Molecular Detection of Minimal Residual Disease before Allogeneic Stem Cell Transplantation Predicts a High Incidence of Early Relapse in Adult Patients with NPM1 Positive Acute Myeloid Leukemia
Abstract
1. Introduction
2. Results
2.1. Patients’ Characteristics
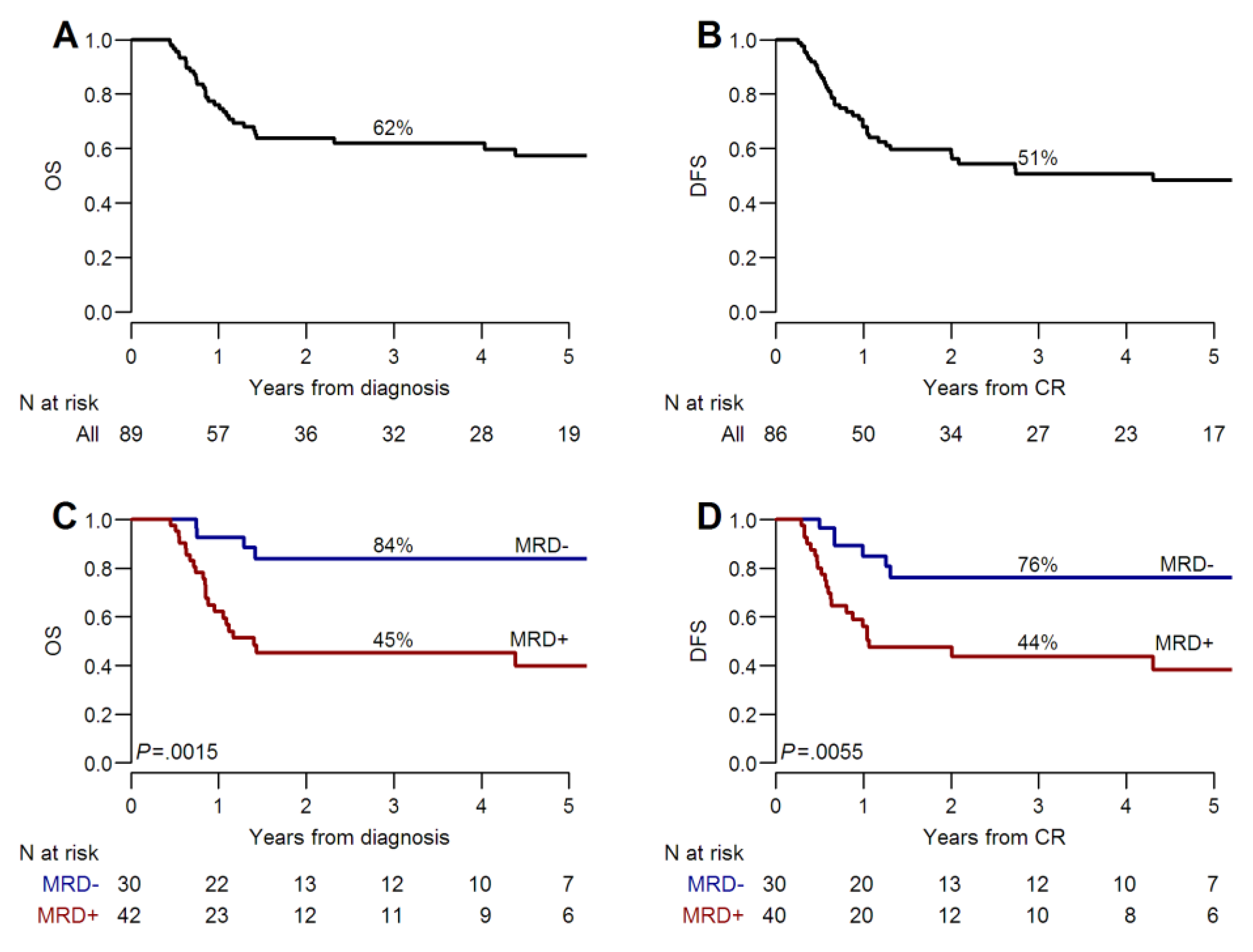
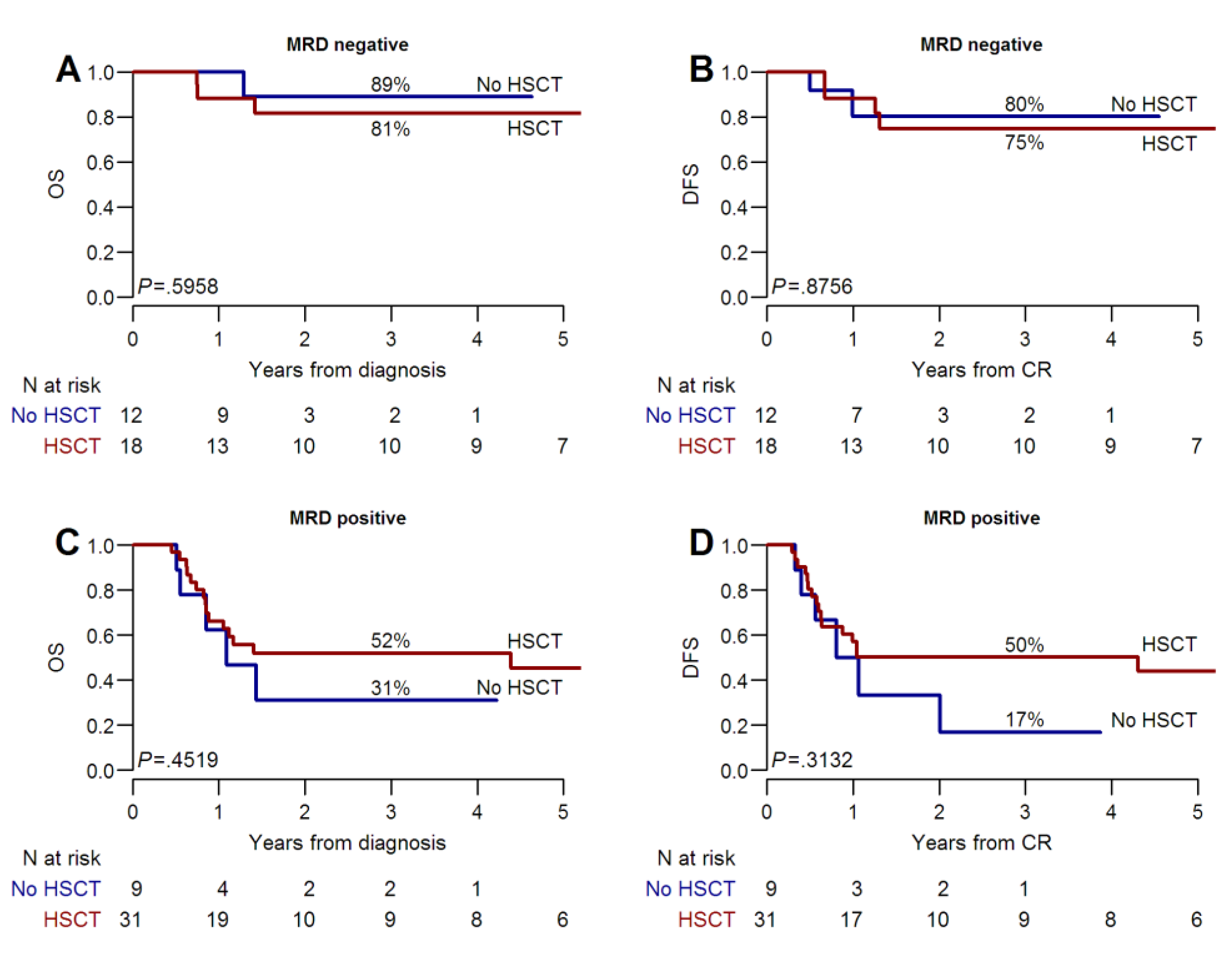
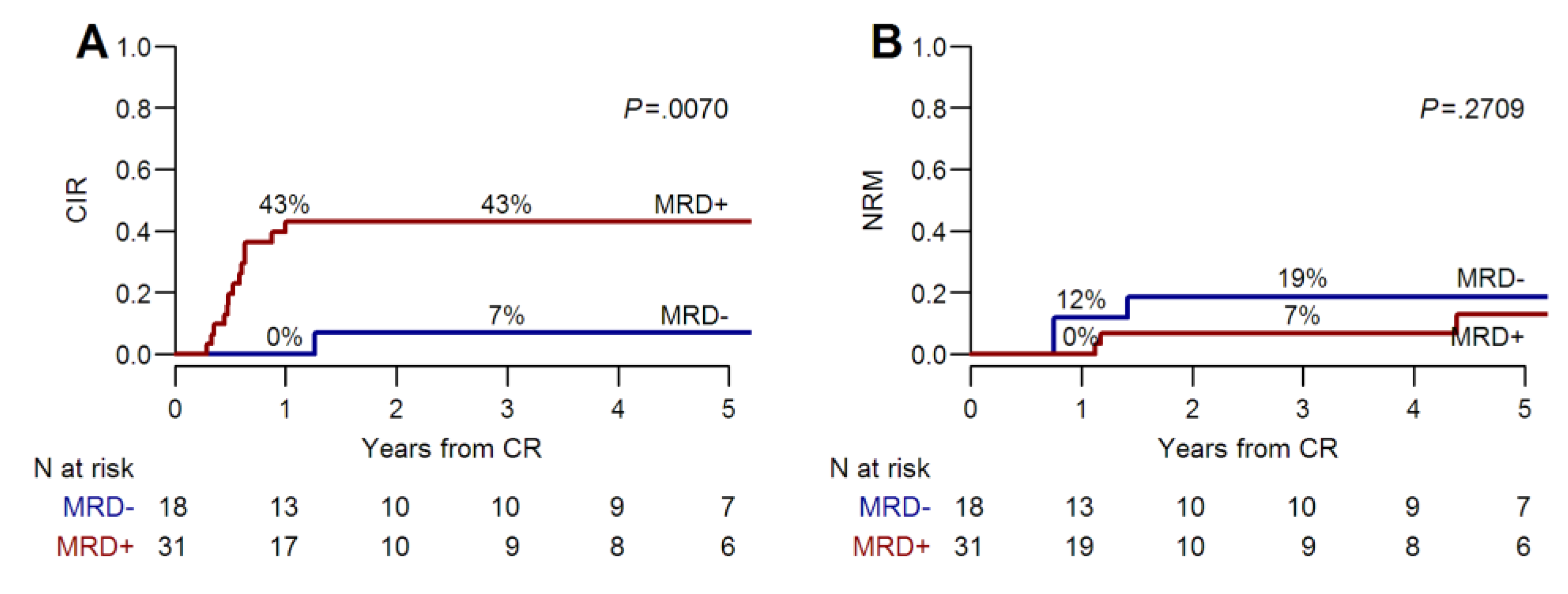
2.2. Long-Term Outcomes
3. Discussion
4. Materials and methods
4.1. Patients, Diagnosis, and Minimal Residual Disease Evaluations
4.2. Study Endpoints and Statistical Methods
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Papaemmanuil, E.; Gerstung, M.; Bullinger, L.; Gaidzik, V.I.; Paschka, P.; Roberts, N.D.; Potter, N.E.; Heuser, M.; Thol, F.; Bolli, N.; et al. Genomic Classification and Prognosis in Acute Myeloid Leukemia. N. Engl. J. Med. 2016, 374, 2209–2221. [Google Scholar] [CrossRef] [PubMed]
- Dohner, H.; Estey, E.; Grimwade, D.; Amadori, S.; Appelbaum, F.R.; Buchner, T.; Dombret, H.; Ebert, B.L.; Fenaux, P.; Larson, R.A.; et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 2017, 129, 424–447. [Google Scholar] [CrossRef] [PubMed]
- Hubmann, M.; Kohnke, T.; Hoster, E.; Schneider, S.; Dufour, A.; Zellmeier, E.; Fiegl, M.; Braess, J.; Bohlander, S.K.; Subklewe, M.; et al. Molecular response assessment by quantitative real-time polymerase chain reaction after induction therapy in NPM1-mutated patients identifies those at high risk of relapse. Haematologica 2014, 99, 1317–1325. [Google Scholar] [CrossRef] [PubMed]
- Ivey, A.; Hills, R.K.; Simpson, M.A.; Jovanovic, J.V.; Gilkes, A.; Grech, A.; Patel, Y.; Bhudia, N.; Farah, H.; Mason, J.; et al. Assessment of Minimal Residual Disease in Standard-Risk AML. N. Engl. J. Med. 2016, 374, 422–433. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, T.; Moller, M.B.; Friis, L.; Bergmann, O.J.; Preiss, B. NPM1 mutation is a stable marker for minimal residual disease monitoring in acute myeloid leukaemia patients with increased sensitivity compared to WT1 expression. Eur. J. Haematol. 2011, 87, 400–408. [Google Scholar] [CrossRef] [PubMed]
