Early Botulinum Toxin Type A Injection for Post-Stroke Spasticity: A Longitudinal Cohort Study
Abstract
1. Introduction
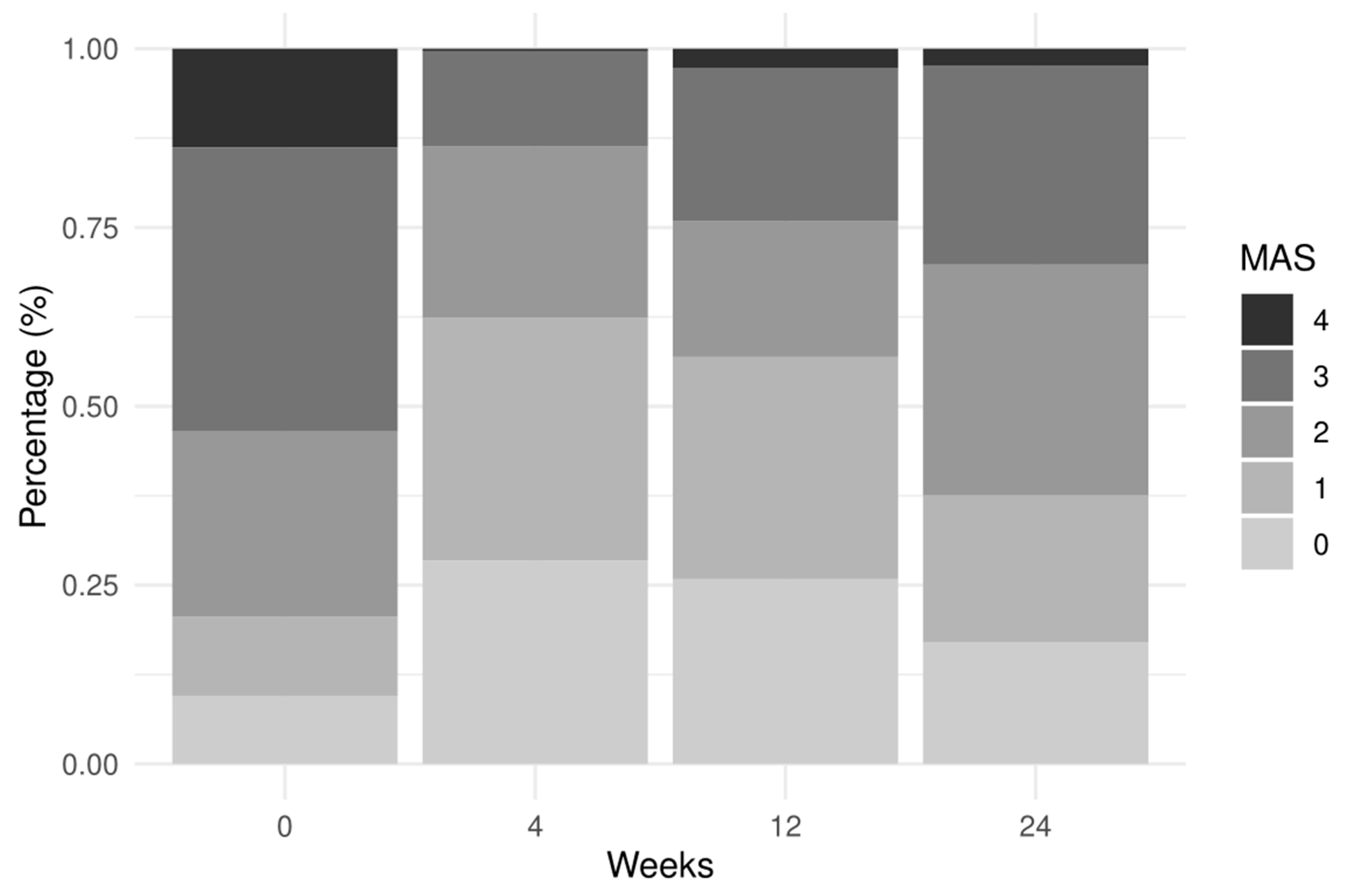
2. Results
3. Discussion
Limitations
4. Conclusions
5. Materials and Methods
5.1. Statistical Methods
Cumulative Logistic Mixed-Effects Model
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lundström, E.; Smits, A.; Terént, A.; Borg, J. Time-course and determinants of spasticity during the first six months following first-ever stroke. J. Rehabil. Med. 2010, 42, 296–301. [Google Scholar] [CrossRef]
- Lance, J.W. The control of muscle tone, reflexes, and movement: Robert Wartenberg Lecture. Neurology 1980, 30, 1303–1313. [Google Scholar] [CrossRef]
- Wissel, J.; Verrier, M.; Simpson, D.M.; Charles, D.; Guinto, P.; Papapetropoulos, S.; Sunnerhagen, K.S. Post-stroke spasticity: Predictors of early development and considerations for therapeutic intervention. PM R 2015, 7, 60–67. [Google Scholar] [CrossRef]
- Zeng, H.; Chen, J.; Guo, Y.; Tan, S. Prevalence and risk factors for spasticity after stroke: A systematic review and meta-analysis. Front. Neurol. 2021, 11, 616097. [Google Scholar] [CrossRef]
- Doussoulin, A.; Rivas, C.; Bacco, J.; Sepúlveda, P.; Carvallo, G.; Gajardo, C.; Soto, A.; Rivas, R. Prevalence of spasticity and postural patterns in the upper extremity post stroke. J. Stroke Cerebrovasc. Dis. 2020, 29, 105253. [Google Scholar] [CrossRef]
- Brainin, M.; Norrving, B.; Sunnerhagen, K.S.; Goldstein, L.B.; Cramer, S.C.; Donnan, G.A.; Duncan, P.W.; Francisco, G.; Good, D.; Graham, G.; et al. International PSS Disability Study Group. Poststroke chronic disease management: Towards improved identification and interventions for poststroke spasticity-related complications. Int. J. Stroke 2011, 6, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Sommerfeld, D.K.; Eek, E.U.; Svensson, A.K.; Holmqvist, L.W.; von Arbin, M.H. Spasticity after stroke: Its occurrence and association with motor impairments and activity limitations. Stroke 2004, 35, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Sunnerhagen, K.S.; Opheim, A.; Alt Murphy, M. Onset, time course and prediction of spasticity after stroke or traumatic brain injury. Ann. Phys. Rehabil. Med. 2019, 62, 431–434. [Google Scholar] [CrossRef] [PubMed]
- Sunnerhagen, K.S. Predictors of spasticity after stroke. Curr. Phys. Med. Rehabil. Rep. 2016, 4, 182–185. [Google Scholar] [CrossRef]
