Prevalence and Characterization of Self-Reported Gluten Sensitivity in The Netherlands
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Questionnaire
2.3. Statistical Analysis
3. Results
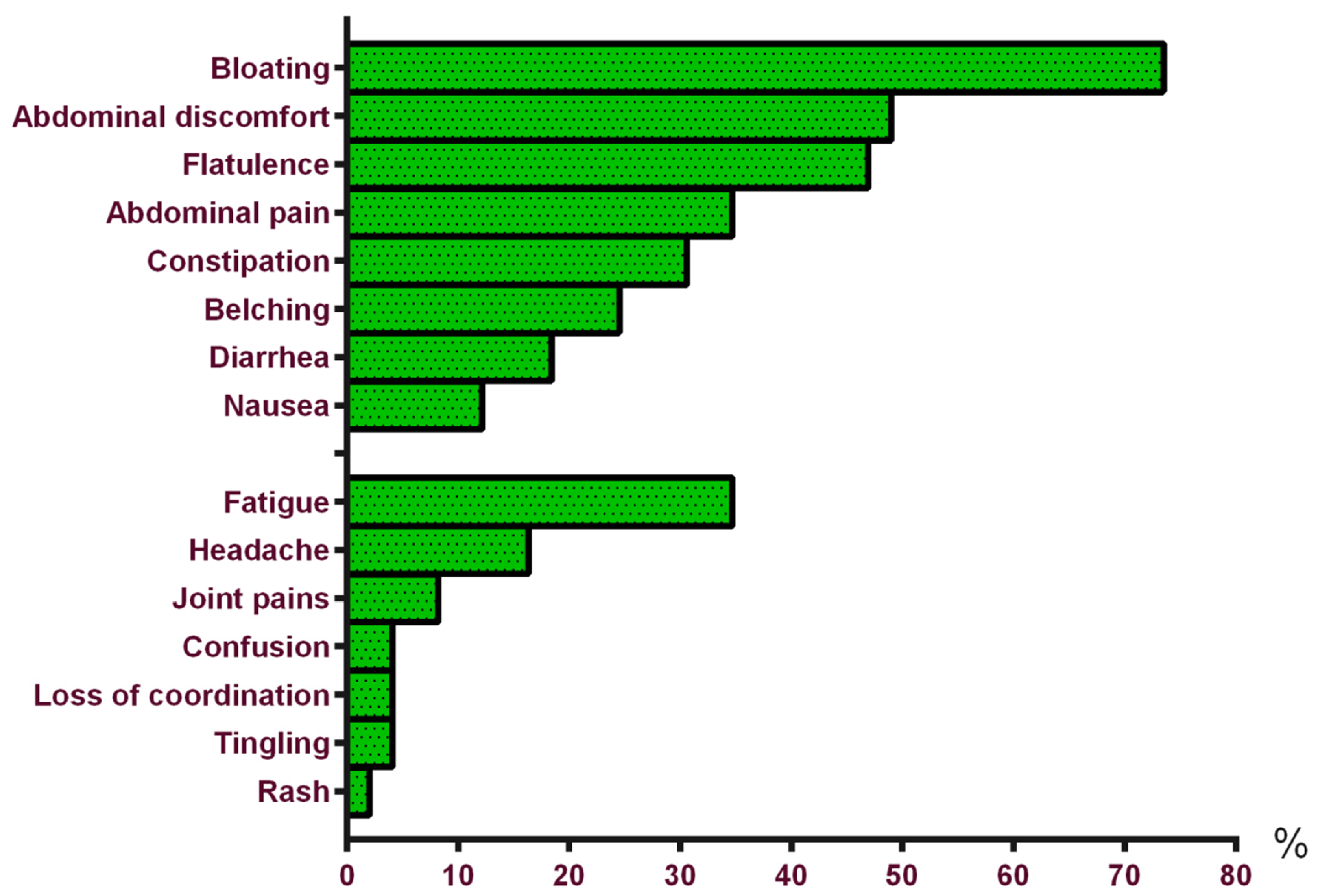
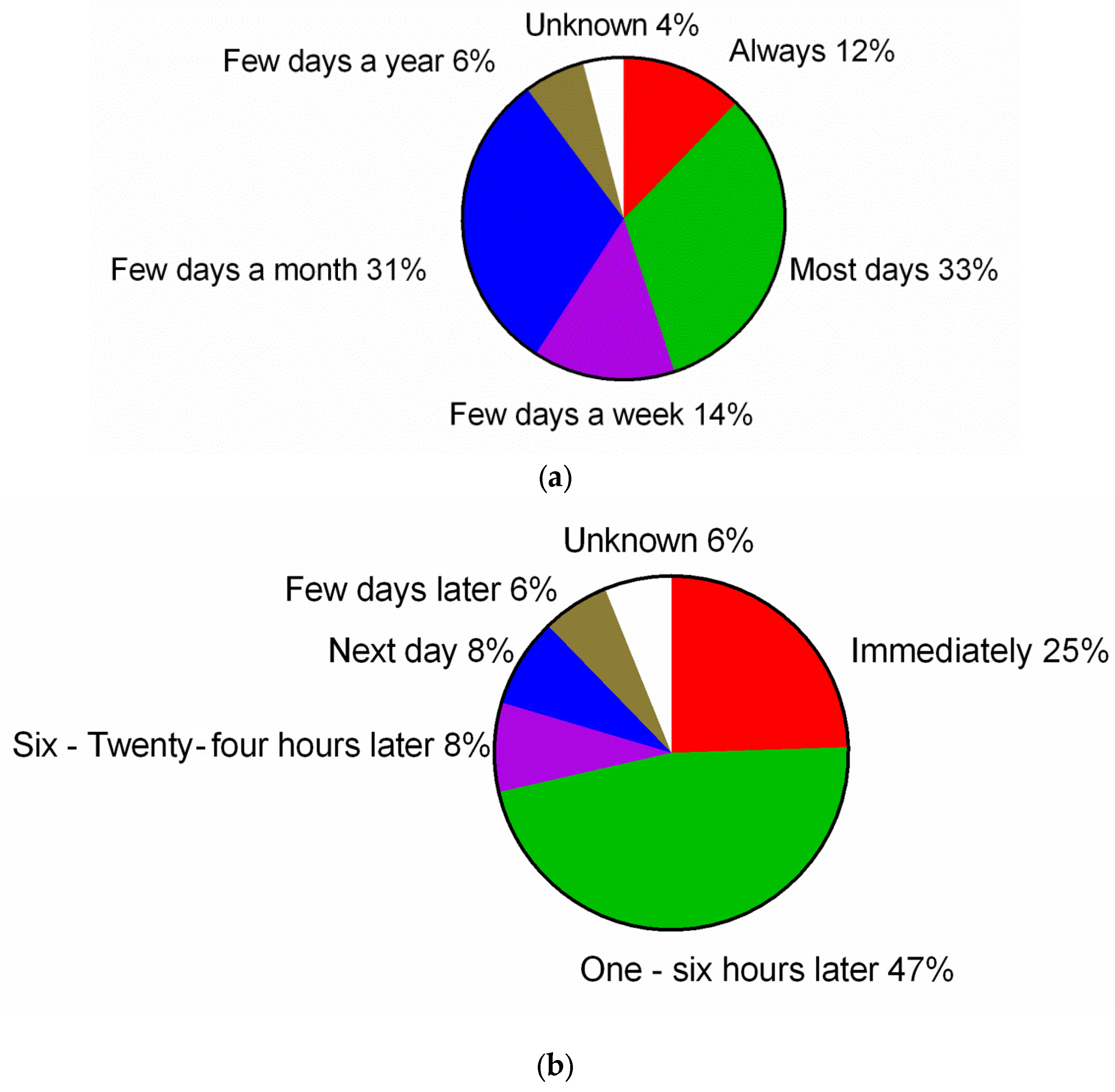
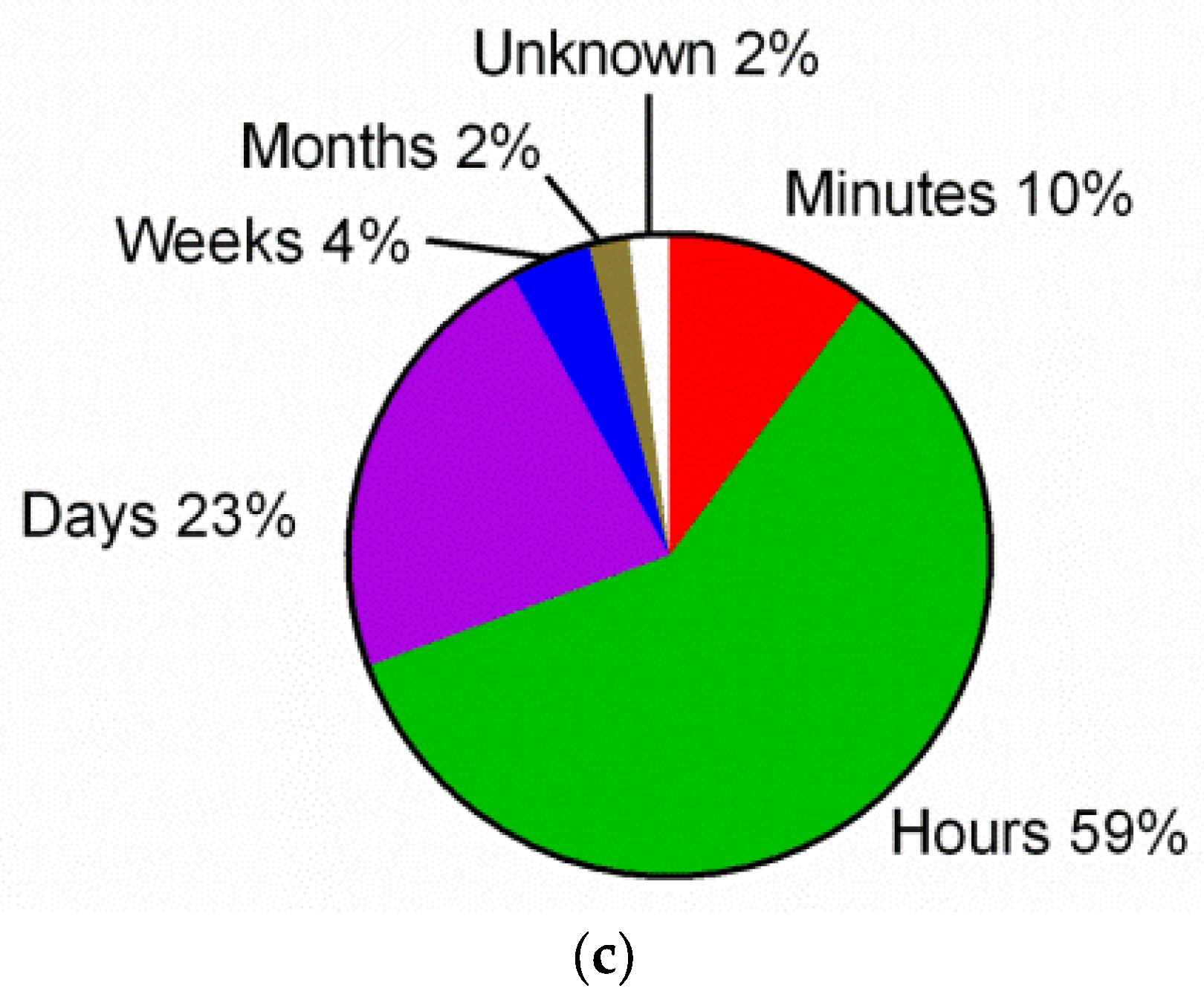
3.1. Characteristics of Self-Reported Gluten Sensitivity
3.2. Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols (FODMAPs)
