Physiotherapy for Cervical Dystonia: A Systematic Review of Randomised Controlled Trials
Abstract
1. Introduction
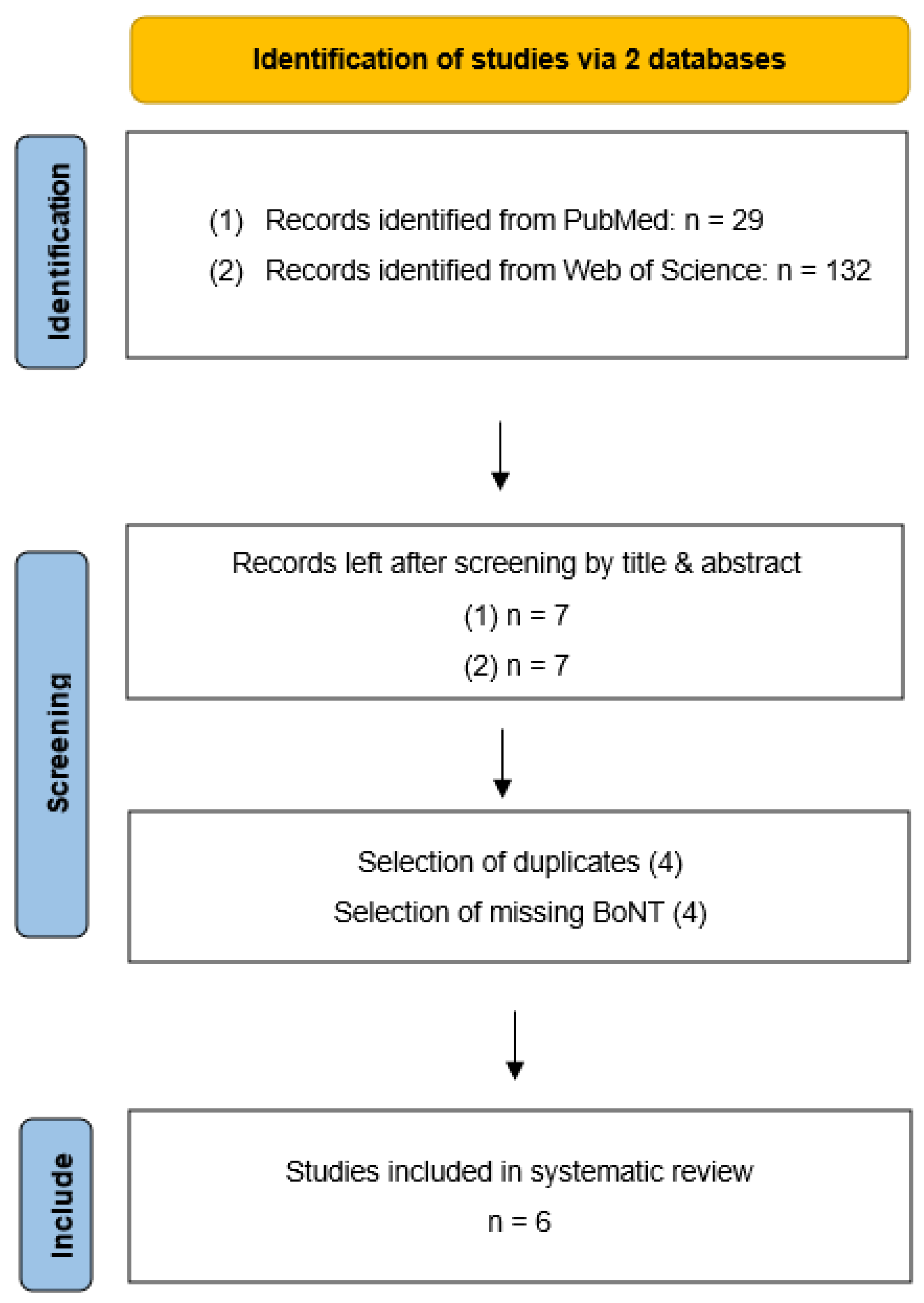
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Albanese, A.; Bhatia, K.; Bressman, S.B.; DeLong, M.R.; Fahn, S.; Fung, V.S.C.; Hallett, M.; Jankovic, J.; Jinnah, H.A.; Klein, C.; et al. Phenomenology and classification of dystonia: A consensus update. Mov. Disord. Off. J. Mov. Disord. Soc. 2013, 28, 863–873. [Google Scholar] [CrossRef] [PubMed]
- Reichel, G.; Stenner, A.; Jahn, A. The phenomenology of cervical dystonia. Fortschr. Der Neurol.-Psychiatr. 2009, 77, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Castelao, M.; Marques, R.E.; Duarte, G.S.; Rodrigues, F.B.; Ferreira, J.; Sampaio, C.; Moore, A.P.; Costa, J. Botulinum toxin type A therapy for cervical dystonia. Cochrane Database Syst. Rev. 2017, 12, CD003633. [Google Scholar] [CrossRef] [PubMed]
- Ip, C.W.; Bäumer, T.; Ceballos-Baumann, A. Dystonie, S1-Leitlinie. Deutsche Gesellschaft für Neurologie. Leitlinien für Diagnostik und Therapie in der Neurologie; Deutsche Gesellschaft für Neurologie: Berlin, Germany, 2021. [Google Scholar]
- De Pauw, J.; van der Velden, K.; Meirte, J.; van Daele, U.; Truijen, S.; Cras, P.; Mercelis, R.; De Hertogh, W. The effectiveness of physiotherapy for cervical dystonia: A systematic literature review. J. Neurol. 2014, 261, 1857–1865. [Google Scholar] [CrossRef] [PubMed]
- Loudovici-Krug, D.; Günther, A.; Best, N.; Derlien, S. Physiotherapy for Cervical Dystonia: A Systematic Review of Randomized Controlled Trials. Available online: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=333352 (accessed on 25 July 2022).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Cashin, A.G.; McAuley, J.H. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J. Physiother. 2019, 66, 59. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. Bmj 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Jost, W.H.; Hefter, H.; Stenner, A.; Reichel, G. Rating scales for cervical dystonia: A critical evaluation of tools for outcome assessment of botulinum toxin therapy. J. Neural Transm. 2013, 120, 487–496. [Google Scholar] [CrossRef] [PubMed]
- Dec-Ćwiek, M.; Porębska, K.; Sawczyńska, K.; Kubala, M.; Witkowska, M.; Zmijewska, K.; Antczak, J.; Pera, J. KinesioTaping after botulinum toxin type A for cervical dystonia in adult patients. Brain Behav. 2022, 12, e2541. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.; Rundle-Gonzalez, V.; Kulkarni, S.J.; Martinez-Ramirez, D.; Almeida, L.; Okun, M.S.; Shukla, A.W. A randomized study of botulinum toxin versus botulinum toxin plus physical therapy for treatment of cervical dystonia. Park. Relat. Disord. 2019, 63, 195–198. [Google Scholar] [CrossRef] [PubMed]
