathological Study of Primary Liver Cancer, 6th ed.; Kanehara & Co.: Tokyo, Japan, 2015; pp. 26–30. [Google Scholar]
- Sumida, Y.; Yoneda, M.; Hyogo, H.; Itoh, Y.; Ono, M.; Fujii, H.; Eguchi, Y.; Suzuki, Y.; Aoki, N.; Kanemasa, K.; et al. Validation of the FIB4 index in a Japanese nonalcoholic fatty liver disease population. BMC Gastroenterol. 2012. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, A.C.; El-Bacha, I.; Vianna, M.V.; Parise, E.R. Utility and limitations of APRI and FIB4 to predict staging in a cohort of nonselected outpatients with hepatitis C. Ann. Hepatol. 2016, 15, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, H.; Sugimoto, K.; Oshiro, H.; Iwatsuka, K.; Kono, S.; Yoshimasu, Y.; Kasai, Y.; Furuichi, Y.; Sakamaki, K.; Itoi, T. Liver fibrosis: Noninvasive assessment using supersonic shear imaging and FIB4 index in patients with non-alcoholic fatty liver disease. J. Med. Ultrason. 2017, 45, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Kanda, Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef]
- R Development Core Team RFfSC. R: A Language and Environment for Statistical Computing; The R Foundation for Statistical Computing: Vienna, Austria, 2005. [Google Scholar]
- Adams, L.A.; George, J.; Bugianesi, E.; Rossi, E.; De Boer, W.B.; van der Poorten, D.; Ching, H.L.; Bulsara, M.; Jeffrey, G.P. Complex non-invasive fibrosis models are more accurate than simple models in non-alcoholic fatty liver disease. J. Gastroenterol. Hepatol. 2011, 26, 1536–1543. [Google Scholar] [CrossRef] [PubMed]
- Tahiri, M.; Sodqi, M.; Lahdami, F.E.; Marih, L.; Lamdini, H.; Hliwa, W.; Lahcen, A.O.; Badre, W.; Haddad, F.; Chakib, A.; et al. Risk factors for liver fibrosis among human immunodeficiency virus monoinfected patients using the FIB4 index in Morocco. World J. Hepatol. 2013, 5, 584–588. [Google Scholar] [CrossRef]
- Chrostek, L.; Panasiuk, A. Liver fibrosis markers in alcoholic liver disease. World J. Gastroenterol. 2014, 20, 8018–8023. [Google Scholar] [CrossRef]
- Arrayhani, M.; Sqalli, T.; Tazi, N.; El Youbi, R.; Chaouch, S.; Aqodad, N.; Ibrahimi, S.A. Non invasive assessment of liver fibrosis in chronic hemodialysis patients with viral hepatitis C. Pan. Afr. Med. J. 2015, 22, 273. [Google Scholar] [CrossRef]
- Mussini, C.; Lorenzini, P.; Puoti, M.; Lichtner, M.; Lapadula, G.; Di Giambenedetto, S.; Antinori, A.; Madeddu, G.; Cozzi-Lepri, A.; d’Arminio Monforte, A.; et al. Prognostic value of the Fibrosis-4 Index in human immunodeficiency virus type-1 infected patients initiating antiretroviral therapy with or without hepatitis C virus. PLoS ONE 2015, 10, e0140877. [Google Scholar] [CrossRef]