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Cooper, B.T.; Holmes, G.K.; Ferguson, R.; Thompson, R.; Cooke, W.T. Proceedings: Chronic diarrhoea and gluten sensitivity. Gut 1976, 17, 398. [Google Scholar] [PubMed]
- Ellis, A.; Linaker, B.D. Non-coeliac gluten sensitivity? Lancet 1978, 1, 1358–1359. [Google Scholar] [CrossRef]
- Sapone, A.; Bai, J.C.; Ciacci, C.; Dolinsek, J.; Green, P.H.; Hadjivassiliou, M.; Kaukinen, K.; Rostami, K.; Sanders, D.S.; Schumann, M.; et al. Spectrum of gluten-related disorders: Consensus on new nomenclature and classification. BMC Med. 2012, 10, 13. [Google Scholar] [CrossRef] [PubMed]
- Catassi, C.; Elli, L.; Bonaz, B.; Bouma, G.; Carroccio, A.; Castillejo, G.; Cellier, C.; Cristofori, F.; de Magistris, L.; Dolinsek, J.; et al. Diagnosis of non-celiac gluten sensitivity (ncgs): The salerno experts’ criteria. Nutrients 2015, 7, 4966–4977. [Google Scholar] [CrossRef] [PubMed]
- The Great Gluten-Free Scam. Available online: http://www.telegraph.co.uk/food-and-drink/news/the-great-gluten-free-scam/ (accessed on 1 September 2016).
