Challenges in Implementing the Integrated Community-Based Outpatient Therapeutic Program for Severely Malnourished Children in Rural Southern Ethiopia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
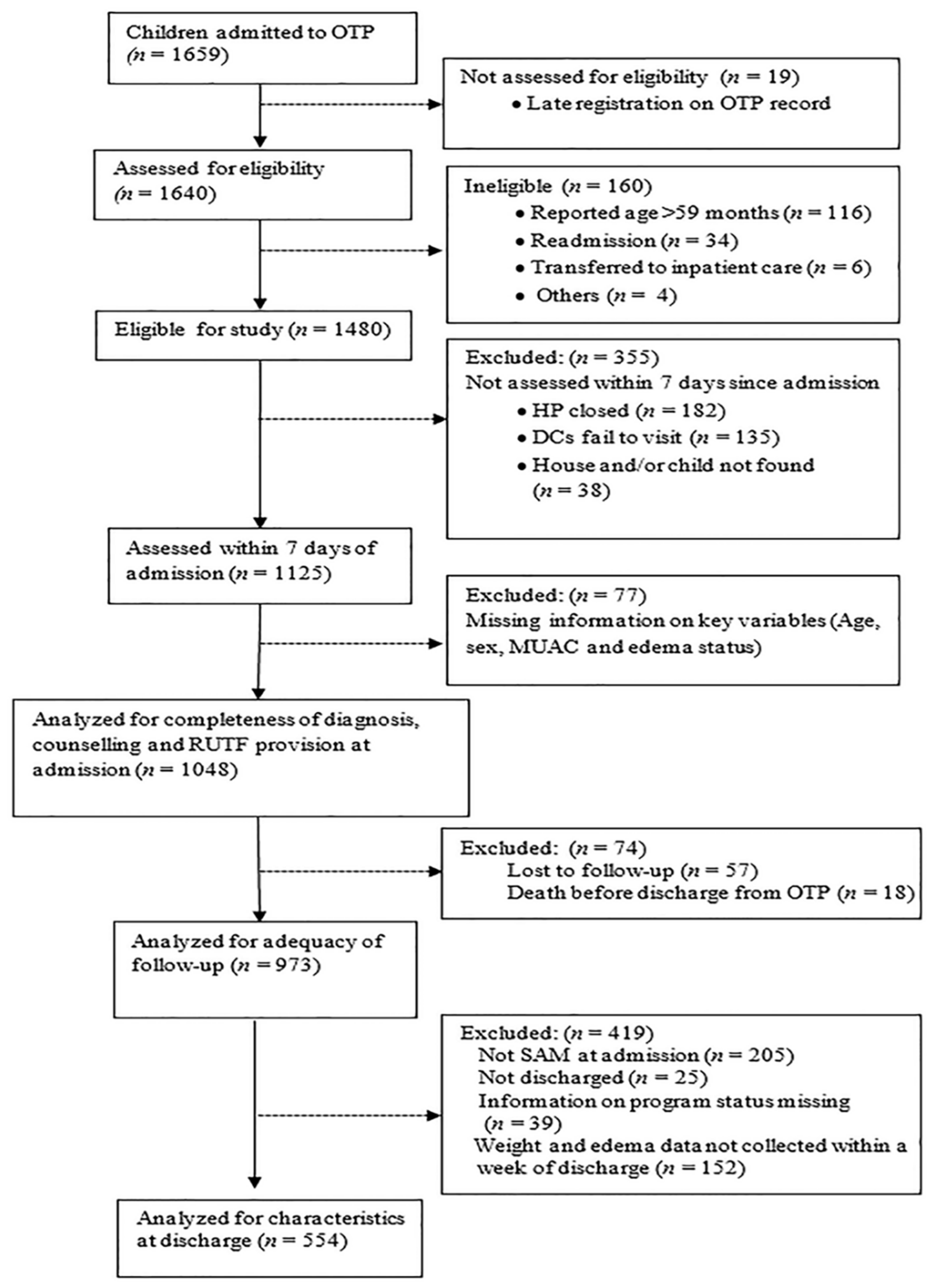
2.2. Participants and Data Collection
2.3. Outcome Measures and Statistical Analysis
2.4. Ethical Considerations
3. Results
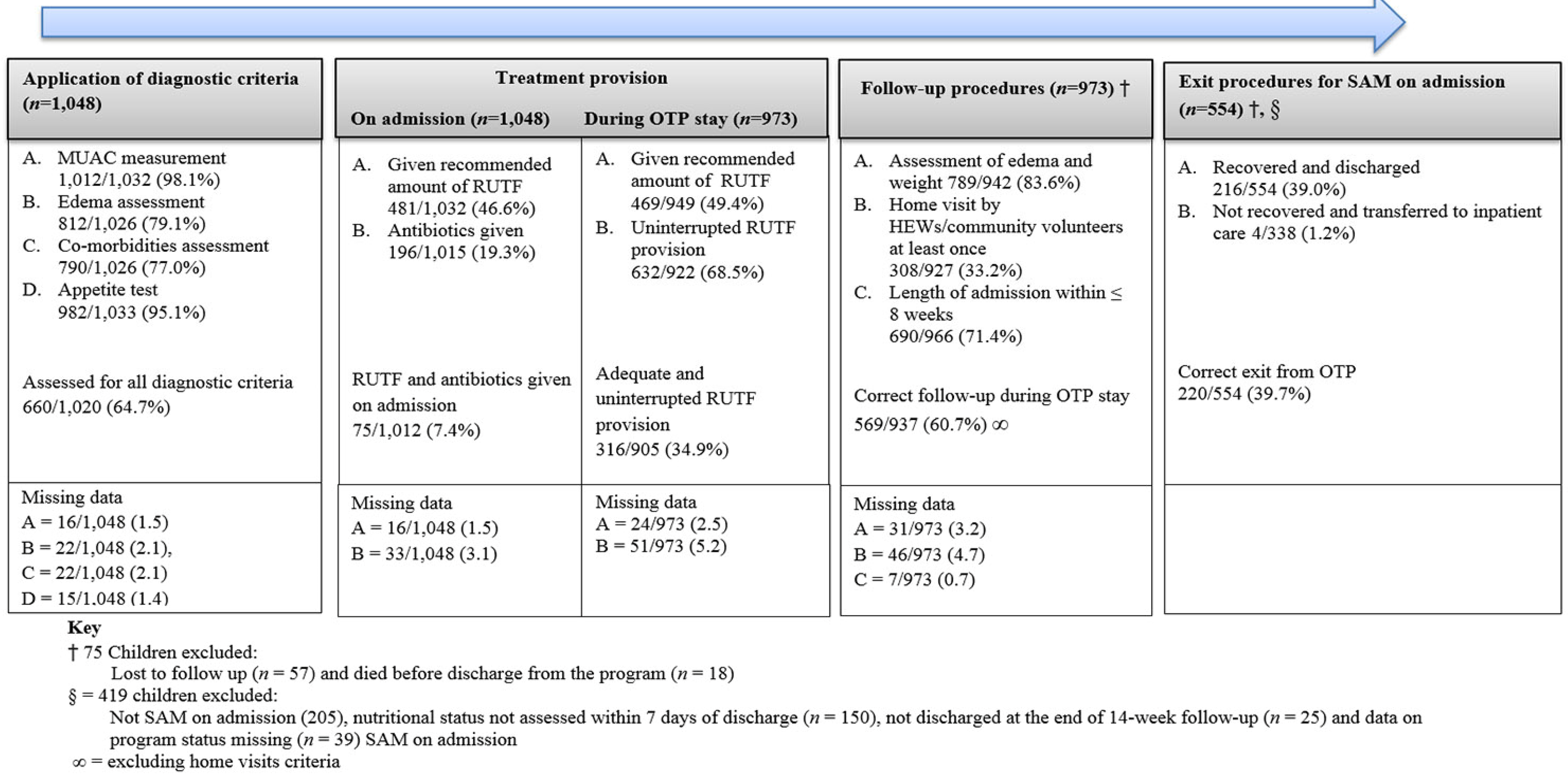
3.1. SAM Diagnosis and Provision of Treatment
3.2. Length of Admission, Follow-Up of Nutritional Status and Exit from C-OTP
3.3. Perceptions of RUTF Usage and OTP Service Provision
4. Discussion
4.1. Service Provision-Related Constraints
4.2. Constraints Related to Home-Based Management
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| CHW | Community Health Workers |
| C-OTP | Community-based Outpatient Therapeutic Program |
| HEW | Health Extension Workers |
| MUAC | Mid-Upper Arm Circumference |
| SAM | Severe Acute Malnutrition |
| WHO | World Health Organization |
References
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, A.A.; Christian, P.; De Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Ashworth, A. Efficacy and effectiveness of community-based treatment of severe malnutrition. Food Nutr. Bull. 2006, 27, S24–S48. [Google Scholar] [CrossRef] [PubMed]
- Federal Ministry of Health Ethiopia. Protocol for the Management of Severe Acute Malnutrition; Federal Ministry of Health: Addis Ababa, Ethiopia, 2007.
