Infection with a Nonencapsulated Bacillus anthracis Strain in Rabbits—The Role of Bacterial Adhesion and the Potential for a Safe Live Attenuated Vaccine
Abstract
1. Introduction
2. Results
2.1. Pathogenicity of Vollum∆pXO2 Strain in Rabbits Following Different Infection Routes
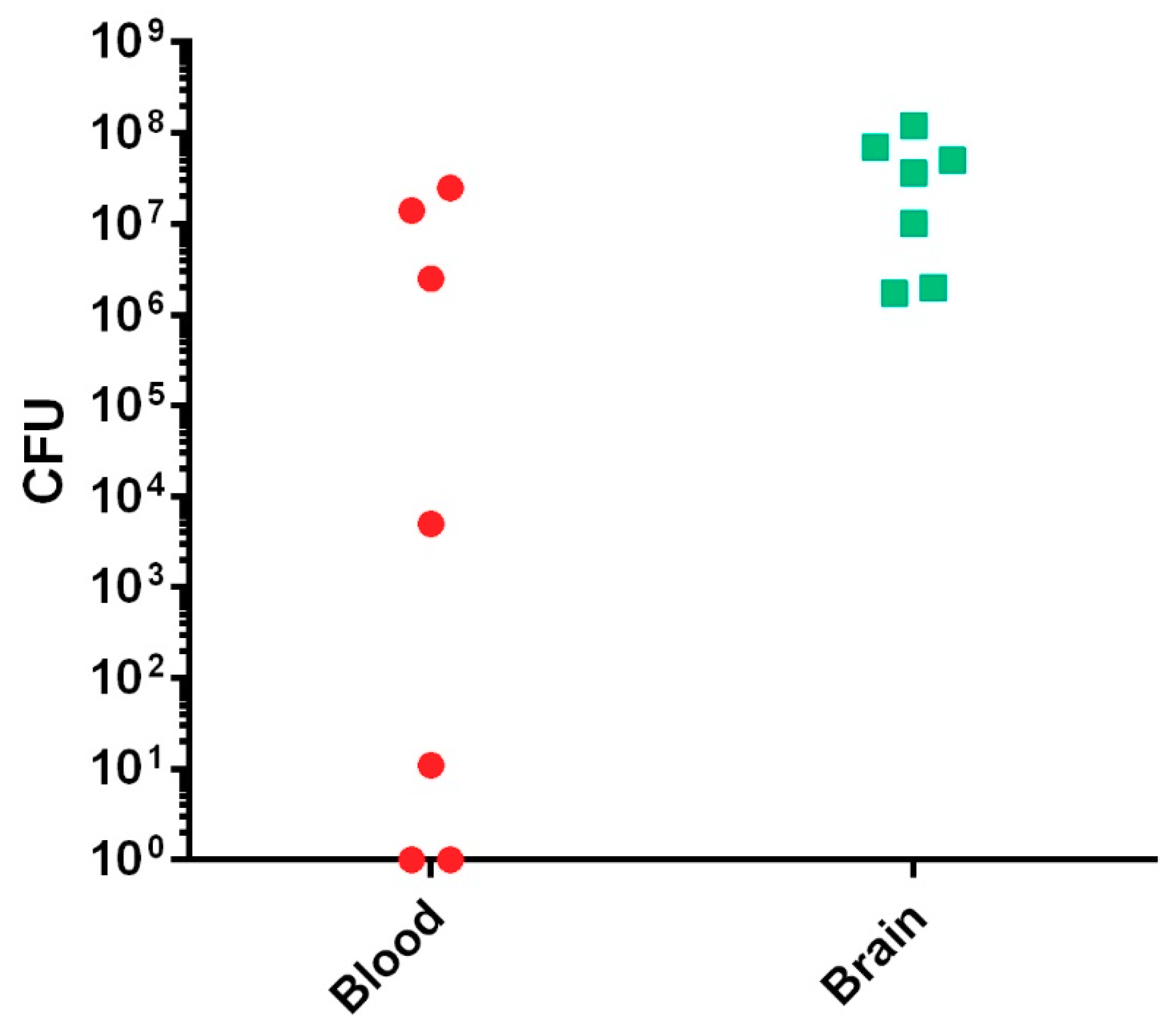
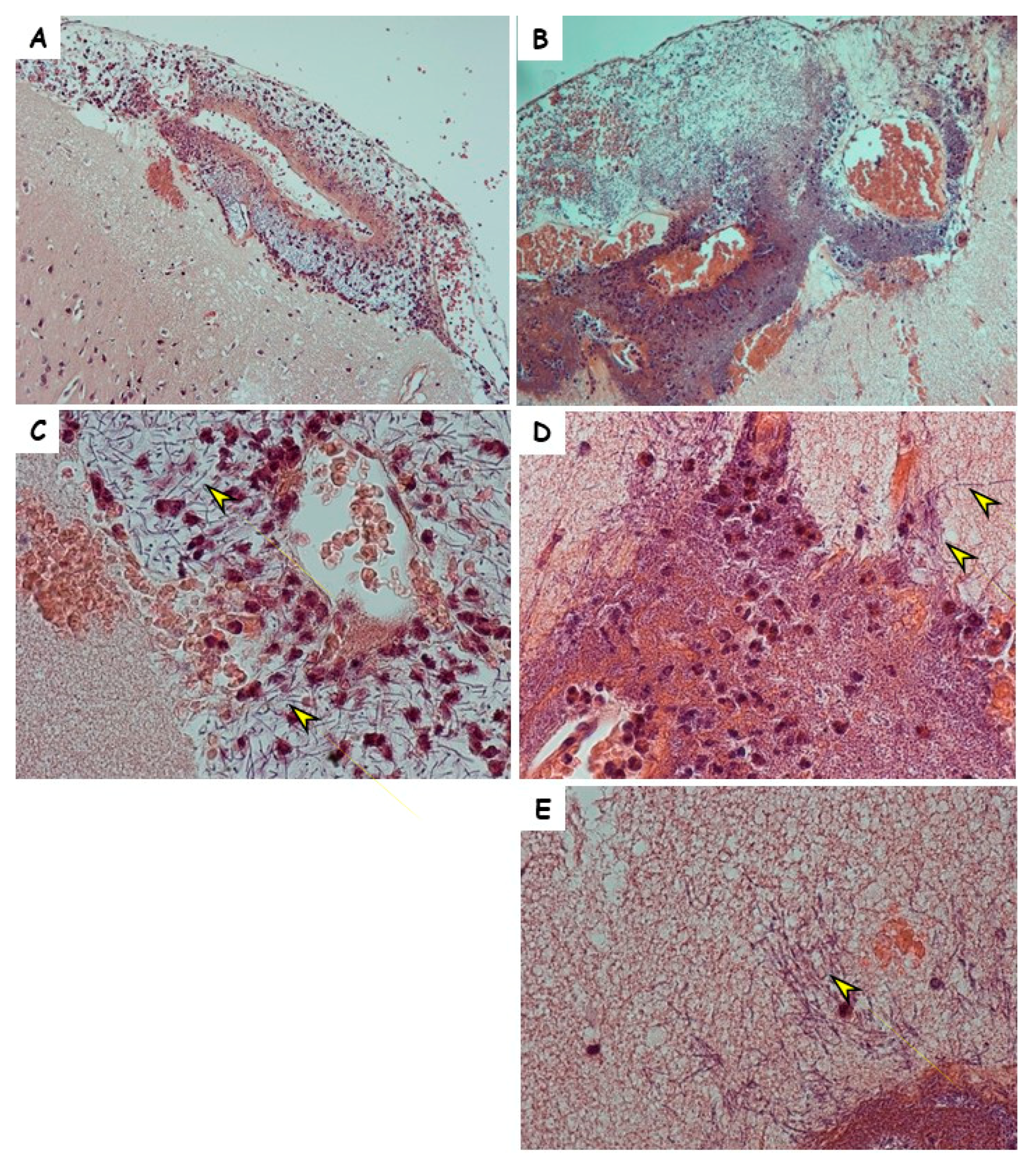
2.2. Brain Pathology of the Vollum∆pXO2 Infection
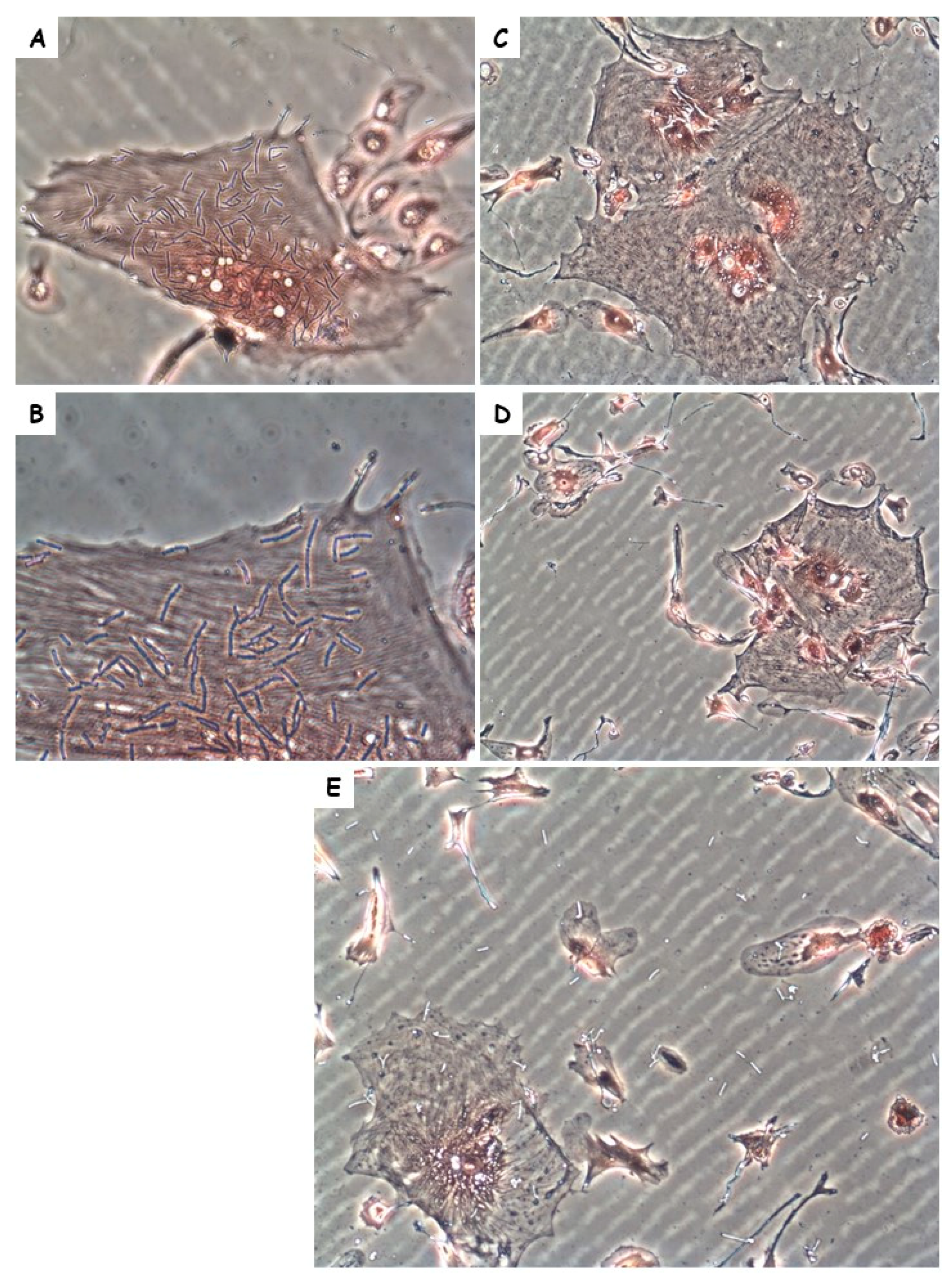
2.3. Role of BslA Adherence Protein in the Pathogenicity of Vollum∆pXO2
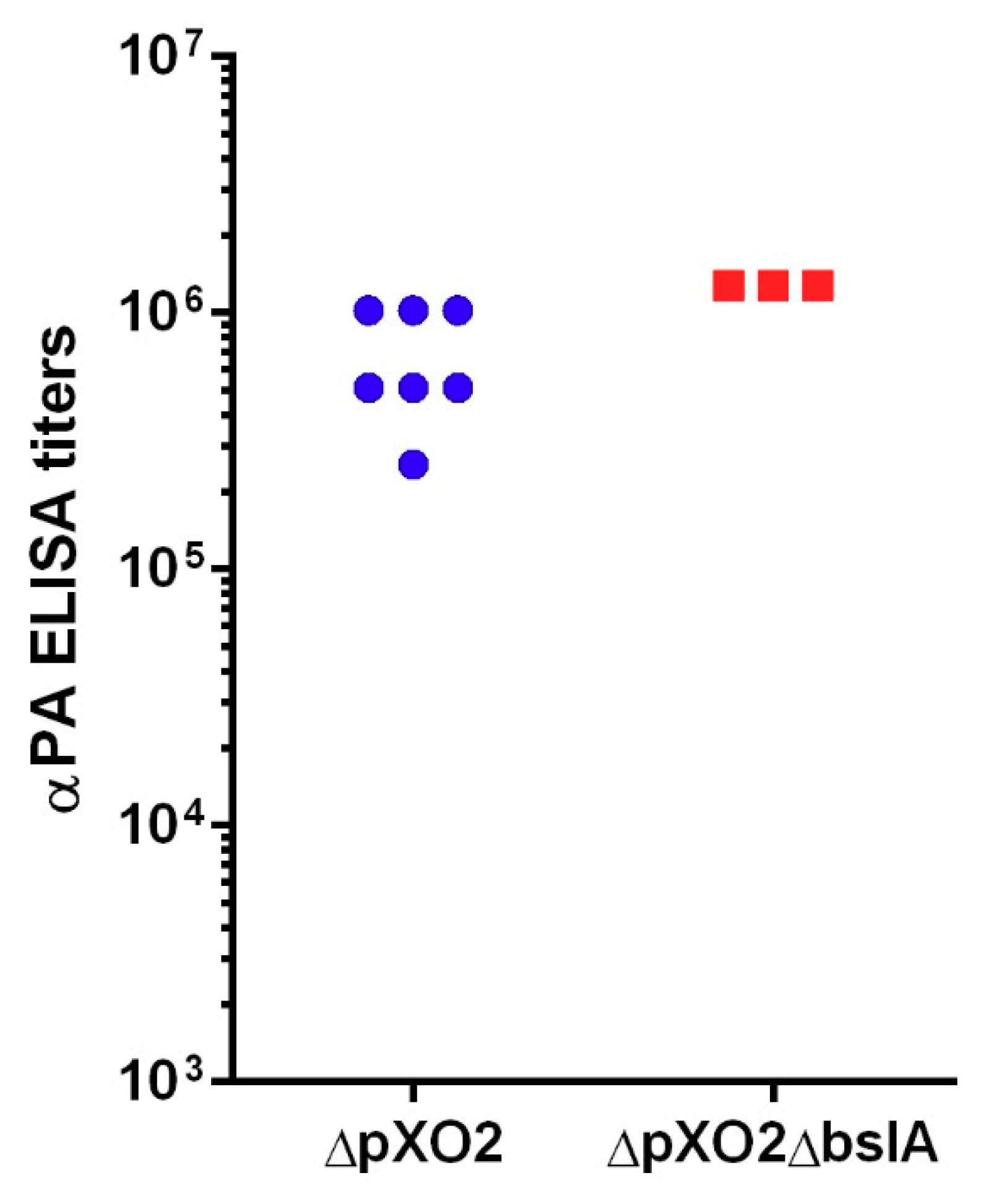
2.4. Vaccine Potential of the Vollum∆pXO2∆bslA Strain
3. Discussion
4. Materials and Methods
4.1. Bacteria Strains, Media, and Growth Conditions
4.2. Rabbit Infections
4.3. Determination of Tissue Bacterial Burdens
4.4. Isolation of Rabbit Primary Brain Endothelial Cells (RB-PBEC)
4.5. In Vitro Bacterial Adhesion Assay Using RB-PBEC
4.6. Histopathological Tissue Processing
4.7. Histopathological Staining
4.8. Image Acquisition
Author Contributions
Funding
Conflicts of Interest
References
- Dixon, T.C.; Meselson, M.; Guillemin, J.; Hanna, P.C. Anthrax. N. Engl. J. Med. 1999, 341, 815–826. [Google Scholar] [CrossRef] [PubMed]
- Hanna, P. Anthrax pathogenesis and host response. Curr. Top. Microbiol. Immunol. 1998, 225, 13–35. [Google Scholar] [PubMed]
