Therapeutic Effects of Urethral Sphincter Botulinum Toxin A Injection on Dysfunctional Voiding with Different Videourodynamic Characteristics in Non-Neurogenic Women
Abstract
1. Introduction
2. Results
3. Discussion
4. Conclusions
5. Materials and Methods
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Blaivas, J.G. Pathophysiology of lower urinary tract dysfunction. Urol. Clin. N. Am. 1985, 12, 215–224. [Google Scholar]
- Carson, C.C.; Segura, J.W.; Osborne, D.M. Evaluation and treatment of the female urethral syndrome. J. Urol. 1980, 124, 609–610. [Google Scholar] [CrossRef]
- Massey, J.A.; Abrams, P.H. Obstructed voiding in the female. Br. J. Urol. 1988, 61, 36–39. [Google Scholar] [CrossRef]
- Nitti, V.W.; Fiske, J. Cystometrogram versus cystometrogram plus voiding pressure-flow studies in women with lower urinary tract symptoms. J. Urol. 1999, 161, 201. [Google Scholar] [CrossRef]
- Groutz, A.; Blaivas, J.G.; Pies, C.; Sassone, A.M. Learned voiding dysfunction (non-neurogenic, neurogenic bladder) among adults. Neurourol. Urodyn. 2001, 20, 259–268. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, S.M.; Lin, H.H.; Kuo, H.C. Videourodynamic Studies of Women with Voiding Dysfunction. Sci. Rep. 2017, 7, 6845. [Google Scholar] [CrossRef] [PubMed]
- Chuang, F.C.; Huang, K.H.; Kuo, H.C. Lower urinary tract symptoms and vdeo urodynamic characteristics of women with clinically unsuspected bladder outlet obstruction. Low Urin. Tract Symptoms 2013, 5, 23–27. [Google Scholar] [CrossRef]
- Chen, Y.C.; Kuo, H.C. Clinical and video urodynamic characteristics of adult women with dysfunctional voiding. J. Formosan Med. Assoc. 2014, 113, 161–165. [Google Scholar] [CrossRef]
- Haylen, B.T.; de Ridder, D.; Freeman, R.M.; Swift, S.E.; Berghmans, B.; Lee, J.; Monga, A.; Petri, E.; Rizk, D.E.; Sand, P.K.; et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol. Urodyn. 2010, 29, 4–20. [Google Scholar] [CrossRef] [PubMed]
- Allen, T.D.; Bright, T.C., 3rd. Urodynamic patterns in children with dysfunctional voiding problems. J. Urol. 1978, 119, 247–249. [Google Scholar] [CrossRef]
- Minardi, D.; d’Anzeo, G.; Parri, G.; Polito, M., Jr.; Piergallina, M.; El Asmar, Z.; Marchetti, M.; Muzzonigro, G. The role of uroflowmetry biofeedback and biofeedback training of the pelvic floor muscles in the treatment of recurrent urinary tract infections in women with dysfunctional voiding: A randomized controlled prospective study. Urology 2010, 75, 1299–1304. [Google Scholar] [CrossRef] [PubMed]
