Low Systemic Levels of Chemokine C-C Motif Ligand 3 (CCL3) are Associated with a High Risk of Venous Thromboembolism in Patients with Glioma
Abstract
:1. Introduction
2. Results
2.1. Baseline Characteristic of the Study Population
2.2. VTE Events during Follow-Up
2.3. Serum Cytokine Levels and Risk of VTE
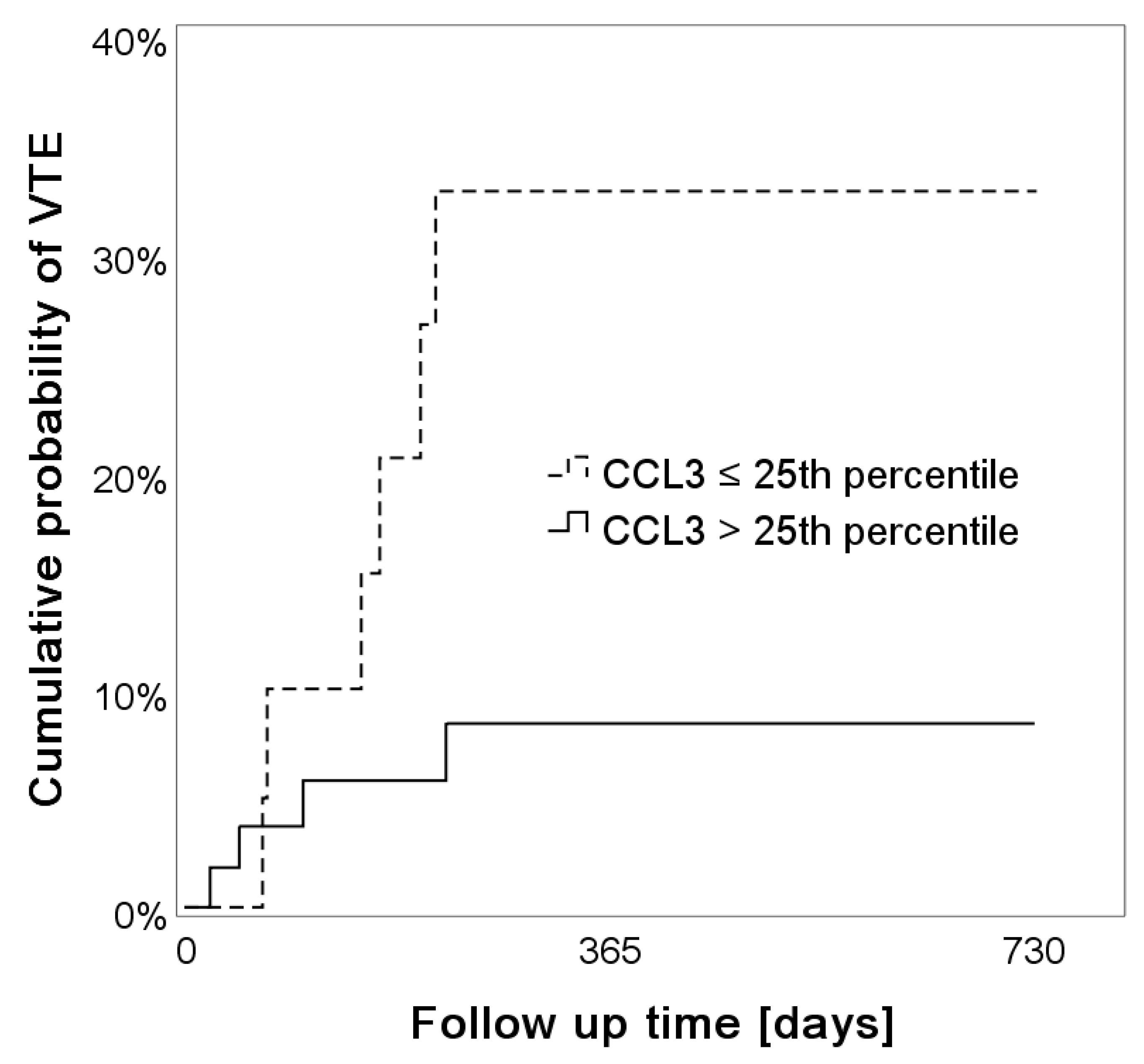
2.4. Low Levels of Systemic CCL3 Predict the Risk of VTE
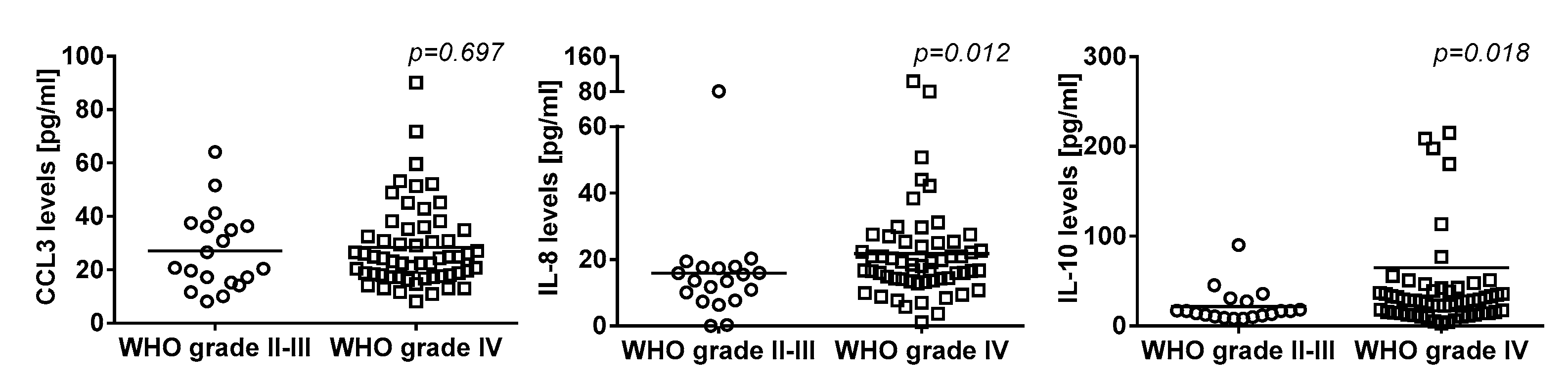
2.5. Association of Systemic Cytokine Levels and Tumor Grade
3. Discussion
4. Materials and Methods
4.1. Vienna Cancer and Thrombosis Study (CATS)
4.2. Blood Sampling
4.3. Serum Cytokine Levels
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Michota, F. Venous thromboembolism: Epidemiology, characteristics, and consequences. Clin. Cornerstone 2005, 7, 8–15. [Google Scholar] [CrossRef]
- Tagalakis, V.; Patenaude, V.; Kahn, S.R.; Suissa, S. Incidence of and mortality from venous thromboembolism in a real-world population: The Q-VTE Study Cohort. Am. J. Med. 2013, 126, 832.e13–832.e21. [Google Scholar] [CrossRef] [PubMed]
- Falanga, A.; Russo, L. Epidemiology, risk and outcomes of venous thromboembolism in cancer. Hamostaseologie 2012, 32, 115–125. [Google Scholar] [PubMed]
- Ay, C.; Pabinger, I.; Cohen, A.T. Cancer-associated venous thromboembolism: Burden, mechanisms, and management. Thromb. Haemost. 2017, 117, 219–230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mauracher, L.-M.; Posch, F.; Martinod, K.; Grilz, E.; Däullary, T.; Hell, L.; Brostjan, C.; Zielinski, C.; Ay, C.; Wagner, D.D.; et al. Citrullinated histone H3, a biomarker of neutrophil extracellular trap formation, predicts the risk of venous thromboembolism in cancer patients. J. Thromb. Haemost. 2018, 16, 508–518. [Google Scholar] [CrossRef] [PubMed]
- Branchford, B.R.; Carpenter, S.L. The Role of Inflammation in Venous Thromboembolism. Front. Pediatr. 2018, 6, 142. [Google Scholar] [CrossRef]
- Saghazadeh, A.; Hafizi, S.; Rezaei, N. Inflammation in venous thromboembolism: Cause or consequence? Int. Immunopharmacol. 2015, 28, 655–665. [Google Scholar] [CrossRef]
- Joseph, L.; Fink, L.M.; Hauer-Jensen, M. Cytokines in coagulation and thrombosis: A preclinical and clinical review. Blood Coagul. Fibrinolysis 2002, 13, 105–116. [Google Scholar] [CrossRef]
- Turner, M.D.; Nedjai, B.; Hurst, T.; Pennington, D.J. Cytokines and chemokines: At the crossroads of cell signalling and inflammatory disease. Biochim. Biophys. Acta 2014, 1843, 2563–2582. [Google Scholar] [CrossRef] [Green Version]
