A Monoclonal Antibody Combination against both Serotypes A and B Botulinum Toxin Prevents Inhalational Botulism in a Guinea Pig Model
Abstract
1. Introduction
2. Results
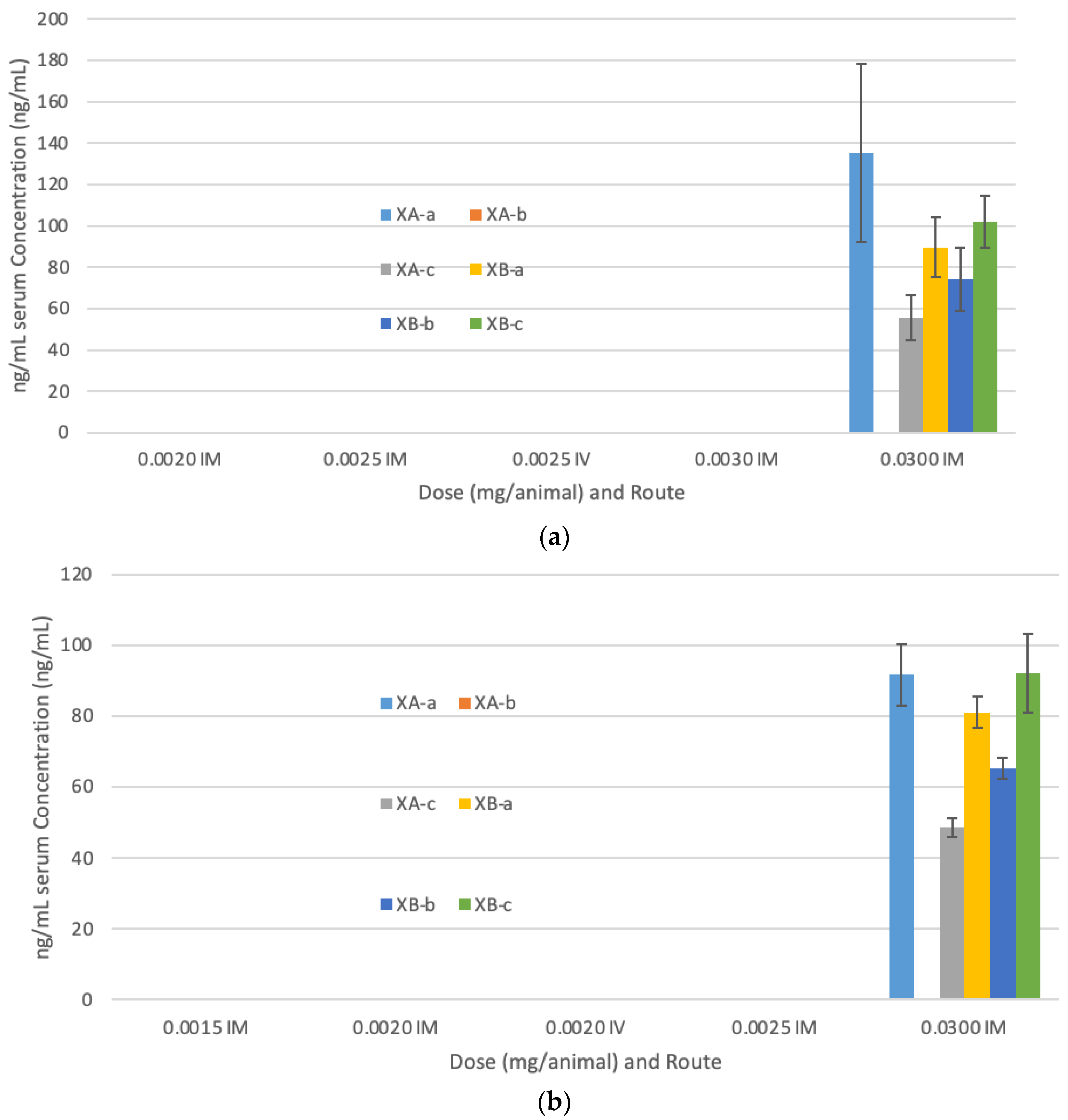
2.1. Evaluation of Dose and Route of Administration of G03-52-01 Neutralizing Antibody Concentration (NAC) in Guinea Pigs
2.2. G03-52-01 Protects Guinea Pigs against Lethal Aerosol Challenge with BoNT/A and BoNT/B
3. Discussion
4. Conclusions
5. Materials and Methods
5.1. Monoclonal Antibodies
5.2. BoNT Challenge Material
5.3. Control Samples
5.4. Pharmacokinetics
5.4.1. Electrochemiluminescence
5.4.2. ELISA
5.5. Measurement of Neutralizing Antibody Concentration (NAC)
5.6. Animal Challenge Studies
5.7. Aerosol Exposure System
5.8. Measurement of BoNT Challenge Concentrations
5.9. Statistical Methods
Author Contributions
Funding
Conflicts of Interest
References
- Lacy, D.B.; Stevens, R.C. Sequence homology and structural analysis of the clostridial neurotoxins. J. Mol. Biol. 1999, 291, 1091–1104. [Google Scholar] [CrossRef] [PubMed]
- Moller, V.; Scheibel, I. Preliminary report on the isolation of an apparently new type of CI. botulinum. Acta Pathol. Microbiol. Scand. 1960, 48, 80. [Google Scholar] [CrossRef] [PubMed]
- Sobel, J. Botulism. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2005, 41, 1167–1173. [Google Scholar] [CrossRef]
- Dembek, Z.F.; Smith, L.A.; Rusnak, J.M. Botulism: Cause, effects, diagnosis, clinical and laboratory identification, and treatment modalities. Disaster Med. Public Health Prep. 2007, 1, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Hatheway, C.L. Botulism: The present status of the disease. Curr. Top. Microbiol. Immunol. 1995, 195, 55–75. [Google Scholar]
- Bai, L.; Peng, X.; Liu, Y.; Sun, Y.; Wang, X.; Wang, X.; Lin, G.; Zhang, P.; Wan, K.; Qiu, Z. Clinical analysis of 86 botulism cases caused by cosmetic injection of botulinum toxin (BoNT). Medicine 2018, 97, e10659. [Google Scholar] [CrossRef]
- Chertow, D.S.; Tan, E.T.; Maslanka, S.E.; Schulte, J.; Bresnitz, E.A.; Weisman, R.S.; Bernstein, J.; Marcus, S.M.; Kumar, S.; Malecki, J.; et al. Botulism in 4 adults following cosmetic injections with an unlicensed, highly concentrated botulinum preparation. JAMA 2006, 296, 2476–2479. [Google Scholar] [CrossRef]