- Espuña-Pons, M.; Cardozo, L.; Chapple, C.; Sievert, K.D.; van Kerrebroeck, P.; Kirby, M.G. Overactive bladder symptoms and voiding dysfunction in neurologically normal women. Neurourol. Urodyn. 2012, 31, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Lo, C.W.; Wu, M.Y.; Yang, S.S.; Jaw, F.S.; Chang, S.J. Comparing the Efficacy of OnabotulinumtoxinA, Sacral Neuromodulation, and Peripheral Tibial Nerve Stimulation as Third Line Treatment for the Management of Overactive Bladder Symptoms in Adults: Systematic Review and Network Meta-Analysis. Toxins 2020, 12, 128. [Google Scholar] [CrossRef]
- Jiang, Y.H.; Chen, S.F.; Jhang, J.F.; Kuo, H.C. Therapeutic effect of urethral sphincter onabotulinumtoxinA injection for urethral sphincter hyperactivity. Neurourol. Urodyn. 2018, 37, 2651–2657. [Google Scholar] [CrossRef] [PubMed]
- Kao, Y.L.; Huang, K.H.; Kuo, H.C.; Ou, Y.C. The Therapeutic Effects and Pathophysiology of Botulinum Toxin A on Voiding Dysfunction Due to Urethral Sphincter Dysfunction. Toxins 2019, 11, 728. [Google Scholar] [CrossRef]
- Kuo, H.C. Dysfunctional voiding in women with lower urinary tract symptoms. Tzu Chi Med. J. 2000, 12, 217–223. [Google Scholar]
- Kuo, H.C. Botulinum A toxin urethral injection for the treatment of lower urinary tract dysfunction. J. Urol. 2003, 170, 1908–1912. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, W.; Firlit, C.F.; Schoenberg, H.W. The female urethral syndrome: External sphincter spasm as etiology. J. Urol. 1980, 124, 48–49. [Google Scholar] [CrossRef]
- Deindl, F.M.; Vodusek, D.B.; Bischoff, C.H.; Hofmann, R.; Hartung, R. Dysfunctional voiding in women: Which muscles are responsible? Br. J. Urol. 1998, 82, 814–819. [Google Scholar] [CrossRef]
- Hinman, F., Jr. Nonneurogenic neurogenic bladder (the Hinmann syndrome)—15 years later. J. Urol. 1986, 136, 769–777. [Google Scholar] [CrossRef]
