The Elias University Hospital Approach: A Visual Guide to Ultrasound-Guided Botulinum Toxin Injection in Spasticity, Part IV—Distal Lower Limb Muscles
Abstract
1. Introduction
2. General Methodology
3. Distal Lower Limb Muscles Implicated in Post-Stroke Spasticity
3.1. Gastrocnemius Muscles (Gastroc)
3.1.1. Overview
3.1.2. Lateral Head of Gastrocnemius (LG)
Ultrasound Identification
Key Ultrasound Landmarks
- Muscle position: It is the most superficial and prominent muscle in the posterior compartment of the leg, and one of the largest in the region. The soleus—and, if present, the plantaris—is located deep to it.
- External fascia: It presents a well-defined fascia separating it from the subcutaneous plane, soleus, and plantaris muscle/tendon, during BoNT-A injection.
- Dynamic evaluation: During dynamic evaluation, scanning toward the ankle joint, the lateral head of the gastrocnemius progressively decreases and eventually disappears while the soleus increases in thickness; distally, both merge into the Achilles tendon with the soleus (and plantaris, if present). On medial scanning the intersection of the lateral and medial gastrocnemius heads is visualized—the medial sural cutaneous nerve typically courses between these heads. Because the gastrocnemius is a biarticular muscle crossing both the knee and ankle joints, it is assessed with the knee extended to place the muscle on maximal stretch and thereby reveal its contribution to ankle plantarflexion. Muscle contraction is visible during plantar flexion of the foot at the ankle joint, as well as during knee flexion.
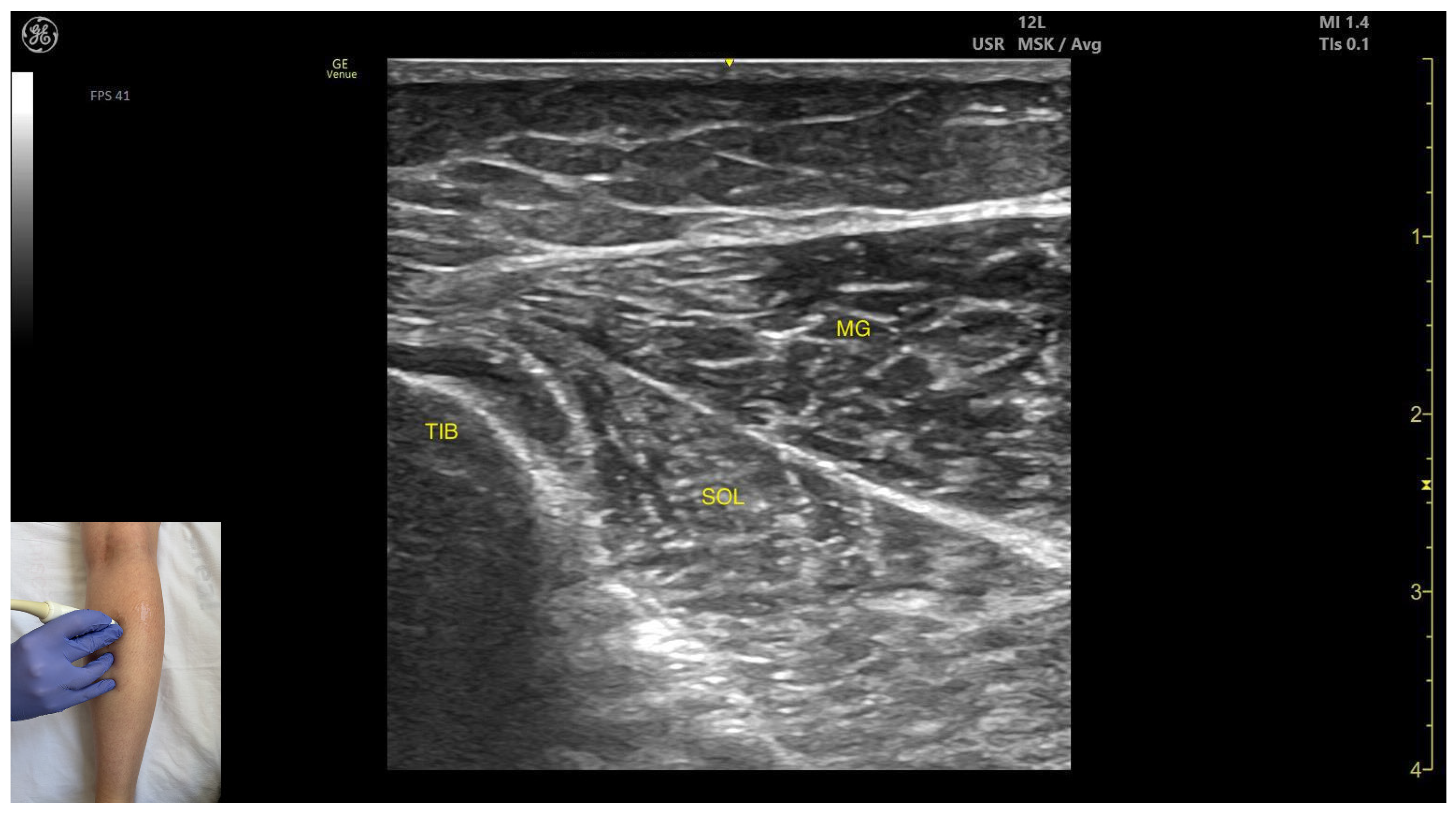
3.1.3. Medial Head of Gastrocnemius (MG)
Ultrasound Identification
Key Ultrasound Landmarks
- Muscle position: It is the most superficial and prominent, and of the largest muscles in the posterior compartment of the leg. The soleus—and if present, the plantaris—is located deep to it.
- Muscle morphology: The medial head of the gastrocnemius is larger and extends more distally than the lateral head of the gastrocnemius.
- External fascia: It presents a well-defined fascia separating it from the subcutaneous plane, soleus, and plantaris muscle/tendon aiding in safe BoNT-A injection.
- Dynamic evaluation: During dynamic evaluation, scanning toward the ankle joint reveals the medial head of the gastrocnemius progressively decreases and eventually disappears while the soleus increases in thickness; further distally, both converge to form the calcaneal (Achilles) tendon, often with the plantaris tendon interposed when present. On lateral scanning the intersection of the medial and lateral gastrocnemius heads is visualized—the medial sural cutaneous nerve typically courses between these heads. The gastrocnemius, spanning both the knee and ankle joints as a biarticular muscle, is evaluated with the knee fully extended to place it under maximal longitudinal tension, thereby accentuating its functional role in ankle plantarflexion. Contraction is visible during plantar flexion of the foot at the ankle joint, as well as during knee flexion.
3.1.4. Clinical Implications & Injection Strategy
3.2. Soleus (SOL)
3.2.1. Overview
3.2.2. Ultrasound Identification
3.2.3. Key Ultrasound Landmarks:
- Muscle morphology: It appears as a flat muscle in the posterior compartment of the leg.
- Muscle position: At this level, the soleus lies deep to the intersection of the gastrocnemius heads, within which the medial sural cutaneous nerve courses.
- External fascia: A pronounced fascia separates it from the subcutaneous plane, gastrocnemius muscles, and the plantaris muscle/tendon (if present), which is relevant during BoNT-A injection.
- Dynamic evaluation: During dynamic evaluation, scanning laterally reveals enlargement of the lateral gastrocnemius head, and deep to the soleus, the neurovascular bundle emerges, comprising the posterior tibial artery, the two posterior tibial veins, and the posterior tibial nerve. Medial scanning highlights enlargement of the medial head of the gastrocnemius (MG), while the neurovascular bundle maintains its anatomical course. The soleus, a monoarticular muscle acting exclusively at the ankle joint, is optimally assessed with the knee flexed; this positioning diminishes gastrocnemius involvement, allowing for isolated evaluation of soleus contractile activity via EMG or dynamic ultrasound imaging. Muscle contraction is visible during plantar flexion maneuvers of the foot at the ankle joint.