- Kronke, J.; Schlenk, R.F.; Jensen, K.O.; Tschurtz, F.; Corbacioglu, A.; Gaidzik, V.I.; Paschka, P.; Onken, S.; Eiwen, K.; Habdank, M.; et al. Monitoring of minimal residual disease in NPM1-mutated acute myeloid leukemia: A study from the German-Austrian acute myeloid leukemia study group. J. Clin. Oncol. 2011, 29, 2709–2716. [Google Scholar] [CrossRef]
- Schnittger, S.; Kern, W.; Tschulik, C.; Weiss, T.; Dicker, F.; Falini, B.; Haferlach, C.; Haferlach, T. Minimal residual disease levels assessed by NPM1 mutation-specific RQ-PCR provide important prognostic information in AML. Blood 2009, 114, 2220–2231. [Google Scholar] [CrossRef]
- Schuurhuis, G.J.; Heuser, M.; Freeman, S.; Bene, M.C.; Buccisano, F.; Cloos, J.; Grimwade, D.; Haferlach, T.; Hills, R.K.; Hourigan, C.S.; et al. Minimal/measurable residual disease in AML: A consensus document from the European LeukemiaNet MRD Working Party. Blood 2018, 131, 1275–1291. [Google Scholar] [CrossRef]
- Shayegi, N.; Kramer, M.; Bornhauser, M.; Schaich, M.; Schetelig, J.; Platzbecker, U.; Rollig, C.; Heiderich, C.; Landt, O.; Ehninger, G.; et al. The level of residual disease based on mutant NPM1 is an independent prognostic factor for relapse and survival in AML. Blood 2013, 122, 83–92. [Google Scholar] [CrossRef]
- Kayser, S.; Benner, A.; Thiede, C.; Martens, U.; Huber, J.; Stadtherr, P.; Janssen, J.W.; Rollig, C.; Uppenkamp, M.J.; Bochtler, T.; et al. Pretransplant NPM1 MRD levels predict outcome after allogeneic hematopoietic stem cell transplantation in patients with acute myeloid leukemia. Blood Cancer J. 2016, 6, e449. [Google Scholar] [CrossRef]
- Araki, D.; Wood, B.L.; Othus, M.; Radich, J.P.; Halpern, A.B.; Zhou, Y.; Mielcarek, M.; Estey, E.H.; Appelbaum, F.R.; Walter, R.B. Allogeneic Hematopoietic Cell Transplantation for Acute Myeloid Leukemia: Time to Move Toward a Minimal Residual Disease-Based Definition of Complete Remission? J. Clin. Oncol. 2016, 34, 329–336. [Google Scholar] [CrossRef]
- Bassan, R.; Intermesoli, T.; Masciulli, A.; Pavoni, C.; Boschini, C.; Gianfaldoni, G.; Marmont, F.; Cavattoni, I.; Mattei, D.; Terruzzi, E.; et al. Randomized trial comparing standard vs. sequential high-dose chemotherapy for inducing early CR in adult AML. Blood Adv. 2019, 3, 1103–1117. [Google Scholar] [CrossRef] [PubMed]