- Simpson, D.M.; Hallett, M.; Ashman, E.J.; Comella, C.L.; Green, M.W.; Gronseth, G.S.; Armstrong, M.J.; Gloss, D.; Potrebic, S.; Jankovic, J.; et al. Practice guideline update summary: Botulinum neurotoxin for the treatment of blepharospasm, cervical dystonia, adult spasticity, and headache: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology 2016, 86, 1818–1826. [Google Scholar] [CrossRef] [PubMed]
- Sheean, G. Botulinum toxin should be first-line treatment for poststroke spasticity. J. Neurol Neurosurg Psychiatry 2009, 80, 359. [Google Scholar] [CrossRef]
- Wissel, J.; Ward, A.B.; Erztgaard, P.; Bensmail, D.; Hecht, M.J.; Lejeune, T.M.; Schnider, P.; Altavista, M.C.; Cavazza, S.; Deltombe, T.; et al. European consensus table on the use of botulinum toxin type A in adult spasticity. J. Rehabil. Med. 2009, 41, 13–25. [Google Scholar] [CrossRef] [PubMed]
- Rosales, R.L.; Efendy, F.; Teleg, E.S.; Delos Santos, M.M.; Rosales, M.C.; Ostrea, M.; Tanglao, M.J.; Ng, A.R. Botulinum toxin as early intervention for spasticity after stroke or non-progressive brain lesion: A meta-analysis. J. Neurol. Sci. 2016, 371, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, C.; Ispoglou, S.; Helliwell, B.; Hicklin, D.; Sturman, S.; Pandyan, A. Can the early use of botulinum toxin in post stroke spasticity reduce contracture development? A randomised controlled trial. Clin. Rehabil. 2021, 35, 399–409. [Google Scholar] [CrossRef] [PubMed]
- Ismail, F.; Boulias, C.; Phadke, C.; Dagher, J.; Ethans, K.; Khan, O.; Kleiner, G.; Li Pi Shan, R.; Liem, N.; Lo, A.; et al. Early botulinum toxin injections for spasticity management post-stroke: A Delphi-based Canadian consensus. Arch. Phys. Med. Rehabil. 2019, 100, e175. [Google Scholar] [CrossRef]
- Picelli, A.; Baricich, A.; Cisari, C.; Paolucci, S.; Smania, N.; Sandrini, G. The Italian real-life post-stroke spasticity survey: Unmet needs in the management of spasticity with botulinum toxin type A. Funct. Neurol. 2017, 32, 89–96. [Google Scholar] [CrossRef]
- Smania, N.; Colosimo, C.; Bentivoglio, A.R.; Sandrini, G.; Picelli, A. Use of botulinum toxin type A in the management of patients with neurological disorders: A national survey. Funct. Neurol. 2013, 28, 253–258. [Google Scholar] [CrossRef]
- Wissel, J.; Fheodoroff, K.; Hoonhorst, M.; Müngersdorf, M.; Gallien, P.; Meier, N.; Hamacher, J.; Hefter, H.; Maisonobe, P.; Koch, M. Effectiveness of AbobotulinumtoxinA in post-stroke upper limb spasticity in relation to timing of treatment. Front. Neurol. 2020, 11, 104. [Google Scholar] [CrossRef]
- Urban, P.P.; Wolf, T.; Uebele, M.; Marx, J.J.; Vogt, T.; Stoeter, P.; Bauermann, T.; Weibrich, C.; Vucurevic, G.D.; Schneider, A.; et al. Occurence and clinical predictors of spasticity after ischemic stroke. Stroke 2010, 41, 2016–2020. [Google Scholar] [CrossRef]