- Tassorelli, C.; Mancini, F.; Balloni, L.; Pacchetti, C.; Sandrini, G.; Nappi, G.; Martignoni, E. Botulinum toxin and neuromotor rehabilitation: An integrated approach to idiopathic cervical dystonia. Mov. Disord. Off. J. Mov. Disord. Soc. 2006, 21, 2240–2243. [Google Scholar] [CrossRef] [PubMed]
- Boyce, M.J.; Canning, C.G.; Mahant, N.; Morris, J.; Latimer, J.; Fung, V.S.C. Active exercise for individuals with cervical dystonia: A pilot randomized controlled trial. Clin. Rehabil. 2013, 27, 226–235. [Google Scholar] [CrossRef] [PubMed]
- van den Dool, J.; Visser, B.; Koelman, J.H.; Engelbert, R.H.; Tijssen, M.A. Long-term specialized physical therapy in cervical dystonia: Outcomes of a randomized controlled trial. Arch. Phys. Med. Rehabil. 2019, 100, 1417–1425. [Google Scholar] [CrossRef]
- Stanković, I.; Čolović, H.; Živković, V.; Stamenović, J.; Stanković, A.; Zlatanović, D.; Živković, D.; Stanković, T. The effect of physical therapy in the treatment of patients with cervical dystonia with or without concomitant use of botulinum toxin. Vojnosanit. Pregl. 2018, 75, 1035–1040. [Google Scholar] [CrossRef]
- Counsell, C.; Sinclair, H.; Fowlie, J.; Tyrrell, E.; Derry, N.; Meager, P.; Norrie, J.; Grosset, D. A randomized trial of specialized versus standard neck physiotherapy in cervical dystonia. Park. Relat. Disord. 2016, 23, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Pelosin, E.; Avanzino, L.; Marchese, R.; Stramesi, P.; Bilanci, M.; Trompetto, C.; Abbruzzese, G. Kinesiotaping reduces pain and modulates sensory function in patients with focal dystonia: A randomized crossover pilot study. Neurorehabilit. Neural Repair 2013, 27, 722–731. [Google Scholar] [CrossRef]
- Werner, C.; Loudovici-Krug, D.; Derlien, S.; Rakers, F.; Smolenski, U.C.; Lehmann, T.; Best, N.; Günther, A. Study protocol: Multimodal physiotherapy as an add-on treatment to botulinum neurotoxin type A therapy for patients with cervical dystonia: DysPT-multi—A prospective, multicentre, single-blind, randomized, controlled study. Trials 2021, 22, 740. [Google Scholar] [CrossRef] [PubMed]
| Authors | Patients | Duration/Severity of CD | Medication BoNT-A | Intervention | Measuring Time Points | Results | |
|---|---|---|---|---|---|---|---|
| Control | |||||||
| Dec-Cwiek et al. (2021) | n = 25 4 of which were females 54.7 ± 12.4 | 27.8 ± 12.4 years TWSTRS severity: 1 = 16.6 ± 9.01 2 = 19.11 ± 9.76 3 = 15.97 ± 8.79 | yes | Crossover design: Change of experimental group after 12 weeks Taping: once a week for 4 weeks | 1: BoNT + Kinesiotaping | Baseline 3 m 6 m 9 m | - Significant improvement in dystonia symptoms after BoNT injection regardless of group allocation - Quality of life improved significantly after taping |
| 2: BoNT + Sham taping | |||||||
| 3: BoNT (control) | |||||||
