Quantitative and Qualitative Pain Evaluation in Response to OnabotulinumtoxinA for Chronic Migraine: An Observational Real-Life Study
Abstract
1. Introduction
2. Results
3. Discussion
4. Conclusions
5. Materials and Methods
5.1. Data Collection
5.2. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Steiner, T.J.; Stovner, L.J.; Jensen, R.; Uluduz, D.; Katsarava, Z. Migraine Remains Second among the World’s Causes of Disability, and First among Young Women: Findings from GBD2019. J. Headache Pain 2020, 21, 137. [Google Scholar] [CrossRef] [PubMed]
- Eigenbrodt, A.K.; Ashina, H.; Khan, S.; Diener, H.-C.; Mitsikostas, D.D.; Sinclair, A.J.; Pozo-Rosich, P.; Martelletti, P.; Ducros, A.; Lantéri-Minet, M.; et al. Diagnosis and Management of Migraine in Ten Steps. Nat. Rev. Neurol. 2021, 17, 501–514. [Google Scholar] [CrossRef] [PubMed]
- Straube, A.; Andreou, A. Primary Headaches during Lifespan. J. Headache Pain 2019, 20, 35. [Google Scholar] [CrossRef] [PubMed]
- Andreou, A.P.; Edvinsson, L. Mechanisms of Migraine as a Chronic Evolutive Condition. J. Headache Pain 2019, 20, 117. [Google Scholar] [CrossRef]
- May, A.; Schulte, L.H. Chronic Migraine: Risk Factors, Mechanisms and Treatment. Nat. Rev. Neurol. 2016, 12, 455–464. [Google Scholar] [CrossRef]
- Schwedt, T.J.; Hentz, J.G.; Sahai-Srivastava, S.; Spare, N.M.; Martin, V.T.; Treppendahl, C.; Digre, K.; Bennett, N.L.; Birlea, M.; Watson, D.; et al. Headache Characteristics and Burden from Chronic Migraine with Medication Overuse Headache: Cross-sectional Observations from the Medication Overuse Treatment Strategy Trial. Headache J. Head Face Pain 2021, 61, 351–362. [Google Scholar] [CrossRef]
- Serrano, D.; Lipton, R.B.; Scher, A.I.; Reed, M.L.; Stewart, W.F.; Adams, A.M.; Buse, D.C. Fluctuations in Episodic and Chronic Migraine Status over the Course of 1 Year: Implications for Diagnosis, Treatment and Clinical Trial Design. J. Headache Pain 2017, 18, 101. [Google Scholar] [CrossRef]
- Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd Edition. Cephalalgia 2018, 38, 1–211. [CrossRef]
- Buse, D.C.; Manack, A.N.; Fanning, K.M.; Serrano, D.; Reed, M.L.; Turkel, C.C.; Lipton, R.B. Chronic Migraine Prevalence, Disability, and Sociodemographic Factors: Results from the American Migraine Prevalence and Prevention Study. Headache 2012, 52, 1456–1470. [Google Scholar] [CrossRef]
- Altamura, C.; Corbelli, I.; de Tommaso, M.; Di Lorenzo, C.; Di Lorenzo, G.; Di Renzo, A.; Filippi, M.; Jannini, T.B.; Messina, R.; Parisi, P.; et al. Pathophysiological Bases of Comorbidity in Migraine. Front. Hum. Neurosci. 2021, 15, 640574. [Google Scholar] [CrossRef]