- Foschia, M.; Horstmann, S.; Arendt, E.K.; Zannini, E. Nutritional therapy–facing the gap between coeliac disease and gluten-free food. Int. J. Food Microbiol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Longstreth, G.F.; Thompson, W.G.; Chey, W.D.; Houghton, L.A.; Mearin, F.; Spiller, R.C. Functional bowel disorders. Gastroenterology 2006, 130, 1480–1491. [Google Scholar] [CrossRef] [PubMed]
- Di, S.A.; Biagi, F.; Gobbi, P.G.; Corazza, G.R. How I treat enteropathy-associated t-cell lymphoma. Blood 2012, 119, 2458–2468. [Google Scholar]
- Biesiekierski, J.R.; Peters, S.L.; Newnham, E.D.; Rosella, O.; Muir, J.G.; Gibson, P.R. No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology 2013, 145, 320–328; e321–e323. [Google Scholar] [CrossRef] [PubMed]
- Tanpowpong, P.; Ingham, T.R.; Lampshire, P.K.; Kirchberg, F.F.; Epton, M.J.; Crane, J.; Camargo, C.A., Jr. Coeliac disease and gluten avoidance in new zealand children. Arch. Dis. Child 2012, 97, 12–16. [Google Scholar] [CrossRef] [PubMed]
- DiGiacomo, D.V.; Tennyson, C.A.; Green, P.H.; Demmer, R.T. Prevalence of gluten-free diet adherence among individuals without celiac disease in the USA: Results from the continuous national health and nutrition examination survey 2009–2010. Scand. J. Gastroenterol. 2013, 48, 921–925. [Google Scholar] [CrossRef] [PubMed]
- Aziz, I.; Lewis, N.R.; Hadjivassiliou, M.; Winfield, S.N.; Rugg, N.; Kelsall, A.; Newrick, L.; Sanders, D.S. A UK study assessing the population prevalence of self-reported gluten sensitivity and referral characteristics to secondary care. Eur. J. Gastroenterol. Hepatol. 2014, 26, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Volta, U.; Bardella, M.T.; Calabro, A.; Troncone, R.; Corazza, G.R. An Italian prospective multicenter survey on patients suspected of having non-celiac gluten sensitivity. BMC Med. 2014, 12, 85. [Google Scholar] [CrossRef] [PubMed]
- Castillo, N.E.; Theethira, T.G.; Leffler, D.A. The present and the future in the diagnosis and management of celiac disease. Gastroenterol. Rep. (Oxf.) 2015, 3, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Golley, S.; Corsini, N.; Topping, D.; Morell, M.; Mohr, P. Motivations for avoiding wheat consumption in australia: Results from a population survey. Public Health Nutr. 2015, 18, 490–499. [Google Scholar] [CrossRef] [PubMed]
- Ontiveros, N.; Lopez-Gallardo, J.A.; Vergara-Jimenez, M.J.; Cabrera-Chavez, F. Self-reported prevalence of symptomatic adverse reactions to gluten and adherence to gluten-free diet in an adult mexican population. Nutrients 2015, 7, 6000–6015. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.H.; Neal, B.; Trevena, H.; Crino, M.; Stuart-Smith, W.; Faulkner-Hogg, K.; Yu Louie, J.C.; Dunford, E. Are gluten-free foods healthier than non-gluten-free foods? An evaluation of supermarket products in australia. Br. J. Nutr. 2015, 114, 448–454. [Google Scholar] [CrossRef] [PubMed]
