Cachectic Body Composition and Inflammatory Markers Portend a Poor Prognosis in Patients with Locally Advanced Pancreatic Cancer Treated with Chemoradiation
Abstract
1. Introduction
2. Results
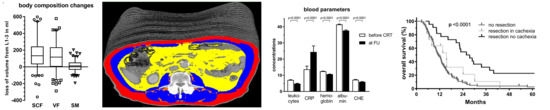
2.1. Weight Loss and Changes in Body Composition
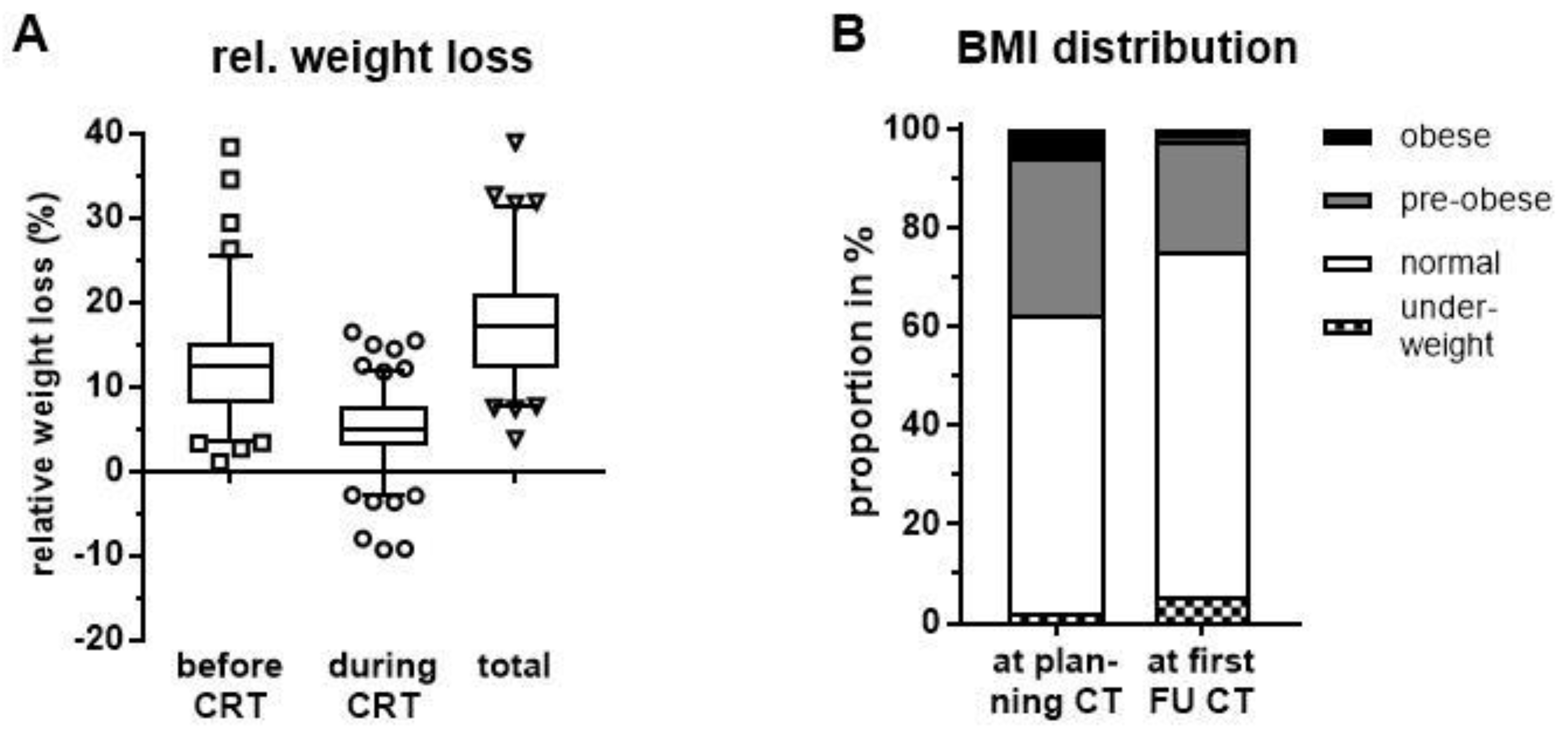
2.2. Cachexia Rates and Associated Blood Values before and after Neoadjuvant Chemoradiation
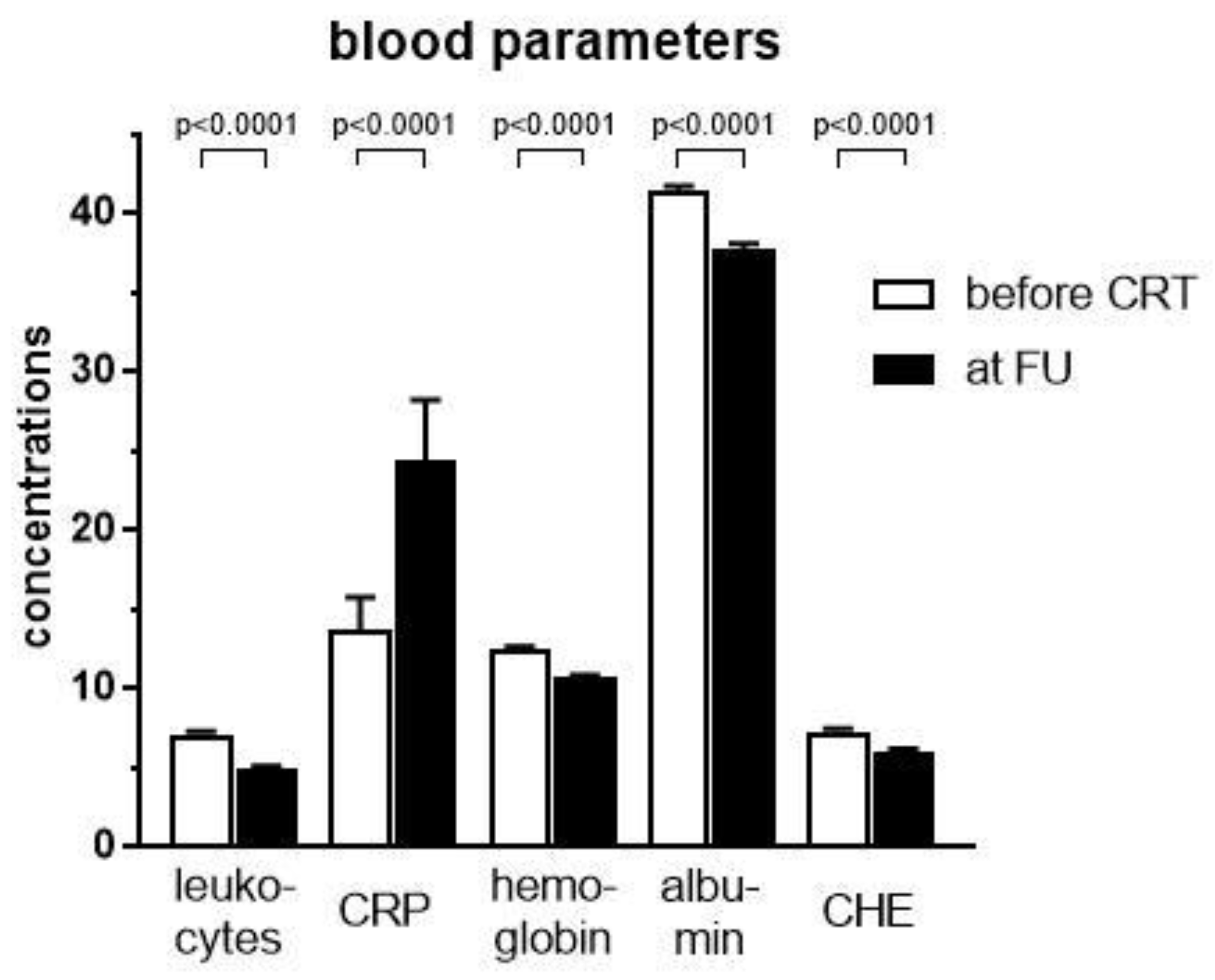
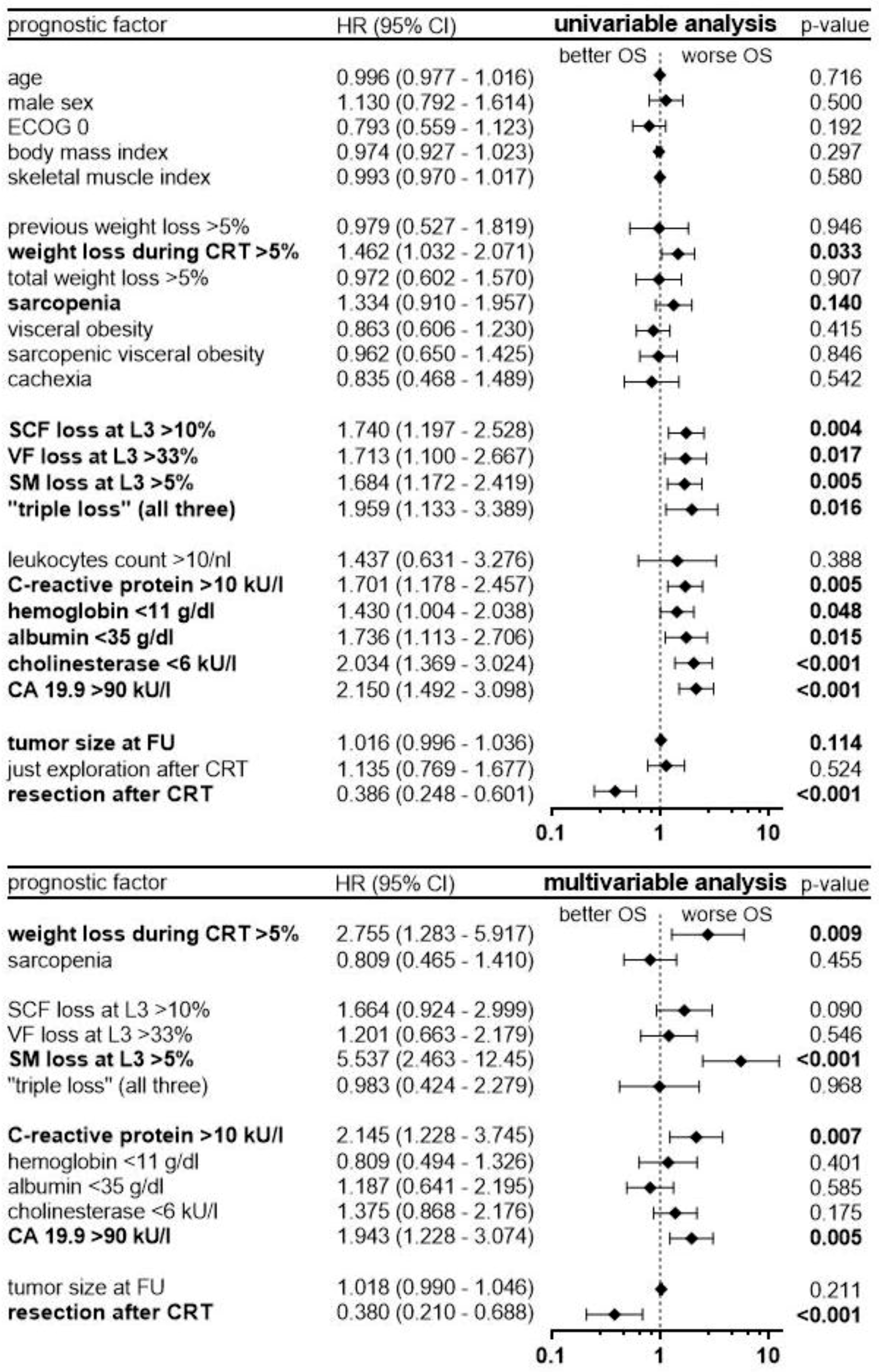
2.3. Survival Analysis
3. Discussion
4. Materials and Methods
4.1. Patient Selection and Treatment Approach
4.2. CT Analysis, Sarcopenia, and Cachexia
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Evans, W.J.; Morley, J.E.; Argiles, J.; Bales, C.; Baracos, V.; Guttridge, D.; Jatoi, A.; Kalantar-Zadeh, K.; Lochs, H.; Mantovani, G.; et al. Cachexia: A new definition. Clin. Nutr. 2008, 27, 793–799. [Google Scholar] [CrossRef] [PubMed]
- Fearon, K.; Arends, J.; Baracos, V. Understanding the mechanisms and treatment options in cancer cachexia. Nat. Rev. Clin. Oncol. 2013, 10, 90–99. [Google Scholar] [CrossRef] [PubMed]
- Danai, L.V.; Babic, A.; Rosenthal, M.H.; Dennstedt, E.A.; Muir, A.; Lien, E.C.; Mayers, J.R.; Tai, K.; Lau, A.N.; Jones-Sali, P.; et al. Altered exocrine function can drive adipose wasting in early pancreatic cancer. Nature 2018, 558, 600–604. [Google Scholar] [CrossRef] [PubMed]
- Cooper, A.B.; Slack, R.; Fogelman, D.; Holmes, H.M.; Petzel, M.; Parker, N.; Balachandran, A.; Garg, N.; Ngo-Huang, A.; Varadhachary, G.; et al. Characterization of anthropometric changes that occur during neoadjuvant therapy for potentially resectable pancreatic cancer. Ann. Surg. Oncol. 2015, 22, 2416–2423. [Google Scholar] [CrossRef]
- Carrara, G.; Pecorelli, N.; De Cobelli, F.; Cristel, G.; Damascelli, A.; Beretta, L.; Braga, M. Preoperative sarcopenia determinants in pancreatic cancer patients. Clin. Nutr. 2017, 36, 1649–1653. [Google Scholar] [CrossRef]
- Sandini, M.; Patino, M.; Ferrone, C.R.; Alvarez-Perez, C.A.; Honselmann, K.C.; Paiella, S.; Catania, M.; Riva, L.; Tedesco, G.; Casolino, R.; et al. Association between changes in body composition and neoadjuvant treatment for pancreatic cancer. JAMA Surg. 2018, 153, 809–815. [Google Scholar] [CrossRef]
- Bachmann, J.; Buchler, M.W.; Friess, H.; Martignoni, M.E. Cachexia in patients with chronic pancreatitis and pancreatic cancer: Impact on survival and outcome. Nutr. Cancer 2013, 65, 827–833. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef]