- Holzer, E. Botulism caused by inhalation. Med. Klin. 1962, 57, 1735–1738. [Google Scholar]
- Park, J.B.; Simpson, L.L. Inhalational poisoning by botulinum toxin and inhalation vaccination with its heavy-chain component. Infect. Immun. 2003, 71, 1147–1154. [Google Scholar] [CrossRef]
- Sanford, D.C.; Barnewall, R.E.; Vassar, M.L.; Niemuth, N.; Metcalfe, K.; House, R.V.; Henderson, I.; Shearer, J.D. Inhalational botulism in rhesus macaques exposed to botulinum neurotoxin complex serotypes A1 and B1. Clin. Vaccine Immunol. CVI 2010, 17, 1293–1304. [Google Scholar] [CrossRef]
- Arnon, S.S.; Schechter, R.; Inglesby, T.V.; Henderson, D.A.; Bartlett, J.G.; Ascher, M.S.; Eitzen, E.; Fine, A.D.; Hauer, J.; Layton, M.; et al. Botulinum toxin as a biological weapon: Medical and public health management. JAMA 2001, 285, 1059–1070. [Google Scholar] [CrossRef]
- Pirazzini, M.; Rossetto, O.; Eleopra, R.; Montecucco, C. Botulinum Neurotoxins: Biology, Pharmacology, and Toxicology. Pharmacol. Rev. 2017, 69, 200–235. [Google Scholar] [CrossRef]
- Al-Saleem, F.H.; Nasser, Z.; Olson, R.M.; Cao, L.; Simpson, L.L. Identification of the factors that govern the ability of therapeutic antibodies to provide postchallenge protection against botulinum toxin: A model for assessing postchallenge efficacy of medical countermeasures against agents of bioterrorism and biological warfare. J. Pharmacol. Exp. Ther. 2011, 338, 503–517. [Google Scholar] [CrossRef] [PubMed]
- Al-Saleem, F.H.; Ancharski, D.M.; Joshi, S.G.; Elias, M.; Singh, A.; Nasser, Z.; Simpson, L.L. Analysis of the mechanisms that underlie absorption of botulinum toxin by the inhalation route. Infect. Immun. 2012, 80, 4133–4142. [Google Scholar] [CrossRef] [PubMed]
- Nowakowski, A.; Wang, C.; Powers, D.B.; Amersdorfer, P.; Smith, T.J.; Montgomery, V.A.; Sheridan, R.; Blake, R.; Smith, L.A.; Marks, J.D. Potent neutralization of botulinum neurotoxin by recombinant oligoclonal antibody. Proc. Natl. Acad. Sci. USA 2002, 99, 11346–11350. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Rodriguez, C.; Razai, A.; Geren, I.N.; Lou, J.; Conrad, F.; Wen, W.H.; Farr-Jones, S.; Smith, T.J.; Brown, J.L.; Skerry, J.C.; et al. A Three Monoclonal Antibody Combination Potently Neutralizes Multiple Botulinum Neurotoxin Serotype E Subtypes. Toxins 2018, 10, 105. [Google Scholar] [CrossRef] [PubMed]