| Hu et al. (2019) | n = 16 9 of which were females 64.5 ± 5.4 (healthy controls: n = 10) | 14.4 ± 10.9 years TWSTRS severity: BoNT = 22.2 ± 11.2 BoNT + PT = 18.4 ± 8.7 | Yes (but patients who reported suboptimal benefits with BoNT alone) | BoNT alone (n = 8) | Baseline 6 w 3 m | - TWSTRS score (including pain), range of motion (ROM) and sensorimotor plasticity (SP) improved in PT-BoNT group - SP reached values of healthy controls | |
| BoNT + PT: 60 min of manual PT followed by six weeks of home-exercise programme/15 min/5× per week (n = 8) | |||||||
| Van den Dool et al. (2019) | n = 96 59 of which were females 58.9 ± 9.2 (finished: n = 72, thereof 42 female) | 12.7 ± 10.4 years TWSTRS severity: SPT: 16.91 ± 4.88 RPT = 16.00 ± 5.1 | yes | SPT: specialised physical therapy (n = 40) Mean: 31 ± 11 PT sessions 6 weeks: 2× per week (30 min) After 6 weeks: 1× per week (6 months in total) After 6 months: 1× per month 5× per day/10–15 min home exercise | Baseline 6 m 12 m | - No significant between group differences after 12 months - Both groups improved significantly - SPT: higher patient perceived effects and general health perception, lower treatment costs | |
| RPT: regular physical therapy (n = 32) Mean: 41 ± 24 PT sessions 1× per week (12 month in total) | |||||||
| Stankovic et al. (2017) | n = 14 11 of which were females 42.3 ± 5.6 | 13.5 ± 6.4 months | yes | BoNT + physical therapy (n = 9) PT five days after BoNT/five times weekly for two weeks | Baseline 1 m 3 m 6 m | - Highly significant increase in all the parameters of TWSTRS and decrease in changes in Tsui scale to all time points for BoNT + PT - Only PT with highly significant decrease of changes in Tsui scale was noticed only after one months | |
| Only physical therapy (n = 5) | |||||||
| Boyce et al. (2012) | n = 20 14 of which were females 57.8 ± 7.8 years | 10.2 ± 7.9 years TWSTRS: IG = 37.7 ± 10.7 CG = 34.7 ± 13.4 | None = 13 BoNT = 7 | Experimental group (n = 9) - Relaxation and individualised exercise program of active exercises to increase muscle strength of antagonist muscles and induce normal head posture - Combined with BoNT-A (n = 3) - 12 weeks program with 8 supervised sessions (30 min) (first 4 weeks: 1× per week and daily home exercises and the following 8 weeks: 1× per two weeks) | Baseline 6 w 3 m 4 m | - Patients were able to perform an active exercise program, but there was only a trend towards better scores on the TWSTRS and decreased depression (Beck Depression Inventory) - A power calculation showed the need to include 34 patients and an improvement of seven points on the TWSTRS for a positive treatment effect | |
| Control group (n = 11) - Whole body relaxation program - Combined with BoNT-A (n = 4) | |||||||