- Neumann, F.J.; Ott, I.; Marx, N.; Luther, T.; Kenngott, S.; Gawaz, M.; Kotzsch, M.; Schömig, A. Effect of human recombinant interleukin-6 and interleukin-8 on monocyte procoagulant activity. Arterioscler. Thromb. Vasc. Biol. 1997, 17, 3399–3405. [Google Scholar] [CrossRef]
- Alfaro, C.; Teijeira, A.; Oñate, C.; Pérez, G.; Sanmamed, M.F.; Andueza, M.P.; Alignani, D.; Labiano, S.; Azpilikueta, A.; Rodriguez-Paulete, A.; et al. Tumor-Produced Interleukin-8 Attracts Human Myeloid-Derived Suppressor Cells and Elicits Extrusion of Neutrophil Extracellular Traps (NETs). Clin. Cancer Res. 2016, 22, 3924–3936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Von Brühl, M.-L.; Stark, K.; Steinhart, A.; Chandraratne, S.; Konrad, I.; Lorenz, M.; Khandoga, A.; Tirniceriu, A.; Coletti, R.; Köllnberger, M.; et al. Monocytes, neutrophils, and platelets cooperate to initiate and propagate venous thrombosis in mice in vivo. J. Exp. Med. 2012, 209, 819–835. [Google Scholar] [CrossRef] [PubMed]
- Abdol Razak, N.; Elaskalani, O.; Metharom, P. Pancreatic Cancer-Induced Neutrophil Extracellular Traps: A Potential Contributor to Cancer-Associated Thrombosis. Int. J. Mol. Sci. 2017, 18, 487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hawbaker, S. Venous thromboembolism in the cancer population: Pathology, risk, and prevention. J. Adv. Pract. Oncol. 2012, 3, 23–33. [Google Scholar]
- Fukuyama, T.; Ichiki, Y.; Yamada, S.; Shigematsu, Y.; Baba, T.; Nagata, Y.; Mizukami, M.; Sugaya, M.; Takenoyama, M.; Hanagiri, T.; et al. Cytokine production of lung cancer cell lines: Correlation between their production and the inflammatory/immunological responses both in vivo and in vitro. Cancer Sci. 2007, 98, 1048–1054. [Google Scholar] [CrossRef]
- Kumar, S.; Kumari, N.; Mittal, R.D.; Mohindra, S.; Ghoshal, U.C. Association between pro-(IL-8) and anti-inflammatory (IL-10) cytokine variants and their serum levels and H. pylori-related gastric carcinogenesis in northern India. Meta Gene 2015, 6, 9–16. [Google Scholar] [CrossRef]
- Orditura, M.; De Vita, F.; Catalano, G.; Infusino, S.; Lieto, E.; Martinelli, E.; Morgillo, F.; Castellano, P.; Pignatelli, C.; Galizia, G. Elevated serum levels of interleukin-8 in advanced non-small cell lung cancer patients: Relationship with prognosis. J. Interferon Cytokine Res. 2002, 22, 1129–1135. [Google Scholar] [CrossRef]