- Rossetto, O.; Montecucco, C. Tables of Toxicity of Botulinum and Tetanus Neurotoxins. Toxins 2019, 11, 686. [Google Scholar] [CrossRef]
- Williamson, C.H.; Sahl, J.W.; Smith, T.J.; Xie, G.; Foley, B.T.; Smith, L.A.; Fernandez, R.A.; Lindstrom, M.; Korkeala, H.; Keim, P.; et al. Comparative genomic analyses reveal broad diversity in botulinum-toxin-producing Clostridia. BMC Genom. 2016, 17, 180. [Google Scholar] [CrossRef]
- Tehran, D.A.; Pirazzini, M. Novel Botulinum Neurotoxins: Exploring Underneath the Iceberg Tip. Toxins 2018, 10, 190. [Google Scholar] [CrossRef]
- Mansfield, M.J.; Doxey, A.C. Genomic insights into the evolution and ecology of botulinum neurotoxins. Pathog. Dis. 2018, 76. [Google Scholar] [CrossRef]
- Zhang, S.; Masuyer, G.; Zhang, J.; Shen, Y.; Lundin, D.; Henriksson, L.; Miyashita, S.I.; Martinez-Carranza, M.; Dong, M.; Stenmark, P. Identification and characterization of a novel botulinum neurotoxin. Nat. Commun. 2017, 8, 14130. [Google Scholar] [CrossRef]
- Jankovic, J.; Brin, M.F. Therapeutic uses of botulinum toxin. N. Engl. J. Med. 1991, 324, 1186–1194. [Google Scholar] [CrossRef] [PubMed]
- Schantz, E.J.; Johnson, E.A. Botulinum toxin: The story of its development for the treatment of human disease. Perspect. Biol. Med. 1997, 40, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Cather, J.C.; Cather, J.C.; Menter, A. Update on botulinum toxin for facial aesthetics. Dermatol. Clin. 2002, 20, 749–761. [Google Scholar] [CrossRef]
- Simpson, L.L.; Maksymowych, A.B.; Kiyatkin, N. Botulinum toxin as a carrier for oral vaccines. Cell. Mol. Life Sci. CMLS 1999, 56, 47–61. [Google Scholar] [CrossRef] [PubMed]
- Zdanovskaia, M.V.; Los, G.; Zdanovsky, A.G. Recombinant derivatives of clostridial neurotoxins as delivery vehicles for proteins and small organic molecules. J. Protein Chem. 2000, 19, 699–707. [Google Scholar] [CrossRef] [PubMed]
- CDC. Available online: https://www.selectagents.gov/sat/list.htm?CDC_AA_refVal=https%3A%2F%2Fwww.selectagents.gov%2FSelectAgentsandToxinsList.html (accessed on 25 October 2020).