- Okamura, Y.; Ashida, R.; Yamamoto, Y.; Ito, T.; Sugiura, T.; Uesaka, K. FIB-4 Index is a predictor of background liver fibrosis and long-term outcomes after curative resection of hepatocellular carcinoma. Ann. Surg. Oncol. 2016, 23, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Akuta, N.; Kobayashi, M.; Suzuki, F.; Sezaki, H.; Fujiyama, S.; Kawamura, Y.; Hosaka, T.; Kobayashi, M.; Saitoh, S.; Suzuki, Y.; et al. Liver fibrosis and body mass index predict hepatocarcinogenesis following eradication of hepatitis C virus RNA by direct-acting antivirals. Oncology 2016, 91, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Sato, Y.; Yoshihisa, A.; Kanno, Y.; Watanabe, S.; Yokokawa, T.; Abe, S.; Misaka, T.; Sato, T.; Suzuki, S.; Oikawa, M.; et al. Liver stiffness assessed by Fibrosis-4 index predicts mortality in patients with heart failure. Open Heart 2017, 4, e000598. [Google Scholar] [CrossRef] [PubMed]
- Owens, D.; Evans, J. Population studies on Gilbert’s syndrome. J. Med. Genet. 1975, 12, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, H.; Shiratori, Y.; Moriyama, M.; Arakawa, Y.; Ide, T.; Sata, M.; Inoue, O.; Yano, M.; Tanaka, M.; Fujiyama, S.; et al. Interferon therapy reduces the risk for hepatocellular carcinoma: National surveillance program of cirrhotic and noncirrhotic patients with chronic hepatitis C in Japan. IHIT Study Group. Inhibition of hepatocarcinogenesis by interferon therapy. Ann. Intern. Med. 1999, 131, 174–181. [Google Scholar] [CrossRef] [PubMed]

| FIB4 Grade | ||||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| TNM stage by LCSGJ | I | FIB4-T 0 | FIB4-T 1 | FIB4-T 2 |
| II | FIB4-T 1 | FIB4-T 2 | FIB4-T 3 | |
| III | FIB4-T 2 | FIB4-T 3 | FIB4-T 4 | |
| IV | FIB4-T 3 | FIB4-T 4 | FIB4-T 5 | |
| Variable | Value | % |
|---|---|---|
| Age, year (median (range) | 70 (21–98) | |
| Sex (male) | 2779 | 73.1 |
| Cause of parenchymal disorder | ||
| HBV | 421 | 11.1 |
| HCV | 2566 | 67.5 |
| Non-B, Non-C | 777 | 20.4 |
| Child–Pugh stage | ||
| A | 2660 | 70.0 |
| B | 918 | 24.2 |
| C | 222 | 5.8 |
| FIB4 grade (FIB4 index), n | ||
| 1 (–3.25) | 1107 | 29.1 |
| 2 (3.26–6.70) | 1452 | 38.2 |
| 3 (6.71–) | 1241 | 32.7 |
| TNM stage by LCSGJ | ||
| I | 816 | 21.5 |
| II | 1522 | 40.1 |
| III | 890 | 23.4 |
| IV | 572 | 15.1 |
| Initial treatment modality | ||
| Surgery | 982 | 25.8 |
| Percutaneous ablation therapy | 1201 | 31.6 |
| PEIT | 68 | 1.8 |
| RFA | 1133 | 29.8 |
| TACE | 1006 | 26.5 |
| Others | 237 | 6.2 |
| BSC | 474 | 12.5 |
| Factor | Patients Number | Survival Rate (%) | MST, Year | |||
|---|---|---|---|---|---|---|
| 1 Year | 3 Years | 5 Years | ||||
| FIB4-T | 0 | 240 | 97 | 88 | 77 | 9.6 |
| 1 | 804 | 94 | 80 | 66 | 8.0 | |
| 2 | 1038 | 92 | 72 | 51 | 5.2 | |