3.2.4. Clinical Implications and Injection Strategy
3.3. Tibialis Posterior (TP)
3.3.1. Overview
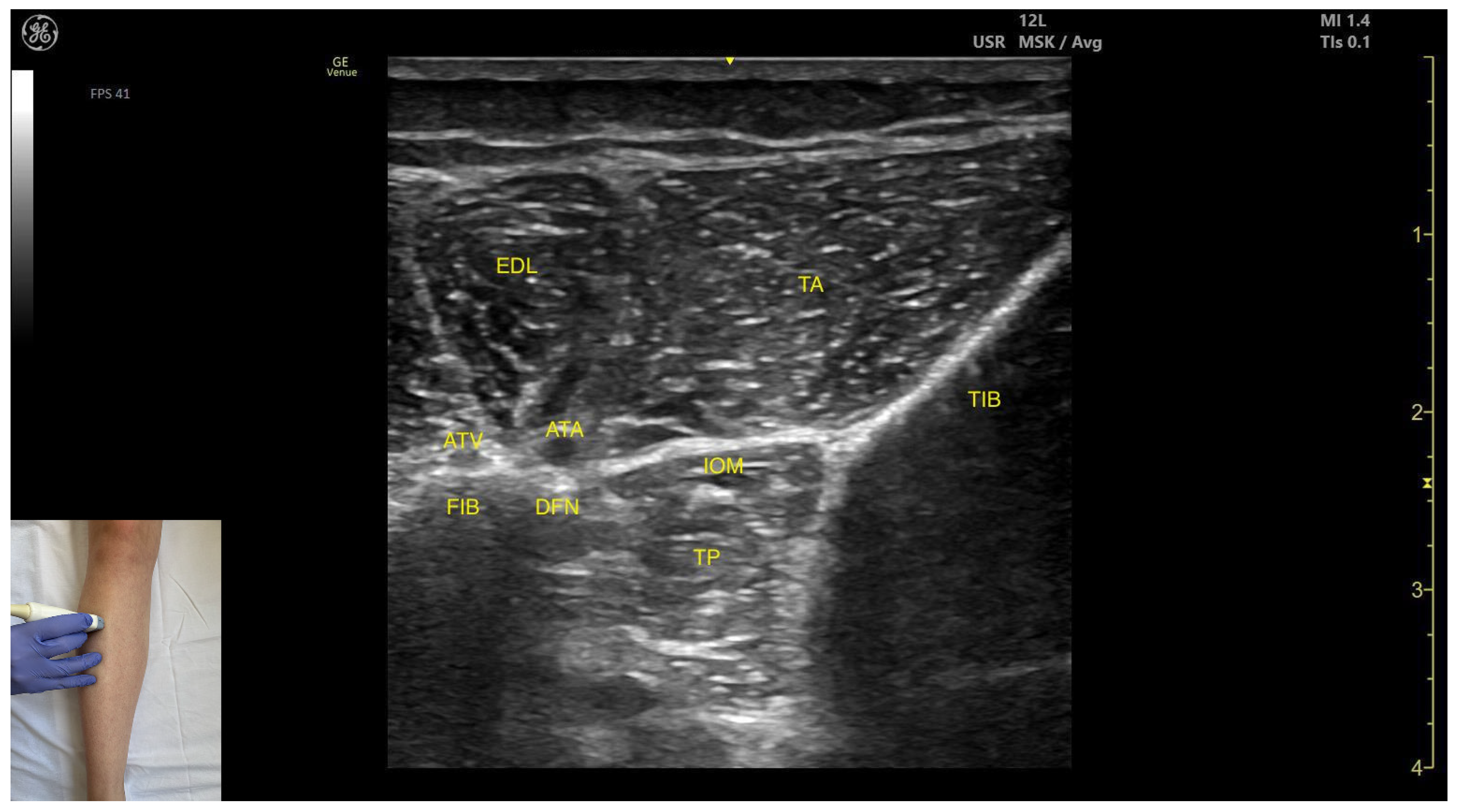
3.3.2. Anterior Window
Ultrasound Identification
Key Ultrasound Landmarks
- Muscle position: It is the deepest muscle in the posterior compartment of the leg.
- Neurovascular bundle: Superficial to the interosseous membrane lies the neurovascular bundle composed of the deep peroneal nerve, anterior tibial artery, and anterior tibial vein.
- External fascia: TP has a pronounced fascia that separates it from the tibialis anterior and extensor digitorum longus during BoNT-A injection.
- Dynamic evaluation: During dynamic evaluation muscle contraction is visible during inversion and plantar flexion of the ankle joint.
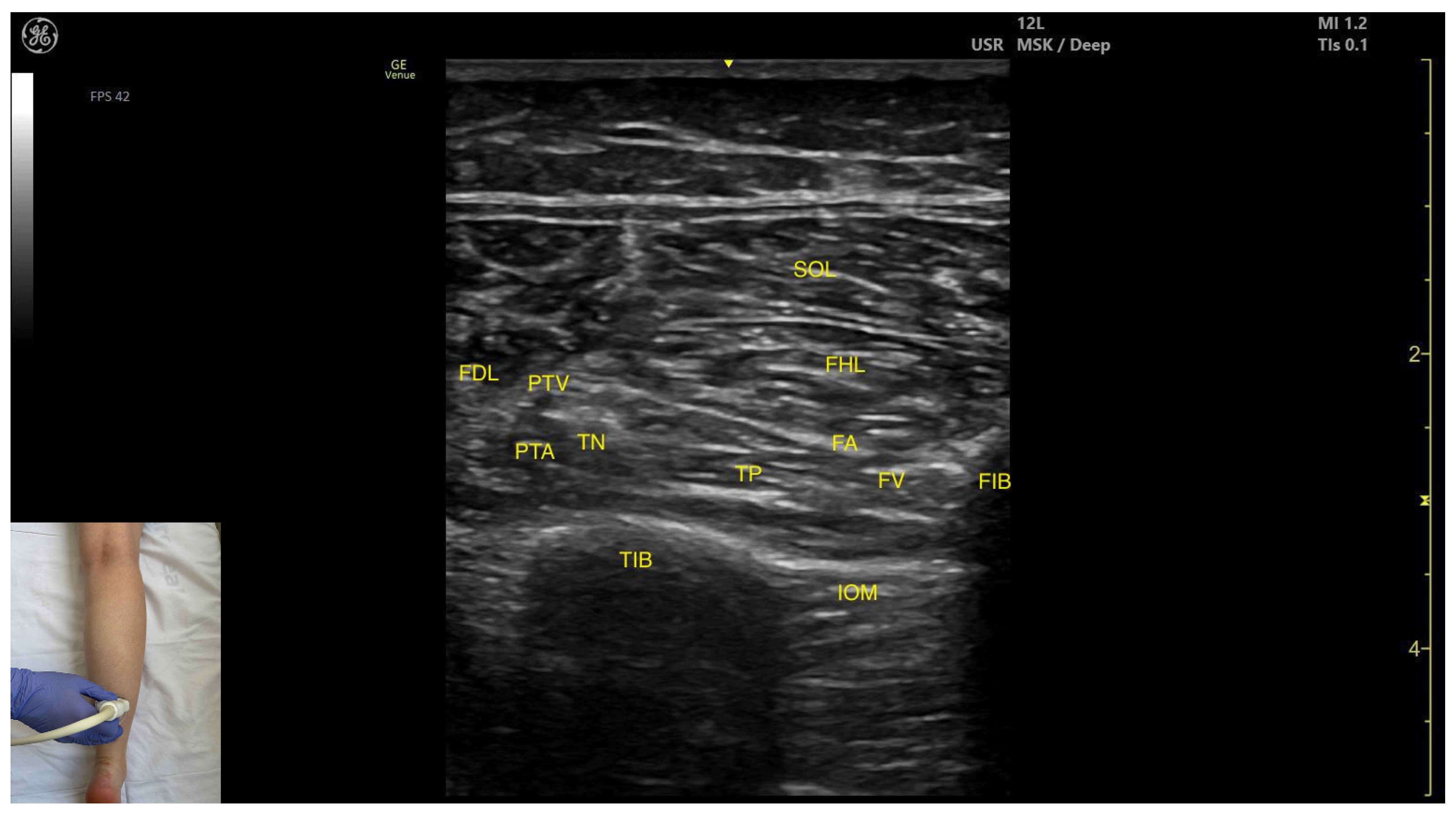
3.3.3. Medial Window
Ultrasound Identification
Key Ultrasound Landmarks
- Muscle position: The tibialis posterior is the deepest muscle in the posterior compartment of the leg. It is bordered superficially and medially by the flexor digitorum longus and superficially and laterally by the flexor hallucis longus. The interosseous membrane lies deep to the TP.