- Coleman, K.; Zilinskas, R.A. Fake botox, real threat. Sci. Am. 2010, 302, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Lim, E.C.; Seet, R.C. Use of botulinum toxin in the neurology clinic. Nat. Rev. Neurol. 2010, 6, 624–636. [Google Scholar] [CrossRef] [PubMed]
- CDC. Notice of CDC’s discontinuation of investigational pentavalent (ABCDE) botulinum toxoid vaccine for workers at risk for occupational exposure to botulinum toxins. Mmwr. Morb. Mortal. Wkly. Rep 2011, 60, 1454. [Google Scholar]
- Siegel, L.S. Human immune response to botulinum pentavalent (ABCDE) toxoid determined by a neutralization test and by an enzyme-linked immunosorbent assay. J. Clin. Microbiol. 1988, 26, 2351–2356. [Google Scholar] [CrossRef]
- Webb, R.P.; Smith, T.J.; Smith, L.A.; Wright, P.M.; Guernieri, R.L.; Brown, J.L.; Skerry, J.C. Recombinant Botulinum Neurotoxin Hc Subunit (BoNT Hc) and Catalytically Inactive Clostridium botulinum Holoproteins (ciBoNT HPs) as Vaccine Candidates for the Prevention of Botulism. Toxins 2017, 9, 269. [Google Scholar] [CrossRef]
- Webb, R.P.; Smith, L.A. What next for botulism vaccine development? Expert Rev. Vaccines 2013, 12, 481–492. [Google Scholar] [CrossRef]
- Hart, M.K.; Saviolakis, G.A.; Welkos, S.L.; House, R.V. Advanced Development of the rF1V and rBV A/B Vaccines: Progress and Challenges. Adv. Prev. Med. 2012, 2012, 731604. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.fda.gov/vaccines-blood-biologics/approved-blood-products/bat-botulism-antitoxin-heptavalent-b-c-d-e-f-g-equine (accessed on 25 October 2020).
- Arnon, S.S.; Schechter, R.; Maslanka, S.E.; Jewell, N.P.; Hatheway, C.L. Human botulism immune globulin for the treatment of infant botulism. N. Engl. J. Med. 2006, 354, 462–471. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Dong, J.; Lou, J.; Wen, W.; Conrad, F.; Geren, I.N.; Garcia-Rodriguez, C.; Smith, T.J.; Smith, L.A.; Ho, M.; et al. Monoclonal Antibodies that Inhibit the Proteolytic Activity of Botulinum Neurotoxin Serotype/B. Toxins (Basel) 2015, 7, 3405–3423. [Google Scholar] [CrossRef] [PubMed]
- Tomic, M.T.; Espinoza, Y.; Martinez, Z.; Pham, K.; Cobb, R.R.; Snow, D.M.; Earnhart, C.G.; Pals, T.; Syar, E.E.; Niemuth, N.; et al. Monoclonal antibody combinations prevent serotype A and serotype B inhalational botulism in a guinea pig model. Toxins 2019, 11, 208. [Google Scholar] [CrossRef] [PubMed]
- Nayak, S.U.; Griffiss, J.M.; McKenzie, R.; Fuchs, E.J.; Jurao, R.A.; An, A.T.; Ahene, A.; Tomic, M.; Hendrix, C.W.; Zenilman, J.M. Safety and pharmacokinetics of XOMA 3AB, a novel mixture of three monoclonal antibodies against botulinum toxin A. Antimicrob. Agents Chemother. 2014, 58, 5047–5053. [Google Scholar] [CrossRef]