- De Paepe, H.; Renson, C.; Van Laecke, E.; Raes, A.; Vande Walle, J.; Hoebeke, P. Pelvic-floor therapy and toilet training in young children with dysfunctional voiding and obstipation. BJU Int. 2000, 85, 889–893. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Lee, K.S.; Choo, M.S.; Kim, J.C.; Lee, J.G.; Seo, J.T.; Lee, J.Z.; Lee, J.Y.; Oh, S.J.; Na, Y.G. Efficacy of an Alpha-Blocker for the Treatment of Nonneurogenic Voiding Dysfunction in Women: An 8-Week, Randomized, Double-Blind, Placebo-Controlled Trial. Int. Neurourol. J. 2018, 22, 30–40. [Google Scholar] [CrossRef] [PubMed]
- McGuire, E.J.; Savastano, J.A. Urodynamic studies in enuresis and the non-neurogenic neurogenic bladder. J. Urol. 1984, 132, 29–302. [Google Scholar] [CrossRef]
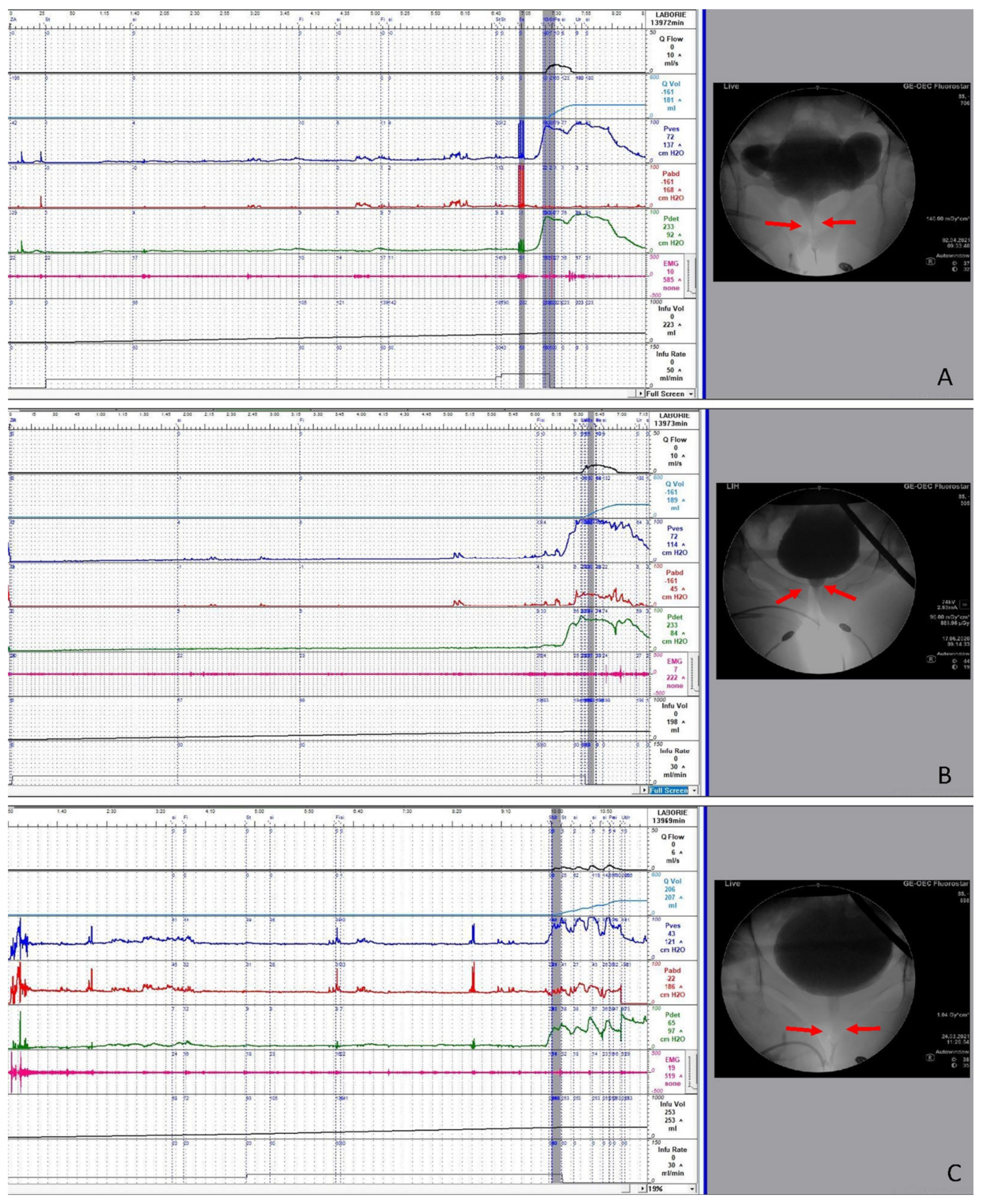
- Peng, C.H.; Chen, S.F.; Kuo, H.C. Videourodynamic analysis of the urethral sphincter overactivity and the poor relaxing pelvic floor muscles in women with voiding dysfunction. Neurourol. Urodyn. 2017, 36, 2169–2175. [Google Scholar] [CrossRef] [PubMed]
- Chow, P.M.; Hsiao, S.M.; Kuo, H.C. Obstructive patterns in videourodynamic studies predict responses of female dysfunctional voiding treated with or without urethral botulinum toxin injection: A long-term follow-up study. Int. Urogynecol. J. 2020, 31, 2557–2564. [Google Scholar] [CrossRef]
- Fam, B.A.; Sarkarati, M.; Yalla, S.V. Spinal cord injury. In Neurourology and Urodynamics; Yalla, S.V., McGuire, E.J., Elbadawi., A., Eds.; Macmillan Publishing Company: New York, NY, USA, 1988; pp. 291–302. [Google Scholar]
- Kuo, T.L.C.; Ng, L.G.; Chapple, C.R. Pelvic floor spasm as a cause of voiding dysfunction. Curr. Opin. Urol. 2015, 25, 311–316. [Google Scholar] [CrossRef]
| Parameter | Successful (n = 55) | Failure (n = 26) | p-Value |
|---|---|---|---|
| Age | 59.7 ± 13.9 | 60.4 ± 19.3 | 0.857 |
| FSF (mL) | 146.6 ± 70.6 | 115.0 ± 52.8 | 0.046 |
| FS (mL) | 216.2 ± 86.4 | 184.9 ± 68.3 | 0.109 |
| US (mL) | 254.7 ± 99.3 | 215.5 ± 84.2 | 0.086 |
| Pdet.Qmax (cmH2O) | 59.0 ± 44.5 | 50.8 ± 35.2 | 0.414 |
| Compliance | 71.0 ± 66.6 | 58.9 ± 67.2 | 0.451 |
| Qmax (mL/s) | 8.06 ± 5.77 | 6.88 ± 4.09 | 0.352 |
| Volume (mL) | 158.3 ± 110.8 | 122.9 ± 78.7 | 0.104 |
| PVR (mL) | 179.8 ± 141.7 | 167.7 ± 101.9 | 0.698 |
| CBC (mL) | 338.1 ± 137.3 | 290.6 ± 105.1 | 0.123 |
| VE | 48.5 ± 32.5 | 44.8 ± 28.3 | 0.614 |
| BOOI | 42.8 ± 47.0 | 37.0 ± 35.7 | 0.578 |
| DO | 42(76.4%) | 18 (69.2%) | 0.629 |
| DV subtype | 0.376 | ||
| BND + DV | 4 (7.3%) | 3 (11.5%) | |
| Mid-urethra DV | 40 (72.7%) | 15 (57.7%) | |
| Distal urethra DV | 11 (20%) | 8 (30.8%) | |