- Rosales, R.L.; Balcaitiene, J.; Berard, H.; Maisonobe, P.; Goh, K.J.; Kumthornthip, W.; Mazlan, M.; Latif, L.A.; Delos Santos, M.M.D.; Chotiyarnwong, C.; et al. Early AbobotulinumtoxinA (Dysport®) in post-stroke adult upper limb spasticity: ONTIME pilot study. Toxins 2018, 10, 253. [Google Scholar] [CrossRef]
- Field, M.; Splevins, A.; Picaut, P.; van der Schans, M.; Langenberg, J.; Noort, D.; Snyder, D.; Foster, K. AbobotulinumtoxinA (Dysport®), OnabotulinumtoxinA (Botox®), and IncobotulinumtoxinA (Xeomin®) neurotoxin content and potential implications for duration of response in patients. Toxins 2018, 10, 535. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W.; Smith, M.B. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys. Ther. 1987, 67, 206–207. [Google Scholar] [CrossRef]
- Paternostro-Sluga, T.; Grim-Stieger, M.; Posch, M.; Schuhfried, O.; Vacariu, G.; Mittermaier, C.; Bittner, C.; Fialka-Moser, V. Reliability and validity of the Medical Research Council (MRC) scale and a modified scale for testing muscle strength in patients with radial palsy. J. Rehabil. Med. 2008, 40, 665–671. [Google Scholar] [CrossRef] [PubMed]
- Italian Stroke Organization. Available online: https://www.iso-stroke.it (accessed on 29 December 2020).
- Winstein, C.J.; Stein, J.; Arena, R.; Bates, B.; Cherney, L.R.; Cramer, S.C.; Deruyter, F.; Eng, J.J.; Fisher, B.; Harvey, R.L.; et al. American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Quality of Care and Outcomes Research. Guidelines for adult stroke rehabilitation and recovery: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2016, 47, e98–e169. [Google Scholar] [CrossRef] [PubMed]
- Collin, C.; Wade, D. Assessing motor impairment after stroke: A pilot reliability study. J. Neurol. Neurosurg. Psychiatry 1990, 53, 576–579. [Google Scholar] [CrossRef] [PubMed]
- Duncan, P.W.; Propst, M.; Nelson, S.G. Reliability of the Fugl-Meyer assessment of sensorimotor recovery following cerebrovascular accident. Phys. Ther. 1983, 63, 1606–1610. [Google Scholar] [CrossRef] [PubMed]
- Banks, J.L.; Marotta, C.A. Outcomes validity and reliability of the modified Rankin scale: Implications for stroke clinical trials: A literature review and synthesis. Stroke 2007, 38, 1091–1096. [Google Scholar] [CrossRef] [PubMed]
- Regression Models for Ordinal Data. R Package Version 2019.12-10. Available online: https://CRAN.R-project.org/package=ordinal (accessed on 29 December 2020).