- Semrad, T.J.; O’Donnell, R.; Wun, T.; Chew, H.; Harvey, D.; Zhou, H.; White, R.H. Epidemiology of venous thromboembolism in 9489 patients with malignant glioma. J. Neurosurg. 2007, 106, 601–608. [Google Scholar] [CrossRef]
- Riedl, J.; Preusser, M.; Nazari, P.M.S.; Posch, F.; Panzer, S.; Marosi, C.; Birner, P.; Thaler, J.; Brostjan, C.; Lötsch, D.; et al. Podoplanin expression in primary brain tumors induces platelet aggregation and increases risk of venous thromboembolism. Blood 2017, 129, 1831–1839. [Google Scholar] [CrossRef] [Green Version]
- Unruh, D.; Schwarze, S.R.; Khoury, L.; Thomas, C.; Wu, M.; Chen, L.; Chen, R.; Liu, Y.; Schwartz, M.A.; Amidei, C.; et al. Mutant IDH1 and thrombosis in gliomas. Acta Neuropathol. (Berl.) 2016, 132, 917–930. [Google Scholar] [CrossRef] [Green Version]
- Mir Seyed Nazari, P.; Riedl, J.; Preusser, M.; Posch, F.; Thaler, J.; Marosi, C.; Birner, P.; Ricken, G.; Hainfellner, J.A.; Pabinger, I.; et al. Combination of isocitrate dehydrogenase 1 (IDH1) mutation and podoplanin expression in brain tumors identifies patients at high or low risk of venous thromboembolism. J. Thromb. Haemost. 2018, 16, 1121–1127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thaler, J.; Ay, C.; Kaider, A.; Reitter, E.-M.; Haselböck, J.; Mannhalter, C.; Zielinski, C.; Marosi, C.; Pabinger, I. Biomarkers predictive of venous thromboembolism in patients with newly diagnosed high-grade gliomas. Neuro-Oncology 2014, 16, 1645–1651. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riedl, J.; Ay, C. Venous Thromboembolism in Brain Tumors: Risk Factors, Molecular Mechanisms, and Clinical Challenges. Semin. Thromb. Hemost. 2019, 45, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, A.; Gruen, M.L.; Gutierrez, D.A.; Surmi, B.K.; Orr, J.S.; Webb, C.D.; Hasty, A.H. Impact of macrophage inflammatory protein-1α deficiency on atherosclerotic lesion formation, hepatic steatosis, and adipose tissue expansion. PLoS ONE 2012, 7, e31508. [Google Scholar] [CrossRef]
- Menten, P.; Wuyts, A.; Van Damme, J. Macrophage inflammatory protein-1. Cytokine Growth Factor Rev. 2002, 13, 455–481. [Google Scholar] [CrossRef]
- Collins, K.S.; Balasubramaniam, K.; Viswanathan, G.; Natasari, A.; Tarn, J.; Lendrem, D.; Mitchell, S.; Zaman, A.; Ng, W.F. Assessment of blood clot formation and platelet receptor function ex vivo in patients with primary Sjogren’s syndrome. BMJ Open 2013, 3, 002739. [Google Scholar] [CrossRef]