- Swartz, M.N. Recognition and management of anthrax—An update. N. Engl. J. Med. 2001, 345, 1621–1626. [Google Scholar] [CrossRef] [PubMed]
- Sirisanthana, T.; Brown, A.E. Anthrax of the gastrointestinal tract. Emerg. Infect. Dis. 2002, 8, 649–651. [Google Scholar] [CrossRef] [PubMed]
- Brachman, P.C. Inhalation anthrax. Ann. N. Y. Acad. Sci. 1980, 353, 11. [Google Scholar] [CrossRef]
- Walsh, J.J.; Pesik, N.; Quinn, C.P.; Urdaneta, V.; Dykewicz, C.A.; Boyer, A.E.; Guarner, J.; Wilkins, P.; Norville, K.J.; Barr, J.R.; et al. A case of naturally acquired inhalation anthrax: Clinical care and analyses of anti-protective antigen immunoglobulin g and lethal factor. Clin. Infect. Dis. 2007, 44, 968–971. [Google Scholar] [CrossRef] [PubMed]
- Jernigan, D.B.; Raghunathan, P.L.; Bell, B.P.; Brechner, R.; Bresnitz, E.A.; Butler, J.C.; Cetron, M.; Cohen, M.; Doyle, T.; Fischer, M.; et al. Investigation of bioterrorism-related anthrax, united states, 2001: Epidemiologic findings. Emerg. Infect. Dis. 2002, 8, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
- Meselson, M.; Guillemin, J.; Hugh-Jones, M.; Langmuir, A.; Popova, I.; Shelokov, A.; Yampolskaya, O. The sverdlovsk anthrax outbreak of 1979. Science 1994, 266, 1202–1208. [Google Scholar] [CrossRef] [PubMed]