| Overall | Women (n = 31) | Men (n = 52) | p-Value | |
|---|---|---|---|---|
| Study center, No. (%) | 0.58 | |||
| Center #1 | 8 (9.6) | 2 (6.5) | 6 (11.5) | |
| Center #2 | 12 (14.5) | 6 (19.4) | 6 (11.5) | |
| Center #3 | 15 (18.1) | 3 (9.7) | 12 (23.1) | |
| Center #4 | 6 (7.2) | 3 (9.7) | 3 (5.8) | |
| Center #5 | 8 (9.6) | 3 (9.7) | 5 (9.6) | |
| Center #6 | 8 (9.6) | 3 (9.7) | 5 (9.6) | |
| Center #7 | 1 (1.2) | 1 (3.2) | 0 (0.0) | |
| Center #8 | 7 (8.4) | 4 (12.9) | 3 (5.8) | |
| Center #9 | 18 (21.7) | 6 (19.4) | 12 (23.1) | |
| Age, years. Mean (±SD) | 63.9 (12.5) | 65.5 (12.5) | 63.0 (12.5) | 0.38 |
| Time since stroke onset, Mean (±SD) | 136.1 (95.1) | 118.4 (86.6) | 146.7 (99.1) | 0.18 |
| Type of stroke, No. (%) | 0.87 | |||
| Hemorrhagic | 25 (30.1) | 9 (29.0) | 16 (30.8) | |
| Ischemic | 58 (69.9) | 22 (71.0) | 36 (69.2) | |
| Lesion side, No. (%) | 0.93 | |||
| Right | 45 (54.2) | 17 (54.8) | 28 (53.8) | |
| Left | 38 (45.8) | 14 (45.2) | 24 (46.2) | |
| Hospital regimen, No. (%) | 0.56 | |||
| Outpatient | 33 (39.8) | 10 (32.3) | 23 (44.2) | |
| Day hospital | 10 (12.0) | 4 (12.9) | 6 (11.5) | |
| Inpatient | 40 (48.2) | 17 (54.8) | 23 (44.2) | |
| Injection technique, No. (%) | 0.56 | |||
| Ultrasound-guided | 54 (65.1) | 18 (58.1) | 36 (69.2) | |
| Electrical stimulation | 11 (13.3) | 5 (16.1) | 6 (11.5) | |
| Manual needle placement | 18 (21.7) | 8 (25.8) | 10 (19.2) | |
| Vial dilution, No. (%) | 0.67 | |||
| 1 mL | 11 (13.3) | 5 (16.1) | 6 (11.5) | |
| 1.5 mL | 5 (6.0) | 3 (9.7) | 2 (3.8) | |
| 2 mL | 56 (67.5) | 19 (61.3) | 37 (71.2) | |
| 2.5 mL | 11 (13.3) | 4 (12.9) | 7 (13.5) |
| Muscles | Overall | Women (n = 31) | Men (n = 52) | p-Value * |
|---|---|---|---|---|
| Shoulder External Rotators, Median (IQR) | 1.00 (2.00) | 1.00 (2.00) | 1.00 (2.00) | 0.27 |
| Shoulder Abductors, Median (IQR) | 2.00 (2.00) | 1.00 (2.00) | 2.00 (1.00) | 0.20 |
| Elbow Extensors, Median (IQR) | 1.00 (2.00) | 1.00 (2.00) | 2.00 (3.00) | 0.04 |
| Elbow Flexors, Median (IQR) | 2.00 (2.00) | 1.00 (2.00) | 2.00 (3.00) | 0.06 |
| Forearm Supinators, Median (IQR) | 1.00 (2.00) | 0.00 (1.00) | 1.00 (2.25) | 0.08 |
| Wrist Extensors, Median (IQR) | 0.00 (2.00) | 0.00 (1.00) | 1.00 (2.00) | 0.08 |
| Finger extensors, Median (IQR) | 0.00 (2.00) | 0.00 (1.00) | 1.00 (2.00) | 0.05 |
| Hip Extensors, Median (IQR) | 3.00 (1.00) | 2.00 (1.00) | 3.00 (1.00) | 0.14 |
| Hip External Rotators, Median (IQR) | 2.00 (1.00) | 2.00 (2.00) | 3.00 (1.25) | 0.13 |