- Aziz, I.; Karajeh, M.A.; Zilkha, J.; Tubman, E.; Fowles, C.; Sanders, D.S. Change in awareness of gluten-related disorders among chefs and the general public in the uk: A 10-year follow-up study. Eur. J. Gastroenterol. Hepatol. 2014, 26, 1228–1233. [Google Scholar] [CrossRef] [PubMed]
- Biesiekierski, J.R.; Newnham, E.D.; Shepherd, S.J.; Muir, J.G.; Gibson, P.R. Characterization of adults with a self-diagnosis of nonceliac gluten sensitivity. Nutr. Clin. Pract. 2014, 29, 504–509. [Google Scholar] [CrossRef] [PubMed]
- Fasano, A.; Sapone, A.; Zevallos, V.; Schuppan, D. Nonceliac gluten sensitivity. Gastroenterology 2015, 148, 1195–1204. [Google Scholar] [CrossRef] [PubMed]
- Young, E.; Stoneham, M.D.; Petruckevitch, A.; Barton, J.; Rona, R. A population study of food intolerance. Lancet 1994, 343, 1127–1130. [Google Scholar] [CrossRef]
- Lind, R.; Arslan, G.; Eriksen, H.R.; Kahrs, G.; Haug, T.T.; Florvaag, E.; Berstad, A. Subjective health complaints and modern health worries in patients with subjective food hypersensitivity. Dig. Dis. Sci. 2005, 50, 1245–1251. [Google Scholar] [CrossRef] [PubMed]
- Volta, U.; Pinto-Sanchez, M.I.; Boschetti, E.; Caio, G.P.; De Giorgio, R.; Verdu, E.F. Dietary triggers in irritable bowel syndrome: Is there a role for gluten. J. Neurogastroenterol. Motil. 2016, 22, 547–557. [Google Scholar] [CrossRef] [PubMed]
- Chey, W.D. Food: The main course to wellness and illness in patients with irritable bowel syndrome. Am. J. Gastroenterol. 2016, 111, 366–371. [Google Scholar] [CrossRef] [PubMed]
- Berstad, A. Functional dyspepsia-a conceptual framework. Gut 2000, 47, iv3–iv4, discussion iv10. [Google Scholar] [CrossRef] [PubMed]
- Volta, U.; Tovoli, F.; Cicola, R.; Parisi, C.; Fabbri, A.; Piscaglia, M.; Fiorini, E.; Caio, G. Serological tests in gluten sensitivity (nonceliac gluten intolerance). J. Clin. Gastroenterol. 2012, 46, 680–685. [Google Scholar] [CrossRef] [PubMed]
- Cecilio, L.A.; Bonatto, M.W. The prevalence of hla dq2 and dq8 in patients with celiac disease, in family and in general population. Arq. Bras. Cir. Dig 2015, 28, 183–185. [Google Scholar] [CrossRef] [PubMed]
- Wahnschaffe, U.; Schulzke, J.D.; Zeitz, M.; Ullrich, R. Predictors of clinical response to gluten-free diet in patients diagnosed with diarrhea-predominant irritable bowel syndrome. Clin. Gastroenterol. Hepatol. 2007, 5, 844–850, quiz 769. [Google Scholar] [CrossRef] [PubMed]
- Uhde, M.; Ajamian, M.; Caio, G.; De Giorgio, R.; Indart, A.; Green, P.H.; Verna, E.C.; Volta, U.; Alaedini, A. Intestinal cell damage and systemic immune activation in individuals reporting sensitivity to wheat in the absence of coeliac disease. Gut 2016. [Google Scholar] [CrossRef] [PubMed]