- Kawao, N.; Tamura, Y.; Horiuchi, Y.; Okumoto, K.; Yano, M.; Okada, K.; Matsuo, O.; Kaji, H. The Tissue Fibrinolytic System Contributes to the Induction of Macrophage Function and CCL3 during Bone Repair in Mice. PLoS ONE 2015, 10, e0123982. [Google Scholar] [CrossRef] [Green Version]
- Xu, B.J.; An, Q.A.; Srinivasa Gowda, S.; Yan, W.; Pierce, L.A.; Abel, T.W.; Rush, S.Z.; Cooper, M.K.; Ye, F.; Shyr, Y.; et al. Identification of blood protein biomarkers that aid in the clinical assessment of patients with malignant glioma. Int. J. Oncol. 2012, 40, 1995–2003. [Google Scholar] [CrossRef] [Green Version]
- Owens, A.P.; Mackman, N. Tissue factor and thrombosis: The clot starts here. Thromb. Haemost. 2010, 104, 432–439. [Google Scholar] [CrossRef]
- Osnes, L.T.; Westvik, A.B.; Joø, G.B.; Okkenhaug, C.; Kierulf, P. Inhibition of IL-1 induced tissue factor (TF) synthesis and procoagulant activity (PCA) in purified human monocytes by IL-4, IL-10 and IL-13. Cytokine 1996, 8, 822–827. [Google Scholar] [CrossRef]
- Mosevoll, K.A.; Johansen, S.; Wendelbo, Ø.; Nepstad, I.; Bruserud, Ø.; Reikvam, H. Cytokines, Adhesion Molecules, and Matrix Metalloproteases as Predisposing, Diagnostic, and Prognostic Factors in Venous Thrombosis. Front. Med. 2018, 5, 147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bode, M.; Mackman, N. Regulation of tissue factor gene expression in monocytes and endothelial cells: Thromboxane A2 as a new player. Vasc. Pharmacol. 2014, 62, 57–62. [Google Scholar] [CrossRef] [Green Version]
- Kamimura, M.; Viedt, C.; Dalpke, A.; Rosenfeld, M.E.; Mackman, N.; Cohen, D.M.; Blessing, E.; Preusch, M.; Weber, C.M.; Kreuzer, J.; et al. Interleukin-10 suppresses tissue factor expression in lipopolysaccharide-stimulated macrophages via inhibition of Egr-1 and a serum response element/MEK-ERK1/2 pathway. Circ. Res. 2005, 97, 305–313. [Google Scholar] [CrossRef] [Green Version]
- Brill, A.; Fuchs, T.A.; Savchenko, A.S.; Thomas, G.M.; Martinod, K.; De Meyer, S.F.; Bhandari, A.A.; Wagner, D.D. Neutrophil extracellular traps promote deep vein thrombosis in mice. J. Thromb. Haemost. 2012, 10, 136–144. [Google Scholar] [CrossRef] [Green Version]
- Martinod, K.; Wagner, D.D. Thrombosis: Tangled up in NETs. Blood 2014, 123, 2768–2776. [Google Scholar] [CrossRef]