- Neurovascular bundle: Within the intermuscular fascial plane between the flexor digitorum longus, flexor hallucis longus, and soleus, the tibial nerve, posterior tibial artery, and posterior tibial vein are situated.
- External fascia: The TP does not have a well-defined fascia that separates it from flexor digitorum longus and flexor hallucis longus, during BoNT-A injection.
- Dynamic evaluation: Muscle contraction becomes evident during ankle inversion and plantar flexion at the ankle joint.
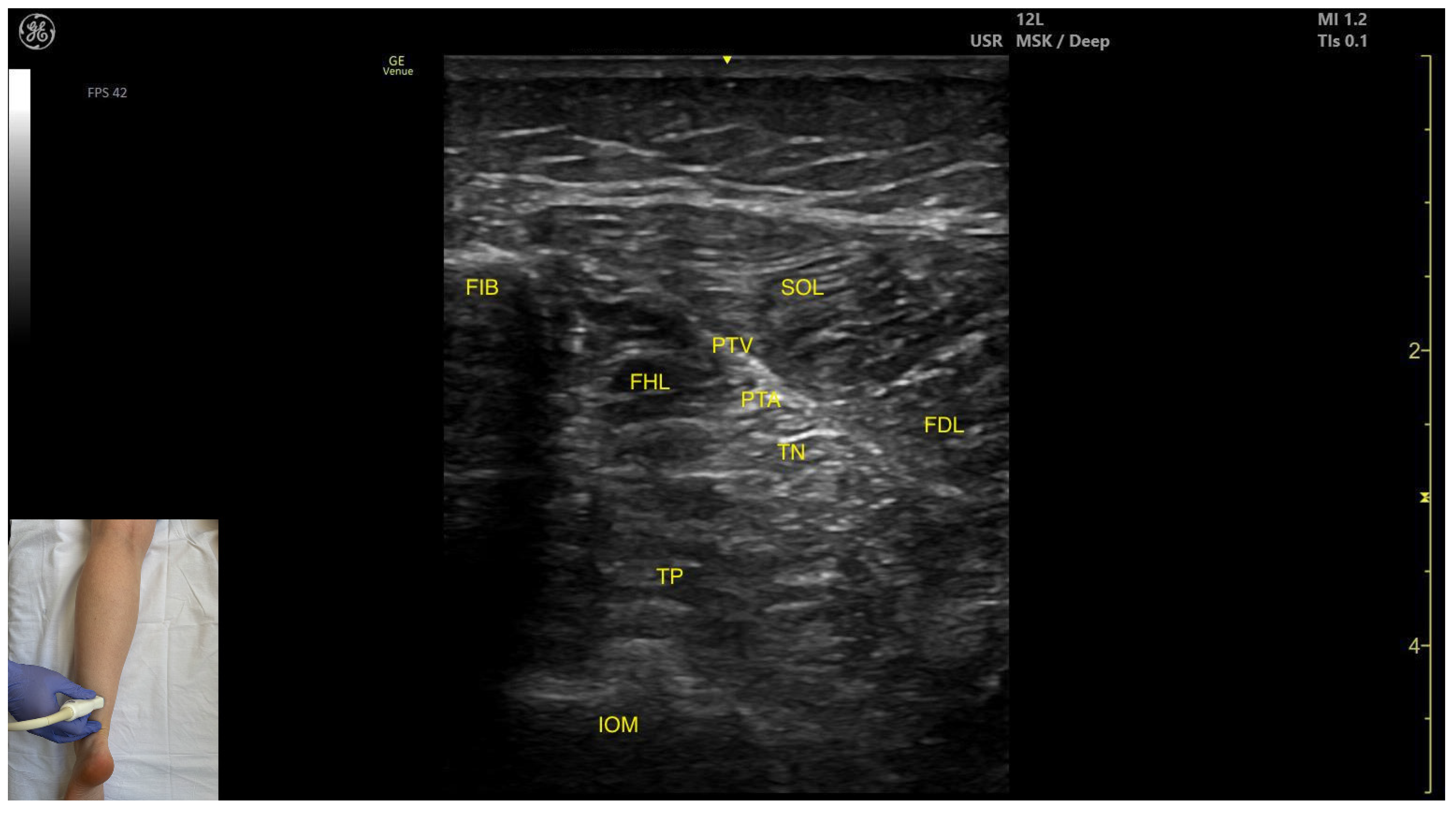
3.3.4. Posterior Window
Ultrasound Identification
Key Ultrasound Landmarks
- Muscle position: The tibialis posterior is the deepest muscle in the posterior compartment of the leg. It is bordered superficially and medially by the flexor digitorum longus, and superficially and laterally by the flexor hallucis longus. The interosseous membrane is located deep to the TP.
- Neurovascular bundle: In the intermuscular fascia between the TP and the FHL run the fibular artery and vein. Additionally, in the intermuscular fascia formed by the soleus, FDL and FHL are the tibial nerve, the posterior tibial artery and the posterior tibial vein.
- External fascia: The TP has pronounced fascia that separates it from the flexor digotorum longus and the flexor hallucis longus, which is relevant for BoNT-A injection.
- Dynamic evaluation: Muscle contraction is visible during ankle inversion and plantar flexion at the ankle joint.
3.3.5. Clinical Implications and Injection Strategy
3.4. Flexor Hallucis Longus (FHL)
3.4.1. Overview
3.4.2. Ultrasound Identification
3.4.3. Key Ultrasound Landmarks
- Muscle morphology: It is a strong, unipennate muscle. In our clinical practice it is referred to as the “shark tail”
- Muscle position: It is located superficial to the fibular cortex. The SOL lies superficial to the FHL. Deep and medial to it lies the tibialis posterior (TP) and, deep to TP, the interosseous membrane. Medial to this region is the flexor digitorum longus (FDL). At this level, the usual anatomical relationship of the FHL and FDL is paradoxically reversed.
- Neurovascular bundle: The tibial nerve, posterior tibial artery, and posterior tibial vein lie within the intermuscular fascia between tibialis posterior, SOL, FDL.
- External fascia: The FHL has a well-defined fascia that separates it from soleus, aiding in safe BoNT-A injection. It does not have a pronounced fascia that separates it from the tibialis posterior and flexor digitorum longus.