- Ghaneh, P.; Kleeff, J.; Halloran, C.M.; Raraty, M.; Jackson, R.; Melling, J.; Jones, O.; Palmer, D.H.; Cox, T.F.; Smith, C.J.; et al. The impact of positive resection margins on survival and recurrence following resection and adjuvant chemotherapy for pancreatic ductal adenocarcinoma. Ann. Surg. 2019, 269, 520–529. [Google Scholar] [CrossRef]
- Strobel, O.; Hank, T.; Hinz, U.; Bergmann, F.; Schneider, L.; Springfeld, C.; Jager, D.; Schirmacher, P.; Hackert, T.; Buchler, M.W. Pancreatic cancer surgery: The new r-status counts. Ann. Surg. 2017, 265, 565–573. [Google Scholar] [CrossRef]
- Dobiasch, S.; Goerig, N.L.; Fietkau, R.; Combs, S.E. Essential role of radiation therapy for the treatment of pancreatic cancer: Novel study concepts and established treatment recommendations. Strahlenther. Onkol. 2018, 194, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Habermehl, D.; Kessel, K.; Welzel, T.; Hof, H.; Abdollahi, A.; Bergmann, F.; Rieken, S.; Weitz, J.; Werner, J.; Schirmacher, P.; et al. Neoadjuvant chemoradiation with gemcitabine for locally advanced pancreatic cancer. Radiat. Oncol. 2012, 7, 28. [Google Scholar] [CrossRef] [PubMed]
- Hackert, T.; Sachsenmaier, M.; Hinz, U.; Schneider, L.; Michalski, C.W.; Springfeld, C.; Strobel, O.; Jager, D.; Ulrich, A.; Buchler, M.W. Locally advanced pancreatic cancer: Neoadjuvant therapy with folfirinox results in resectability in 60% of the patients. Ann. Surg. 2016, 264, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Zaky, A.M.; Wolfgang, C.L.; Weiss, M.J.; Javed, A.A.; Fishman, E.K.; Zaheer, A. Tumor-vessel relationships in pancreatic ductal adenocarcinoma at multidetector ct: Different classification systems and their influence on treatment planning. Radiographics 2017, 37, 93–112. [Google Scholar] [CrossRef] [PubMed]
- Combs, S.E.; Habermehl, D.; Kessel, K.A.; Bergmann, F.; Werner, J.; Naumann, P.; Jager, D.; Buchler, M.W.; Debus, J. Prognostic impact of CA 19-9 on outcome after neoadjuvant chemoradiation in patients with locally advanced pancreatic cancer. Ann. Surg. Oncol. 2014, 21, 2801–2807. [Google Scholar] [CrossRef]
- Park, J.K.; Paik, W.H.; Ryu, J.K.; Kim, Y.T.; Kim, Y.J.; Kim, J.; Song, B.J.; Park, J.M.; Yoon, Y.B. Clinical significance and revisiting the meaning of CA 19-9 blood level before and after the treatment of pancreatic ductal adenocarcinoma: Analysis of 1446 patients from the pancreatic cancer cohort in a single institution. PLoS ONE 2013, 8, e78977. [Google Scholar] [CrossRef][Green Version]