| CNS lesion | 13 (24.1%) | 2 (7.7%) | 0.125 |
| Storage LUTS | 37 (67.3%) | 20 (76.9%) | 0.375 |
| Voiding LUTS | 49 (89.1%) | 22 (84.6%) | 0.719 |
| Parameter | BND + DV (n = 7) | Mid-Urethra DV (n = 55) | Distal Urethra DV (n = 19) | p Value |
|---|---|---|---|---|
| Age | 58.3 ± 20.5 | 57.1 ± 15.4 | 68.7 ± 11.6 | 0.018 |
| FSF (mL) | 140.9 ± 75.1 | 137.7 ± 72.1 | 131.3 ± 47.9 | 0.923 |
| FS (mL) | 215.7 ± 117.2 | 196.4 ± 80.5 | 230.7 ± 69.6 | 0.279 |
| US (mL) | 265.4 ± 109.1 | 226.4 ± 92.4 | 279.1 ± 94.5 | 0.093 |
| Pdet.Qmax (cmH2O) | 86.9 ± 60.6 | 61.8 ± 41.2 | 29.4 ± 14.3 | 0.001 |
| Compliance | 65.7 ± 55.7 | 61.7 ± 64.7 | 83.2 ± 75.9 | 0.483 |
| Qmax (mL/s) | 5.7 ± 4.0 | 7.9 ± 5.6 | 7.7 ± 4.8 | 0.588 |
| Volume (mL) | 98.1 ± 55.6 | 155.6 ± 112.4 | 139.8 ± 80.8 | 0.359 |
| PVR (mL) | 211.4 ± 159.9 | 160.0 ± 134.4 | 209.0 ± 98.4 | 0.277 |
| CBC (mL) | 309.6 ± 126.3 | 315.6 ± 129.1 | 348.8 ± 133.7 | 0.608 |
| VE | 0.407 ± 0.322 | 0.513 ± 0.337 | 0.384 ± 0.196 | 0.252 |
| BOOI | 75.4 ± 62.4 | 45.9 ± 43.7 | 13.9 ± 10.2 | 0.001 |
| DO | 6 (85.7%) | 41 (74.5%) | 9 (47.4%) | 0.063 |
| CNS lesion | 0 | 11 (20.4%) | 4 (21.1%) | 0.539 |
| Storage LUTS | 5 (71.4%) | 40 (72.7%) | 12 (63.2%) | 0.798 |
| Voiding LUTS | 6 (85.7%) | 48 (87.3) | 17 (89.5%) | 1.000 |
| Successful outcome | 4 (57.1%) | 40 (72.7%) | 11 (57.9%) | 0.376 |
| GRA= +3 | 0 | 12 (21.8%) | 3 (15.8%) | |
| GRA= +2 | 2 (28.6%) | 18 (32.7%) | 5 (26.3%) | |
| GRA= +1 | 2 (28.6%) | 10 (18.2%) | 3 (15.8%) | |
| GRA= 0 | 3 (42.9%) | 12 (21.8%) | 8 (42.1%) | |
| GRA= −1 | 0 | 3 (5.5%) | 0 |
| Total DV (n = 81) | BND + DV (n = 7) | Mid-Urethra DV (n = 55) | Distal Urethra DV (n = 19) | |||||
|---|---|---|---|---|---|---|---|---|
| BL | FU | BL | FU | BL | FU | BL | FU | |
| Storage LUTS | 57 (70.4%) | 41 (50.6%) | 5 (71.4%) | 3 (42.9%) | 40 (72.7%) | 30 (54.5%) | 12 (63.2%) | 8 (42.1%) |
| Frequency/urgency/nocturia | 19 | 17 | 1 | 1 | 10 | 10 | 8 | 6 |
| Urgency incontinence | 38 | 24 | 4 | 2 | 30 | 20 | 4 | 2 |
| Voiding LUTS | 71 (87.7%) | 34 (42.0%) | 6 (85.7%) | 2 (28.6%) | 48 (87.3%) | 21 (38.2%) | 17 (89.5%) | 11 (57.9%) |
| Difficult urination | 67 | 34 | 5 | 2 | 45 | 21 | 17 | 11 |
| Urinary retention | 4 | 0 | 1 | 0 | 3 | 0 | 0 | 0 |
| Painful LUTS | 11 (13.6%) | 4 (4.9%) | 1 (14.3%) | 0 (0%) | 5 (9.1%) | 2 (3.6%) | 0 | 0 |
| Bladder pain | 6 | 2 | 1 | 0 | 5 | 2 | 0 | 0 |
