A Systematic Review and Meta-Analysis of Efficacy of Botulinum Toxin A for Neuropathic Pain
Abstract
:1. Introduction
2. Meta-Analysis Results
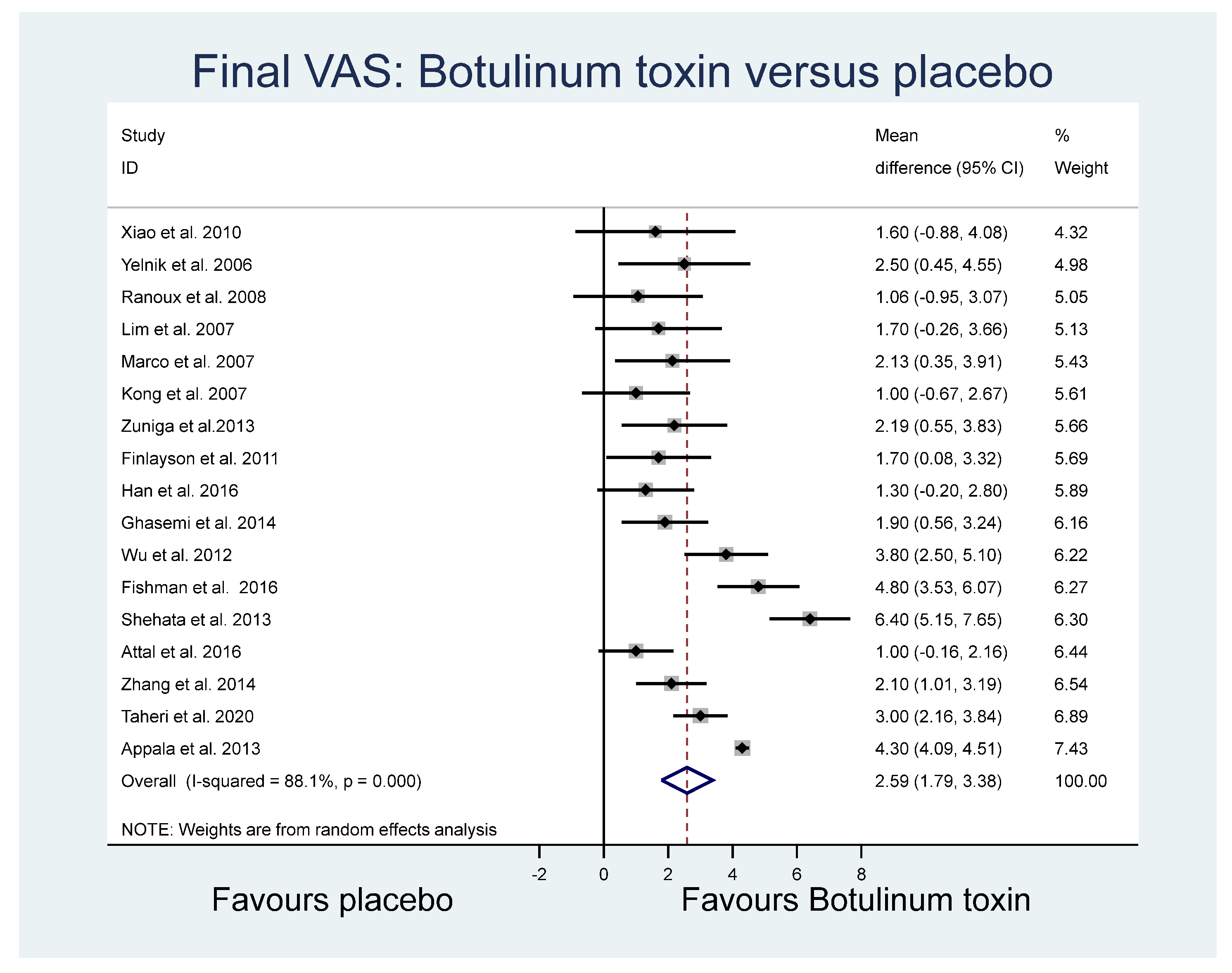
2.1. Final Visual Analogue Scale (VAS) Measures
2.2. VAS Difference
2.3. 50% Reduction in VAS
2.4. Pain Frequency (Number of Neuralgia Attacks in a Single Day)
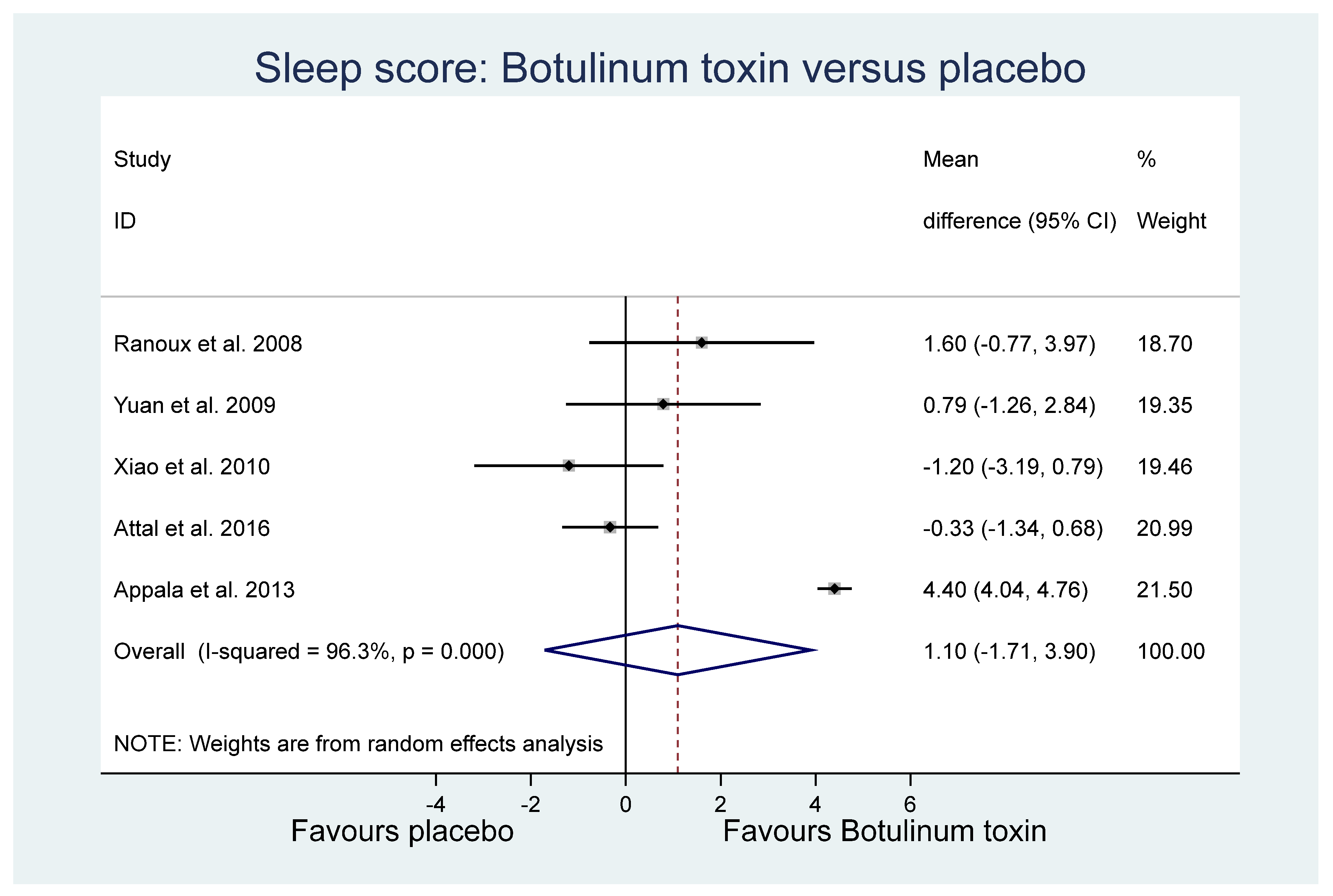
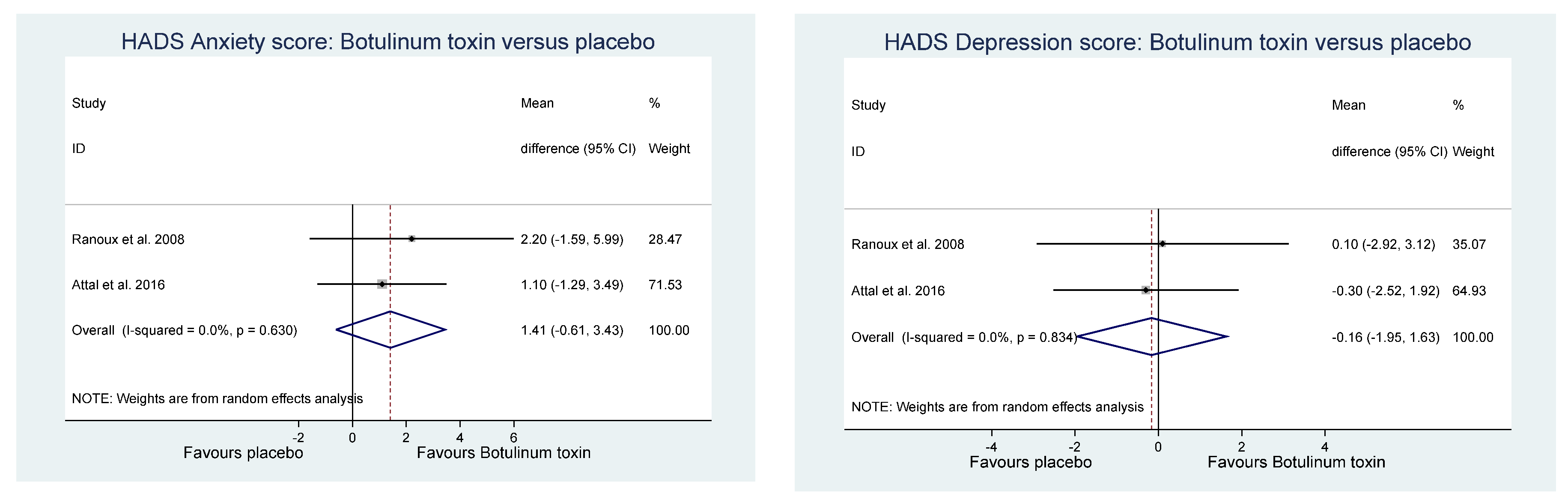
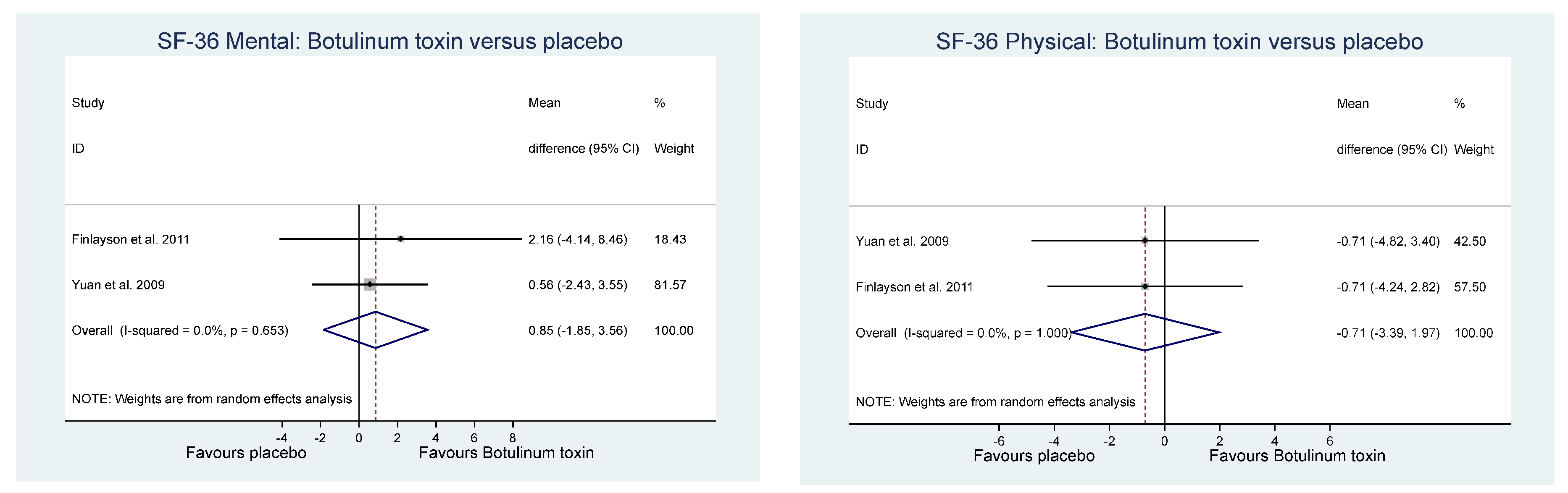
2.5. Other Relevant Outcomes
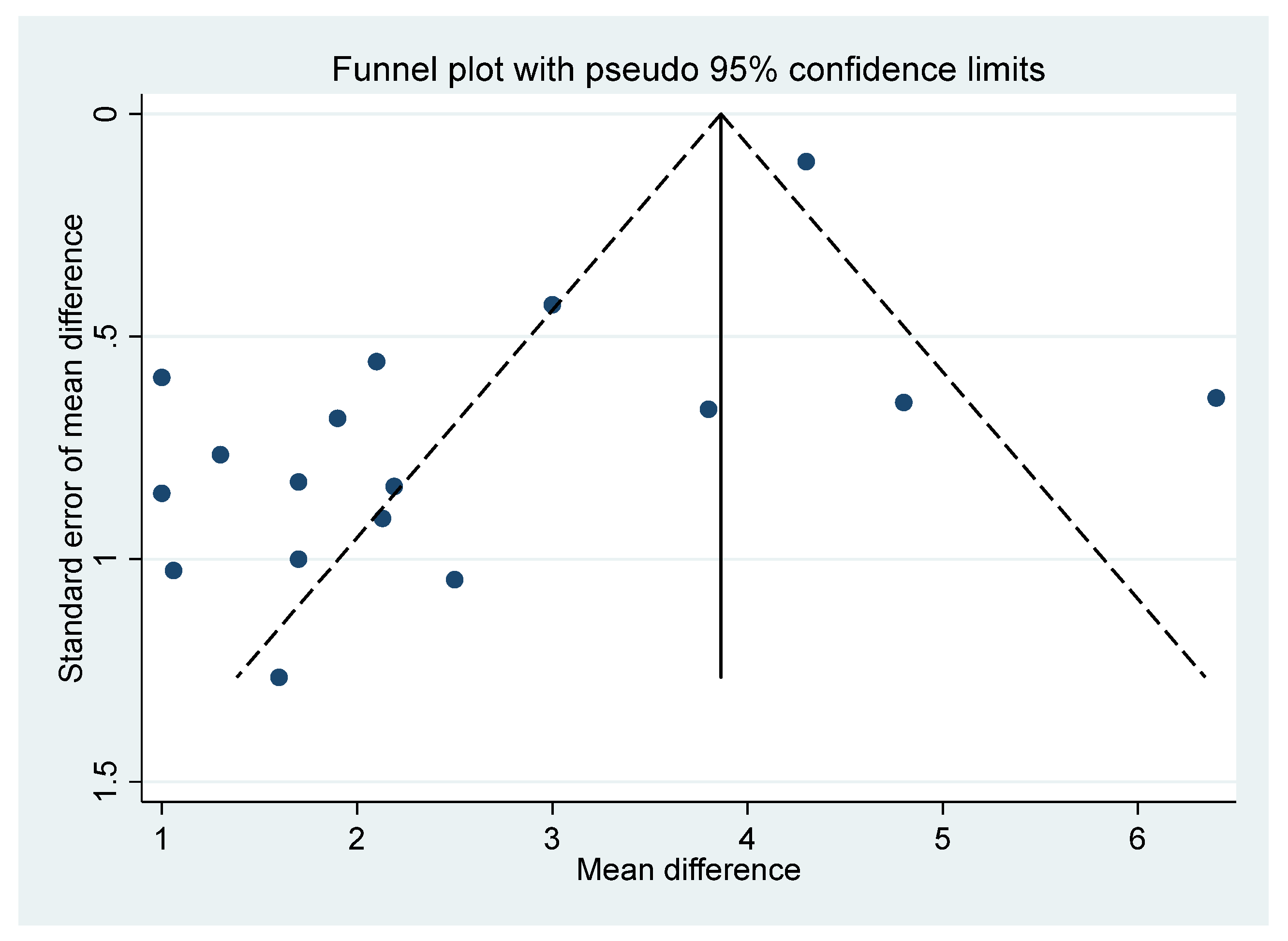
2.6. Final VAS Funnel Plot
3. Discussion
4. Conclusions
5. Methods
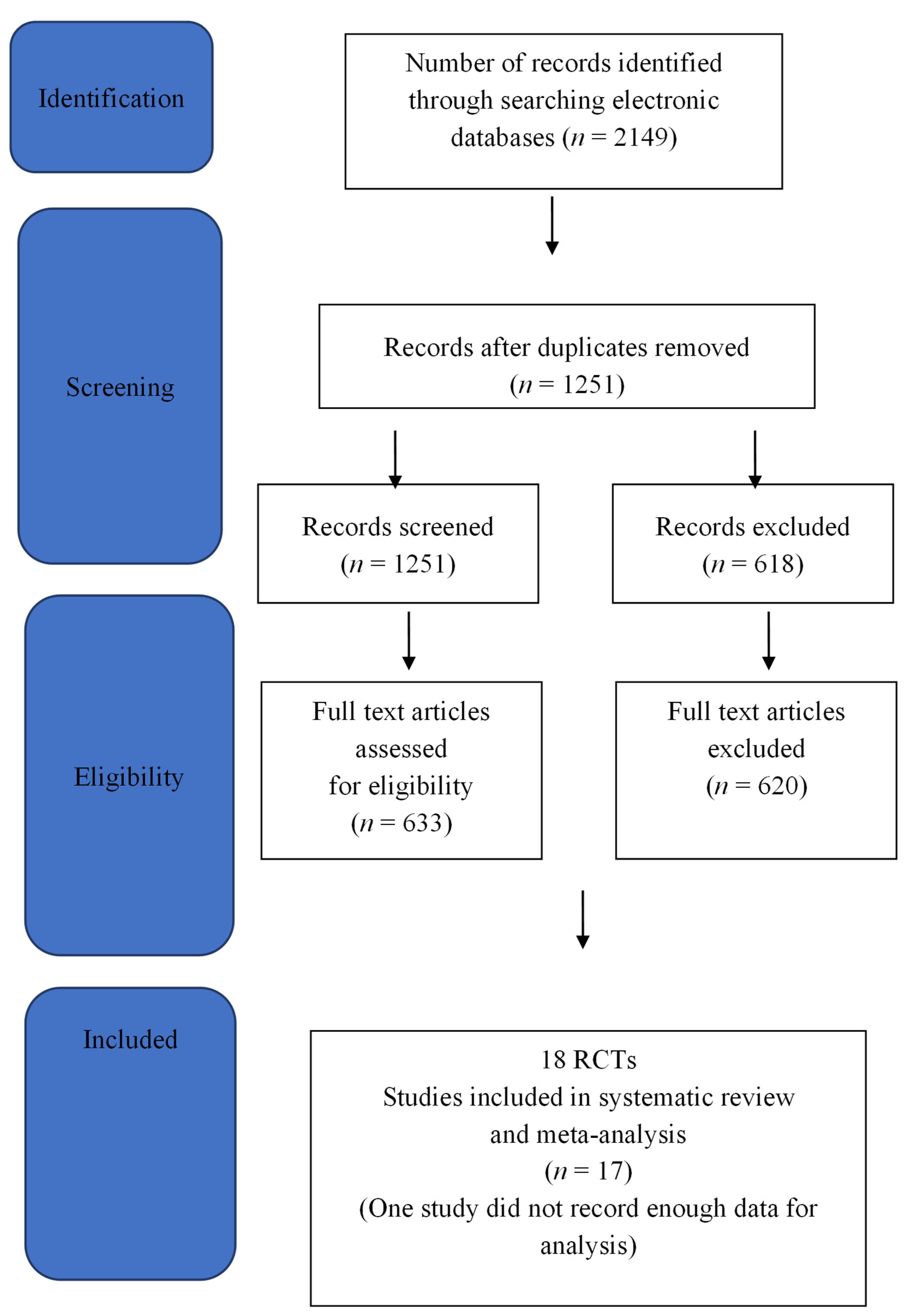
5.1. Search Methods
5.2. Document Sources
5.3. Document Identification Methods
5.4. Data Extraction
5.5. Selection Methods of Included Documents in the Analysis
5.6. Assessment of Methodological Quality
5.7. Selecting Documents for Systematic Review
5.8. Qualitative Analysis
5.9. Statistical Methods
5.10. RCT Quality Analysis
5.10.1. Importance of the Study Questions and Relationship with Sample Size
5.10.2. Sample Quality and Where the Sample Should Be Drawn
5.10.3. Study Error, Bias, and Confounding
5.10.4. Limitations in Study Design
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Smith, B.H.; Hébert, H.L.; Veluchamy, A. Neuropathic pain in the community: Prevalence, impact, and risk factors. Pain 2020, 161, S127–S137. [Google Scholar] [CrossRef] [PubMed]
- Wan, A. GP pain management: What are the P’s and A’s of pain management. Aust. Fam. Physician 2014, 43, 537–540. [Google Scholar] [PubMed]
- Crofford, L.J. Chronic Pain: Where the Body Meets the Brain. Trans. Am. Clin. Climatol. Assoc. 2015, 126, 167–183. [Google Scholar] [PubMed]