- Porporato, P.E. Understanding cachexia as a cancer metabolism syndrome. Oncogenesis 2016, 5, e200. [Google Scholar] [CrossRef]
- Blum, D.; Stene, G.B.; Solheim, T.S.; Fayers, P.; Hjermstad, M.J.; Baracos, V.E.; Fearon, K.; Strasser, F.; Kaasa, S.; Euro, I. Validation of the consensus-definition for cancer cachexia and evaluation of a classification model—A study based on data from an international multicentre project (epcrc-csa). Ann. Oncol. 2014, 25, 1635–1642. [Google Scholar] [CrossRef]
- Schwarz, S.; Prokopchuk, O.; Esefeld, K.; Groschel, S.; Bachmann, J.; Lorenzen, S.; Friess, H.; Halle, M.; Martignoni, M.E. The clinical picture of cachexia: A mosaic of different parameters (experience of 503 patients). BMC Cancer 2017, 17, 130. [Google Scholar] [CrossRef]
- Zalite, I.O.; Zykus, R.; González, M.F.; Saygili, F.; Pukitis, A.; Gaujoux, S.; Charnley, R.; Lyadov, V.; Saygılı, F. Influence of cachexia and sarcopenia on survival in pancreatic ductal adenocarcinoma: A systematic review. Pancreatology 2015, 15, 19–24. [Google Scholar] [CrossRef]
- Cloyd, J.M.; Nogueras-Gonzalez, G.M.; Prakash, L.R.; Petzel, M.Q.B.; Parker, N.H.; Ngo-Huang, A.T.; Fogelman, D.; Denbo, J.W.; Garg, N.; Kim, M.P.; et al. Anthropometric changes in patients with pancreatic cancer undergoing preoperative therapy and pancreatoduodenectomy. J. Gastrointest. Surg. 2018, 22, 703–712. [Google Scholar] [CrossRef] [PubMed]
- Delitto, D.; Judge, S.M.; George, T.J., Jr.; Sarosi, G.A.; Thomas, R.M.; Behrns, K.E.; Hughes, S.J.; Judge, A.R.; Trevino, J.G. A clinically applicable muscular index predicts long-term survival in resectable pancreatic cancer. Surgery 2017, 161, 930–938. [Google Scholar] [CrossRef] [PubMed]
- Ninomiya, G.; Fujii, T.; Yamada, S.; Yabusaki, N.; Suzuki, K.; Iwata, N.; Kanda, M.; Hayashi, M.; Tanaka, C.; Nakayama, G.; et al. Clinical impact of sarcopenia on prognosis in pancreatic ductal adenocarcinoma: A retrospective cohort study. Int. J. Surg. 2017, 39, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Okumura, S.; Kaido, T.; Hamaguchi, Y.; Kobayashi, A.; Shirai, H.; Yao, S.; Yagi, S.; Kamo, N.; Hatano, E.; Okajima, H.; et al. Visceral adiposity and sarcopenic visceral obesity are associated with poor prognosis after resection of pancreatic cancer. Ann. Surg. Oncol. 2017, 24, 3732–3740. [Google Scholar] [CrossRef] [PubMed]