- Martinod, K.; Demers, M.; Fuchs, T.A.; Wong, S.L.; Brill, A.; Gallant, M.; Hu, J.; Wang, Y.; Wagner, D.D. Neutrophil histone modification by peptidylarginine deiminase 4 is critical for deep vein thrombosis in mice. Proc. Natl. Acad. Sci. USA 2013, 110, 8674–8679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Aken, B.E.; Reitsma, P.H.; Rosendaal, F.R. Interleukin 8 and venous thrombosis: Evidence for a role of inflammation in thrombosis. Br. J. Haematol. 2002, 116, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Gao, Q.; Zhang, P.; Wang, W.; Ma, H.; Tong, Y.; Zhang, J.; Lu, Z. The correlation analysis of tumor necrosis factor-alpha-308G/A polymorphism and venous thromboembolism risk: A meta-analysis. Phlebology 2016, 31, 625–631. [Google Scholar] [CrossRef]
- Jezovnik, M.K.; Poredos, P. Idiopathic venous thrombosis is related to systemic inflammatory response and to increased levels of circulating markers of endothelial dysfunction. Int. Angiol. 2010, 29, 226–231. [Google Scholar]
- Mahemuti, A.; Abudureheman, K.; Aihemaiti, X.; Hu, X.; Xia, Y.; Tang, B.; Upur, H. Association of interleukin-6 and C-reactive protein genetic polymorphisms levels with venous thromboembolism. Chin. Med. J. (Engl.) 2012, 125, 3997–4002. [Google Scholar]
- Matos, M.F.; Lourenço, D.M.; Orikaza, C.M.; Bajerl, J.A.H.; Noguti, M.A.E.; Morelli, V.M. The role of IL-6, IL-8 and MCP-1 and their promoter polymorphisms IL-6 -174GC, IL-8 -251AT and MCP-1 -2518AG in the risk of venous thromboembolism: A case-control study. Thromb. Res. 2011, 128, 216–220. [Google Scholar] [CrossRef] [PubMed]
- Roumen-Klappe, E.M.; den Heijer, M.; van Uum, S.H.M.; van der Ven-Jongekrijg, J.; van der Graaf, F.; Wollersheim, H. Inflammatory response in the acute phase of deep vein thrombosis. J. Vasc. Surg. 2002, 35, 701–706. [Google Scholar] [CrossRef] [Green Version]
- Malaponte, G.; Polesel, J.; Candido, S.; Sambataro, D.; Bevelacqua, V.; Anzaldi, M.; Vella, N.; Fiore, V.; Militello, L.; Mazzarino, M.C.; et al. IL-6-174 G > C and MMP-9-1562 C > T polymorphisms are associated with increased risk of deep vein thrombosis in cancer patients. Cytokine 2013, 62, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Reitter, E.-M.; Ay, C.; Kaider, A.; Pirker, R.; Zielinski, C.; Zlabinger, G.; Pabinger, I. Interleukin levels and their potential association with venous thromboembolism and survival in cancer patients. Clin. Exp. Immunol. 2014, 177, 253–260. [Google Scholar] [CrossRef]
- Brat, D.J.; Van Meir, E.G. Vaso-occlusive and prothrombotic mechanisms associated with tumor hypoxia, necrosis, and accelerated growth in glioblastoma. Lab. Investig. 2004, 84, 397–405. [Google Scholar] [CrossRef]