- Upshur, C.C.; Luckmann, R.S.; Savageau, J.A. Primary care provider concerns about management of chronic pain in community clinic populations. J. Gen. Intern. Med. 2006, 21, 652–655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Intiso, D. Therapeutic Use of Botulinum Toxin in Neurorehabilitation. J. Toxicol. 2012, 2012, 802893. [Google Scholar] [CrossRef] [Green Version]
- Gooriah, R.; Ahmed, F. Therapeutic uses of botulinum toxin. J. Clin. Toxicol. 2015, 5, 1–7. [Google Scholar]
- Pirazzini, M.; Rossetto, O.; Eleorpra, R.; Montecucco Witkin, J.M. Botulinum neurotoxins: Biology, pharammcologyand toxicology. Pharmacol. Rev. 2017, 69, 200–235. [Google Scholar] [CrossRef] [PubMed]
- Yuan, R.Y.; Sheu, J.J.; Yu, J.M.; Chen, W.T.; Tseng, I.J.; Chang, H.H.; Hu, C.J. Botulinum toxin for diabetic neuropathic pain: A randomized double-blind crossover trial. Neurology 2009, 72, 1473–1478. [Google Scholar] [CrossRef]
- Yelnik, A.P.; Colle, F.M.; Bonan, I.V.; Vicaut, E. Treatment of shoulder pain in spastic hemiplegia by reducing spasticity of the subscapular muscle: A randomised, double blind, placebo controlled study of botulinum toxin A. J. Neurol. Neurosurg. Psychiatry 2007, 78, 845–848. [Google Scholar] [CrossRef]
- Marco, E.; Duarte, E.; Vila, J.; Tejero, M.; Guillen, A. Is Botulinum Toxin Type A Effective in The Treatment of Spastic Shoulder Pain in Patients After Stroke Unclear Risk. A Double-blind Randomized Clinical Trial. J. Rehabil. Med. 2007, 39, 440–447. [Google Scholar] [CrossRef] [Green Version]