- Naumann, P.; Eberlein, J.; Farnia, B.; Hackert, T.; Debus, J.; Combs, S.E. Continued weight loss and sarcopenia predict poor outcomes in locally advanced pancreatic cancer treated with chemoradiation. Cancers 2019, 11, 709. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.; Senesse, P.; Gioulbasanis, I.; Antoun, S.; Bozzetti, F.; Deans, C.; Strasser, F.; Thoresen, L.; Jagoe, R.T.; Chasen, M.; et al. Diagnostic criteria for the classification of cancer-associated weight loss. J. Clin. Oncol. 2015, 33, 90–99. [Google Scholar] [CrossRef]
- Fearon, K.; Strasser, F.; Anker, S.D.; Bosaeus, I.; Bruera, E.; Fainsinger, R.L.; Jatoi, A.; Loprinzi, C.; MacDonald, N.; Mantovani, G.; et al. Definition and classification of cancer cachexia: An international consensus. Lancet Oncol. 2011, 12, 489–495. [Google Scholar] [CrossRef]
- Nemer, L.; Krishna, S.G.; Shah, Z.K.; Conwell, D.L.; Cruz-Monserrate, Z.; Dillhoff, M.; Guttridge, D.C.; Hinton, A.; Manilchuk, A.; Pawlik, T.M.; et al. Predictors of pancreatic cancer-associated weight loss and nutritional interventions. Pancreas 2017, 46, 1152–1157. [Google Scholar] [CrossRef]
- Choi, Y.; Oh, D.Y.; Kim, T.Y.; Lee, K.H.; Han, S.W.; Im, S.A.; Kim, T.Y.; Bang, Y.J. Skeletal muscle depletion predicts the prognosis of patients with advanced pancreatic cancer undergoing palliative chemotherapy, independent of body mass index. PLoS ONE 2015, 10, e0139749. [Google Scholar] [CrossRef]
- Griffin, O.M.; Duggan, S.N.; Ryan, R.; McDermott, R.; Geoghegan, J.; Conlon, K.C. Characterising the impact of body composition change during neoadjuvant chemotherapy for pancreatic cancer. Pancreatology 2019, 19, 850–857. [Google Scholar] [CrossRef]
- Hendifar, A.E.; Petzel, M.Q.B.; Zimmers, T.A.; Denlinger, C.S.; Matrisian, L.M.; Picozzi, V.J.; Rahib, L.; Precision Promise, C. Pancreas cancer-associated weight loss. Oncologist 2019, 24, 691–701. [Google Scholar] [CrossRef] [PubMed]
- Dehestani, B.; le Roux, C.W. The role of the small bowel in unintentional weight loss after treatment of upper gastrointestinal cancers. J. Clin. Med. 2019, 8, 942. [Google Scholar] [CrossRef] [PubMed]
- Naumann, P.; Habermehl, D.; Welzel, T.; Debus, J.; Combs, S.E. Outcome after neoadjuvant chemoradiation and correlation with nutritional status in patients with locally advanced pancreatic cancer. Strahlenther. Onkol. 2013, 189, 745–752. [Google Scholar] [CrossRef] [PubMed]