- Do, T.P.; Hougaard, A.; Dussor, G.; Brennan, K.C.; Amin, F.M. Migraine Attacks Are of Peripheral Origin: The Debate Goes On. J. Headache Pain 2023, 24, 3. [Google Scholar] [CrossRef]
- Coppola, G.; Parisi, V.; Di Renzo, A.; Pierelli, F. Cortical Pain Processing in Migraine. J. Neural Transm. 2020, 127, 551–566. [Google Scholar] [CrossRef]
- Suzuki, K.; Suzuki, S.; Shiina, T.; Kobayashi, S.; Hirata, K. Central Sensitization in Migraine: A Narrative Review. J. Pain Res. 2022, 15, 2673–2682. [Google Scholar] [CrossRef]
- Mínguez-Olaondo, A.; Quintas, S.; Morollón Sánchez-Mateos, N.; López-Bravo, A.; Vila-Pueyo, M.; Grozeva, V.; Belvís, R.; Santos-Lasaosa, S.; Irimia, P. Cutaneous Allodynia in Migraine: A Narrative Review. Front. Neurol. 2021, 12, 831035. [Google Scholar] [CrossRef]
- Della Pietra, A.; Mikhailov, N.; Giniatullin, R. The Emerging Role of Mechanosensitive Piezo Channels in Migraine Pain. Int. J. Mol. Sci. 2020, 21, 696. [Google Scholar] [CrossRef]
- Vernieri, F.; Paolucci, M.; Altamura, C.; Pasqualetti, P.; Mastrangelo, V.; Pierangeli, G.; Cevoli, S.; D’Amico, D.; Grazzi, L. Onabotulinumtoxin-A in Chronic Migraine: Should Timing and Definition of Non-Responder Status Be Revised? Suggestions From a Real-Life Italian Multicenter Experience. Headache 2019, 59, 1300–1309. [Google Scholar] [CrossRef]
- Dodick, D.W.; Turkel, C.C.; Degryse, R.E.; Aurora, S.K.; Silberstein, S.D.; Lipton, R.B.; Diener, H.C.; Brin, M.F. OnabotulinumtoxinA for Treatment of Chronic Migraine: Pooled Results from the Double-Blind, Randomized, Placebo-Controlled Phases of the PREEMPT Clinical Program. Headache 2010, 50, 921–936. [Google Scholar] [CrossRef]
- Altamura, C.; Ornello, R.; Ahmed, F.; Negro, A.; Miscio, A.M.; Santoro, A.; Alpuente, A.; Russo, A.; Silvestro, M.; Cevoli, S.; et al. OnabotulinumtoxinA in Elderly Patients with Chronic Migraine: Insights from a Real-Life European Multicenter Study. J. Neurol. 2022, 270, 986–994. [Google Scholar] [CrossRef]
- Viticchi, G.; Falsetti, L.; Salvemini, S.; Bartolini, M.; Paolucci, S.; Buratti, L.; Silvestrini, M. Efficacy of Onabotulinum Toxin A on Obsessive-Compulsive Traits in a Population of Chronic Migraine Patients. Brain Sci. 2022, 12, 1563. [Google Scholar] [CrossRef]
- Corbelli, I.; Verzina, A.; Leone De Magistris, I.; De Vanna, G.; Eusebi, P.; Mataluni, G.; Pisani, A.; Prudenzano, A.M.P.; Trojano, M.; Delussi, M.; et al. Sustained Efficacy, Safety and High Adherence Rate of Onabotulinum Toxin Type A in Chronic Migraine Patients: A Multicentric Prospective Real-Life Study. Toxins 2022, 15, 34. [Google Scholar] [CrossRef]