- Kong, K.-H.; Neo, J.-J.; Chua, K.S. A randomized controlled study of botulinum toxin A in the treatment of hemiplegic shoulder pain associated with spasticity. Clin. Rehabil. 2007, 21, 28–35. [Google Scholar] [CrossRef]
- Lim, J.-Y.; Koh, J.-H.; Paik, N.-J. Intramuscular Botulinum Toxin-A Reduces Hemiplegic Shoulder Pain. Stroke 2008, 39, 126–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ranoux, D.; Attal, N.; Morain, F.; Bouhassira, D. Botulinum toxin type a induces direct analgesic effects in chronic neuropathic pain. Ann. Neurol. 2008, 64, 274–283. [Google Scholar] [CrossRef]
- Xiao, L.; Mackey, S.; Hui, H.; Xong, D.; Zhang, Q.; Zhang, D. Subcutaneous Injection of Botulinum Toxin A Is Beneficial in Postherpetic Neuralgia. Pain Med. 2010, 11, 1827–1833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Finlayson, H.C.; O’Connor, R.J.; Brasher, P.M.; Travlos, A. Botulinum toxin injection for management of thoracic thoracic outlet syndrome: A double-blind, randomized trial. Pain 2011, 152, 2023–2028. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-J.; Lian, Y.-J.; Zheng, Y.-K.; Zhang, H.-F.; Chen, Y.; Xie, N.-C.; Wang, L.-J. Botulinum toxin type A for the treatment of trigeminal neuralgia: Results from a randomized, double-blind, placebo-controlled trial. Cephalalgia 2012, 32, 443–450. [Google Scholar] [CrossRef]
- Shehata, H.S.; El-Tamawy, M.S.; Shalaby, N.M.; Ramzy, G. Botulinum toxin-type A: Could it be an effective treatment option in intractable trigeminal neuralgia? J. Headache Pain 2013, 19, 92–98. [Google Scholar] [CrossRef] [Green Version]
- Apalla, Z.; Sotiriou, E.; Lallas, A.; Lazaridou, E.; Loannides, D. Botulinum Toxin A in Postherpetic Neuralgia A Parallel, Randomized, Double-Blind, Single-Dose, Placebo-controlled Trial. Clin. J. Pain 2013, 29, 857–864. [Google Scholar] [CrossRef]