- World Health Organization. Guideline: Updates on the Management of Severe Acute Malnutrition in Infants and Children; WHO: Geneva, Switzerland, 2013. [Google Scholar]
- World Health Organization; World Food Program; United Nations Children’s Fund. Community-Based Management of Severe Acute Malnutrition: A Joint Statement by the World Health Organization, the World Food Program, the United Nations System Standing Committee on Nutrition and the United Nations Children’s Fund. 2007. Available online: http://www.who.int/nutrition/topics/Statement_community_based_man_sev_acute_mal_eng.pdf (accessed on 10 March 2016).
- Chamois, S. Decentralization of out-patient management of severe malnutrition in Ethiopia. Field Exch. 2009, 36, 12–13. [Google Scholar]
- Kapil, U. Ready to Use Therapeutic Food (RUTF) in the management of severe acute malnutrition in India. Indian Pediatr. 2009, 46, 381–382. [Google Scholar] [PubMed]
- Defourny, I.; Drouhin, E.; Terzian, M.; Tatay, M.; Sekkenes, J.; Tectonidis, M. Scaling up the treatment of acute childhood malnutrition in Niger. Field Exch. 2006, 28, 2–4. [Google Scholar]
- Sandige, H.; Ndekha, M.J.; Briend, A.; Ashorn, P.; Manary, M.J. Home-based treatment of malnourished Malawian children with locally produced or imported ready-to-use food. J. Pediatr. Gastroenterol. Nutr. 2004, 39, 141–146. [Google Scholar] [CrossRef] [PubMed]
- The Sphere Project. Minimum standards in food security and nutrition. In Humanitarian Charter and Minimum Standards in Disaster Response, 3rd ed.; Oxfam Publishing: Oxford, UK, 2011; pp. 164–173. [Google Scholar]
- Emergency Nutrition Network. Validation of Sphere Standards in a Normal Integrated CTC Setup. 2009. Available online: http://www.en-net.org/question/112.aspx (accessed on 10 March 2016).
- United Nations Children’s Fund. Evaluation of Community Management of Acute Malnutrition (CMAM); Global Synthesis Report; United Nations Children’s Fund: New York, NY, USA, 2013. [Google Scholar]
- Tadesse, E.; Berhane, Y.; Hjern, A.; Olsson, P.; Ekström, E.C. Perceptions of usage and unintended consequences of provision of ready-to-use therapeutic food for management of severe acute child malnutrition. A Qual. Study South. Ethiop. Health Policy Plan 2015, 30, 1334–1341. [Google Scholar] [CrossRef] [PubMed]
- Wakabi, W. Extension workers drive Ethiopia’s primary health care. Lancet 2008, 372, 880. [Google Scholar] [CrossRef]
- Eklund, M.; Tsinuel, G. Effectiveness of integrated outpatient care of severe acute malnutrition in Ethiopia. Field Exch. 2008, 34, 8. [Google Scholar]
- Emergency Nutrition Network. International Workshop on the Integration of Community-Based Management of Acute Malnutrition, Washington DC, Workshop Report; Emergency Nutrition Network: Oxford, UK, 2008. [Google Scholar]
- Yebyo, H.G.; Kendall, C.; Nigusse, D.; Lemma, W. Outpatient therapeutic feeding program outcomes and determinants in treatment of severe acute malnutrition in Tigray, northern Ethiopia: A retrospective cohort study. PLoS ONE 2013, 8, e65840. [Google Scholar] [CrossRef] [PubMed]
- Tadesse, E.; Worku, A.; Berhane, Y.; Ekström, E.C. Program outcome of a large scale integrated outpatient therapeutic program (OTP) and acute malnutrition beyond participating in the program: A longitudinal study in rural southern Ethiopia. PLoS ONE. in press.