- Burstein, R.; Blumenfeld, A.M.; Silberstein, S.D.; Manack Adams, A.; Brin, M.F. Mechanism of Action of OnabotulinumtoxinA in Chronic Migraine: A Narrative Review. Headache 2020, 60, 1259–1272. [Google Scholar] [CrossRef] [PubMed]
- Baraldi, C.; Lo Castro, F.; Ornello, R.; Sacco, S.; Pani, L.; Guerzoni, S. OnabotulinumtoxinA: Still the Present for Chronic Migraine. Toxins 2023, 15, 59. [Google Scholar] [CrossRef] [PubMed]
- Sebastianelli, G.; Casillo, F.; Di Renzo, A.; Abagnale, C.; Cioffi, E.; Parisi, V.; Di Lorenzo, C.; Serrao, M.; Pierelli, F.; Schoenen, J.; et al. Effects of Botulinum Toxin Type A on the Nociceptive and Lemniscal Somatosensory Systems in Chronic Migraine: An Electrophysiological Study. Toxins 2023, 15, 76. [Google Scholar] [CrossRef] [PubMed]
- Mathew, N.T.; Kailasam, J.; Meadors, L. Predictors of Response to Botulinum Toxin Type A (BoNTA) in Chronic Daily Headache. Headache 2008, 48, 194–200. [Google Scholar] [CrossRef]
- Torres-Ferrus, M.; Gallardo, V.J.; Alpuente, A.; Pozo-Rosich, P. Influence of Headache Pain Intensity and Frequency on Migraine-Related Disability in Chronic Migraine Patients Treated with OnabotulinumtoxinA. J. Headache Pain 2020, 21, 88. [Google Scholar] [CrossRef]
- DosSantos, M.F.; de Souza Moura, B.; DaSilva, A.F. Reward Circuitry Plasticity in Pain Perception and Modulation. Front. Pharmacol. 2017, 8, 790. [Google Scholar] [CrossRef]
- Rogers, D.G.; Protti, T.A.; Smitherman, T.A. Fear, Avoidance, and Disability in Headache Disorders. Curr. Pain Headache Rep. 2020, 24, 33. [Google Scholar] [CrossRef]
- Aurora, S.K.; Dodick, D.W.; Turkel, C.C.; Degryse, R.E.; Silberstein, S.D.; Lipton, R.B.; Diener, H.C.; Brin, M.F. OnabotulinumtoxinA for Treatment of Chronic Migraine: Results from the Double-Blind, Randomized, Placebo-Controlled Phase of the PREEMPT 1 Trial. Cephalalgia 2010, 30, 793–803. [Google Scholar] [CrossRef]
- Giri, S.; Tronvik, E.; Linde, M.; Pedersen, S.A.; Hagen, K. Randomized Controlled Studies Evaluating Topiramate, Botulinum Toxin Type A, and MABs Targeting CGRP in Patients with Chronic Migraine and Medication Overuse Headache: A Systematic Review and Meta-Analysis. Cephalalgia 2023, 43, 03331024231156922. [Google Scholar] [CrossRef]
- Frank, F.; Ulmer, H.; Sidoroff, V.; Broessner, G. CGRP-Antibodies, Topiramate and Botulinum Toxin Type A in Episodic and Chronic Migraine: A Systematic Review and Meta-Analysis. Cephalalgia 2021, 41, 1222–1239. [Google Scholar] [CrossRef]