- Zúñiga, C.; Piedimonte, F.; Díaz, S.; Micheli, F. Acute Treatment of Trigeminal Neuralgia With Onabotulinum Toxin A. Clin. Neuropharmacol. 2013, 36, 146–150. [Google Scholar] [CrossRef]
- Ghasemi, M.; Ansari, M.; Basiri, K.; Shaygannejad, V. The effects of intradermal botulinum toxin type a injections on pain symptoms of patients with diabetic neuropathy. J. Res. Med. Sci. 2014, 19, 106–111. [Google Scholar]
- Zhang, H.; Lian, Y.; Ma, Y.; Chen, Y.; He, C.; Xie, N.; Wu, C. Two doses of botulinum toxin type A for the treatment of trigeminal neuralgia: Observation of therapeutic effect from a randomized, double-blind, placebo-controlled trial. J. Headache Pain 2014, 15, 65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Han, Z.; Song, D.H.; Oh, H.; Chung, M.E. Botulinum toxin type A for neuropathic pain in patients with spinal cord injury. Ann. Neurol. 2016, 79, 569–578. [Google Scholar] [CrossRef] [PubMed]
- Attal, N.; de Andrade, D.C.; Adam, F.; Ranoux, D.; Teixeira, M.J.; Galhardoni, R.; Raicher, I.; Üçeyler, N.; Sommer, C.; Bouhassira, D. Safety and efficacy of repeated injections of botulinum toxin A in peripheral neuropathic pain (BOTNEP): A randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2016, 15, 555–565. [Google Scholar] [CrossRef]
- Fishman, L.M.; Wilkins, A.N.; Rosner, B. Electro physiologically identified piriformis syndrome is successfully treated with incobotulinum toxin and physical therapy. Muscle Nerve 2017, 56, 258–263. [Google Scholar] [CrossRef]