- Hailu, A.; Regassa, N. Correlates of household food security in densely populated areas of southern Ethiopia: Does the household structure matter? Stud. Home Community Sci. 2007, 1, 85–91. [Google Scholar]
- Teklu, T. Environment Stress and Increased Vulnerability to Impoverishment and Survival in Ethiopia: A Synthesis. 2003. Available online: http://scholarworks.wmich.edu/cgi/viewcontent.cgi?article=1065&context=africancenter_icad_archive (accessed on 15 September 2014).
- Guimón, J.; Guimón, P. Innovation to Fight Hunger: The Case of Plumpy’nut. 2009. Available online: http://globelics2009dakar.merit.unu.edu/papers/1250617817_JG_1.pdf (accessed on 10 March 2016).
- United Nations Children’s Fund. Improving Child Nutrition. The Achievable Imperative for Global Progress. 2013. Available online: http://www.unicef.org/publications/files/Nutrition_Report_final_lo_res_8_April.pdf (accessed on 6 March 2015).
- Collins, S.; Sadler, K.; Dent, N.; Khara, T.; Guerrero, S.; Myatt, M.; Saboya, M.; Walsh, A. Key issues in the success of community-based management of severe malnutrition. Food Nutr. Bull. 2006, 27, S49–S82. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Epi Info™ version 6. 2008. Available online: https://wwwn.cdc.gov/epiinfo/html/ei6_downloads.htm (accessed on 14 September 2015). [Google Scholar]
- Field, A. Discovering Statistics Using SPSS, 3rd Revised ed.; Sage Publications: London, UK, 2009. [Google Scholar]
- Federal Ministry of Health Ethiopia. Management of Severe Acute Malnutrition at Health Post Level: Quick Reference for Health Extension Workers; Federal Ministry of Health: Addis Ababa, Ethiopia, 2008.
- Puett, C.; Guerrero, S. Barriers to access for severe acute malnutrition treatment services in Pakistan and Ethiopia: A comparative qualitative analysis. Public Health Nutr. 2015, 18, 1873–1882. [Google Scholar] [CrossRef] [PubMed]
- Puett, C.; Alderman, H.; Sadler, K.; Coates, J. “Sometimes they fail to keep their faith in us”: Community health worker perceptions of structural barriers to quality of care and community utilization of services in Bangladesh. Matern. Child Nutr. 2015, 11, 1011–1022. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; Global Health Workforce Alliance. Global Experience of Community Health Workers for Delivery of Health Related Millennium Development Goals: A Systematic Review, Country Case Studies, and Recommendations for Integration into National Health Systems; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Trehan, I.; Amthor, R.E.; Maleta, K.; Manary, M.J. Evaluation of the routine use of amoxicillin as part of the home-based treatment of severe acute malnutrition. Trop. Med. Int. Health 2010, 15, 1022–1028. [Google Scholar] [CrossRef] [PubMed]
- Lazzerini, M.; Tickell, D. Antibiotics in severely malnourished children: Systematic review of efficacy, safety and pharmacokinetics. Bull. World Health Organ. 2011, 89, 594–607. [Google Scholar] [CrossRef] [PubMed]
- Trehan, I.; Goldbach, H.S.; LaGrone, L.N.; Meuli, G.J.; Wang, R.J.; Maleta, K.M.; Manary, M.J. Antibiotics as part of the management of severe acute malnutrition. N. Engl. J. Med. 2013, 368, 444–453. [Google Scholar] [CrossRef] [PubMed]
- Hampshire, K.R.; Panter-Brick, C.; Kilpatrick, K.; Casiday, R.E. Saving lives, preserving livelihoods: Understanding risk, decision-making and child health in a food crisis. Soc. Sci. Med. 2009, 68, 758–765. [Google Scholar] [CrossRef] [PubMed]
- Engle, P.L.; Nieves, I. Intra-household food distribution among Guatemalan families in a supplementary feeding program: Behavior patterns. Soc. Sci. Med. 1993, 36, 1605–1612. [Google Scholar] [CrossRef]
| Perceptions of Resource Availability | Missing Data n (%) | n/n | % |
|---|---|---|---|
| Lack of RUTF in the health post is a problem | 8 (4.5) | ||
| Never/small problem | 112/167 | 67.1 | |
| Common problem | 55/167 | 32.9 | |