- Winner, P.K.; Blumenfeld, A.M.; Eross, E.J.; Orejudos, A.C.; Mirjah, D.L.; Adams, A.M.; Brin, M.F. Long-Term Safety and Tolerability of OnabotulinumtoxinA Treatment in Patients with Chronic Migraine: Results of the COMPEL Study. Drug Saf. 2019, 42, 1013–1024. [Google Scholar] [CrossRef]
- Ornello, R.; Ahmed, F.; Negro, A.; Miscio, A.M.; Santoro, A.; Alpuente, A.; Russo, A.; Silvestro, M.; Cevoli, S.; Brunelli, N.; et al. Early Management of OnabotulinumtoxinA Treatment in Chronic Migraine: Insights from a Real-Life European Multicenter Study. Pain Ther. 2021, 10, 637–650. [Google Scholar] [CrossRef]
- Ahmed, F.; Gaul, C.; Garciá-Moncó, J.C.; Sommer, K.; Martelletti, P. An Open-Label Prospective Study of the Real-Life Use of OnabotulinumtoxinA for the Treatment of Chronic Migraine: The REPOSE Study. J. Headache Pain 2019, 20, 26. [Google Scholar] [CrossRef]
- Lanteri-Minet, M.; Ducros, A.; Francois, C.; Olewinska, E.; Nikodem, M.; Dupont-Benjamin, L. Effectiveness of OnabotulinumtoxinA (BOTOX®) for the Preventive Treatment of Chronic Migraine: A Meta-Analysis on 10 Years of Real-World Data. Cephalalgia 2022, 42, 1543–1564. [Google Scholar] [CrossRef]
- Altamura, C.; Cevoli, S.; Brunelli, N.; Aurilia, C.; Fofi, L.; Egeo, G.; Barbanti, P.; Vernieri, F. When Should We Consider Chronic Patients as Non-Responders to Monoclonal Antibodies Targeting the CGRP Pathway? J. Neurol. 2022, 269, 1032–1034. [Google Scholar] [CrossRef]
- Edvinsson, L.; Haanes, K.A.; Warfvinge, K.; Krause, D.N. CGRP as the Target of New Migraine Therapies—Successful Translation from Bench to Clinic. Nat. Rev. Neurol. 2018, 14, 338–350. [Google Scholar] [CrossRef]
- Barbanti, P.; Egeo, G.; Aurilia, C.; Albanese, M.; Cetta, I.; Di Fiore, P.; Zucco, M.; FilippiBonassi, M.; Bono, F.; Altamura, C.; et al. Fremanezumab in the Prevention of High-Frequency Episodic and Chronic Migraine: A 12-Week, Multicenter, Real-Life, Cohort Study (the FRIEND Study). J. Headache Pain 2022, 23, 46. [Google Scholar] [CrossRef]
- Barbanti, P.; Aurilia, C.; Cevoli, S.; Egeo, G.; Fofi, L.; Messina, R.; Salerno, A.; Torelli, P.; Albanese, M.; Carnevale, A.; et al. Long-term (48 Weeks) Effectiveness, Safety, and Tolerability of Erenumab in the Prevention of High-frequency Episodic and Chronic Migraine in a Real World: Results of the EARLY 2 Study. Headache J. Head Face Pain 2021, 61, 1351–1363. [Google Scholar] [CrossRef]
- Vernieri, F.; Brunelli, N.; Marcosano, M.; Aurilia, C.; Egeo, G.; Lovati, C.; Favoni, V.; Perrotta, A.; Maestrini, I.; Rao, R.; et al. Maintenance of Response and Predictive Factors of 1-year <scp>GalcanezumAb</Scp> Treatment in Real-life Migraine Patients in Italy: The Multicenter Prospective Cohort GARLIT Study. Eur. J. Neurol. 2023, 30, 224–234. [Google Scholar] [CrossRef]