- Salehi, H.; Moussaei, M.; Kamiab, Z.; Vakilian, A. The effects of botulinum toxin type A injection on pain symptoms, quality of life, and sleep quality of patients with diabetic neuropathy: A randomized double-blind clinical trial. Iran. J. Neurol. 2019, 18, 99–107. [Google Scholar] [CrossRef]
- Taheri, M.; Sedaghat, M.; Solhpour, A.; Rostami, P.; Lima, B.S. The Effect of Intradermal Botulinum Toxin a injections on painful diabetic polyneuropathy. Diabetes Metab. Syndr. 2020, 14, 1823–1828. [Google Scholar] [CrossRef]
- Meng, F.; Peng, K.; Yang, J.-P.; Ji, F.-H.; Xia, F.; Meng, X.-W. Botulinum toxin-A for the treatment of neuralgia: A systematic review and meta-analysis. J. Pain Res. 2018, 11, 2343–2351. [Google Scholar] [CrossRef] [Green Version]
- Shackleton, T.; Ram, S.; Black, M.; Ryder, J.; Clark, G.T.; Enciso, R. The efficacy of botulinum toxin for the treatment of trigeminal ad postherpetic neuralgia: A systematic review with meta-analyses. Oral Surgery Oral Med. Oral Path. Oral Rad. 2016, 19, 61–71. [Google Scholar] [CrossRef]
- Morra, M.E.; Elgebaly, A.; Elmaraezy, A.; Khalil, A.M.; Altibi, A.M.A.; Vu, T.L.-H.; Mostafa, M.R.; Huy, N.T.; Hirayama, K. Therapeutic efficacy and safety of botulinum toxin A therapy in trigeminal neuralgia: A systematic review and meta-analysis of randomised controlled trials. J. Headache Pain 2016, 17, 63. [Google Scholar] [CrossRef] [Green Version]
- Nauman, M.; Jankovic, J. Safety of botulinum toxin type A: A systematic review and meta-analysis. Curr. Med. Res. Opin. 2004, 20, 981–990. [Google Scholar] [CrossRef]