- Miyake, K.; Tanaka, T.; McNeil, P.L. Lectin-based food poisoning: A new mechanism of protein toxicity. PLoS ONE 2007, 2, e687. [Google Scholar] [CrossRef] [PubMed]
- Junker, Y.; Zeissig, S.; Kim, S.J.; Barisani, D.; Wieser, H.; Leffler, D.A.; Zevallos, V.; Libermann, T.A.; Dillon, S.; Freitag, T.L.; et al. Wheat amylase trypsin inhibitors drive intestinal inflammation via activation of toll-like receptor 4. J. Exp. Med. 2012, 209, 2395–2408. [Google Scholar] [CrossRef] [PubMed]
- Gibson, P.R.; Shepherd, S.J. Food choice as a key management strategy for functional gastrointestinal symptoms. Am. J. Gastroenterol. 2012, 107, 657–666, quiz 667. [Google Scholar] [CrossRef] [PubMed]
- Nijeboer, P.; Bontkes, H.J.; Mulder, C.J.; Bouma, G. Non-celiac gluten sensitivity. Is it in the gluten or the grain? J. Gastrointestin. Liver Dis. 2013, 22, 435–440. [Google Scholar] [PubMed]
- Burden, M.; Mooney, P.D.; Blanshard, R.J.; White, W.L.; Cambray-Deakin, D.R.; Sanders, D.S. Cost and availability of gluten-free food in the UK: In store and online. Postgrad. Med. J. 2015, 91, 622–626. [Google Scholar] [CrossRef] [PubMed]
| Variables | srGS (n = 49) (6.2%) | Controls (n = 734) (93.5%) | Odds Ratio (95% CI) | p-Value |
|---|---|---|---|---|
| Mean age ± sd (years) | 39 ± 15.1 | 47 ± 18.3 | - | 0.001 |
| Sex (% female) | 79.6 | 58.3 | 2.8 (1.4–5.7) | <0.01 |
| Education level (% high educated) | 49.0 | 39.3 | 1.5 (0.8–2.7) | NS |
| Region (% urban) | 75.5 | 55.7 | 2.5 (1.3–4.8) | <0.01 |
| Rome III criteria for IBS (%) | 36.7 | 9.0 | 5.9 (3.1–11.1) | <0.001 |
| Anxiety (%) | 16.3 | 3.1 | 6.0 (2.5–14.3) | <0.001 |
| Depression (%) | 14.3 | 8.3 | 1.8 (0.8–4.3) | NS |
| Bipolar disorder (%) | 2.0 | 0.4 | 5.1 (0.5–49.7) | NS |
| Schizophrenia (%) | 0 | 0.1 | - | NS |
| Thyroid disease (%) | 4.1 | 4.6 | 0.9 (0.2–3.8) | NS |
| Diabetes mellitus (young age onset) (%) | 4.1 | 1.1 | 3.9 (0.8–18.7) | NS |
| Anemia (%) | 16.3 | 6.1 | 3.0 (1.3–6.8) | 0.01 |
| Chronic Fatigue (%) | 6.1 | 3.1 | 2.0 (0.6–7.0) | NS |
| Fibromyalgia (%) | 0 | 1.2 | - | NS |
| Chronic fatigue syndrome (%) | 2.0 | 0.8 | 2.5 (0.3–21.4) | NS |
| Rheumatoid arthritis (%) | 4.1 | 4.0 | 1.0 (0.2–4.5) | NS |
| Chronic headache (%) | 12.2 | 3.3 | 4.1 (1.6–10.6) | <0.01 |
| Nut allergy (%) | 2.0 | 1.8 | 1.2 (0.1–9.0) | NS |
| Egg allergy (%) | 0 | 0.5 | - | NS |
| Lactose intolerance (%) | 2.0 | 1.4 | 1.5 (0.2–12.0) | NS |
| Inflammatory bowel disease (%) | 4.1 | 1.2 | 3.4 (0.7–16.3) | NS |
| Gastro-intestinal reflux disease (%) | 18.4 | 7.8 | 2.7 (1.2–5.8) | <0.05 |
| Psoriasis (%) | 4.1 | 2.0 | 2.0 (0.5–9.2) | NS |
| Variables | srGS (n = 49) (6.2%) | Controls (n = 734) (93.5%) | Odds Ratio (95% CI) | p-Value |