| 3 | 998 | 78 | 55 | 35 | 3.4 | |
| 4 | 522 | 60 | 36 | 14 | 1.8 | |
| 5 | 198 | 20 | 10 | 5 | 0.3 | |
| FIB4 grade | 1 | 1107 | 88 | 69 | 59 | 6.8 |
| 2 | 1452 | 84 | 62 | 48 | 4.6 | |
| 3 | 1241 | 77 | 52 | 32 | 3.2 | |
| TNM stage by LCSGJ | I | 816 | 95 | 80 | 65 | 7.2 |
| II | 1522 | 91 | 72 | 54 | 5.4 | |
| III | 890 | 81 | 49 | 29 | 2.8 | |
| IV | 572 | 33 | 17 | 9 | 0.4 | |
| Integrated Score | Likelihood Ratio χ2 | Akaike Information Criterion |
|---|---|---|
| FIB4-T | 765 | 26,460 |
| JIS score | 1208 | 26,018 |
| ALBI-T | 1168 | 26,058 |
| Variables | Relative Risk | 95%CI | p-Value | |
|---|---|---|---|---|
| FIB4-T | 0→1 | 1.303 | 1.002–1.695 | 0.048 |
| 1→2 | 1.679 | 1.445–1.951 | <0.001 | |
| 2→3 | 1.645 | 1.455–1.861 | <0.001 | |
| 3→4 | 1.804 | 1.573–2.069 | <0.001 | |
| 4→5 | 2.791 | 2.265–3.440 | <0.001 | |
| JIS score | 0→1 | 1.579 | 1.340–1.860 | <0.001 |
| 1→2 | 1.968 | 1.738–2.227 | <0.001 | |
| 2→3 | 2.143 | 1.868–2.458 | <0.001 | |
| 3→4 | 2.573 | 2.141–3.092 | <0.001 | |
| 4→5 | 2.583 | 1.955–3.411 | <0.001 | |
| ALBI-T | 0→1 | 1.667 | 1.315–2.113 | <0.001 |
| 1→2 | 1.909 | 1.673–2.177 | <0.001 | |
| 2→3 | 1.865 | 1.646–2.113 | <0.001 | |
| 3→4 | 3.039 | 2.607–3.543 | <0.001 | |
| 4→5 | 2.377 | 1.846–3.060 | <0.001 | |
| AFP | >400 ng/mL | 2.499 | 2.223–2.808 | <0.001 |
| PIVKA-II | >200 mAU/mL | 2.588 | 2.338–2.865 | <0.001 |
| Portal invasion | positive | 5.384 | 4.277–6.776 | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kariyama, K.; Nouso, K.; Toyoda, H.; Tada, T.; Hiraoka, A.; Tsuji, K.; Itobayashi, E.; Ishikawa, T.; Wakuta, A.; Oonishi, A.; et al. Utility of FIB4-T as a Prognostic Factor for Hepatocellular Carcinoma. Cancers 2019, 11, 203. https://doi.org/10.3390/cancers11020203
Kariyama K, Nouso K, Toyoda H, Tada T, Hiraoka A, Tsuji K, Itobayashi E, Ishikawa T, Wakuta A, Oonishi A, et al. Utility of FIB4-T as a Prognostic Factor for Hepatocellular Carcinoma. Cancers. 2019; 11(2):203. https://doi.org/10.3390/cancers11020203
Chicago/Turabian StyleKariyama, Kazuya, Kazuhiro Nouso, Hidenori Toyoda, Toshifumi Tada, Atsushi Hiraoka, Kunihiko Tsuji, Ei Itobayashi, Toru Ishikawa, Akiko Wakuta, Ayano Oonishi, and et al. 2019. "Utility of FIB4-T as a Prognostic Factor for Hepatocellular Carcinoma" Cancers 11, no. 2: 203. https://doi.org/10.3390/cancers11020203
APA StyleKariyama, K., Nouso, K., Toyoda, H., Tada, T., Hiraoka, A., Tsuji, K., Itobayashi, E., Ishikawa, T., Wakuta, A., Oonishi, A., Kumada, T., & Kudo, M., on behalf of the Real-Life Practice Experts for HCC (RELPEC) Study Group and HCC 48 Group. (2019). Utility of FIB4-T as a Prognostic Factor for Hepatocellular Carcinoma. Cancers, 11(2), 203. https://doi.org/10.3390/cancers11020203