| Antibiotic not available in the health post (the longest time) | 16 (9.1) | ||
| 1 week–1 month | 12/159 | 7.5 | |
| >1 month | 47/159 | 29.6 | |
| Never had antibiotic | 100/159 | 62.9 | |
| HEW often feel overwhelmed because of all they work | 9 (5.1) | ||
| Strongly disagree/disagree | 19/166 | 11.4 | |
| Neither agree or disagree | 0/166 | 0.0 | |
| Strongly agree/agree | 147/166 | 88.6 | |
| HEW feels that the time they have is sufficient to complete all expected the activities | 8 (4.5) | ||
| Strongly disagree/disagree | 109/167 | 65.3 | |
| Neither agree or disagree | 1/167 | 0.6 | |
| Strongly agree/agree | 57/167 | 34.1 |
| Perceptions of Usage of RUTF | Caregivers | HEWs | ||
|---|---|---|---|---|
| Missing Data n (%) | n/n (%) | Missing Data n (%) | n/n (%) | |
| It is a problem to make malnourished children eat RUTF | 14 (1.4) | 10 (5.7) | ||
| Never difficult | 941/959 (98.1) | 129/165 (78.2) | ||
| Sometimes difficult | 18/959 (1.9) | 36/165 (21.8) | ||
| Caregivers selling of RUTF is a problem | 55 (5.6) | 8 (4.6) | ||
| It is not a/small problem | 424/918 (57.1) | 105/167 (62.9) | ||
| It is a/large problem | 394/918 (42.9) | 62/167 (37.1) | ||
| Is it difficult to avoid sharing RUTF with other non-SAM children in the household | 24 (2.5) | |||
| Not difficult | 635/949 (66.9) | NA | ||
| Difficult | 300/949 (31.6) | NA | ||
| No other children in the HH | 14/949 (1.5) | NA | ||
| RUTFs available in shops | 32 (3.2) | |||
| Yes | 248/941 (26.4) | NA | ||
| Not sure | 642/941 (68.2) | |||
| No | 51/941 (5.4) | |||
| Item | Missing Data n (%) | n/n (%) |
|---|---|---|
| How difficult is it for you to have this schedule for collection of RUTF (n = 939) | 34 (3.5) | |
| Not difficult | 883/939 (94.0) | |
| A little/very difficult | 56/939 (6.0) | |
| How often should you visit the health post to collect RUTF if you have a child with SAM (n = 952) | 21 (2.2) | |
| More than once in a week | 282/952 (29.6) | |
| Once in a week | 670/952 (70.4) | |
| To what extent do you think distance to the health post is a problem to adhere to follow up visits for SAM children (n = 946) | 6 (0.6) | |
| Not at all/small problem | 782/967 (80.9) | |
| Big problem | 185/967 (19.1) | |
| Do caregivers think HEWs listen to their problems? (n = 964) | 9 (0.9) | |
| Yes | 905/964 (93.9) | |
| No | 59/964 (6.1) | |
| Do caregivers think the HEW spent sufficient time with them and their children when visiting the health post for SAM? (n = 965) | 8 (0.8) | |
| Yes | 909/965 (94.2) | |
| No | 56/965 (5.8) | |
| Do caregivers think the HEWs were able to understand their problems/challenges related to managing their SAM child management? (n = 965) | 8 (0.8) | |
| Yes | 913/965 (94.6) | |
| No | 52/965 (5.4) |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tadesse, E.; Ekström, E.-C.; Berhane, Y. Challenges in Implementing the Integrated Community-Based Outpatient Therapeutic Program for Severely Malnourished Children in Rural Southern Ethiopia. Nutrients 2016, 8, 251. https://doi.org/10.3390/nu8050251
Tadesse E, Ekström E-C, Berhane Y. Challenges in Implementing the Integrated Community-Based Outpatient Therapeutic Program for Severely Malnourished Children in Rural Southern Ethiopia. Nutrients. 2016; 8(5):251. https://doi.org/10.3390/nu8050251
Chicago/Turabian StyleTadesse, Elazar, Eva-Charlotte Ekström, and Yemane Berhane. 2016. "Challenges in Implementing the Integrated Community-Based Outpatient Therapeutic Program for Severely Malnourished Children in Rural Southern Ethiopia" Nutrients 8, no. 5: 251. https://doi.org/10.3390/nu8050251
APA StyleTadesse, E., Ekström, E.-C., & Berhane, Y. (2016). Challenges in Implementing the Integrated Community-Based Outpatient Therapeutic Program for Severely Malnourished Children in Rural Southern Ethiopia. Nutrients, 8(5), 251. https://doi.org/10.3390/nu8050251