- Schoenen, J.; Manise, M.; Nonis, R.; Gérard, P.; Timmermans, G. Monoclonal Antibodies Blocking CGRP Transmission: An Update on Their Added Value in Migraine Prevention. Rev. Neurol. 2020, 176, 788–803. [Google Scholar] [CrossRef]
- Blumenfeld, A.M.; Frishberg, B.M.; Schim, J.D.; Iannone, A.; Schneider, G.; Yedigarova, L.; Manack Adams, A. Real-World Evidence for Control of Chronic Migraine Patients Receiving CGRP Monoclonal Antibody Therapy Added to OnabotulinumtoxinA: A Retrospective Chart Review. Pain Ther. 2021, 10, 809–826. [Google Scholar] [CrossRef] [PubMed]
- Argyriou, A.A.; Dermitzakis, E.V.; Xiromerisiou, G.; Vikelis, M. OnabotulinumtoxinA Add-On to Monoclonal Anti-CGRP Antibodies in Treatment-Refractory Chronic Migraine. Toxins 2022, 14, 847. [Google Scholar] [CrossRef] [PubMed]
- Silvestro, M.; Tessitore, A.; Scotto di Clemente, F.; Battista, G.; Tedeschi, G.; Russo, A. Additive Interaction Between Onabotulinumtoxin-A and Erenumab in Patients With Refractory Migraine. Front. Neurol. 2021, 12, 656294. [Google Scholar] [CrossRef] [PubMed]
- Pellesi, L.; Do, T.P.; Ashina, H.; Ashina, M.; Burstein, R. Review Articles Dual Therapy With Anti-CGRP Monoclonal Antibodies and Botulinum Toxin for Migraine Prevention: Is There a Rationale? Headache. Headache 2020, 60, 1056–1065. [Google Scholar] [CrossRef]
- Shimizu, T.; Suzuki, N. Biological Sciences Related to Headache. Handb. Clin. Neurol. 2010, 97, 35–45. [Google Scholar] [CrossRef]
- Zhang, C.; Kaye, J.A.; Cai, Z.; Wang, Y.; Prescott, S.L.; Liberles, S.D. Area Postrema Cell Types That Mediate Nausea-Associated Behaviors. Neuron 2021, 109, 461–472.e5. [Google Scholar] [CrossRef]
- Jakubowski, M.; McAllister, P.J.; Bajwa, Z.H.; Ward, T.N.; Smith, P.; Burstein, R. Exploding vs. Imploding Headache in Migraine Prophylaxis with Botulinum Toxin A. Pain 2006, 125, 286–295. [Google Scholar] [CrossRef]
- Alpuente, A.; Gallardo, V.J.; Torres-Ferrús, M.; Álvarez-Sabin, J.; Pozo-Rosich, P. Short and Mid-Term Predictors of Response to OnabotulinumtoxinA: Real-Life Experience Observational Study. Headache 2020, 60, 677–685. [Google Scholar] [CrossRef]
- Alpuente, A.; Gallardo, V.J.; Torres-Ferrús, M.; Santos-Lasaosa, S.; Guerrero, A.L.; Laínez, J.M.; Viguera, J.; Gago-Veiga, A.; Irimia, P.; Sánchez del Rio, M.; et al. Evaluation of the Concomitant Use of Oral Preventive Treatments and OnabotulinumtoxinA in Chronic Migraine: The PREVENBOX Study. Eur. J. Neurol. 2020, 27, 2102–2108. [Google Scholar] [CrossRef]