- Moayeri, M.; Leppla, S.H. Cellular and systemic effects of anthrax lethal toxin and edema toxin. Mol. Aspects Med. 2009, 30, 439–455. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Moayeri, M.; Leppla, S.H. Anthrax lethal and edema toxins in anthrax pathogenesis. Trends Microbiol. 2014, 22, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Brossier, F.; Weber-Levy, M.; Mock, M.; Sirard, J.-C. Role of toxin functional domains in anthrax pathogenesis. Infect. Immun. 2000, 68, 1781–1786. [Google Scholar] [CrossRef] [PubMed]
- Fouet, A. The surface of Bacillus anthracis. Mol. Aspects Med. 2009, 30, 374–385. [Google Scholar] [CrossRef] [PubMed]
- Candela, T.; Fouet, A. Poly-gamma-glutamate in bacteria. Mol. Microbiol. 2006, 60, 1091–1098. [Google Scholar] [CrossRef] [PubMed]
- Scorpio, A.; Chabot, D.J.; Day, W.A.; Hoover, T.A.; Friedlander, A.M. Capsule depolymerase overexpression reduces Bacillus anthracis virulence. Microbiology 2010, 156, 1459–1467. [Google Scholar] [CrossRef] [PubMed]
- Guidi-Rontani, C. The alveolar macrophage: The trojan horse of Bacillus anthracis. Trends Microbiol. 2002, 10, 405–409. [Google Scholar] [CrossRef]
- Weiner, Z.P.; Glomski, I.J. Updating perspectives on the initiation of Bacillus anthracis growth and dissemination through its host. Infect. Immun. 2012, 80, 1626–1633. [Google Scholar] [CrossRef] [PubMed]