- Reames, H.; Kadull, P.; Housewright, R.; Wilson, J. Studies on Botulinum Toxoids, Types A and B. III. Immunization of Man. J. Immunol. 1947, 55, 309–324. [Google Scholar]
- Fiock, M.A.; Devine, L.F.; Gearinger, N.F.; Duff, J.T.; Wright, G.G.; Kadull, P.J. Studies on immunity to toxins of Clostridium botulinum. VIII. Immunological response of man to purified bivalent AB botulinum toxoid. J. Immunol. 1962, 88, 277–283. [Google Scholar]
- Meng, Q.; Garcia-Rodriguez, C.; Manzanarez, G.; Silberg, M.A.; Conrad, F.; Bettencourt, J.; Pan, X.; Breece, T.; To, R.; Li, M.; et al. Engineered domain-based assays to identify individual antibodies in oligoclonal combinations targeting the same protein. Anal. Biochem. 2012, 430, 141–150. [Google Scholar] [CrossRef]
- Cardella, M.A. Botulism: Proceedings of a Symposium; U.S. Department of Health, Education, Welfare, Public Service: Washington, DC, USA, 1964.
- Meng, Q.; Li, M.; Silberg, M.A.; Conrad, F.; Bettencourt, J.; To, R.; Huang, C.; Ma, J.; Meyer, K.; Shimizu, R.; et al. Domain-based assays of individual antibody concentrations in an oligoclonal combination targeting a single protein. Anal. Biochem. 2012, 421, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Hatheway, C.; Dang, C. Immunogenecity of the neurotoxins of Clostridium botulinum. Botulinum Toxin 1994, 25, 93–107. [Google Scholar]
- Khouri, J.M.; Motter, R.N.; Arnon, S.S. Safety and immunogenicity of investigational recombinant botulinum vaccine, rBV A/B, in volunteers with pre-existing botulinum toxoid immunity. Vaccine 2018, 36, 2041–2048. [Google Scholar] [CrossRef] [PubMed]
- Shearer, J.D.; Vassar, M.L.; Swiderski, W.; Metcalfe, K.; Niemuth, N.; Henderson, I. Botulinum neurotoxin neutralizing activity of immune globulin (IG) purified from clinical volunteers vaccinated with recombinant botulinum vaccine (rBV A/B). Vaccine 2010, 28, 7313–7318. [Google Scholar] [CrossRef]
- Gelzleichter, T.R.; Myers, M.A.; Menton, R.G.; Niemuth, N.A.; Matthews, M.C.; Langford, M.J. Protection against botulinum toxins provided by passive immunization with botulinum human immune globulin: Evaluation using an inhalation model. J. Appl. Toxicol. JAT 1999, 19 (Suppl. 1), S35–S38. [Google Scholar] [CrossRef]
- Guyton, A.C. Measurement of the respiratory volumes of laboratory animals. Am. J. Physiol. 1947, 150, 70–77. [Google Scholar] [CrossRef]

| Treatment Group | Number of Animals | BoNT Serotype and Dose Route | Total Antibody Dose (mg) a | Geometric Mean NAC (U/mL) b 95% Confidence Interval |
|---|---|---|---|---|