- De Tommaso, M.; Brighina, F.; Delussi, M. Effects of Botulinum Toxin A on Allodynia in Chronic Migraine: An Observational Open-Label Two-Year Study. Eur. Neurol. 2019, 81, 37–46. [Google Scholar] [CrossRef]
- Bond, D.S.; Buse, D.C.; Lipton, R.B.; Thomas, J.G.; Rathier, L.; Roth, J.; Pavlovic, J.M.; Evans, E.W.; Wing, R.R. Clinical Pain Catastrophizing in Women With Migraine and Obesity. Headache 2015, 55, 923–933. [Google Scholar] [CrossRef]
- Migliore, S.; Paolucci, M.; Quintiliani, L.; Altamura, C.; Maffi, S.; D’Aurizio, G.; Curcio, G.; Vernieri, F. Psychopathological Comorbidities and Clinical Variables in Patients With Medication Overuse Headache. Front. Hum. Neurosci. 2020, 14, 571035. [Google Scholar] [CrossRef]
- Baliki, M.N.; Apkarian, A.V. Nociception, Pain, Negative Moods, and Behavior Selection. Neuron 2015, 87, 474–491. [Google Scholar] [CrossRef]
- Grazzi, L.; Andrasik, F.; Rizzoli, P.; Bernstein, C.; Sansone, E.; Raggi, A. Acceptance and Commitment Therapy for High Frequency Episodic Migraine without Aura: Findings from a Randomized Pilot Investigation. Headache 2021, 61, 895–905. [Google Scholar] [CrossRef]
- Grazzi, L.; Montisano, D.A.; Rizzoli, P.; Guastafierro, E.; Marcassoli, A.; Fornari, A.; Raggi, A. A Single-Group Study on the Effect of OnabotulinumtoxinA in Patients with Chronic Migraine Associated with Medication Overuse Headache: Pain Catastrophizing Plays a Role. Toxins 2023, 15, 86. [Google Scholar] [CrossRef]
- Silvestro, M.; Tessitore, A.; Orologio, I.; De Micco, R.; Tartaglione, L.; Trojsi, F.; Tedeschi, G.; Russo, A. Galcanezumab Effect on “Whole Pain Burden” and Multidimensional Outcomes in Migraine Patients with Previous Unsuccessful Treatments: A Real-World Experience. J. Headache Pain 2022, 23, 69. [Google Scholar] [CrossRef]
- Blumenfeld, A.; Silberstein, S.D.; Dodick, D.W.; Aurora, S.K.; Turkel, C.C.; Binder, W.J. Method of Injection of OnabotulinumtoxinA for Chronic Migraine: A Safe, Well-Tolerated, and Effective Treatment Paradigm Based on the PREEMPT Clinical Program. Headache 2010, 50, 1406–1418. [Google Scholar] [CrossRef]
- Diener, H.C.; Dodick, D.W.; Aurora, S.K.; Turkel, C.C.; Degryse, R.E.; Lipton, R.B.; Silberstein, S.D.; Brin, M.F. OnabotulinumtoxinA for Treatment of Chronic Migraine: Results from the Double-Blind, Randomized, Placebo-Co.Ntrolled Phase of the PREEMPT 2 Trial. Cephalalgia 2010, 30, 804–814. [Google Scholar] [CrossRef] [PubMed]