- Ferrara, N.; Gerber, H.-P.; LeCouter, J. The biology of VEGF and its receptors. Nat. Med. 2003, 9, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Posch, F.; Thaler, J.; Zlabinger, G.-J.; Königsbrügge, O.; Koder, S.; Zielinski, C.; Pabinger, I.; Ay, C. Soluble Vascular Endothelial Growth Factor (sVEGF) and the Risk of Venous Thromboembolism in Patients with Cancer: Results from the Vienna Cancer and Thrombosis Study (CATS). Clin. Cancer Res. 2016, 22, 200–206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Du, T.; Tan, Z. Relationship between deep venous thrombosis and inflammatory cytokines in postoperative patients with malignant abdominal tumors. Braz. J. Med. Biol. Res. Rev. 2014, 47, 1003–1007. [Google Scholar] [CrossRef]
- Landskron, G.; De la Fuente, M.; Thuwajit, P.; Thuwajit, C.; Hermoso, M.A. Chronic inflammation and cytokines in the tumor microenvironment. J. Immunol. Res. 2014, 2014, 149185. [Google Scholar] [CrossRef] [Green Version]
- Ahlbrecht, J.; Dickmann, B.; Ay, C.; Dunkler, D.; Thaler, J.; Schmidinger, M.; Quehenberger, P.; Haitel, A.; Zielinski, C.; Pabinger, I. Tumor grade is associated with venous thromboembolism in patients with cancer: Results from the Vienna Cancer and Thrombosis Study. J. Clin. Oncol. 2012, 30, 3870–3875. [Google Scholar] [CrossRef]
- Riedl, J.; Kaider, A.; Reitter, E.-M.; Marosi, C.; Jäger, U.; Schwarzinger, I.; Zielinski, C.; Pabinger, I.; Ay, C. Association of mean platelet volume with risk of venous thromboembolism and mortality in patients with cancer. Results from the Vienna Cancer and Thrombosis Study (CATS). Thromb. Haemost. 2014, 111, 670–678. [Google Scholar] [PubMed]
- Ay, C.; Simanek, R.; Vormittag, R.; Dunkler, D.; Alguel, G.; Koder, S.; Kornek, G.; Marosi, C.; Wagner, O.; Zielinski, C.; et al. High plasma levels of soluble P-selectin are predictive of venous thromboembolism in cancer patients: Results from the Vienna Cancer and Thrombosis Study (CATS). Blood 2008, 112, 2703–2708. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ay, C.; Vormittag, R.; Dunkler, D.; Simanek, R.; Chiriac, A.-L.; Drach, J.; Quehenberger, P.; Wagner, O.; Zielinski, C.; Pabinger, I. D-dimer and prothrombin fragment 1 + 2 predict venous thromboembolism in patients with cancer: Results from the Vienna Cancer and Thrombosis Study. J. Clin. Oncol. 2009, 27, 4124–4129. [Google Scholar] [CrossRef] [PubMed]