- Rollig, C.; Bornhauser, M.; Kramer, M.; Thiede, C.; Ho, A.D.; Kramer, A.; Schafer-Eckart, K.; Wandt, H.; Hanel, M.; Einsele, H.; et al. Allogeneic stem-cell transplantation in patients with NPM1-mutated acute myeloid leukemia: Results from a prospective donor versus no-donor analysis of patients after upfront HLA typing within the SAL-AML 2003 trial. J. Clin. Oncol. 2015, 33, 403–410. [Google Scholar] [CrossRef] [PubMed]
- De Lima, M.; Giralt, S.; Thall, P.F.; de Padua Silva, L.; Jones, R.B.; Komanduri, K.; Braun, T.M.; Nguyen, H.Q.; Champlin, R.; Garcia-Manero, G. Maintenance therapy with low-dose azacitidine after allogeneic hematopoietic stem cell transplantation for recurrent acute myelogenous leukemia or myelodysplastic syndrome: a dose and schedule finding study. Cancer 2010, 116, 5420–5431. [Google Scholar] [CrossRef]
- Guillaume, T.; Malard, F.; Magro, L.; Labopin, M.; Tabrizi, R.; Borel, C.; Chevallier, P.; Vigouroux, S.; Peterlin, P.; Garnier, A.; et al. Prospective phase II study of prophylactic low-dose azacitidine and donor lymphocyte infusions following allogeneic hematopoietic stem cell transplantation for high-risk acute myeloid leukemia and myelodysplastic syndrome. Bone Marrow Transpl. 2019. [Google Scholar] [CrossRef] [PubMed]
- Oshikawa, G.; Kakihana, K.; Saito, M.; Aoki, J.; Najima, Y.; Kobayashi, T.; Doki, N.; Sakamaki, H.; Ohashi, K. Post-transplant maintenance therapy with azacitidine and gemtuzumab ozogamicin for high-risk acute myeloid leukaemia. Br. J. Haematol. 2015, 169, 756–759. [Google Scholar] [CrossRef] [PubMed]
- Platzbecker, U.; Wermke, M.; Radke, J.; Oelschlaegel, U.; Seltmann, F.; Kiani, A.; Klut, I.M.; Knoth, H.; Rollig, C.; Schetelig, J.; et al. Azacitidine for treatment of imminent relapse in MDS or AML patients after allogeneic HSCT: Results of the RELAZA trial. Leukemia 2012, 26, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Schmid, C.; Schleuning, M.; Ledderose, G.; Tischer, J.; Kolb, H.J. Sequential regimen of chemotherapy, reduced-intensity conditioning for allogeneic stem-cell transplantation, and prophylactic donor lymphocyte transfusion in high-risk acute myeloid leukemia and myelodysplastic syndrome. J. Clin. Oncol. 2005, 23, 5675–5687. [Google Scholar] [CrossRef] [PubMed]