- Splino, M.; Patocka, J.; Prymula, R.; Chlibek, R. Anthrax vaccines. Ann. Saudi Med. 2005, 25, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Okinaka, R.T.; Challacombe, J.; Drees, K.; Birdsell, D.N.; Janke, N.; Naumann, A.; Seymour, M.; Hornstra, H.; Schupp, J.; Sahl, J.; et al. Genome sequence of Bacillus anthracis sti, a sterne-like georgian/soviet vaccine strain. Genome Announc. 2014, 2. [Google Scholar] [CrossRef] [PubMed]
- Zai, X.; Zhang, J.; Liu, J.; Liu, J.; Li, L.; Yin, Y.; Fu, L.; Xu, J.; Chen, W. Quantitative determination of lethal toxin proteins in culture supernatant of human live anthrax vaccine Bacillus anthracis a16r. Toxins 2016, 8, 56. [Google Scholar] [CrossRef] [PubMed]
- Goossens, P.L. Animal models of human anthrax: The quest for the holy grail. Mol. Aspects Med. 2009, 30, 467–480. [Google Scholar] [CrossRef] [PubMed]
- Chitlaru, T.; Israeli, M.; Rotem, S.; Elia, U.; Bar-Haim, E.; Ehrlich, S.; Cohen, O.; Shafferman, A. A novel live attenuated anthrax spore vaccine based on an acapsular Bacillus anthracis sterne strain with mutations in the htra, lef and cya genes. Vaccine 2017, 35, 6030–6040. [Google Scholar] [CrossRef] [PubMed]