- Herd, C.P.; Tomlinson, C.L.; Rick, C.; Scotton, W.J.; Edwards, J.; Ives, N.J.; Clarke, C.; Sinclair, A.J. Cochrane systematic review and meta-analysis of botulinum toxin for the prevention of migraine. BMJ Open 2019, 9, e027953. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lakhan, S.E.; Velasco, D.N.; Tepper, D. Botulinum Toxin-A for Painful Diabetic Neuropathy: A Meta-Analysis. Pain Med. 2015, 16, 1773–1780. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wei, J.; Zhu, X.; Yang, G.; Shen, J.; Xie, P.; Zuo, X.; Xia, L.; Han, Q.; Zhao, Y. The efficacy and safety of botulinum toxin type A treatment of trigeminal neuralgia and peripheral neuropathic pain: A meta-analysis of randomised controlled trails. Brain Behav. 2019, 9, e01409. [Google Scholar] [CrossRef] [PubMed]
- NHMRC Levels of Evidence and Grades for Recommendations for Developers of Guidelines. Available online: https://www.nhmrc.gov.au/sites/default/files/images/NHMRC%20Levels%20and%20Grades%20(2009).pdf (accessed on 20 November 2021).
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; DeBeer, H.; et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef] [PubMed]
- Finnerup, N.B.; Attal, N.; Haroutounian, S.; McNicol, E.; Baron, R.; Dworkin, R.H.; Gilron, I.; Haanpää, M.; Hansson, P.; Jensen, T.S.; et al. Pharmacotherapy for neuropathic pain in adults: A systematic review and meta-analysis. Lancet Neurol. 2015, 14, 162–173. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.W.; Kim, K.S.; Chung, J.H.; Park, H.J.; Sohn, Y.S.; Jeon, W.J.; Cho, S.Y.; Shin, W.J. Assessing the quality of randomised controlled trails of complex regional pain syndrome published in the Journal of Clinical Pain Medicine Field. J. Korean Med. Sci. 2012, 27, 973–980. [Google Scholar]