- Balsat, M.; Renneville, A.; Thomas, X.; de Botton, S.; Caillot, D.; Marceau, A.; Lemasle, E.; Marolleau, J.P.; Nibourel, O.; Berthon, C.; et al. Postinduction Minimal Residual Disease Predicts Outcome and Benefit From Allogeneic Stem Cell Transplantation in Acute Myeloid Leukemia With NPM1 Mutation: A Study by the Acute Leukemia French Association Group. J. Clin. Oncol. 2017, 35, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Karas, M.; Steinerova, K.; Lysak, D.; Hrabetova, M.; Jungova, A.; Sramek, J.; Jindra, P.; Polivka, J.; Holubec, L. Pre-transplant Quantitative Determination of NPM1 Mutation Significantly Predicts Outcome of AIlogeneic Hematopoietic Stem Cell Transplantation in Patients with Normal Karyotype AML in Complete Remission. Anticancer Res. 2016, 36, 5487–5498. [Google Scholar] [CrossRef]
- Chyla, B.; Popovic, R.; Potluri, J.; Hayslip, J.; Huang, X.; Zhu, M.; Mabry, M.; Bhathena, A. Correlative Biomarkers of Response to Venetoclax in Combination with Chemotherapy or Hypomethylating Agents in Elderly Untreated Patients with Acute Myeloid Leukemia. Blood 2016, 128, 1709. [Google Scholar]
- Lambert, J.; Lambert, J.; Nibourel, O.; Pautas, C.; Hayette, S.; Cayuela, J.M.; Terre, C.; Rousselot, P.; Dombret, H.; Chevret, S.; et al. MRD assessed by WT1 and NPM1 transcript levels identifies distinct outcomes in AML patients and is influenced by gemtuzumab ozogamicin. Oncotarget 2014, 5, 6280–6288. [Google Scholar] [CrossRef] [PubMed]
- Olombel, G.; Guerin, E.; Guy, J.; Perrot, J.Y.; Dumezy, F.; de Labarthe, A.; Bastie, J.N.; Legrand, O.; Raffoux, E.; Plesa, A.; et al. The level of blast CD33 expression positively impacts the effect of gemtuzumab ozogamicin in patients with acute myeloid leukemia. Blood 2016, 127, 2157–2160. [Google Scholar] [CrossRef] [PubMed]