|---|---|---|---|---|
| Celiac disease in all relatives (%) | 8.2 | 2.5 | 3.4 (1.1–10.6) | <0.05 |
| Celiac disease in children of srGS individuals (%) | 6.1 | 0.4 | 15.9 (3.1–80.3) | <0.01 |
| Rheumatoid arthritis (%) | 30.6 | 20.2 | 1.7 (0.9–3.3) | NS |
| Diabetes mellitus (young age onset) (%) | 14.3 | 7.6 | 2.0 (0.9–4.7) | NS |
| Thyroid disease (%) | 20.4 | 8.9 | 2.6 (1.3–5.5) | <0.05 |
| Psoriasis (%) | 8.2 | 7.1 | 1.2 (0.4–3.4) | NS |
| Inflammatory bowel disease (%) | 6.1 | 2.2 | 2.9 (0.8–10.4) | NS |
| Irritable bowel syndrome (%) | 26.5 | 6.7 | 5.0 (2.5–10.1) | <0.001 |
| Variables | Self-Reported Gluten Sensitivity (n = 49) (6.2%) | Controls (n = 734) (93.5%) | Odds Ratio (95% Confidence Interval) | p-Value |
|---|---|---|---|---|
| Legume (%) | 24.5 | 2.7 | 11.6 (5.3–25.5) | <0.001 |
| Cabbage (%) | 36.7 | 7.2 | 7.5 (3.9–14.2) | <0.001 |
| Onion (%) | 38.8 | 10.2 | 5.6 (3.0–10.4) | <0.001 |
| Leek (%) | 32.7 | 5.3 | 8.6 (4.4–17.0) | <0.001 |
| Cauliflower (%) | 22.4 | 3.4 | 8.2 (3.8–17.9) | <0.001 |
| Mushroom (%) | 12.2 | 2.3 | 5.9 (2.2–15.7) | <0.01 |
| Apple (%) | 10.2 | 2.0 | 5.4 (1.9–15.7) | <0.01 |
| Cherry (%) | 2.0 | 0.5 | 3.8 (0.4–34.7) | NS |
| Sugar-free gum (%) | 12.2 | 2.7 | 5.0 (1.9–13.0) | <0.01 |
| Plum (%) | 10.2 | 3.3 | 3.4 (1.2–9.2) | <0.05 |
| Pear (%) | 8.2 | 1.8 | 4.9 (1.5–15.7) | <0.05 |
| Mango (%) | 2.0 | 0.4 | 5.1 (0.5–49.7) | NS |
| Watermelon (%) | 4.1 | 0.3 | 15.6 (2.1–113.0) | <0.05 |
| Milk (%) | 20.4 | 4.6 | 5.3 (2.4–11.5) | <0.001 |
| Buttermilk (%) | 8.2 | 2.0 | 4.3 (1.4–13.4) | <0.05 |
| Yogurt (%) | 14.3 | 3.3 | 4.9 (2.0–12.1) | <0.01 |
| Custard (%) | 18.4 | 1.8 | 12.5 (5.0–30.9) | <0.001 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van Gils, T.; Nijeboer, P.; IJssennagger, C.E.; Sanders, D.S.; Mulder, C.J.J.; Bouma, G. Prevalence and Characterization of Self-Reported Gluten Sensitivity in The Netherlands. Nutrients 2016, 8, 714. https://doi.org/10.3390/nu8110714
Van Gils T, Nijeboer P, IJssennagger CE, Sanders DS, Mulder CJJ, Bouma G. Prevalence and Characterization of Self-Reported Gluten Sensitivity in The Netherlands. Nutrients. 2016; 8(11):714. https://doi.org/10.3390/nu8110714
Chicago/Turabian StyleVan Gils, Tom, Petula Nijeboer, Catharina E. IJssennagger, David S. Sanders, Chris J. J. Mulder, and Gerd Bouma. 2016. "Prevalence and Characterization of Self-Reported Gluten Sensitivity in The Netherlands" Nutrients 8, no. 11: 714. https://doi.org/10.3390/nu8110714
APA StyleVan Gils, T., Nijeboer, P., IJssennagger, C. E., Sanders, D. S., Mulder, C. J. J., & Bouma, G. (2016). Prevalence and Characterization of Self-Reported Gluten Sensitivity in The Netherlands. Nutrients, 8(11), 714. https://doi.org/10.3390/nu8110714