- Dynamic evaluation: During dynamic evaluation, scanning proximally toward the knee joint, the FHL muscle thickness decreases, and it disappears from view, while the soleus thickens and the lateral head of the gastrocnemius appears superficially (Video S1). Muscle contraction is seen during flexion of the hallux at the metatarsophalangeal and interphalangeal joints, as well as during plantar flexion at the ankle joint.
3.4.4. Clinical Implications and Injection Strategy
3.5. Flexor Digitorum Longus (FDL)
3.5.1. Overview
3.5.2. Ultrasound Identification
3.5.3. Key Ultrasound Landmarks
- Muscle position: It is located in the medial compartment of the posterior leg. Superficially, it is covered by the soleus; lateral to the FDL lies the flexor hallucis longus; deep and lateral to it lie the TP with the interosseous membrane located beneath it. At this level, the flexor digitorum longus and flexor hallucis longus are paradoxically reversed in position relative to their usual anatomical course.
- Neurovascular bundle: Within the intermuscular fascia between the flexor digitorum longus, flexor hallucis longus, and soleus are the tibial nerve, posterior tibial artery, and posterior tibial veins.
- External fascia: The FDL has a well-defined fascia that separates it from the soleus, which is relevant during BoNT-A injection. It does not have a pronounced fascia that separates it from the flexor hallucis longus and tibialis posterior.
- Dynamic evaluation: During dynamic evaluation, scanning proximally toward the knee joint, the flexor digitorum longus decreases in thickness and disappears from view, while the soleus increases in size and the medial head of the gastrocnemius appears superficial to the soleus (Video S2). Muscle contraction is visible during flexion of toes II–V (at metatarsophalangeal, proximal and distal interphalangeal joints) and ankle plantar flexion.
3.5.4. Clinical Implications and Injection Strategy
3.6. Tibialis Anterior (TA)
3.6.1. Overview
3.6.2. Ultrasound Identification
3.6.3. Key Ultrasound Landmarks
- Muscle position: It appears as a superficial muscle mass. Deep to the TA lies the interosseous membrane separating it from the tibialis posterior; the extensor digitorum longus lies lateral to the TA.
- External fascia: The TA does not feature a pronounced fascia that separates it from extensor digitorum longus, during BoNT-A injection.
- Dynamic evaluation: During dynamic evaluation, scanning distally toward the ankle, the tibialis anterior decreases in thickness as it transitions into its tendon. Muscle contraction is seen during plantar dorsiflexion and inversion of the ankle joint.
3.6.4. Clinical Implications and Injection Strategy
3.7. Extensor Hallucis Longus (EHL)
3.7.1. Overview
3.7.2. Ultrasound Identification
3.7.3. Key Ultrasound Landmarks
- Muscle morphology: It is an unipennate muscle.
- Muscle position: It appears as a superficial muscle mass at this level. Laterally, the extensor digitorum longus (EDL) is visualized; superficially and laterally is the tendinous portion of the tibialis anterior (TA). Deep to the EHL lie the interosseous membrane and the tibialis posterior (TP).
- External fascia: The ELH does not have a well-defined fascia that separates it from the subcutaneous plane, the extensor digitorum longus, tibialis anterior. The interosseous membrane separates the EHL from the tibialis posterior, during BoNT-A injection.
- Dynamic evaluation: During dynamic evaluation, scanning proximally toward the knee joint shows a reduction in EHL muscle thickness with a concurrent increase in tibialis muscle thickness (Video S3). Muscle contraction is visible during hallux extension at the metatarsophalangeal and interphalangeal joints and during dorsiflexion at the ankle joint. It is clinically relevant in relation to the Babinski sign, often referred to as the “hitchhiker’s great toe,” which is characterized by dorsiflexion of the hallux in response to stimulation of the plantar surface of the foot.
3.7.4. Clinical Implications and Injection Strategy
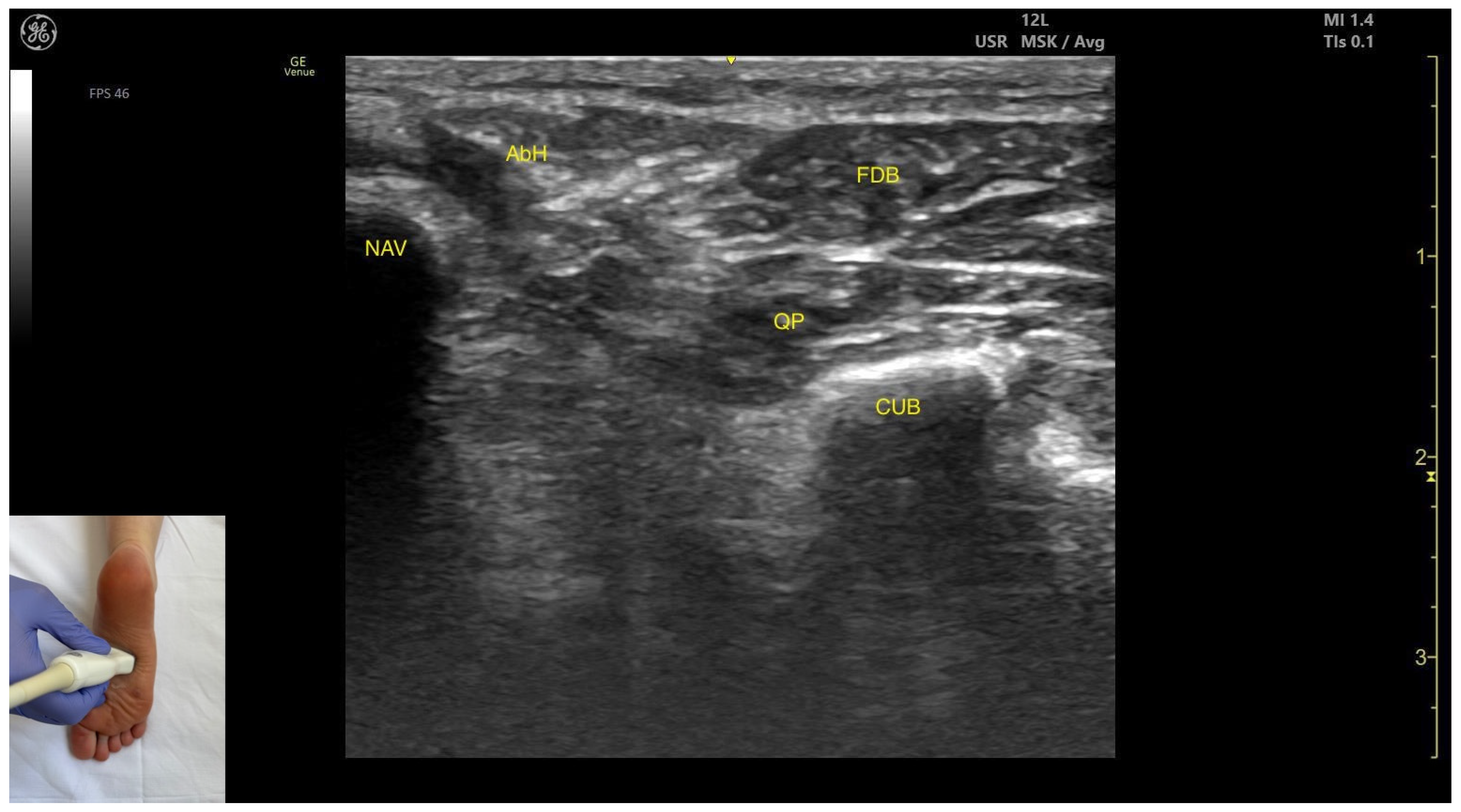
3.8. Flexor Digitorum Brevis (FDB)
3.8.1. Overview
3.8.2. Ultrasound Identification
3.8.3. Key Ultrasound Landmarks
- Muscle position: It is a superficial plantar muscle layer. The quadratus plantae is located deep to the FDB. Medial to the FDB and quadratus plantae the abductor hallucis (AbH) is identified.