- Wei, A.; Strickland, S.A.; Hou, J.-Z.; Fiedler, W.; Lin, T.L.; Walter, R.B.; Enjeti, A.K.; Hong, W.-J.; Chyla, B.; Popovic, R.; et al. Venetoclax with Low-Dose Cytarabine Induces Rapid, Deep, and Durable Responses in Previously Untreated Older Adults with AML Ineligible for Intensive Chemotherapy. Blood 2018, 132, 284. [Google Scholar]
- Wei, A.H.; Chua, C.C.; Tiong, I.S.; Fong, C.Y.; Ting, S.B.; Macraild, S.; Salmon, J.M.; Ivey, A.; Nguyen, J.; Yuen, F.; et al. Molecular Patterns of Response and Outcome in the Chemotherapy and Venetoclax in Elderly AML Trial (CAVEAT study). Blood 2018, 132, 333. [Google Scholar]
- Sakaguchi, M.; Yamaguchi, H.; Najima, Y.; Usuki, K.; Ueki, T.; Oh, I.; Mori, S.; Kawata, E.; Uoshima, N.; Kobayashi, Y.; et al. Prognostic impact of low allelic ratio FLT3-ITD and NPM1 mutation in acute myeloid leukemia. Blood Adv. 2018, 2, 2744–2754. [Google Scholar] [CrossRef]
- Cornelissen, J.J.; Gratwohl, A.; Schlenk, R.F.; Sierra, J.; Bornhauser, M.; Juliusson, G.; Racil, Z.; Rowe, J.M.; Russell, N.; Mohty, M.; et al. The European LeukemiaNet AML Working Party consensus statement on allogeneic HSCT for patients with AML in remission: an integrated-risk adapted approach. Nat. Rev. Clin. Oncol. 2012, 9, 579–590. [Google Scholar] [CrossRef]
- Shouval, R.; Labopin, M.; Bondi, O.; Mishan-Shamay, H.; Shimoni, A.; Ciceri, F.; Esteve, J.; Giebel, S.; Gorin, N.C.; Schmid, C.; et al. Prediction of Allogeneic Hematopoietic Stem-Cell Transplantation Mortality 100 Days After Transplantation Using a Machine Learning Algorithm: A European Group for Blood and Marrow Transplantation Acute Leukemia Working Party Retrospective Data Mining Study. J. Clin. Oncol. 2015, 33, 3144–3151. [Google Scholar] [CrossRef]
- Bazarbachi, A.; Labopin, M.; Kharfan-Dabaja, M.A.; Schwerdtfeger, R.; Volin, L.; Bourhis, J.H.; Socie, G.; Daguindau, E.; Gedde-Dahl, T.; Rambaldi, A.; et al. Allogeneic hematopoietic cell transplantation in acute myeloid leukemia with normal karyotype and isolated Nucleophosmin-1 (NPM1) mutation: outcome strongly correlates with disease status. Haematologica 2016, 101, e34–e37. [Google Scholar] [CrossRef][Green Version]