- Prado, C.M.; Sawyer, M.B.; Ghosh, S.; Lieffers, J.R.; Esfandiari, N.; Antoun, S.; Baracos, V.E. Central tenet of cancer cachexia therapy: Do patients with advanced cancer have exploitable anabolic potential? Am. J. Clin. Nutr. 2013, 98, 1012–1019. [Google Scholar] [CrossRef] [PubMed]
- Prado, C.M.; Lieffers, J.R.; McCargar, L.J.; Reiman, T.; Sawyer, M.B.; Martin, L.; Baracos, V.E. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: A population-based study. Lancet Oncol. 2008, 9, 629–635. [Google Scholar] [CrossRef]
- Mintziras, I.; Miligkos, M.; Wachter, S.; Manoharan, J.; Maurer, E.; Bartsch, D.K. Sarcopenia and sarcopenic obesity are significantly associated with poorer overall survival in patients with pancreatic cancer: Systematic review and meta-analysis. Int. J. Surg. 2018, 59, 19–26. [Google Scholar] [CrossRef]
- Sandini, M.; Bernasconi, D.P.; Fior, D.; Molinelli, M.; Ippolito, D.; Nespoli, L.; Caccialanza, R.; Gianotti, L. A high visceral adipose tissue-to-skeletal muscle ratio as a determinant of major complications after pancreatoduodenectomy for cancer. Nutrition 2016, 32, 1231–1237. [Google Scholar] [CrossRef]
- Rollins, K.E.; Tewari, N.; Ackner, A.; Awwad, A.; Madhusudan, S.; Macdonald, I.A.; Fearon, K.C.; Lobo, D.N. The impact of sarcopenia and myosteatosis on outcomes of unresectable pancreatic cancer or distal cholangiocarcinoma. Clin. Nutr. 2016, 35, 1103–1109. [Google Scholar] [CrossRef]
- Stretch, C.; Aubin, J.M.; Mickiewicz, B.; Leugner, D.; Al-Manasra, T.; Tobola, E.; Salazar, S.; Sutherland, F.R.; Ball, C.G.; Dixon, E.; et al. Sarcopenia and myosteatosis are accompanied by distinct biological profiles in patients with pancreatic and periampullary adenocarcinomas. PLoS ONE 2018, 13, e0196235. [Google Scholar] [CrossRef]
- Wiskemann, J.; Clauss, D.; Tjaden, C.; Hackert, T.; Schneider, L.; Ulrich, C.M.; Steindorf, K. Progressive resistance training to impact physical fitness and body weight in pancreatic cancer patients: A randomized controlled trial. Pancreas 2019, 48, 257–266. [Google Scholar] [CrossRef]
- Patel, H.J.; Patel, B.M. Tnf-alpha and cancer cachexia: Molecular insights and clinical implications. Life Sci. 2017, 170, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Hou, Y.C.; Wang, C.J.; Chao, Y.J.; Chen, H.Y.; Wang, H.C.; Tung, H.L.; Lin, J.T.; Shan, Y.S. Elevated serum interleukin-8 level correlates with cancer-related cachexia and sarcopenia: An indicator for pancreatic cancer outcomes. J. Clin. Med. 2018, 7, 502. [Google Scholar] [CrossRef] [PubMed]