- External fascia: It features a prominent fascia separating it from the subcutaneous tissue, plantar aponeurosis and from the quadratus plantae, which is important during BoNT-A injection.
- Dynamic evaluation: During dynamic evaluation, scanning toward the calcaneous, a reduction in muscle thickness of the flexor digitorum brevis is observed. Muscle contraction is visible during flexion of toes II–V at the proximal interphalangeal joints (Video S4).
3.8.4. Clinical Implications and Injection Strategy
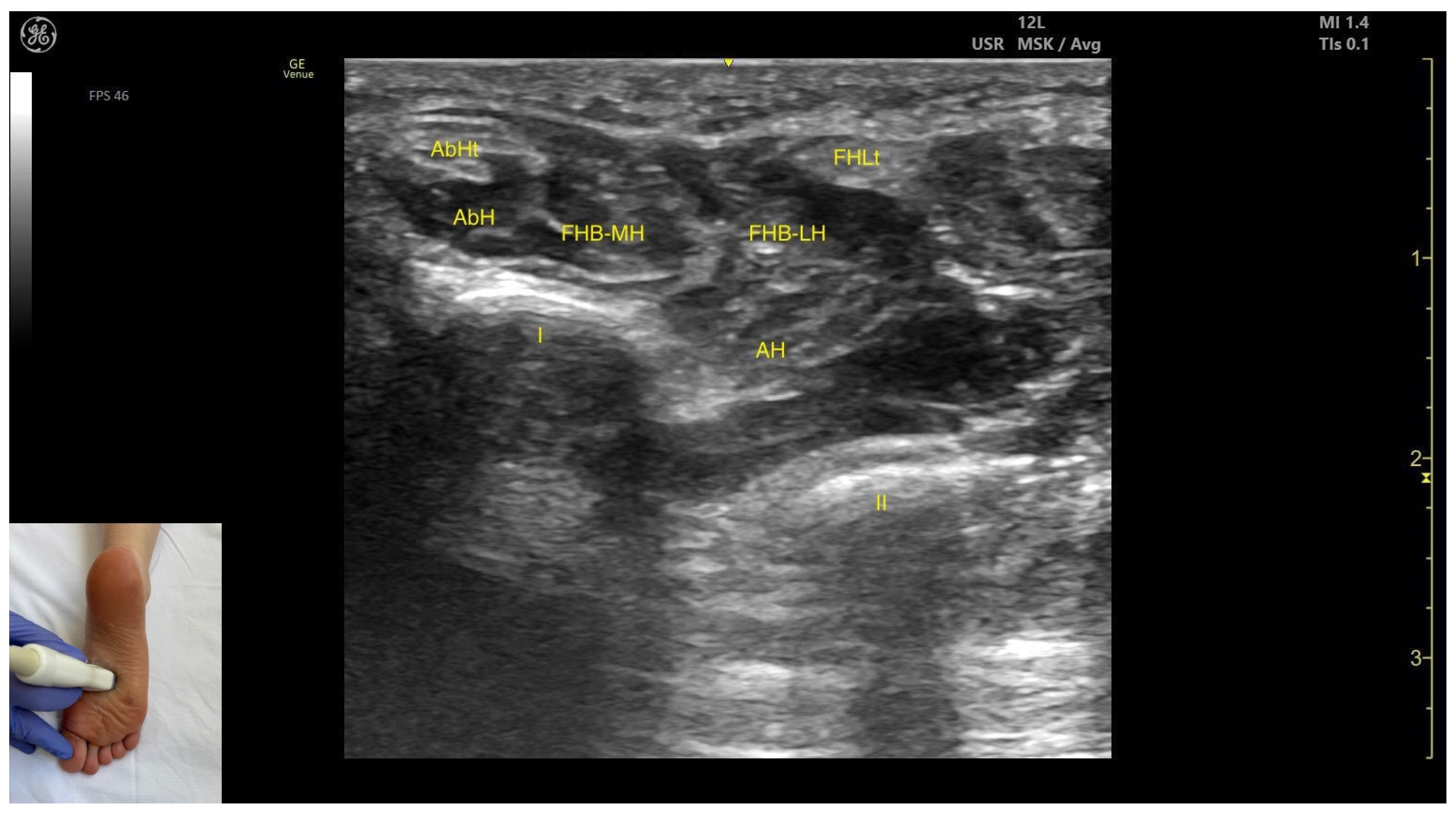
3.9. Flexor Hallucis Brevis (FHB)
3.9.1. Overview
3.9.2. Ultrasound Identification
3.9.3. Key Ultrasound Landmarks
- Muscle position: It appears as a superficial muscle mass at this level. Medially, the abductor hallucis muscle and tendon are present; laterally, the tendon of the flexor hallucis longus is visible. Deep and medial to the FHB lies the adductor hallucis.
- Muscle morphology: It has two heads—medial and lateral—that can be targeted individually during BonT-A injection.
- External fascia: FHB has a pronounced fascia that separates it from the superficial tissue, the abductor hallucis muscle, and the tendon of the flexor hallucis longus, during BoNT-A injection.
- Dynamic evaluation: During dynamic evaluation, scanning distally toward the first metatarsophalangeal joint, a decrease in muscle thickness of the flexor hallucis brevis is observed along with its insertion on the medial and lateral sides of the proximal phalanx of the hallux. Muscle contraction is visible during dynamic evaluation when performing hallux flexion at the first metatarsophalangeal joint.
3.9.4. Clinical Implications and Injection Strategy
- hallux claw foot deformity and hallux claw toe, which include hallux extension at the metatarsophalangeal joint and hallux flexion at the interphalangeal joint
3.10. Extensor Digitorum Longus (EDL)
3.10.1. Overview
3.10.2. Ultrasound Identification
3.10.3. Key Ultrasound Landmarks
- Muscle position: It occupies the most posterior and lateral position within the anterior compartment of the leg. It lies superficially beneath the subcutaneous plane. Medial to it lies the tibialis anterior; lateral to it lies the fibularis longus.
- Neurovascular bundle: The superficial fibular nerve courses within the intermuscular fascia between the EDL and fibularis longus. Deep structures include the interosseous membrane, tibialis posterior muscle, deep fibular nerve, and the anterior tibial artery.
- External fascia: It presents a pronounced fascia that demarcates it from the superficial plane and adjacent muscles (tibialis anterior and tibialis posterior), aiding in safe BoNT-A injection.
- Dynamic evaluation: During dynamic evaluation, scanning toward the ankle joint, the EDL muscle thickness decreases as the EHL appears deep to it. Muscle contraction is visible during toe extension of digits II–V and dorsiflexion at the ankle joint.