- Welkos, S.; Bozue, J.; Twenhafel, N.; Cote, C. Animal models for the pathogenesis, treatment, and prevention of infection by Bacillus anthracis. Microbiol. Spectr. 2015, 3, 1–38. [Google Scholar]
- Levy, H.; Weiss, S.; Altboum, Z.; Schlomovitz, J.; Glinert, I.; Sittner, A.; Shafferman, A.; Kobiler, D. Differential contribution of Bacillus anthracis toxins to pathogenicity in two animal models. Infect. Immun. 2012, 80, 2623–2631. [Google Scholar] [CrossRef] [PubMed]
- Levy, H.; Glinert, I.; Weiss, S.; Bar-David, E.; Sittner, A.; Schlomovitz, J.; Altboum, Z.; Kobiler, D. The central nervous system as target of bacillus anthracis toxin independent virulence in rabbits and guinea pigs. PLoS ONE 2014, 9, e112319. [Google Scholar] [CrossRef] [PubMed]
- Levy, H.; Glinert, I.; Weiss, S.; Sittner, A.; Schlomovitz, J.; Altboum, Z.; Kobiler, D. Toxin-independent virulence of bacillus anthracis in rabbits. PLoS ONE 2014, 9, e84947. [Google Scholar] [CrossRef] [PubMed]
- Sittner, A.; Bar-David, E.; Glinert, I.; Ben-Shmuel, A.; Weiss, S.; Schlomovitz, J.; Kobiler, D.; Levy, H. Pathology of wild-type and toxin-independent bacillus anthracis meningitis in rabbits. PLoS ONE 2017, 12, e0186613. [Google Scholar] [CrossRef] [PubMed]