| Hip Abductors, Median (IQR) | 2.00 (2.00) | 2.00 (1.75) | 2.50 (2.00) | 0.22 |
| Knee Extensors, Median (IQR) | 3.00 (2.00) | 3.00 (1.75) | 3.00 (2.00) | 0.32 |
| Knee Flexors, Median (IQR) | 3.00 (2.00) | 3.00 (1.00) | 3.00 (2.00) | 0.33 |
| Ankle Invertors, Median (IQR) | 1.00 (3.00) | 1.00 (2.00) | 2.00 (2.25) | 0.16 |
| Ankle Dorsiflexors, Median (IQR) | 2.00 (3.00) | 1.00 (2.00) | 2.00 (2.00) | 0.13 |
| Ankle Evertors, Median (IQR) | 1.00 (2.00) | 0.50 (1.75) | 1.50 (2.00) | 0.03 |
| 0 Weeks | 4 Weeks | 12 Weeks | 24 Weeks | p-Value * | |
|---|---|---|---|---|---|
| UL, Median (IQR) | 8.00 (9.50) | 11.50 (15.00) | 14.00 (17.00) | 16.00 (16.20) | 0.001 |
| Wrist, Median (IQR) | 0.00 (3.00) | 0.00 (2.00) | 0.00 (4.00) | 0.00 (4.00) | 0.023 |
| Hand, Median (IQR) | 0.00 (5.00) | 0.00 (5.00) | 0.00 (7.00) | 0.00 (7.00) | 0.283 |
| UL Speed coordination, Median (IQR) | 1.00 (3.00) | 2.00 (3.00) | 2.00 (4.00) | 2.00 (4.00) | 0.045 |
| UL Motor function, Median (IQR) | 9.00 (20.50) | 12.00 (25.80) | 18.00 (28.00) | 18.00 (28.00) | 0.016 |
| UL Sensation, Median (IQR) | 10.00 (5.00) | 10.50 (4.00) | 10.50 (4.00) | 11.00 (4.00) | 0.218 |
| UL Passive motility, Median (IQR) | 19.00 (7.50) | 20.00 (6.00) | 20.00 (7.00) | 19.50 (7.00) | 0.358 |
| UL Pain, Median (IQR) | 16.00 (10.50) | 20.00 (10.00) | 20.00 (8.00) | 20.00 (7.00) | 0.007 |
| LL, Median (IQR) | 13.00 (7.00) | 15.00 (8.00) | 16.00 (10.50) | 16.00 (11.00) | 0.002 |
| LL Speed coordination, Median (IQR) | 2.00 (3.00) | 3.00 (2.00) | 3.00 (2.00) | 3.00 (2.75) | <0.001 |
| LL Motor function, Median (IQR) | 15.00 (9.00) | 17.00 (7.00) | 18.00 (8.00) | 19.00 (10.00) | <0.001 |
| LL Sensation, Median (IQR) | 10.00 (6.00) | 11.00 (3.00) | 11.00 (4.00) | 12.00 (3.00) | 0.049 |
| LL Passive motility, Median (IQR) | 18.00 (4.00) | 18.00 (4.00) | 18.00 (3.50) | 18.00 (3.00) | 0.192 |
| LL Pain, Median (IQR) | 20.00 (2.00) | 20.00 (2.00) | 20.00 (0.00) | 20.00 (0.80) | 0.291 |
| Muscles | Total n = 1167 (100%) | Women n = 406 (100%) | Men n = 761 (100%) | p-Value * |
|---|---|---|---|---|
| Shoulder Adductors | n = 76 (6.4%) | n = 32 (7.6%) | n = 44 (5.7%) | |
| Elbow Extensors | n = 32 (2.7%) | n = 0 (0.0%) | n = 32 (4.2%) | |
| Finger Flexors | n = 192 (16.2%) | n = 68 (16.2%) | n = 124 (16.1%) | |
| Toe Flexors | n = 36 (3.0%) | n = 16 (3.8%) | n = 20 (2.6%) | |
| Elbow Flexors | n = 184 (15.5%) | n = 72 (17.1%) | n = 112 (14.6%) | |