3.10.4. Clinical Implications and Injection Strategy
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BoNT-A | Botulinum toxin type A |
| EUH | Elias University Hospital |
| Gastroc | Gastrocnemius |
| LG | Lateral head of gastrocnemius |
| MG | Medial head of gastrocnemius |
| SOL | Soleus |
| FIB | Fibula |
| TIB | Tibia |
| US | Ultrasound |
| MAS | Modified Ashworth Scale |
| PROM | Passive range of motion |
| GMFM | Gross Motor Function Measure |
| TP | Tibialis posterior |
| ATV | Anterior tibial vein |
| ATA | Anterior tibial artery |
| DFN | Deep fibular nerve |
| EDL | Extensor digitorum longus |
| TA | Tibialis anterior |
| IOM | Interosseous membrane |
| FDL | Flexor digitorum longus |
| FHL | Flexor hallucis longus |
| PTA | Posterior tibial artery |
| PTV | Posterior tibial vein |
| TN | Tibial nerve |
| FA | Fibular artery |
| FV | Fibular vein |
| EHL | Extensor hallucis longus |
| TAt | Tibialis anterior tendon |
| FDB | Flexor digitorum brevis |
| NAV | Navicular |
| AH | Adductor hallucis |
| QP | Quadratus plantae |
| CUB | Cuboid |
| FHB | Flexor hallucis brevis |
| AbH | Abductor hallucis |
| FHB-MH | Flexor hallucis brevis medial head |
| FHB-LH | Flexor hallucis brevis lateral head |
| FL | Fibularis longus |
| SFN | Superficial fibular nerve |
| MSCN | Medial sural cutaneous nerve |
| EMG | Electromyography |
| FDB2 | Flexor digitorum brevis to second toe |
| FDB3 | Flexor digitorum brevis to third toe |
| FDB4 | Flexor digitorum brevis to fourth toe |
| FDB5 | Flexor digitorum brevis to fifth toe |
References
- Zeng, H.; Chen, J.; Guo, Y.; Tan, S. Prevalence and Risk Factors for Spasticity After Stroke: A Systematic Review and Meta-Analysis. Front. Neurol. 2021, 11, 616097. [Google Scholar] [CrossRef]
- Kaymak, B.; Kara, M.; Tok, F.; Ulaşli, A.M.; Öztürk, G.T.; Chang, K.-V.; Hsïao, M.-Y.; Hung, C.-Y.; Yağiz On, A.; Özçakar, L. Sonographic Guide for Botulinum Toxin Injections of the Lower Limb: EUROMUSCULUS/USPRM Spasticity Approach. Eur. J. Phys. Rehabil. Med. 2018, 54, 486–498. [Google Scholar] [CrossRef] [PubMed]
- Alter, K.E.; Hallett, M.; Karp, B.; Lungu, C.; Hallett, M.; Karp, B.; Lungu, C.; Hallett, M.; Karp, B.; Hallett, M.; et al. Ultrasound-Guided Chemodenervation Procedures; Springer Publishing Company: Berlin/Heidelberg, Germany, 2012; ISBN 978-1-936287-60-4. [Google Scholar]
- Jost, W. (Ed.) Atlas of Botulinum Toxin Injection, 3rd ed.; Quintessence Publishing: Batavia, IL, USA, 2019; ISBN 978-1-78698-030-4. [Google Scholar]
- Popescu, M.N.; Petca, R.C.; Beiu, C.; Dumitrascu, M.C.; Petca, A.; Mehedintu, C.; Farcasanu, P.D.; Sandru, F. Efficiency of Different Preparations of Botulinum Toxin Type A, Xeomin and Dysport, in the Management of Spastic Upper Limb After Stroke. Rev. De Chim. 2019, 70, 3490–3494. [Google Scholar] [CrossRef]
- Popescu, M.N.; Căpeț, C.; Beiu, C.; Berteanu, M. The Elias University Hospital Approach: A Visual Guide to Ultrasound-Guided Botulinum Toxin Injection in Spasticity: Part III—Proximal Lower Limb Muscles. Toxins 2025, 17, 240. [Google Scholar] [CrossRef] [PubMed]
- Popescu, M.N.; Căpeț, C.; Beiu, C.; Berteanu, M. The Elias University Hospital Approach: A Visual Guide to Ultrasound-Guided Botulinum Toxin Injection in Spasticity: Part I—Distal Upper Limb Muscles. Toxins 2025, 17, 107. [Google Scholar] [CrossRef]
- Popescu, M.N.; Căpeț, C.; Beiu, C.; Berteanu, M. The Elias University Hospital Approach: A Visual Guide to Ultrasound-Guided Botulinum Toxin Injection in Spasticity: Part II—Proximal Upper Limb Muscles. Toxins 2025, 17, 276. [Google Scholar] [CrossRef]
- Drake, R.L.; Vogl, W.A.; Mitchell, A.W.M. Gray’s Anatomy for Students; Elsevier: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Picelli, A.; Di Censo, R.; Angeli, C.; Spina, S.; Santamato, A.; Baricich, A.; Smania, N.; Filippetti, M. Is the Silfverskiöld Test a Valid Tool for Evaluating Calf Muscles Spastic Overactivity in Patients with Stroke? A Retrospective Observational Study. Eur. J. Phys. Rehabil. Med. 2024, 60, 761–766. [Google Scholar] [CrossRef]
- Moore, K.; Agur, A.; Dalley, A. Clinically Oriented Anatomy, 8th ed.; Moore, K.L., Dalley, A.F., II, Agur, A.M.R., Eds.; Wolters Kluwer: Alphen aan den Rijn, The Netherlands, 2018. [Google Scholar]
- Olewnik, Ł.; Wysiadecki, G.; Podgórski, M.; Polguj, M.; Topol, M. The Plantaris Muscle Tendon and Its Relationship with the Achilles Tendinopathy. BioMed Res. Int. 2018, 2018, 9623579. [Google Scholar] [CrossRef]
- Patra, A.; Tiwari, V.; Chaudhary, P.; Asghar, A.; Kaur, H.; Trzeciak, M.; Paziewski, M.; Sychta, M.; Mazur, M.; Walocha, J.A. Newly Proposed Classification of Plantaris Tendon Insertion Based on Branching Patterns: A Morphological Study. Folia Morphol. 2025; online first. [Google Scholar] [CrossRef]
- Netter, F.H. Atlas of Human Anatomy, 6th ed.; Elsevier: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Arampatzis, A.; Kharazi, M.; Theodorakis, C.; Mersmann, F.; Bohm, S. Biarticular Mechanisms of the Gastrocnemii Muscles Enhance Ankle Mechanical Power and Work during Running. R. Soc. Open Sci. 2023, 10, 230007. [Google Scholar] [CrossRef]
- Lenhart, R.L.; Francis, C.A.; Lenz, A.L.; Thelen, D.G. Empirical Evaluation of Gastrocnemius and Soleus Function during Walking. J. Biomech. 2014, 47, 2969–2974. [Google Scholar] [CrossRef]
- Santamato, A.; Cinone, N.; Panza, F.; Letizia, S.; Santoro, L.; Lozupone, M.; Daniele, A.; Picelli, A.; Baricich, A.; Intiso, D.; et al. Botulinum Toxin Type A for the Treatment of Lower Limb Spasticity after Stroke. Drugs 2019, 79, 143–160. [Google Scholar] [CrossRef] [PubMed]
- Gracies, J.-M. Physiological Effects of Botulinum Toxin in Spasticity. Mov. Disord. 2004, 19, S120–S128. [Google Scholar] [CrossRef] [PubMed]
- Picelli, A.; Tamburin, S.; Bonetti, P.; Fontana, C.; Barausse, M.; Dambruoso, F.; Gajofatto, F.; Santilli, V.; Smania, N. Botulinum Toxin Type A Injection Into the Gastrocnemius Muscle for Spastic Equinus in Adults with Stroke: A Randomized Controlled Trial Comparing Manual Needle Placement, Electrical Stimulation and Ultrasonography-Guided Injection Techniques. Am. J. Phys. Med. Rehabil. 2012, 91, 957–964. [Google Scholar] [CrossRef] [PubMed]
- Park, G.-Y.; Kwon, D.R. Sonoelastographic Evaluation of Medial Gastrocnemius Muscles Intrinsic Stiffness After Rehabilitation Therapy With Botulinum Toxin A Injection in Spastic Cerebral Palsy. Arch. Phys. Med. Rehabil. 2012, 93, 2085–2089. [Google Scholar] [CrossRef]