- Abramova, F.A.; Grinberg, L.M.; Yampolskaya, O.V.; Walker, D.H. Pathology of inhalational anthrax in 42 cases from the sverdlovsk outbreak of 1979. Proc. Natl. Acad. Sci. USA 1993, 90, 2291–2294. [Google Scholar] [CrossRef] [PubMed]
- Grinberg, L.M.; Abramova, F.A.; Yampolskaya, O.V.; Walker, D.H.; Smith, J.H. Quantitative pathology of inhalational anthrax i: Quantitative microscopic findings. Mod. Pathol. 2001, 14, 482–495. [Google Scholar] [CrossRef] [PubMed]
- Twenhafel, N.A. Pathology of inhalational anthrax animal models. Vet. Pathol. 2010, 47, 819–830. [Google Scholar] [CrossRef] [PubMed]
- Kern, J.; Schneewind, O. Bsla, the s-layer adhesin of b. Anthracis, is a virulence factor for anthrax pathogenesis. Mol. Microbiol. 2010, 75, 324–332. [Google Scholar] [CrossRef] [PubMed]
- Ebrahimi, C.M.; Kern, J.W.; Sheen, T.R.; Ebrahimi-Fardooee, M.A.; van Sorge, N.M.; Schneewind, O.; Doran, K.S. Penetration of the blood-brain barrier by bacillus anthracis requires the pxo1-encoded bsla protein. J. Bacteriol. 2009, 191, 7165–7173. [Google Scholar] [CrossRef] [PubMed]
- Kern, J.W.; Schneewind, O. Bsla, a pxo1-encoded adhesin of bacillus anthracis. Mol. Microbiol. 2008, 68, 504–515. [Google Scholar] [CrossRef] [PubMed]
- Longstreth, J.; Skiadopoulos, M.H.; Hopkins, R.J. Licensure strategy for pre- and post-exposure prophylaxis of biothrax vaccine: The first vaccine licensed using the fda animal rule. Expert Rev. Vaccines 2016, 15, 1467–1479. [Google Scholar] [CrossRef] [PubMed]