- Houts, C.R.; Wirth, R.J.; McGinley, J.S.; Gwaltney, C.; Kassel, E.; Snapinn, S.; Cady, R. Content Validity of HIT-6 as a Measure of Headache Impact in People With Migraine: A Narrative Review. Headache 2020, 60, 28–39. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, D.; Mosconi, P.; Genco, S.; Usai, S.; Prudenzano, A.M.; Grazzi, L.; Leone, M.; Puca, F.M.; Bussone, G. The Migraine Disability Assessment (MIDAS) Questionnaire: Translation and Reliability of the Italian Version. Cephalalgia 2001, 21, 947–952. [Google Scholar] [CrossRef] [PubMed]
- Afshinmajd, S.; Davati, A.; Akbari, F. The Effects of Body Mass Index on the Treatment of the Patients with Migraine Headaches. Iran J. Neurol. 2011, 10, 35–38. [Google Scholar]
- Melzack, R. The Short-Form McGill Pain Questionnaire. Pain 1987, 30, 191–197. [Google Scholar] [CrossRef]
- Strand, L.I.; Ljunggren, A.E.; Bogen, B.; Ask, T.; Johnsen, T.B. The Short-Form McGill Pain Questionnaire as an Outcome Measure: Test-Retest Reliability and Responsiveness to Change. Eur. J. Pain 2008, 12, 917–925. [Google Scholar] [CrossRef]
- Ruan, X.; Padnos, I.W.; Kaye, A.D. Validation of a New “Objective Pain Score” vs. “Numeric Rating Scale” For the Evaluation of Acute Pain: A Comparative Study. Anesth Pain Med. 2016, 6, e32101. [Google Scholar] [CrossRef]
- García-Azorín, D.; Martínez, B.; Gutiérrez, M.; Ruiz-Piñero, M.; Echavarría, A.; Sierra, Á.; Guerrero, Á.L. Real-World Evaluation of the Tolerability to Onabotulinum Toxin A: The RETO Study. Toxins 2022, 14, 850. [Google Scholar] [CrossRef]
- Nozawa, K.; Matsuyama, S.; Higa, S.; Yamamoto, Y.; Asami, Y. Physician Consultation Rates and Characteristics among Workers with Chronic Pain or Headache Who Participated in a Behavioural Change Program: A Retrospective Database Analysis Using Real-World Healthcare Data. BMJ Open 2022, 12, e056846. [Google Scholar] [CrossRef]
- Mattoo, B.; Tanwar, S.; Bhatia, R.; Tripathi, M.; Bhatia, R. Repetitive Transcranial Magnetic Stimulation in Chronic Tension-Type Headache: A Pilot Study. Indian J. Med. Res. 2019, 150, 73–80. [Google Scholar] [CrossRef]
- Silberstein, S.; Tfelt-Hanfsen, P.; Dodick, D.W.; Limmroth, V.; Lipton, R.B.; Pascual, J.; Wang, S.J. Guidelines for Controlled Trials of Prophylactic Treatment of Chronic Migraine in Adults. Cephalalgia 2008, 28, 484–495. [Google Scholar] [CrossRef]
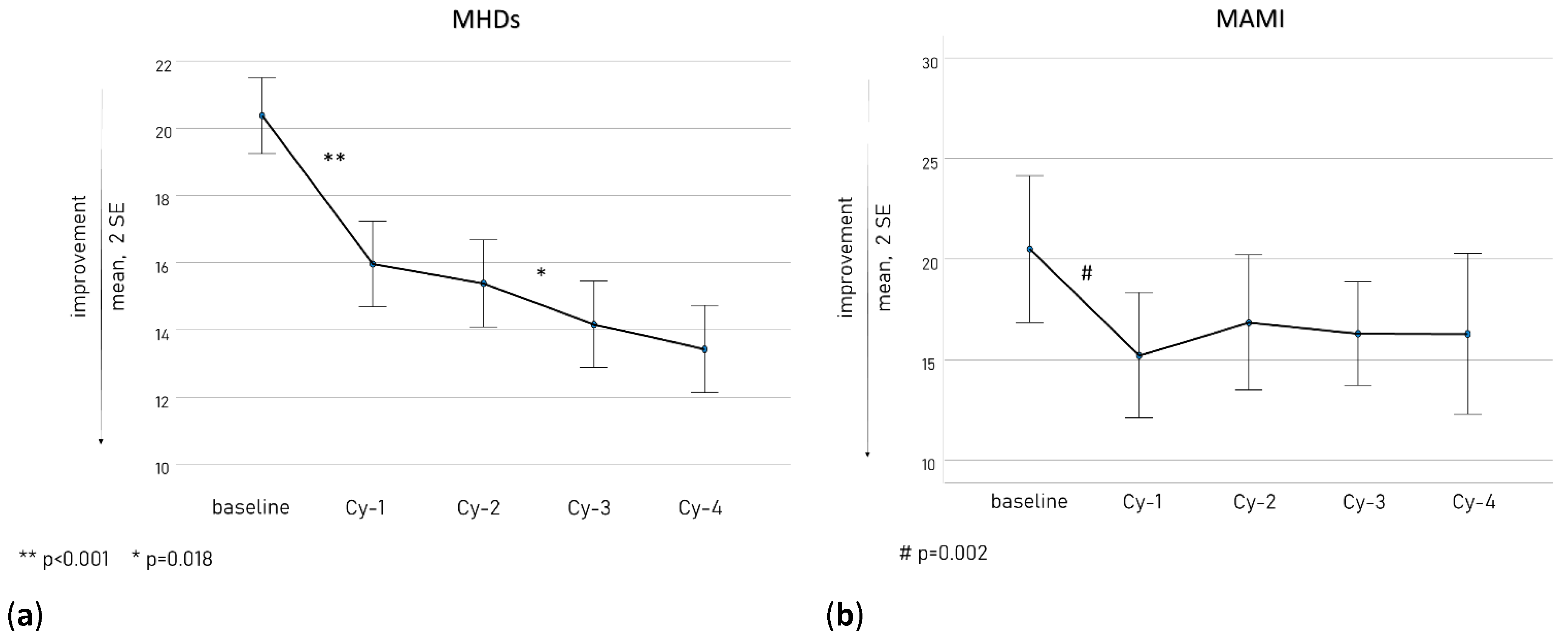
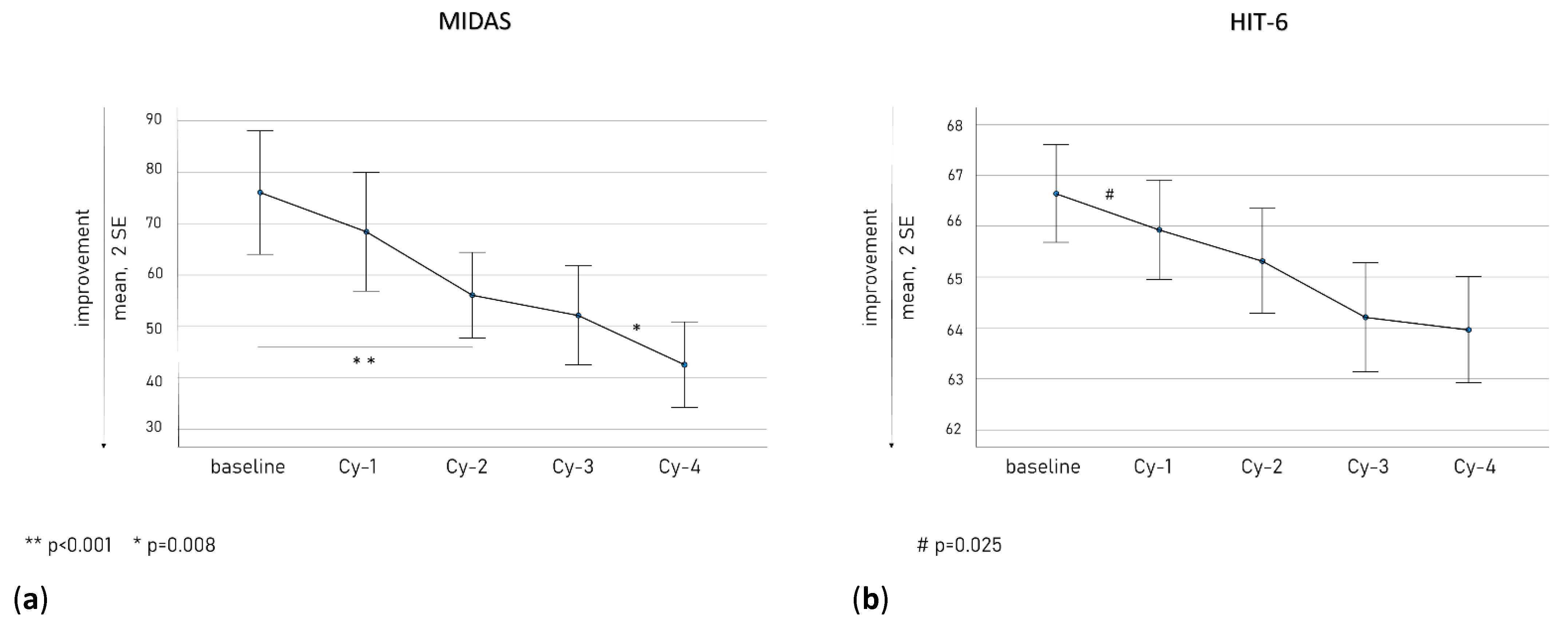
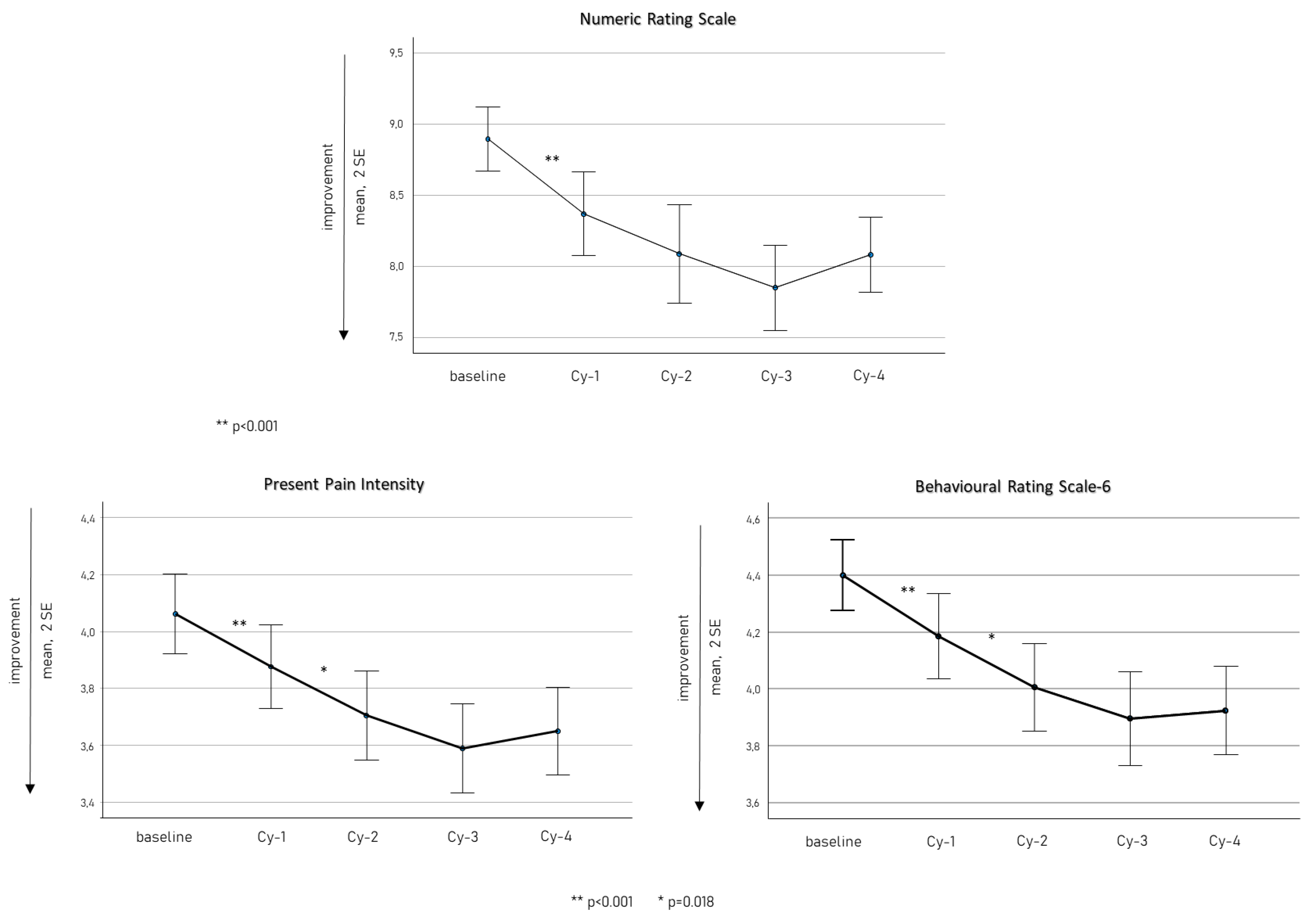
| Mean (SD) | Baseline | Cy-4 | p |
|---|---|---|---|
| Female n, (%) | 122 (80.3) | ||
| Age | 51.5 (11.3) | ||
| Monthly Headache Days | 20.4 (6.9) | 13.4 (7.8) | <0.001 |