- Poire, X.; Labopin, M.; Polge, E.; Blaise, D.; Chevallier, P.; Maertens, J.; Deconinck, E.; Forcade, E.; Rambaldi, A.; Baerlocher, G.M.; et al. Hematopoietic stem cell transplantation for adult patients with isolated NPM1 mutated acute myeloid leukemia in first remission. Am. J. Hematol. 2019, 94, 231–239. [Google Scholar] [CrossRef]
- Angenendt, L.; Rollig, C.; Montesinos, P.; Martinez-Cuadron, D.; Barragan, E.; Garcia, R.; Botella, C.; Martinez, P.; Ravandi, F.; Kadia, T.; et al. Chromosomal Abnormalities and Prognosis in NPM1-Mutated Acute Myeloid Leukemia: A Pooled Analysis of Individual Patient Data From Nine International Cohorts. J. Clin. Oncol. 2019, JCO–19, 00416. [Google Scholar] [CrossRef] [PubMed]
- Gorello, P.; Cazzaniga, G.; Alberti, F.; Dell’Oro, M.G.; Gottardi, E.; Specchia, G.; Roti, G.; Rosati, R.; Martelli, M.F.; Diverio, D.; et al. Quantitative assessment of minimal residual disease in acute myeloid leukemia carrying nucleophosmin (NPM1) gene mutations. Leukemia 2006, 20, 1103–1108. [Google Scholar] [CrossRef] [PubMed]
- Cheson, B.D.; Bennett, J.M.; Kopecky, K.J.; Buchner, T.; Willman, C.L.; Estey, E.H.; Schiffer, C.A.; Doehner, H.; Tallman, M.S.; Lister, T.A.; et al. Revised recommendations of the International Working Group for Diagnosis, Standardization of Response Criteria, Treatment Outcomes, and Reporting Standards for Therapeutic Trials in Acute Myeloid Leukemia. J. Clin. Oncol. 2003, 21, 4642–4649. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | All Patients N = 89 | MRD Negative, N = 30 | MRD Positive, N = 42 | p^ |
|---|---|---|---|---|
| Age, median (range) | 54 (16–73) | 52.5 (19–68) | 54.5 (22–68) | 0.97 |
| Sex, N (%) | 0.55 | |||
| Male | 41 (46.1) | 15 (50) | 18 (42.9) | |
| Female | 48 (53.9) | 15 (50) | 24 (57.1) | |
| LDH U/L, median (range) | 1124.5 (301–6000) | 819 (355–2550) | 1371 (351–4382) | 0.06 |
| WBC (×109/L), median (range) | 33.1 (1.2–262.9) | 17.4 (1.3–180) | 73 (2–262.9) | 0.0004 |
| Hemoglobin (g/dL), median (range) | 8.9 (0.4–13.9) | 8 (3.3–13.9) | 9.3 (5.7–13.8) | 0.07 |
| Platelets (×109/L), median (range) | 51 (5–698) | 46 (6–393) | 53 (13–698) | 0.47 |
| Cytogenetic | 0.30 | |||