- Malietzis, G.; Johns, N.; Al-Hassi, H.O.; Knight, S.C.; Kennedy, R.H.; Fearon, K.C.; Aziz, O.; Jenkins, J.T. Low muscularity and myosteatosis is related to the host systemic inflammatory response in patients undergoing surgery for colorectal cancer. Ann. Surg. 2016, 263, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Mitsunaga, S.; Kinoshita, T.; Hasebe, T.; Nakagohri, T.; Konishi, M.; Takahashi, S.; Gotohda, N.; Ochiai, A. Low serum level of cholinesterase at recurrence of pancreatic cancer is a poor prognostic factor and relates to systemic disorder and nerve plexus invasion. Pancreas 2008, 36, 241–248. [Google Scholar] [CrossRef]
- Babic, A.; Rosenthal, M.H.; Bamlet, W.R.; Takahashi, N.; Sugimoto, M.; Danai, L.V.; Morales-Oyarvide, V.; Khalaf, N.; Dunne, R.F.; Brais, L.K.; et al. Post diagnosis loss of skeletal muscle, but not adipose tissue, is associated with shorter survival of patients with advanced pancreatic cancer. Cancer Epidemiol. Biomarkers Prev. 2019. [Google Scholar] [CrossRef]
- Balentine, C.J.; Enriquez, J.; Fisher, W.; Hodges, S.; Bansal, V.; Sansgiry, S.; Petersen, N.J.; Berger, D.H. Intra-abdominal fat predicts survival in pancreatic cancer. J. Gastrointest. Surg. 2010, 14, 1832–1837. [Google Scholar] [CrossRef]
- Gaujoux, S.; Torres, J.; Olson, S.; Winston, C.; Gonen, M.; Brennan, M.F.; Klimstra, D.S.; D’Angelica, M.; Dematteo, R.; Fong, Y.; et al. Impact of obesity and body fat distribution on survival after pancreaticoduodenectomy for pancreatic adenocarcinoma. Ann. Surg. Oncol. 2012, 19, 2908–2916. [Google Scholar] [CrossRef]
- Schweitzer, L.; Geisler, C.; Pourhassan, M.; Braun, W.; Gluer, C.C.; Bosy-Westphal, A.; Muller, M.J. What is the best reference site for a single mri slice to assess whole-body skeletal muscle and adipose tissue volumes in healthy adults? Am. J. Clin. Nutr. 2015, 102, 58–65. [Google Scholar] [CrossRef]
- Tewari, N.; Awad, S.; Macdonald, I.A.; Lobo, D.N. A comparison of three methods to assess body composition. Nutrition 2018, 47, 1–5. [Google Scholar] [CrossRef]
- Shuster, A.; Patlas, M.; Pinthus, J.H.; Mourtzakis, M. The clinical importance of visceral adiposity: A critical review of methods for visceral adipose tissue analysis. Br. J. Radiol. 2012, 85, 1–10. [Google Scholar] [CrossRef]
- Yoshizumi, T.; Nakamura, T.; Yamane, M.; Islam, A.H.; Menju, M.; Yamasaki, K.; Arai, T.; Kotani, K.; Funahashi, T.; Yamashita, S.; et al. Abdominal fat: Standardized technique for measurement at ct. Radiology 1999, 211, 283–286. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Mean |