| 1-Vehicle | 6 | A, IM. | 0 | LLOQ |
| 2-Anti-BoNT/A/B | 13 | A, IM | 0.030 | 0.11 (0.027, 0.43) |
| 3-Anti-BoNT/A/B | 13 | A, IM | 0.006 | LLOQ |
| 4-Anti-BoNT/A/B | 13 | A, IM | 0.003 | LLOQ |
| 5-Anti-BoNT/A/B | 13 | A, IM | 0.002 | LLOQ |
| 6-Vehicle | 6 | B, IM. | 0 | LLOQ |
| 7-Anti-BoNT/A/B | 13 | B, IM | 0.030 | 0.46 (0.30, 0.69) |
| 8-Anti-BoNT/A/B | 13 | B, IM | 0.006 | 0.097 (0.022, 0.44) |
| 9-Anti-BoNT/A/B | 13 | B, IM | 0.003 | 0.015 (0.0083, 0.028) |
| 10-Anti-BoNT/A/B | 13 | B, IM | 0.002 | LLOQ |
| Treatment Group | Number of Animals | BoNT Serotype and Dose Route | Total Dose (mg) a | Geometric Mean NAC (U/mL) 95% Confidence Intervals b |
|---|---|---|---|---|
| 1-Vehicle | 5 | A, IM. | 0 | LLOQ |
| 2-Anti-BoNT/A/B | 13 | A, IM | 0.03 | 0.15 (0.016, 1.4) |
| 3- Anti-BoNT/A/B | 13 | A, IM | 0.003 | LLOQ |
| 4- Anti-BoNT/A/B | 13 | A, IM | 0.0025 | LLOQ |
| 5- Anti-BoNT/A/B | 13 | A, IM | 0.002 | LLOQ |
| 6- Anti-BoNT/A/B | 13 | A, IV | 0.0025 | LLOQ |
| 7-Vehicle | 5 | B, IM. | 0 | LLOQ |
| 8-Anti-BoNT/A/B | 13 | B, IM | 0.03 | 0.38 (0.25, 0.057) |
| 9- Anti-BoNT/A/B | 13 | B, IM | 0.0025 | 0.01 (0.008, 0.013) |
| 10- Anti-BoNT/A/B | 13 | B, IM | 0.002 | 0.015 (0.0036, 0.63) |
| 11- Anti-BoNT/A/B | 13 | B, IM | 0.0015 | LLOQ |
| 12- Anti-BoNT/A/B | 13 | B, IV | 0.002 | 0.014 (0.0044, 0.0046) |
| Parameters | Study 1 | Study 2 | |||
|---|---|---|---|---|---|
| BoNT/A1 | BoNT/B1 | BoNT/A1 | BoNT/B1 | ||
| Guinea pig LD50 delivered | Target | 100 | 100 | 100 | 100 |
| Actual | 27 (Run 1), 31 (Run 2) | 46 (Run 3), 37 (Run 4) | 169 (Run 1), 238 (Run 2) | 191 (Run 3), 180 (run 4) | |
| Inhaled dose (MIPLD50/animal) * | Average | 4596 | 8351 | 32,131 | 37,059 |
| Total accumulated tidal volume (TATV) (L) | Actual | 2.20 | 2.20 | 2.17 | 2.19 |
| Impinger concentration (MIPLD50/mL) * | Actual | 1.39E + 04 | 2.34E + 03 | 2.26E + 04 | 3.54E + 04 |
| Nebulizer suspension concentration (MIPLD50/mL) * | Average | 3.22E + 06 | 5.81E + 05 | 4.52E + 06 | 7.51E + 06 |
| Aerosol conc. (MIPLD50/L) * | Average | 2.09E + 03 | 3.80E + 03 | 1.48E + 04 | 1.70E + 04 |
| Mass median aerodynamic diameter (µm) | Actual | 1.11 | 1.08 | 1.07 | 1.00 |
| Exposure time (min) | Actual | 12.00 | 12.00 | 12.00 | 12.00 |
| Number of animals per exposure | Actual | 20 | 20 | 20 | 20 |
| Treatment Group | Total mAb Concentration (mg) | BoNT Challenge Serotype and Route | Average Time to Death (h) | Average Weight Gain (g) after 14 Days * | Mortality (Number Dead/Total Animals) |
|---|---|---|---|---|---|
| First Challenge Experiment | |||||
| 1-PBS | 0 | A1 | 11.8 | - | 6/6 |
| 2-Anti-BoNT/A/B | 0.03 | A1, IM | N/A | 145.4 | 0/10 |