| Normal karyotype | 84 (94.4) | 27 (90.0) | 41 (97.6) | |
| Abnormal ° | 5 (5.6) | 3 (10.0) | 1 (2.4) | |
| FLT3-ITD, N (%) | 1.00 | |||
| Negative | 56 (66.7) | 19 (65.5) | 24 (63.2) | |
| Positive§, allelic ratio <0.5 | 10 (11.9) | 3 (10.3) | 4 (10.5) | |
| Positive§, allelic ratio ≥0.5 | 18 (21.4) | 7 (24.1) | 10 (26.3) | |
| MRD post consolidation #, N (%) | - | |||
| Negative | 30 (41.7) | 30 (41.7) | - | |
| Positive ≤0.1 | 10 (13.9) | - | 10 (23.8) | |
| Positive >0.1 | 32 (44.4) | - | 32 (76.2) | |
| Consolidation | 0.11 | |||
| No alloHSCT | 32 (37.2) | 12 (40) | 9 (22.5) | |
| AlloHSCT * | 54 (62.8) | 18 (60) | 31 (77.5) | |
| Donor type, N (%) | 0.31 | |||
| Sibling | 10 (18.5) | 1 (5.6) | 8 (25.8) | |
| Unrelated | 35 (64.8) | 15 (83.3) | 17 (48.4) | |
| Cord Blood | 6 (11.1) | 1 (5.6) | 4 (12.9) | |
| Haploidentical | 3 (5.6) | 1 (5.6) | 2 (6.5) |
| Factors | Univariate | Multivariable | ||
|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | |
| Consolidation # | ||||
| With AlloHSCT | 1.00 | 1.00 | ||
| Without AlloHSCT | 1.31 (0.59–2.89) | 0.51 | 0.31 (0.08–1.19) | 0.08 |
| Age (years) | 1.02 (0.99–1.05) | 0.24 | 1.03 (0.97–1.1) | 0.33 |
| WBC (×109/L) | 1.01 (1–1.01) | 0.03 | 1.00 (0.99–1.01) | 0.98 |
| FLT3-ITD | ||||
| Negative | 1.00 | 1.00 | ||
| Positive, allelic ratio < 0.5 | 10.95 (3.9–30.71) | <0.0001 | 13.53 (2.87–63.78) | 0.001 |
| Positive, allelic ratio ≥ 0.5 | 8.19 (3.15–21.29) | <0.0001 | 13.29 (3.33–53.01) | 0.0002 |
| MRD post-consolidation * | ||||
| Negative | 1.00 | 1.00 | ||
| Positive ≤ 0.1 | 2.21 (0.49–9.88) | 0.30 | 12.55 (1.83–86.11) | 0.01 |
| Positive > 0.1 | 5.6 (1.87–16.79) | 0.002 | 6.54 (1.71–25.04) | 0.006 |
| Factors | Univariate | Multivariable | ||
|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | |
| Consolidation # | ||||
| With AlloHSCT | 1.00 | 1.00 | ||
| Without AlloHSCT | 0.75 (0.39–1.43) | 0.38 | 0.25 (0.07–0.86) | 0.03 |
| Age (years) | 1.01 (0.98–1.04) | 0.37 | 1.00 (0.95–1.06) | 0.89 |
| WBC (×109/L) | 1.01 (1.00–1.01) | 0.03 | 1.00 (1.00–1.01) | 0.27 |
| FLT3-ITD | ||||
| Negative | 1.00 | 1.00 | ||