| Monthly Acute Medication Intake | 20.9 (14.3) | 14.3 (14.4) | <0.001 |
| MIDAS | 74.1 (64.7) | 42.6 (44.9) | <0.001 |
| HIT-6 | 66.7 (5.7) | 64.0 (6.2) | <0.001 |
| NRS | 8.9 (1.4) | 8.07 (1.6) | <0.001 |
| PPI | 4.0 (0.8) | 3.7 (0.9) | <0.001 |
| BRS-6 | 4.4 (0.7) | 3.9 (0.9) | <0.001 |
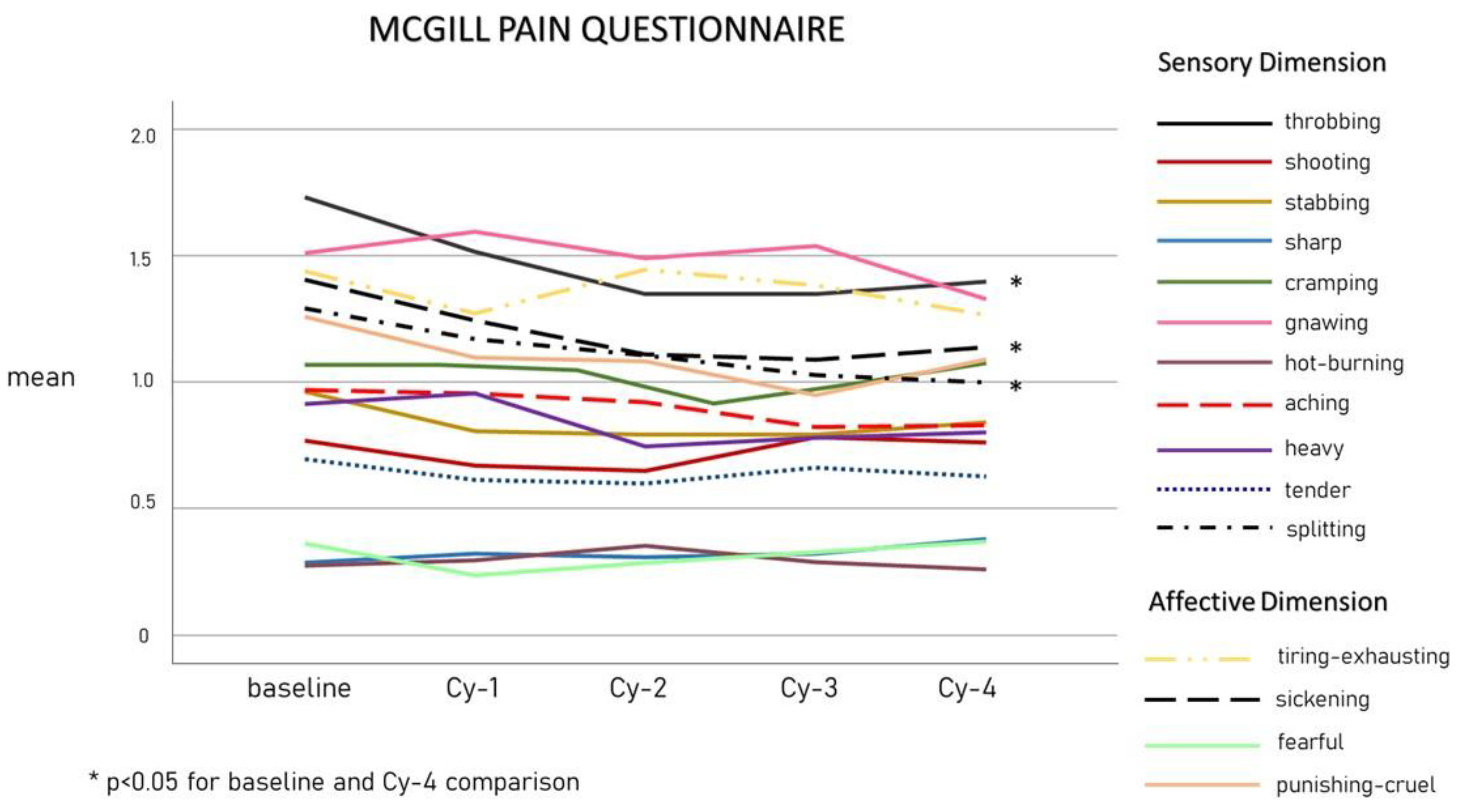
| mean (SD) | baseline | Cy-4 | p |
| McGill Pain Questionnaire | |||
| Sensory dimension of pain experience | |||
| Throbbing | 1.7 (1.3) | 1.4 (1.2) | 0.004 |
| Shooting | 0.8 (1.2) | 0.8 (1.2) | 0.956 |
| Stabbing | 0.9 (1.2) | 0.8 (1.2) | 0.444 |
| Sharp | 0.3 (0.8) | 0.4 (0.9) | 0.313 |
| Cramping | 1.0 (1.3) | 1.1 (1.2) | 0.797 |
| Gnawing | 1.5 (1.4) | 1.3 (1.9) | 0.389 |
| Hot-burning | 0.3 (0.8) | 0.3 (0.7) | 1.000 |
| Aching | 0.9 (1.3) | 0.8 (1.2) | 0.242 |
| Heavy | 0.9 (1.3) | 0.8 (1.2) | 0.281 |
| Tender | 0.7 (1.1) | 0.6 (1.0) | 0.484 |
| Splitting | 1.3 (1.4) | 1.0 (1.3) | 0.018 |
| Affective dimension of pain experience | |||
| Tiring—exhausting | 1.3 (1.4) | 1.2 (1.3) | 0.254 |
| Sickening | 1.4 (1.3) | 1.1 (1.2) | 0.017 |
| Fearful | 0.4 (0.9) | 0.4 (0.9) | 0.748 |
| Punishing—cruel | 1.4 (1.4) | 1.3 (1.3) | 0.218 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Altamura, C.; Brunelli, N.; Viticchi, G.; Salvemini, S.; Cecchi, G.; Marcosano, M.; Fofi, L.; Silvestrini, M.; Vernieri, F. Quantitative and Qualitative Pain Evaluation in Response to OnabotulinumtoxinA for Chronic Migraine: An Observational Real-Life Study. Toxins 2023, 15, 284. https://doi.org/10.3390/toxins15040284
Altamura C, Brunelli N, Viticchi G, Salvemini S, Cecchi G, Marcosano M, Fofi L, Silvestrini M, Vernieri F. Quantitative and Qualitative Pain Evaluation in Response to OnabotulinumtoxinA for Chronic Migraine: An Observational Real-Life Study. Toxins. 2023; 15(4):284. https://doi.org/10.3390/toxins15040284
Chicago/Turabian StyleAltamura, Claudia, Nicoletta Brunelli, Giovanna Viticchi, Sergio Salvemini, Gianluca Cecchi, Marilena Marcosano, Luisa Fofi, Mauro Silvestrini, and Fabrizio Vernieri. 2023. "Quantitative and Qualitative Pain Evaluation in Response to OnabotulinumtoxinA for Chronic Migraine: An Observational Real-Life Study" Toxins 15, no. 4: 284. https://doi.org/10.3390/toxins15040284
APA StyleAltamura, C., Brunelli, N., Viticchi, G., Salvemini, S., Cecchi, G., Marcosano, M., Fofi, L., Silvestrini, M., & Vernieri, F. (2023). Quantitative and Qualitative Pain Evaluation in Response to OnabotulinumtoxinA for Chronic Migraine: An Observational Real-Life Study. Toxins, 15(4), 284. https://doi.org/10.3390/toxins15040284