| 3-Anti-BoNT/A/B | 0.006 | A1, IM | N/A | 148.9 | 0/10 |
| 4-Anti-BoNT/A/B | 0.003 | A1, IM | N/A | 91.1 | 0/10 |
| 5-Anti-BoNT/A/B | 0.002 | A1, IM | 116.4 | 70.6 | 9/10 |
| 6-PBS | 0 | B1 | 11.5 | - | 6/6 |
| 7-Anti-BoNT/A/B | 0.03 | B1, IM | N/A | 157.4 | 0/10 |
| 8-mAb/A/B | 0.006 | B1, IM. | N/A | 156.9 | 0/10 |
| 9-mAb/A/B | 0.003 | B1, IM | 222.2 | 135.8 | 1/10 |
| 10-Anti-BoNT/A/B | 0.002 | B1, IM | 129.5 | 91.8 | 5/10 |
| Second Challenge Experiment | |||||
| 1-PBS | 0 | A1 | 7.8 | - | 5/5 |
| 2-Anti-BoNT/A/B | 0.03 | A1, IM. | N/A | 131.1 | 0/10 |
| 3-Anti-BoNT/A/B | 0.003 | A1, IM | 53.6 | - | 10/10 |
| 4-Anti-BoNT/A/B | 0.0025 | A1, IM | 28.6 | - | 10/10 |
| 5-Anti-BoNT/A/B | 0.002 | A1, IM | 19.6 | - | 10/10 |
| 6-Anti-BoNT/A/B | 0.0025 | A1, IV | 42.9 | - | 10/10 |
| 7-PBS | 0 | B1 | 10.6 | - | 5/5 |
| 8-Anti-BoNT/A/B | 0.03 | B1, IM. | N/A | 115.2 | 0/10 |
| 9-Anti-BoNT/A/B | 0.0025 | B1, IM | 91.5 | 37.3 | 8/10 |
| 10-Anti-BoNT/A/B | 0.002 | B1, IM | 58.1 | - | 10/10 |
| 11-Anti-BoNT/A/B | 0.0015 | B1, IM | 41.4 | - | 10/10 |
| 12-Anti-BoNT/A/B | 0.002 | B1, IV | 67.2 | - | 10/10 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Snow, D.M.; Cobb, R.R.; Martinez, J.; Finger-Baker, I.; Collins, L.; Terpening, S.; Syar, E.S.; Niemuth, N.; Kobs, D.; Barnewall, R.; et al. A Monoclonal Antibody Combination against both Serotypes A and B Botulinum Toxin Prevents Inhalational Botulism in a Guinea Pig Model. Toxins 2021, 13, 31. https://doi.org/10.3390/toxins13010031
Snow DM, Cobb RR, Martinez J, Finger-Baker I, Collins L, Terpening S, Syar ES, Niemuth N, Kobs D, Barnewall R, et al. A Monoclonal Antibody Combination against both Serotypes A and B Botulinum Toxin Prevents Inhalational Botulism in a Guinea Pig Model. Toxins. 2021; 13(1):31. https://doi.org/10.3390/toxins13010031
Chicago/Turabian StyleSnow, Doris M., Ronald R. Cobb, Juan Martinez, Isaac Finger-Baker, Laura Collins, Sara Terpening, Emily S. Syar, Nancy Niemuth, Dean Kobs, Roy Barnewall, and et al. 2021. "A Monoclonal Antibody Combination against both Serotypes A and B Botulinum Toxin Prevents Inhalational Botulism in a Guinea Pig Model" Toxins 13, no. 1: 31. https://doi.org/10.3390/toxins13010031
APA StyleSnow, D. M., Cobb, R. R., Martinez, J., Finger-Baker, I., Collins, L., Terpening, S., Syar, E. S., Niemuth, N., Kobs, D., Barnewall, R., Farr-Jones, S., Marks, J. D., & Tomic, M. T. (2021). A Monoclonal Antibody Combination against both Serotypes A and B Botulinum Toxin Prevents Inhalational Botulism in a Guinea Pig Model. Toxins, 13(1), 31. https://doi.org/10.3390/toxins13010031