| Thumb Flexors | n = 80 (6.7%) | n = 24 (5.7%) | n = 56 (7.3%) | 0.003 |
| Wrist Flexors | n = 204 (17.2%) | n = 68 (16.2%) | n = 136 (17.7%) | |
| Ankle Plantiflexors | n = 132 (11.1%) | n = 56 (13.3%) | n = 76 (9.9%) | |
| Forearm Pronators | n = 112 (9.4%) | n = 36 (8.6%) | n = 76 (9.9%) | |
| Ankle Invertors | n = 64 (5.4%) | n = 24 (5.7%) | n = 40 (5.2%) | |
| Others | n = 76 (6.4%) | n = 24 (5.7%) | n = 52 (6.8%) |
| Predictors | Odds Ratio | 95% CI | p-Value |
|---|---|---|---|
| Follow-up (4 weeks) | 0.05 | 0.03–0.09 | <0.001 |
| Follow-up (12 weeks) | 0.06 | 0.04–0.11 | <0.001 |
| Follow-up (24 weeks) | 0.24 | 0.14–0.41 | <0.001 |
| TSO (>90 days) | 1.71 | 0.74–3.98 | 0.210 |
| Age groups (60,70) | 0.73 | 0.32–1.64 | 0.444 |
| Age group (70,100) | 0.35 | 0.15–0.80 | 0.013 |
| Sex (Male) | 1.18 | 0.58–2.40 | 0.643 |
| Vial dilution (mL) | 0.12 | 0.05–0.30 | <0.001 |
| Follow-up (4 weeks) * TSO (>90 days) | 2.05 | 1.02–4.13 | 0.044 |
| Follow-up (12 weeks) * TSO (>90 days) | 2.87 | 1.46–5.65 | 0.002 |
| Follow-up (24 weeks) * TSO (>90 days) | 1.12 | 0.56–2.26 | 0.747 |
| Observations/Subjects | 1167/83 | ||
| Marginal R2/Conditional R2 | 0.266/0.601 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Picelli, A.; Santamato, A.; Cosma, M.; Baricich, A.; Chisari, C.; Millevolte, M.; Prete, C.D.; Mazzù, I.; Girardi, P.; Smania, N. Early Botulinum Toxin Type A Injection for Post-Stroke Spasticity: A Longitudinal Cohort Study. Toxins 2021, 13, 374. https://doi.org/10.3390/toxins13060374
Picelli A, Santamato A, Cosma M, Baricich A, Chisari C, Millevolte M, Prete CD, Mazzù I, Girardi P, Smania N. Early Botulinum Toxin Type A Injection for Post-Stroke Spasticity: A Longitudinal Cohort Study. Toxins. 2021; 13(6):374. https://doi.org/10.3390/toxins13060374
Chicago/Turabian StylePicelli, Alessandro, Andrea Santamato, Michela Cosma, Alessio Baricich, Carmelo Chisari, Marzia Millevolte, Cristina Del Prete, Ilenia Mazzù, Paolo Girardi, and Nicola Smania. 2021. "Early Botulinum Toxin Type A Injection for Post-Stroke Spasticity: A Longitudinal Cohort Study" Toxins 13, no. 6: 374. https://doi.org/10.3390/toxins13060374
APA StylePicelli, A., Santamato, A., Cosma, M., Baricich, A., Chisari, C., Millevolte, M., Prete, C. D., Mazzù, I., Girardi, P., & Smania, N. (2021). Early Botulinum Toxin Type A Injection for Post-Stroke Spasticity: A Longitudinal Cohort Study. Toxins, 13(6), 374. https://doi.org/10.3390/toxins13060374