|---|---|
| Age, in years (SD) | 63.6 (± 9.2) |
| Gender, n (%) | |
| Male | 77 (54.6%) |
| Female | 64 (45.4%) |
| Tumor Site, n (%) | |
| Head | 73 (51.8%) |
| Body | 22 (15.6%) |
| Tail | 2 (1.4%) |
| Multiple | 44 (31.2%) |
| Tumor Stage, n (%) | |
| I | 0 (0%) |
| II | 0 (0%) |
| III | 141 (100%) |
| IV | 0 (0%) |
| ECOG score, n (%) | |
| 0 | 72 (51.1%) |
| 1 | 58 (41.1%) |
| 2 | 11 (7.8%) |
| 3 | 0 (0%) |
| Prior chemotherapy | |
| None | 126 (85.8%) |
| Gemcitabine | 8 (5.0%) |
| Gemcitabine + Erlotinib | 5 (3.6%) |
| Gemcitabine + Cisplatin | 1 (0.7%) |
| Capecitabine | 1 (0.7%) |
| FOLFIRINOX | 3 (2.1%) |
| Unknown | 3 (2.1%) |
| Height, in cm | 170 (± 9.1) |
| Weight, in kg (SD; range) | 70.1 (± 12.3; 44–115)) |
| CA 19.9, in kU/L (SD; range; median) | 1,286.5 (± 3,272; 0.1–27,031; 230.3) |
| Timeline, in days (SD) | |
| Planning CT to treatment initiation | 9.0 (± 6) |
| Treatment duration | 38.3 (± 4) |
| Treatment completion to follow-up CT | 29.4 (± 9) |
| Planning CT to follow-up CT | 78.3 (± 11) |
| Parameter | No Surgery (n = 69) | Surgical Exploration (n = 39) | Surgical Resection (n = 33) |
|---|---|---|---|
| Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | |
| SCF area in cm2 | |||
| —before CRT | 139.3 (119.9–158.7) | 147.3 (123.0–171.5) | 141.7 (111.1–172.4) |
| —at first FU | 107.0 (92.4–121.7) | 122.4 (103.7–141.1) | 123.9 (94.5–153.3) |
| —deficit | 32.3 (22.9–41.6) | 24.8 (13.0–36.6) | 17.8 (6.7–29.0) |
| VF area in cm2 | |||
| —before CRT | 113.6 (95.8–131.5) | 131.9 (110.9–152.9) | 96.7 (75.6–117.8) |
| —at first FU | 93.0 (79.6–106.4) | 109.3 (94.2–124.4) | 82.4 (62.5–102.4) |
| —deficit | 20.6 (12.9–28.4) | 22.6 (11.9–33.3) | 14.2 (5.1–23.4) |
| SM area in cm2 | |||
| —before CRT | 124.4 (118.5–130.2) | 131.7 (120.6–142.8) | 122.8 (112.8–132.9) |
| —at first FU | 119.6 (114.1–125.0) | 127.4 (116.7–138.2) | 118.6 (109.8–127.4) |
| —deficit | 4.8 (2.0–7.6) | 4.3 (1.4–7.2) | 4.2 (0.4–8.1) |
| Tumor size in cm | |||
| —before CRT | 5.0 × 3.7 (4.8−5.3 × 3.5−4.0) | 4.7 × 3.4 (4.3−5.2 × 3.0−3.7) | 4.6 × 3.5 (4.1−5.2 × 3.1−4.0) |
| —at first FU | 4.8 × 3.5 (4.5−5.1 × 3.2−3.7) | 4.4 × 3.2 (4.0−4.8 × 2.9−3.5) | 4.2 × 3.2 (3.7−4.6 × 2.9−3.6) |
| Parameter | Before CRT at Planning CT n (%) | After CRT at CT for First FU n (%) | p-Value † |
|---|---|---|---|
| Cachectic weight (loss >5%) | 83 (58.9%) | 120 (85.1%) | <0.0001 |
| Sarcopenia (SMI below cut-offs) | 89 (63.1%) | 96 (68.1%) | 0.1892 |