- Egeo, G.; Fofi, L.; Barbanti, P. Botulinum Neurotoxin for the Treatment of Neuropathic Pain. Front. Neurol. 2020, 11, 716. [Google Scholar] [CrossRef]
- Datta Gupta, A.; Wilson, D.H. Spasticity/Dystonia—Current Pharmaceutical Benefits Scheme-Guidelines for Treatment with Botulinum Toxin—A Case for Change. Med. J. Aust. 2018, 208, 379–381. [Google Scholar] [CrossRef]
- Levy, N.; Sturgess, J.; Mills, P. “Pain as the fifth vital sign” and dependence on the “numerical pain scale” is being abandoned in the US: Why? Br. J. Anaesth. 2018, 120, 435–438. [Google Scholar] [CrossRef] [Green Version]
- Matak, I.; Riederer, P.; Lackovic, Z. Botulinum toxin’s axonal transport properties from periphery to spinal cord. Neurochem. Int. 2012, 61, 236–239. [Google Scholar] [CrossRef] [Green Version]
- Sterne, J.A.C.; Sutton, A.J.; Ioannidis, J.P.A.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rucker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [Green Version]
- Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 edited by Julian PT and Sally Green. Available online: https://handbook-5-1.cochrane.org/ (accessed on 20 November 2021).
- Song, F.; Khan, K.S.; Dinnes, J.; Sutton, A.J. Asymmetric funnel plots and publication bias in meta-analyses of diagnostic accuracy. Int. J. Epidemiol. 2002, 31, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Lucas, R.E. Re-evaluating the strengths and weaknesses of self-report measures of subjective well-being. In Handbook of Well-Being; Diener, E., Oishi, S., Tay, L., Eds.; DEF Publishers: Salt Lake City, UT, USA, 2018; Available online: nobascholar.com (accessed on 20 November 2021).