| Miction pain | 5 | 2 | 2 | 1 | 3 | 1 | 0 | 0 |
| Parameter | Successful (n = 55) | Failure (n = 26) | p | |
|---|---|---|---|---|
| FSF (mL) | BL FU | 152.3 ± 79.5 150.4 ± 94.3 | 119.2 ± 52.4 131.7 ± 105.6 | 0.652 |
| FS (mL) | BL FU | 225.2 ± 97.0 206.9 ± 102.8 | 195.4 ± 67.7 173.1 ± 125.9 | 0.910 |
| US (mL) | BL FU | 257.8 ± 107.6 232.1 ± 119.9 | 226.0 ± 82.6 192.8 ± 136.3 | 0.839 |
| Pdet.Qmax (cmH2O) | BL FU | 59.9 ± 38.8 44.4 ± 33.6 * | 51.2 ± 36.0 36.2 ± 35.7 | 0.959 |
| Compliance | BL FU | 60.9 ± 52.8 64.2 ± 63.8 | 69.6 ± 84.7 57.3 ± 61.2 | 0.526 |
| Qmax (mL/s) | BL FU | 8.51 ± 6.21 8.83 ± 8.19 | 7.53 ± 4.72 4.85 ± 4.33 | 0.254 |
| Volume (mL) | BL FU | 146.2 ± 108.2 160.1 ± 140.7 | 126.5 ± 87.1 82.9 ± 73.4 | 0.185 |
| PVR (mL) | BL FU | 206.0 ± 137.5 132.6 ± 156.1 * | 195.3 ± 101.6 243.3 ± 239.2 | 0.032 |
| CBC (mL) | BL FU | 352.2 ± 145.2 292.6 ± 136.9 * | 321.9 ± 116.6 326.2 ± 215.4 | 0.185 |
| Voiding efficiency | BL FU | 42.7 ± 28.3 58.2 ± 36.8 * | 40.3 ± 27.4 34.3 ± 32.4 | 0.057 |
| BOOI | BL FU | 42.9 ± 41.8 26.7 ± 39.5 * | 36.1 ± 37.4 26.5 ± 32.8 | 0.630 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiang, Y.-H.; Lee, C.-L.; Chen, S.-F.; Kuo, H.-C. Therapeutic Effects of Urethral Sphincter Botulinum Toxin A Injection on Dysfunctional Voiding with Different Videourodynamic Characteristics in Non-Neurogenic Women. Toxins 2021, 13, 362. https://doi.org/10.3390/toxins13050362
Jiang Y-H, Lee C-L, Chen S-F, Kuo H-C. Therapeutic Effects of Urethral Sphincter Botulinum Toxin A Injection on Dysfunctional Voiding with Different Videourodynamic Characteristics in Non-Neurogenic Women. Toxins. 2021; 13(5):362. https://doi.org/10.3390/toxins13050362
Chicago/Turabian StyleJiang, Yuan-Hong, Cheng-Ling Lee, Sheng-Fu Chen, and Hann-Chorng Kuo. 2021. "Therapeutic Effects of Urethral Sphincter Botulinum Toxin A Injection on Dysfunctional Voiding with Different Videourodynamic Characteristics in Non-Neurogenic Women" Toxins 13, no. 5: 362. https://doi.org/10.3390/toxins13050362
APA StyleJiang, Y.-H., Lee, C.-L., Chen, S.-F., & Kuo, H.-C. (2021). Therapeutic Effects of Urethral Sphincter Botulinum Toxin A Injection on Dysfunctional Voiding with Different Videourodynamic Characteristics in Non-Neurogenic Women. Toxins, 13(5), 362. https://doi.org/10.3390/toxins13050362