| Visceral obesity (VF at L3 >100 cm2) | 79 (56.0%) | 57 (40.4%) | <0.0001 |
| Sarcopenic visceral obesity | 48 (34.0%) | 38 (27.0%) | 0.0639 |
| Sarcopenic obesity | 2 (1.4%) | 1 (0.7%) | <0.0001 |
| Cachexia by definition | 89 (63.1%) | 128 (90.8%) | <0.0001 |
| Parameter | Before CRT at Planning CT Mean (95% CI) | After CRT at CT for First FU Mean (95% CI) | Correlation Coefficient to Weight Loss | Correlation Coefficient to Muscle Loss | Correlation Coefficient to Resectability |
|---|---|---|---|---|---|
| Leukocyte, n/nL | 7.1 (6.7–7.5) | 4.9 (4.4–5.3) | 0.120 † (p = 0.16) | 0.216 † (p = 0.01) | 0.032 † (p = 0.71) |
| C-reactive protein, mg/L | 13.7 (9.7–17.7) | 24.4 (17.0–31.9) | 0.260 † (p = 0.002) | 0.096 † (p = 0.26) | −0.139 † (p = 0.10) |
| Hemoglobin, g/dL | 12.5 (12.2–12.7) | 10.7 (10.5–10.9) | −0.025 * (p = 0.77) | 0.089 * (p = 0.29) | 0.209 * (p = 0.01) |
| Albumin, g/L | 41.4 (40.9–42.0) | 37.7 (36.9–38.5) | −0.206 † (p = 0.02) | 0.085 † (p = 0.35) | 0.023 † (p = 0.81) |
| Cholinesterase, kU/L | 7.3 (7.0–7.6) | 6.0 (5.6–6.3) | −0.187 † (p = 0.04) | −0.220 † (p = 0.02) | 0.188 † (p = 0.03) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naumann, P.; Eberlein, J.; Farnia, B.; Liermann, J.; Hackert, T.; Debus, J.; Combs, S.E. Cachectic Body Composition and Inflammatory Markers Portend a Poor Prognosis in Patients with Locally Advanced Pancreatic Cancer Treated with Chemoradiation. Cancers 2019, 11, 1655. https://doi.org/10.3390/cancers11111655
Naumann P, Eberlein J, Farnia B, Liermann J, Hackert T, Debus J, Combs SE. Cachectic Body Composition and Inflammatory Markers Portend a Poor Prognosis in Patients with Locally Advanced Pancreatic Cancer Treated with Chemoradiation. Cancers. 2019; 11(11):1655. https://doi.org/10.3390/cancers11111655
Chicago/Turabian StyleNaumann, Patrick, Jonathan Eberlein, Benjamin Farnia, Jakob Liermann, Thilo Hackert, Jürgen Debus, and Stephanie E. Combs. 2019. "Cachectic Body Composition and Inflammatory Markers Portend a Poor Prognosis in Patients with Locally Advanced Pancreatic Cancer Treated with Chemoradiation" Cancers 11, no. 11: 1655. https://doi.org/10.3390/cancers11111655
APA StyleNaumann, P., Eberlein, J., Farnia, B., Liermann, J., Hackert, T., Debus, J., & Combs, S. E. (2019). Cachectic Body Composition and Inflammatory Markers Portend a Poor Prognosis in Patients with Locally Advanced Pancreatic Cancer Treated with Chemoradiation. Cancers, 11(11), 1655. https://doi.org/10.3390/cancers11111655