- Ay, C.; Posch, F.; Kaider, A.; Zielinski, C.; Pabinger, I. Estimating risk of venous thromboembolism in patients with cancer in the presence of competing mortality. J. Thromb. Haemost. 2015, 13, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Marubini, E.; Valsecchi, M.G. Analysing Survival Data from Clinical Trials and Observational Studies; Wiley: Hoboken, NY, USA, 2004. [Google Scholar]
- Fine, J.P.; Gray, R.J. A Proportional Hazards Model for the Subdistribution of a Competing Risk. J. Am. Stat. Assoc. 1999, 94, 496–509. [Google Scholar] [CrossRef]
- Bender, R.; Lange, S. Adjusting for multiple testing—When and how? J. Clin. Epidemiol. 2001, 54, 343–349. [Google Scholar] [CrossRef]
| Median (Interquartile Range) or Count (%) | |
|---|---|
| Age | 54 (46–67) |
| Female sex | 35/76 (46.1%) |
| Newly-diagnosed glioma | 63/76 (82.9%) |
| IDH1 Status | |
| IDH1 mutation | 14/76 (18.4%) |
| IDH1 wildtype | 62/76 (81.6%) |
| Tumor Grade | |
| WHO grade IV | 57/76 (75%) |
| WHO grade III | 14/76 (18.4%) |
| WHO grade II | 5/76 (6.6%) |
| Histology | |
| Glioblastoma | 56/76 (73.7%) |
| Gliosarcoma | 1/76 (1.3%) |
| Anaplastic astrocytoma | 12/76 (15.8%) |
| Anaplastic oligodendroglioma | 2/76 (2.6%) |
| Diffuse astrocytoma | 4/76 (5.3%) |
| Diffuse oligodendroglioma | 1/76 (1.3%) |
| Serum Cytokine Levels | |
| IL-1β [pg/mL] | 1.9 (0.8–3.7) |
| IL-4 [pg/mL] | 11.5 (11.5–26.6) |
| IL-6 [pg/mL] | 3.8 (1.6–8.9) |
| IL-8 [pg/mL] | 16.7 (12.9–22.3) |
| IL-10 [pg/mL] | 25.6 (13.5–36.6) |
| IL-11 [pg/mL] | 0.0 (0.0–8.2) |
| CCL3 [pg/mL] | 24.3 (17.2–35.8) |
| TNF-α [pg/mL] | 11.7 (7.1–19.2) |
| VEGF [pg/mL] | 143.1 (81.7–243.7) |
| Serum Cytokine Levels | HR * | 95% CI | p-Value | |
|---|---|---|---|---|
| CCL3 [pg/mL] | 0.385 | 0.160 | 0.925 | 0.033 |
| IL-1β [pg/mL] | 1.046 | 0.732 | 1.495 | 0.804 |
| IL-4 [pg/mL] | 0.907 | 0.634 | 1.298 | 0.593 |
| IL-6 [pg/mL] | 0.894 | 0.602 | 1.328 | 0.597 |
| IL-8 [pg/mL] | 0.918 | 0.585 | 1.442 | 0.711 |
| IL-10 [pg/mL] | 0.822 | 0.505 | 1.340 | 0.433 |
| IL-11 [pg/mL] | 0.621 | 0.284 | 1.357 | 0.232 |
| TNF-α [pg/mL] | 1.097 | 0.697 | 1.727 | 0.689 |
| VEGF [pg/mL] | 0.995 | 0.640 | 1.548 | 0.983 |
| Model #1 | Adjusted HR | 95% CI | p-Value | |
| CCL3 (pg/mL) 1 | 0.329 | 0.128 | 0.843 | 0.021 |
| Sex | 1.807 | 0.475 | 6.867 | 0.475 |
| Age | 1.028 | 0.971 | 1.088 | 0.341 |
| Tumor grade 2 | 1.197 | 0.215 | 6.684 | 0.837 |
| Model #2 | Adjusted HR | 95% CI | p-Value | |
| CCL3 (pg/mL) 1 | 0.203 | 0.059 | 0.694 | 0.011 |
| D-dimer | 0.811 | 0.632 | 1.042 | 0.102 |
| sP-selectin | 1.068 | 1.017 | 1.122 | 0.009 |
| Platelets (G/L) | 0.986 | 0.974 | 0.997 | 0.013 |
| Model #3 | Adjusted HR | 95% CI | p-Value | |