- Kobiler, D.; Gozes, Y.; Rosenberg, H.; Marcus, D.; Reuveny, S.; Altboum, Z. Efficiency of protection of guinea pigs against infection with bacillus anthracis spores by passive immunization. Infect. Immun. 2002, 70, 544–560. [Google Scholar] [CrossRef] [PubMed]
- Levy, H.; Weiss, S.; Altboum, Z.; Schlomovitz, J.; Rothschild, N.; Blachinsky, E.; Kobiler, D. Lethal factor is not required for bacillus anthracis virulence in guinea pigs and rabbits. Microb. Pathog. 2011, 51, 345–351. [Google Scholar] [CrossRef] [PubMed]
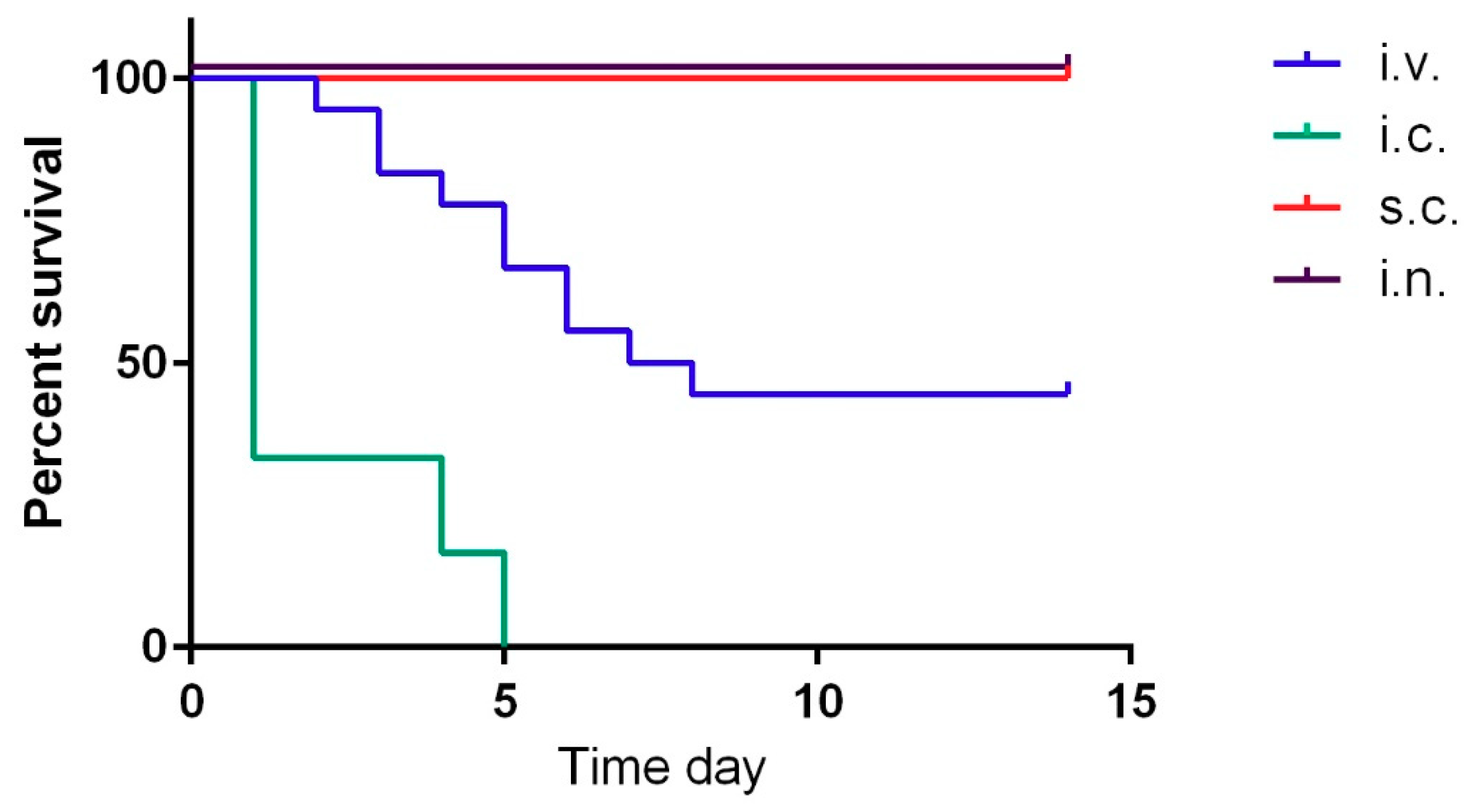
| Infection Route | Dose * (WT LD50) | Dead/Infected | Mean Time to Death (MTTD) (Days) |
|---|---|---|---|
| s.c. | 2 × 107 (106) | 0/4 | / |
| i.n. | 2 × 107 (103) | 0/4 | / |
| i.v. | 1 × 107 (106) | 10/18 ** | 4.9 |
| i.c. | 1 × 105 (104) | 6/6 *** | 2.1 |
| Infection Route | Dose (CFU) | Dead/Infected | Challenge Route | Strain | Dose (CFU) | Dead/Challenged |
|---|---|---|---|---|---|---|
| i.v. | 2 × 107 | 0/4 | s.c. | Vollum | 103 | 0/4 |