| Positive, allelic ratio < 0.5 | 5.52 (2.22–13.73) | 0.0002 | 8.11 (2–32.84) | 0.003 |
| Positive, allelic ratio ≥ 0.5 | 5.07 (2.27–11.3) | 0.0001 | 11.18 (3.32–37.7) | 0.0001 |
| MRD post-consolidation * | ||||
| Negative | 1.00 | 1.00 | ||
| Positive ≤ 0.1 | 1.98 (0.56–7.01) | 0.29 | 8.71 (1.49–50.88) | 0.02 |
| Positive > 0.1 | 4.04 (1.59–10.28) | 0.003 | 5.66 (1.68–19.04) | 0.005 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lussana, F.; Caprioli, C.; Stefanoni, P.; Pavoni, C.; Spinelli, O.; Buklijas, K.; Michelato, A.; Borleri, G.; Algarotti, A.; Micò, C.; et al. Molecular Detection of Minimal Residual Disease before Allogeneic Stem Cell Transplantation Predicts a High Incidence of Early Relapse in Adult Patients with NPM1 Positive Acute Myeloid Leukemia. Cancers 2019, 11, 1455. https://doi.org/10.3390/cancers11101455
Lussana F, Caprioli C, Stefanoni P, Pavoni C, Spinelli O, Buklijas K, Michelato A, Borleri G, Algarotti A, Micò C, et al. Molecular Detection of Minimal Residual Disease before Allogeneic Stem Cell Transplantation Predicts a High Incidence of Early Relapse in Adult Patients with NPM1 Positive Acute Myeloid Leukemia. Cancers. 2019; 11(10):1455. https://doi.org/10.3390/cancers11101455
Chicago/Turabian StyleLussana, Federico, Chiara Caprioli, Paola Stefanoni, Chiara Pavoni, Orietta Spinelli, Ksenija Buklijas, Anna Michelato, GianMaria Borleri, Alessandra Algarotti, Caterina Micò, and et al. 2019. "Molecular Detection of Minimal Residual Disease before Allogeneic Stem Cell Transplantation Predicts a High Incidence of Early Relapse in Adult Patients with NPM1 Positive Acute Myeloid Leukemia" Cancers 11, no. 10: 1455. https://doi.org/10.3390/cancers11101455
APA StyleLussana, F., Caprioli, C., Stefanoni, P., Pavoni, C., Spinelli, O., Buklijas, K., Michelato, A., Borleri, G., Algarotti, A., Micò, C., Grassi, A., Intermesoli, T., & Rambaldi, A. (2019). Molecular Detection of Minimal Residual Disease before Allogeneic Stem Cell Transplantation Predicts a High Incidence of Early Relapse in Adult Patients with NPM1 Positive Acute Myeloid Leukemia. Cancers, 11(10), 1455. https://doi.org/10.3390/cancers11101455