- Kawano, A.; Yanagizono, T.; Kadouchi, I.; Umezaki, T.; Chosa, E. Ultrasonographic Evaluation of Changes in the Muscle Architecture of the Gastrocnemius with Botulinum Toxin Treatment for Lower Extremity Spasticity in Children with Cerebral Palsy. J. Orthop. Sci. 2018, 23, 389–393. [Google Scholar] [CrossRef]
- Van Campenhout, A.; Molenaers, G. Localization of the Motor Endplate Zone in Human Skeletal Muscles of the Lower Limb: Anatomical Guidelines for Injection with Botulinum Toxin: Review. Dev. Med. Child Neurol. 2011, 53, 108–119. [Google Scholar] [CrossRef]
- Heo, Y.; Lee, H.; Hwang, S.-J. Bicipital Origin and the Course of the Plantaris Muscle. Anat. Cell Biol. 2021, 54, 289–291. [Google Scholar] [CrossRef]
- Cunnane, B.T.; Sinha, U.; Malis, V.; Hernandez, R.D.; Smitaman, E.; Sinha, S. Effect of Different Ankle Joint Positions on Medial Gastrocnemius Muscle Fiber Strains during Isometric Plantarflexion. Sci. Rep. 2023, 13, 14986. [Google Scholar] [CrossRef]
- Suzuki, T.; Chino, K.; Fukashiro, S. Gastrocnemius and Soleus Are Selectively Activated When Adding Knee Extensor Activity to Plantar Flexion. Hum. Mov. Sci. 2014, 36, 35–45. [Google Scholar] [CrossRef]
- Kovács, B.; Csala, D.; Yang, S.; Tihanyi, J.; Gu, Y.; Hortobágyi, T. Knee Position Affects Medial Gastrocnemius and Soleus Activation during Dynamic Plantarflexion: No Evidence for an Inter-Muscle Compensation in Healthy Young Adults. Biol. Open 2024, 13, BIO061810. [Google Scholar] [CrossRef]
- Picelli, A.; Filippetti, M.; Melotti, C.; Guerrazzi, F.; Modenese, A.; Smania, N. Does Botulinum Toxin Treatment Affect the Ultrasonographic Characteristics of Post-Stroke Spastic Equinus? A Retrospective Pilot Study. Toxins 2020, 12, 797. [Google Scholar] [CrossRef] [PubMed]
- Hefter, H.; Nickels, W.; Samadzadeh, S.; Rosenthal, D. Comparing Soleus Injections and Gastrocnemius Injections of Botulinum Toxin for Treating Adult Spastic Foot Drop: A Monocentric Observational Study. J. Int. Med. Res. 2021, 49. [Google Scholar] [CrossRef] [PubMed]
- Aymard, C.; Giboin, L.-S.; Lackmy-Vallée, A.; Marchand-Pauvert, V. Spinal Plasticity in Stroke Patients after Botulinum Neurotoxin A Injection in Ankle Plantar Flexors. Physiol. Rep. 2013, 1, e00173. [Google Scholar] [CrossRef]
- Hesse, S.; Krajnik, J.; Luecke, D.; Jahnke, M.T.; Gregoric, M.; Mauritz, K.H. Ankle Muscle Activity Before and After Botulinum Toxin Therapy for Lower Limb Extensor Spasticity in Chronic Hemiparetic Patients. Stroke 1996, 27, 455–460. [Google Scholar] [CrossRef]
- Boyaci, A.; Tutoglu, A.; Boyaci, N.; Koca, I.; Calik, M.; Sakalar, A.; Kilicaslan, N. Changes in Spastic Muscle Stiffness after Botulinum Toxin A Injections as Part of Rehabilitation Therapy in Patients with Spastic Cerebral Palsy. Neurorehabilit. Int. Interdiscip. J. 2014, 35, 123–129. [Google Scholar] [CrossRef]
- Li, S. Ankle and Foot Spasticity Patterns in Chronic Stroke Survivors with Abnormal Gait. Toxins 2020, 12, 646. [Google Scholar] [CrossRef]
- Spina, S.; Facciorusso, S.; Botticelli, C.; Intiso, D.; Ranieri, M.; Colamaria, A.; Fiore, P.; Ciritella, C.; Genêt, F.; Santamato, A. Ultrasonographic Evaluation of Three Approaches for Botulinum Toxin Injection into Tibialis Posterior Muscle in Chronic Stroke Patients with Equinovarus Foot: An Observational Study. Toxins 2021, 13, 829. [Google Scholar] [CrossRef]
- Yi, K.; Rha, D.; Lee, S.C.; Cong, L.; Lee, H.; Lee, Y.; Kim, H.; Hu, K. Intramuscular Nerve Distribution Pattern of Ankle Invertor Muscles in Human Cadaver Using Sihler Stain. Muscle Nerve 2016, 53, 742–747. [Google Scholar] [CrossRef]
- Lee, J.; Lee, B.; An, X.; Chung, R.; Han, S. Location of the Motor Entry Point and Intramuscular Motor Point of the Tibialis Posterior Muscle: For Effective Motor Point Block. Clin. Anat. 2011, 24, 91–96. [Google Scholar] [CrossRef]
- Palastanga, N.; Soames, R. Anatomy and Human Movement Structure and Function, 7th ed.; Elsevier: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Takekawa, T.; Kobayashi, K.; Yamada, N.; Takagi, S.; Hara, T.; Kitajima, T.; Sato, T.; Sugihara, H.; Kinoshita, K.; Abo, M. Effects of Flexor Digitorum Longus Muscle Anatomical Structure on the Response to Botulinum Toxin Treatment in Patients with Post-Stroke Claw Foot Deformity. Toxins 2022, 14, 666. [Google Scholar] [CrossRef]
- Suputtitada, A. Local Botulinum Toxin Type A Injections in the Treatment of Spastic Toes. Am. J. Phys. Med. Rehabil. 2002, 81, 770–775. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.G.; Chung, M.E.; Song, D.H.; Kim, J.Y.; Sul, B.M.; Oh, C.H.; Park, N.S. Determination of Injection Site in Flexor Digitorum Longus for Effective and Safe Botulinum Toxin Injection. Ann. Rehabil. Med. 2015, 39, 32. [Google Scholar] [CrossRef] [PubMed]
- Yi, K.-H.; Cong, L.; Bae, J.-H.; Park, E.-S.; Rha, D.; Kim, H.-J. Neuromuscular Structure of the Tibialis Anterior Muscle for Functional Electrical Stimulation. Surg. Radiol. Anat. 2017, 39, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Chummy, S.S. Last’s Anatomy: Regional and Applied, 12th ed.; Churchill Livingstone: Amsterdam, The Netherlands, 2011; ISBN 978-0-7020-3394-0. [Google Scholar]
- Ambesh, P.; Paliwal, V.K.; Shetty, V.; Kamholz, S. The Babinski Sign: A Comprehensive Review. J. Neurol. Sci. 2017, 372, 477–481. [Google Scholar] [CrossRef]
- Gaber, T.A.-Z.K.; Basu, B.; Shakespeare, D.; Singh, R.; Salam, S.; McFarlane, J. Botulinum Toxin in the Management of Hitchhiker’s Toe. Neurorehabilit. Int. Interdiscip. J. 2011, 28, 395–399. [Google Scholar] [CrossRef]
- Lee, J.; Han, S.; Ye, J.; Lee, B.; An, X.; Kwon, S. Effective Zone of Botulinum Toxin a Injections in Hallux Claw Toe Syndrome: An Anatomical Study. Muscle Nerve 2012, 45, 217–221. [Google Scholar] [CrossRef]
- Wu, K.P.-H.; Chen, C.-K.; Lin, S.-C.; Pei, Y.-C.; Lin, R.-H.; Tsai, W.-C.; Fuk-Tan Tang, S. Botulinum Toxin Type A Injections for Patients with Painful Hallux Valgus: A Double-Blind, Randomized Controlled Study. Clin. Neurol. Neurosurg. 2015, 129, S58–S62. [Google Scholar] [CrossRef]
- Cheong, I.Y.; Kim, D.K.; Oh, Y.J.; Park, B.K.; Kim, K.H.; Kim, D.H. Optimal Needle Placement for Extensor Hallucis Longus Muscle: A Cadaveric Study. Ann. Rehabil. Med. 2016, 40, 457. [Google Scholar] [CrossRef]
- Meiser, V.C.; Kreysa, H.; Guntinas-Lichius, O.; Volk, G.F. Comparison of In-Plane and out-of-Plane Needle Insertion with vs. without Needle Guidance. Eur. Arch. Otorhinolaryngol. 2016, 273, 2697–2705. [Google Scholar] [CrossRef]