| CCL3 (pg/mL) 1 | 0.348 | 0.146 | 0.830 | 0.017 |
| Podoplanin 3 | 2.021 | 1.060 | 3.855 | 0.033 |
| Model #4 | Adjusted HR | 95% CI | p-Value | |
| CCL3 (pg/mL) 1 | 0.412 | 0.174 | 0.975 | 0.044 |
| IDH1 mutation 4 | 0.450 | 0.056 | 3.636 | 0.454 |
| Serum Cytokine Levels n = 76 | WHO Grade II–III n = 19 | WHO Grade IV n = 57 | p-Value |
|---|---|---|---|
| CCL3 (pg/mL) | 20.7 (15.2–36.4) | 24.3 (17.8–35.1) | 0.697 |
| IL-1β (pg/mL) | 1.9 (1.1–4.8) | 1.9 (0.6–3.4) | 0.211 |
| IL-4 (pg/mL) | 11.5 (11.5–37.3) | 11.5 (9.5–26.6) | 0.536 |
| IL-6 (pg/mL) | 3.8 (1.4–8.4) | 3.8 (1.8–9.8) | 0.719 |
| IL-8 (pg/mL) | 13.6 (7.7–17.6) | 18.1 (18.1–25.2) | 0.012 |
| IL-10 (pg/mL) | 16.6 (10.7–27.3) | 28.4 (14.5–40.6) | 0.018 |
| IL-11 (pg/mL) | 0 (0–37.2) | 0 (0–5.9) | 0.249 |
| TNF-α (pg/mL) | 11.4 (7.8–17.1) | 11.7 (6.7–20.9) | 0.540 |
| VEGF (pg/mL) | 160.8 (81.7–376) | 137.0 (81.7–241.1) | 0.819 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mir Seyed Nazari, P.; Marosi, C.; Moik, F.; Riedl, J.; Özer, Ö.; Berghoff, A.S.; Preusser, M.; Hainfellner, J.A.; Pabinger, I.; Zlabinger, G.J.; et al. Low Systemic Levels of Chemokine C-C Motif Ligand 3 (CCL3) are Associated with a High Risk of Venous Thromboembolism in Patients with Glioma. Cancers 2019, 11, 2020. https://doi.org/10.3390/cancers11122020
Mir Seyed Nazari P, Marosi C, Moik F, Riedl J, Özer Ö, Berghoff AS, Preusser M, Hainfellner JA, Pabinger I, Zlabinger GJ, et al. Low Systemic Levels of Chemokine C-C Motif Ligand 3 (CCL3) are Associated with a High Risk of Venous Thromboembolism in Patients with Glioma. Cancers. 2019; 11(12):2020. https://doi.org/10.3390/cancers11122020
Chicago/Turabian StyleMir Seyed Nazari, Pegah, Christine Marosi, Florian Moik, Julia Riedl, Öykü Özer, Anna Sophie Berghoff, Matthias Preusser, Johannes A. Hainfellner, Ingrid Pabinger, Gerhard J. Zlabinger, and et al. 2019. "Low Systemic Levels of Chemokine C-C Motif Ligand 3 (CCL3) are Associated with a High Risk of Venous Thromboembolism in Patients with Glioma" Cancers 11, no. 12: 2020. https://doi.org/10.3390/cancers11122020
APA StyleMir Seyed Nazari, P., Marosi, C., Moik, F., Riedl, J., Özer, Ö., Berghoff, A. S., Preusser, M., Hainfellner, J. A., Pabinger, I., Zlabinger, G. J., & Ay, C. (2019). Low Systemic Levels of Chemokine C-C Motif Ligand 3 (CCL3) are Associated with a High Risk of Venous Thromboembolism in Patients with Glioma. Cancers, 11(12), 2020. https://doi.org/10.3390/cancers11122020