| Tassorelli et al. (2006) | n = 40 13 of which were females 51.3 ± 15.6 years | 11.5 ± 2.9 years | yes | - n = 20 - BoNT-A combined with physiotherapy: massage, stretching, postural re-education, strengthening of the axial muscles and 30 min biofeedback - 10 sessions of 60–90 min for two weeks | Baseline 3 m 6 m 9 m | - No significant decrease of severity of dystonia in both groups in the Tsui scale and TWSTRS - Significant less pain and increased ADL functioning in PT-group - The effects of BoNT-A lasted significantly longer, and a significantly lower dose was needed for the next injection | |
| - n = 20 - BoNT alone | |||||||
| PEDro Scale | Dec-Cwiek et al. (2021) [11] | Hu et al. (2019) [12] | van den Dool et al. (2019) [15] | Stankovic et al. (2017) [16] | Boyce et al. (2012) [14] | Tassorelli et al. (2006) [13] |
|---|---|---|---|---|---|---|
| 1. Eligibility criteria | y | y | Y | n.a. | y | y |
| 2. Randomly allocated | y | y | Y | y | y | y |
| 3. Allocation concealed | n | n | Y | n | Y | n |
| 4. Similar at baseline | y | y | y | y | Y | y |
| 5. Blinding of subjects | y | n | n | n | n | n |
| 6. Blinding of therapists | n | n | n | n | n | n |
| 7. Blinding of assessors | y | y | y | y | y | n |
| 8. One key outcome of 85% | n | y | n | y | y | y |
| 9. Allocated treatment/ITT | y | y | y | y | y | y |
| 10. Between-group statistical comparison | y | y | y | y | y | y |
| 11. Point measures and measures of variability | y | y | y | n | y | y |
| good | good | good | good | good | good |
| Study ID | D1 | D2 | D3 | D4 | D5 | Overall | ||
|---|---|---|---|---|---|---|---|---|
| Dec-Cwiek et al. (2021) [11] |  |  |  |  |  |  |  | Low risk |
| Hu et al. (2019) [12] |  |  |  |  |  |  |  | Some concerns |
| van den Dool et al. (2019) [15] |  |  |  |  |  |  |  | High risk |
| Stankovic et al. (2017) [16] |  |  |  |  |  |  | ||
| Boyce et al. (2012) [14] |  |  |  |  |  |  | D1 | Randomisation process |
| Tassorelli et al. (2006) [13] |  |  |  |  |  |  | D2 | Deviations from the intended interventions |
| D3 | Missing outcome data | |||||||
| D4 | Measurement of the outcome | |||||||
| D5 | Selection of the reported result |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Loudovici-Krug, D.; Derlien, S.; Best, N.; Günther, A. Physiotherapy for Cervical Dystonia: A Systematic Review of Randomised Controlled Trials. Toxins 2022, 14, 784. https://doi.org/10.3390/toxins14110784
Loudovici-Krug D, Derlien S, Best N, Günther A. Physiotherapy for Cervical Dystonia: A Systematic Review of Randomised Controlled Trials. Toxins. 2022; 14(11):784. https://doi.org/10.3390/toxins14110784
Chicago/Turabian StyleLoudovici-Krug, Dana, Steffen Derlien, Norman Best, and Albrecht Günther. 2022. "Physiotherapy for Cervical Dystonia: A Systematic Review of Randomised Controlled Trials" Toxins 14, no. 11: 784. https://doi.org/10.3390/toxins14110784
APA StyleLoudovici-Krug, D., Derlien, S., Best, N., & Günther, A. (2022). Physiotherapy for Cervical Dystonia: A Systematic Review of Randomised Controlled Trials. Toxins, 14(11), 784. https://doi.org/10.3390/toxins14110784