| s.c. | 2 × 107 | 0/4 | s.c. | Vollum | 103 | 0/4 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Glinert, I.; Weiss, S.; Sittner, A.; Bar-David, E.; Ben-Shmuel, A.; Schlomovitz, J.; Kobiler, D.; Levy, H. Infection with a Nonencapsulated Bacillus anthracis Strain in Rabbits—The Role of Bacterial Adhesion and the Potential for a Safe Live Attenuated Vaccine. Toxins 2018, 10, 506. https://doi.org/10.3390/toxins10120506
Glinert I, Weiss S, Sittner A, Bar-David E, Ben-Shmuel A, Schlomovitz J, Kobiler D, Levy H. Infection with a Nonencapsulated Bacillus anthracis Strain in Rabbits—The Role of Bacterial Adhesion and the Potential for a Safe Live Attenuated Vaccine. Toxins. 2018; 10(12):506. https://doi.org/10.3390/toxins10120506
Chicago/Turabian StyleGlinert, Itai, Shay Weiss, Assa Sittner, Elad Bar-David, Amir Ben-Shmuel, Josef Schlomovitz, David Kobiler, and Haim Levy. 2018. "Infection with a Nonencapsulated Bacillus anthracis Strain in Rabbits—The Role of Bacterial Adhesion and the Potential for a Safe Live Attenuated Vaccine" Toxins 10, no. 12: 506. https://doi.org/10.3390/toxins10120506
APA StyleGlinert, I., Weiss, S., Sittner, A., Bar-David, E., Ben-Shmuel, A., Schlomovitz, J., Kobiler, D., & Levy, H. (2018). Infection with a Nonencapsulated Bacillus anthracis Strain in Rabbits—The Role of Bacterial Adhesion and the Potential for a Safe Live Attenuated Vaccine. Toxins, 10(12), 506. https://doi.org/10.3390/toxins10120506