- Wang, Y.; Meng, F.; Zhang, Y.; Xu, M.; Yue, S. Full-Movement Neuromuscular Electrical Stimulation Improves Plantar Flexor Spasticity and Ankle Active Dorsiflexion in Stroke Patients: A Randomized Controlled Study. Clin. Rehabil. 2016, 30, 577–586. [Google Scholar] [CrossRef]
- Allart, E.; Rogeau, C.; Grauwin, M.-Y.; Nachef, N.; Lannes, X.; Rousseaux, M.; Thevenon, A.; Fontaine, C. Treatment of Dystonia in Extensor Hallucis Longus and Digitorum Muscles with Neurotomy of the Branches of the Deep Fibular Nerve: Preliminary Results. Orthop. Traumatol. Surg. Res. 2015, 101, 341–344. [Google Scholar] [CrossRef]
- Rucco, V.; Lorenzini, L.; Pellegrini, E. Clawed Toes Deformity Due to Spasticity of the Extensor Digitorum Muscle. A Case Report. Eura Medicophys. 2004, 40, 269–272. [Google Scholar]







| Muscle | Key Anatomical Landmarks | Nearby Structures at Risk | Ultrasound Technique Tip | Injection Precautions |
|---|---|---|---|---|
| Lateral Head of Gastrocnemius | ~8 cm distal to the popliteal crease, on the lateral side | Medial sural cutaneous nerve (superficial), soleus and plantaris muscle/tendon if present (deep) | Transverse scan on the posterior aspect of the leg | Avoid medial sural cutaneous nerve injury |
| Medial Head of Gastrocnemius | ~8 cm distal to the popliteal crease, on the medial side | Medial sural cutaneous nerve (superficial), soleus and plantaris muscle/tendon if present (deep) | Transverse scan on the posterior aspect of the leg | Avoid medial sural cutaneous nerve injury |
| Soleus | ~8 cm distal to the popliteal crease on the midline | Gastrocnemius (superficial) and plantaris muscle/tendon (if present); posterior tibial artery, tibial veins, and the posterior tibial nerve (deep) | Transverse scan on the posterior aspect of the leg | Avoid neurovascular injury |
| Tibialis Posterior (anterior window) | ~10 cm distal to the knee joint, in the lateral portion | Interosseous membrane, deep fibular nerve, anterior tibial artery, and anterior tibial vein (superficial); tibialis anterior (superficial and medial), extensor digitorum longus (superficial and lateral); | Transverse scan on the anterior aspect of the leg | Avoid neurovascular injury |
| Tibialis Posterior (medial window) | Distal third of the leg, in the medial portion | Flexor digitorum longus (superficial and medial), flexor hallucis longus (superficial and lateral); tibial nerve, posterior tibial artery, and posterior tibial vein (superficial); interosseous membrane (deep) | Transverse scan on the distal third of the leg | Avoid neurovascular injury |
| Tibialis Posterior (posterior window) | Distal third of the posterior leg | Flexor digitorum longus, tibial nerve, posterior tibial artery and posterior tibial vein (superficial and medial); flexor hallucis longus, fibular artery and vein (superficial and lateral); interosseous membrane (deep) | Transverse scan on the distal third of the leg | Avoid neurovascular injury |
| Flexor Hallucis Longus | Distal third of the posterior leg, in the lateral portion | Soleus (superficial); tibialis posterior, flexor digitorum longus (deep and medial); Interosseous membrane (deep) | Transverse scan on the distal third of the posterior leg | Confirm muscle position and relations |
| Flexor Digitorum Longus | Distal third of the posterior leg in the medial portion | Soleus (superficial); flexor hallucis longus, tibial nerve, posterior tibial artery, and posterior tibial veins (lateral); tibialis posterior, interosseous membrane (deep and lateral); | Transverse scan distal third of the posterior leg | Avoid neurovascular injury |
| Tibialis anterior | Proximal third of the anterior aspect of the leg, in the lateral portion | Extensor digitorum longus (lateral); Interosseous membrane, tibialis posterior (deep) | Transverse scan on proximal third of the anterior aspect of the leg | Confirm muscle position and relations |
| Extensor Hallucis Longus | Distal third of the anterior aspect of the leg, in lateral portion | Tendinous portion of the tibialis anterior (superficial and lateral), extensor digitorum longus (lateral); interosseous membrane and tibialis posterior (deep) | Transverse scan on distal third of the anterior aspect of the leg | Confirm muscle position and relations |
| Flexor Digitorum Brevis | Mid-plantar aspect of the foot | Plantar aponeurosis (superficial); abductor hallucis (medial); quadratus plantae (deep) | Transverse scan at mid-plantar aspect of the foot | Visualize flexor digitorum brevis as most superficial muscle and confirm muscle position and relations |
| Flexor Hallucis Brevis | ~1–2 cm proximal to the first metatarsophalangeal joint | Abductor hallucis muscle and tendon (medial); flexor hallucis longus tendon (lateral); adductor hallucis (deep and medial) | Transverse scan ~1–2 cm proximal to the first metatarsophalangeal joint | Visualize flexor hallucis brevis as most superficial muscle and confirm muscle position and relations |
| Extensor Digitorum Longus | Proximal third of the anterior aspect of the leg, in the lateral portion | Tibialis anterior (medial); Fibularis longus (lateral); superficial fibular nerve, anterior tibial artery, deep fibular nerve (deep) | Transverse scan on proximal third of the anterior aspect of the leg | Visualize extensor digitorum longus as most superficial muscle and confirm muscle position and relations |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Popescu, M.N.; Căpeț, C.; Popescu, C.; Berteanu, M. The Elias University Hospital Approach: A Visual Guide to Ultrasound-Guided Botulinum Toxin Injection in Spasticity, Part IV—Distal Lower Limb Muscles. Toxins 2025, 17, 508. https://doi.org/10.3390/toxins17100508
Popescu MN, Căpeț C, Popescu C, Berteanu M. The Elias University Hospital Approach: A Visual Guide to Ultrasound-Guided Botulinum Toxin Injection in Spasticity, Part IV—Distal Lower Limb Muscles. Toxins. 2025; 17(10):508. https://doi.org/10.3390/toxins17100508
Chicago/Turabian StylePopescu, Marius Nicolae, Claudiu Căpeț, Cristina Popescu, and Mihai Berteanu. 2025. "The Elias University Hospital Approach: A Visual Guide to Ultrasound-Guided Botulinum Toxin Injection in Spasticity, Part IV—Distal Lower Limb Muscles" Toxins 17, no. 10: 508. https://doi.org/10.3390/toxins17100508
APA StylePopescu, M. N., Căpeț, C., Popescu, C., & Berteanu, M. (2025). The Elias University Hospital Approach: A Visual Guide to Ultrasound-Guided Botulinum Toxin Injection in Spasticity, Part IV—Distal Lower Limb Muscles. Toxins, 17(10), 508. https://doi.org/10.3390/toxins17100508