- Smith, B.H.; Torrance, N.; Ferguson, J.A.; Bennett, M.I.; Serpell, M.G.; Dunn, K.M. Towards a definition of refractory neuropathic pain for epidemiological research. An international Delphi survey of experts. BMC Neurol. 2012, 12, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bendiger, T.; Plunkett, N. Measurement of pain medicine. An international Delphi Survey of Experts. BJA Educ. 2016, 16, 310–315. [Google Scholar]

| Authors/Year | Primary Outcome | Other Outcome | Sample Size | Power | Sample Source | Blinding | Entry Criteria | NP Diagnosed | Pain Source | BT Dose (Units) | SD/CI | Study Effect Sig. | Study Duration | n of Doses |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yelnik et al., 2006 | VAS | No | n = 20 | No | Not Given | DBND | Yes | No | HSP | 500 | Yes | Yes | 4 weeks | 1 |
| Lim et al., 2008 | NPS | No | n = 29 | Yes | In/Out | DBND | Yes | No | HSP | 100 | Yes | Yes | 12 weeks | 1 |
| Marco et al., 2007 | VAS | No | n = 31 | Yes | In | DBD | Yes | No | HSP | 500 | Yes | Yes | 6 months | 1 |
| Kong et al., 2007 | VAS | No | n = 17 | Yes | Out | DBND | Yes | No | HSP | 500 | No | Yes | 12 weeks | 1 |
| Ranoux et al., 2008 | BPI VAS | No | n = 29 | No | Pat | DBND | Yes | No | PHN, PT, PO | 20–190 | Yes | Yes | 24 weeks | 1 |
| Yuan et al., 2009 | VAS | Yes | n = 18 | No | Com | DBND | Yes | Yes | DN | 50 | Yes | Yes | 12 weeks | 2 |
| Xiao et al., 2010 | VAS | Yes | n = 60 | No | Ins | DBDD | Yes | No | PHN | 200 | No | Yes | 3 months | 1 |
| Finlayson et al., 2011 | VAS | No | n = 38 | Yes | Out | DBD | Yes | Yes | PS | 75 | Yes | No | 6 months | 1 |
| Wu et al., 2012 | VAS | Yes | n = 42 | No | Out | DBND | Yes | No | TN | 100 | No | Yes | 13 weeks | 1 |
| Zuniga et al., 2013 | VAS | No | n = 36 | No | Out | DBD | nYes | No | PHN | 50 | Yes | Yes | 12 weeks | 1 |
| Shehata et al., 2013 | VAS | Yes | n = 20 | No | Hos | DBD | Yes | Yes | TN | 100 | Yes | Yes | 12 weeks | 1 |
| Apalla et al., 2013 | VAS | No | n = 30 | Yes | Out | DBD | Yes | No | PHN | 100 | Yes | Yes | 16 weeks | 1 |
| Ghasemi et al., 2014 | NPS | Yes | n = 40 | No | Com | DBND | Yes | Yes | DN | 100 | Yes | Yes | 3 weeks | 1 |
| Zhang et al., 2014 | VAS | No | n = 84 | No | Out/In | DBD | Yes | No | TN | 25 & 75 | Yes | Yes | 9 weeks | 1 |
| Han et al., 2016 | VAS | No | n = 40 | Yes | Com | DBD | Yes | No | SCI | 200 | Yes | Yes | 8 weeks | 1 |
| Fishman et al., 2017 | VAS | No | n = 28 | No | Out | DBND | Yes | Yes | PS | 300 | Yes | Yes | 12 weeks | 1 |
| Taheri et al., 2020 | VAS | No | n = 141 | Yes | Out | DBD | Yes | Yes | DN | 150 | Yes | Yes | 16 weeks | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Datta Gupta, A.; Edwards, S.; Smith, J.; Snow, J.; Visvanathan, R.; Tucker, G.; Wilson, D. A Systematic Review and Meta-Analysis of Efficacy of Botulinum Toxin A for Neuropathic Pain. Toxins 2022, 14, 36. https://doi.org/10.3390/toxins14010036
Datta Gupta A, Edwards S, Smith J, Snow J, Visvanathan R, Tucker G, Wilson D. A Systematic Review and Meta-Analysis of Efficacy of Botulinum Toxin A for Neuropathic Pain. Toxins. 2022; 14(1):36. https://doi.org/10.3390/toxins14010036
Chicago/Turabian StyleDatta Gupta, Anupam, Suzanne Edwards, Jessica Smith, John Snow, Renuka Visvanathan, Graeme Tucker, and David Wilson. 2022. "A Systematic Review and Meta-Analysis of Efficacy of Botulinum Toxin A for Neuropathic Pain" Toxins 14, no. 1: 36. https://doi.org/10.3390/toxins14010036
APA StyleDatta Gupta, A., Edwards, S., Smith, J., Snow, J., Visvanathan, R., Tucker, G., & Wilson, D. (2022). A Systematic Review and Meta-Analysis of Efficacy of Botulinum Toxin A for Neuropathic Pain. Toxins, 14(1), 36. https://doi.org/10.3390/toxins14010036





