Transcultural Diabetes Nutrition Algorithm (tDNA): Venezuelan Application
Abstract
:1. Introduction
2. Transcultural Factors for Venezuela
2.1. Geographic, Demographic, Cultural, and Regional Characteristics of Venezuela
2.2. Non-Communicable Diseases in Latin America and Venezuela
2.3. Healthcare System in Venezuela
2.4. Cardio-Metabolic Comorbidities and Related Risk Factors: Venezuelan Disparities by Gender, Region, Ethnicity, and Population (Urban vs. Rural)
2.5. Physical Activity in Venezuela
| Region | Obesity (%) | Diabetes (%) | Prediabetes (%) | Hypertension (%) | Dyslipidemia (%) | Metabolic Syndrome (%) | Physical Inactivity (%) | Typical Foods | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| High Cholesterol | High LDL | Low HDL | High Triglycerides | Atherogenic Dyslipidemia | ||||||||
| Capital | 35.0 U, M *,a [24] 30.0 U, M *,a [24] | 9.5 U, M *,a [25] 8.0 U, M * [26] 6.7 U, O *,a [27] | 9.0 U, M *,a [25] 10.0 U, M * [26] | 34.0 U, M * [26] 43.4 U, O *,a [27] | 51.6 U, O *,a [27] 33.0 U, O a [28] | 81.1 U, O *,a [27] 56.0 U, O *,a [25] 42.9 U, M *,a [26] 4 4.0 U, O a [28] | 43.0 U, M *,a [25] 31.4 U, M * [26] 51.3 U, O *,a [27] 34.0 U, O a [28] | 45.5 U, O *,a [27] 20.0 U, M *,a [26] 37.0 U, O *,a [25] 33.6 U, C *,a [29] | 31.5 U, O [30] Ma: 9.0, Fe: 34.0 U, O [31] | Roasted or stewed chicken, beef or fish. With rice, pasta and salad. Italian, French and Portuguese influence | ||
| Central | 39.0 U, O [32] | 9.0 U, O [32] | 28.1 U, O [32] | 59.0 U, O [32] | 25.0 U, O [32] | 90.0 U, O [32] | 51.0 U, O [32] | |||||
| Western | 25.1 U,C * [20] 26.7 U, M * [33] | 6.0 U, C * [2] 11.0 U, M * [33] | 15.8 U, M * [33] 1.0 U, C * [2] | 23.6 U, C * [34] 24.7 U, C * [20] 29.0 UR, S * [35] 28.3 U, M * [33] | 5.7 U, C * [20] 24.8 U, M * [33] | 26.0 U, M * [33] | 68.7 U, M * [33] | 49.0 U, M * [33] | 36.9 U, M * [33] | 34.9 U, M * [33] 25.8 U, C * [20] | Sheep, goat and rabbit meat. Cheese and milk whey | |
| Andeans | 12.1 R, M * [30] 24.3 U, M * [33] | 8.6 R, M * [30] 14.9 U, M * [33] | 18.6 U, M * [30] 4.5 U, M * [33] | 25.4 R, M * [36] 34.4 U, M * [33] | 11.6 U, M * [33] 22.1 R, M * [36] 33.0 U, C * [37] | 14.6 U, M * [33] 13.9 R, M * [36] | 43.1 R, M * [36] 69.6 U, M * [33] 76.0 U, C * [37] | 45.0 R, M * [36] 39.5 U, M * [33] 56.0 U, C * [37] | 16.8 R, M * [36] 26.6 U, M * [33] | 26.7 U, R * [30] 38.5 U, C * [37] 27.6 U, M * [38] 23.8 U, M * [33] | Potatoes, wheat and tuber. Beef, sheep and chicken meat. Fish (cultured trout). Similar to other Andean regions | |
| Zulia | ND | Ma:7.8, Fe:7.4 S, U * [3] | Ma: 19.6, Fe: 14.9 S, U * [3] | 36.9 U, C * [39] | 39.3 U, O [40] Ma: 40.2, Fe: 46.0 U, O [41] | 65.3 UR, S [3] | 32.3 UR, S [3] 55.9 U, O [40] Ma: 47.8, Fe: 12.2 U, O [41] | 26.0 UR, S * [3] | 31.2 S, U * [3] 32.1 U, O [40] | 71.3 UR, S * [3] | Platain (patacón), fried wheat cake | |
| North-Eastern | ND | ND | N|D | ND | ND | ND | ND | ND | ND | ND | ND | River and sea fish, seafood, shrimp, lobster. Tuber as yam, potatoes, ocumo. Sea food rice (paella) |
| Guayana | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | Guayanés cheese, fried fish with arepa, rice, salad and sliced plantain (tajadas) |
| Llanos | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | Beef, deer, chiguire, turtle and lapa meat. Barbecue with cachapas, cheese and milk cream |
2.6. Aspects of Nutrition in Venezuelan (Dietary Habits, Food Availability, Typical Foods, and Their Glycemic Indices)
| Current Typical Day Menu 1 | Current Typical Day Menu 2 | Recommended Menu Mediterranean-Like | |||
|---|---|---|---|---|---|
| Breakfast | Servings | Breakfast | Servings | Breakfast | Servings |
| Fried empanadas | 2 units (200 g) | Fried empanadas | 2 units (200 g) | Oat with low fat milk | ½ cup (120 cc) |
| Low fat milk | ½ glass (120 cc) | ||||
| Coffee with milk | 1 cup | Malta | 222 cc | Oat | 1 spoon (7 g) |
| Sugar | 1 spoon (12 g) | Sugar | 1 spoon (12 g) | ||
| Integral bread | 2 slices (50 g) | ||||
| Goat cheese | 6 spoon (30 g) | ||||
| Orange slides | 1 unit (150 g) | ||||
| Natural fruit juice | 1 glass (240 cc) | ||||
| Paw | 1 cup (150 g) | ||||
| Sugar | ½ spoon (6 g) | ||||
| Black coffee | 1 cup | ||||
| Lunch | Servings | Lunch | Servings | Lunch | Servings |
| Beef steak | 210 g | Fried chicken | 210 g | Black Beans soap | ½ cup (180 cc) |
| Pasta | 1 cup (170 g) | White rice | 1 cup (170 g) | Meat shredded | 1 cup (130 g) |
| Fried plantain (Tajada) | 1/4 unit (75 g) | Fried plantain (Tajada) | 1/4 unit (75 g) | Green (species) | ¼ cup (10 g) |
| Banana | 1 unit (200 g) | Banana | 1 unit (200 g) | White rice | ½ cup (100 g) |
| White bread | 1 unit (35 g) | White bread | 1 unit (35 g) | Mix salad | 3 cup |
| Soda | 1 glass (240 cc) | Natural fruit juice | 1 glass (240 cc) | Tomato | 1 cup (80 g) |
| Coffee with milk | 1 unit | Melón | 1 cup (150 g) | Lettuce | 1 cup (80 g) |
| Sugar | 1 spoon (12 g) | Sugar | 1 spoon (12 g) | Onion | 1 cup (80 g) |
| Avocado | ¼ unit (50 g) | ||||
| Olive Oil | 2 spoon (7 cc) | ||||
| Cut fruit | 1 cup (200 g) | ||||
| Melón | 1 cup (150 g) | ||||
| Sugar | ½ spoon (10 g) | ||||
| Snack | |||||
| Salad fruit (Tizana) | 1 cup (200 g) | ||||
| Dinner | Servings | Dinner | Servings | Dinner | Servings |
| Arepa with white cheese | 2 unit (240 g)/60 g | Arepa with white cheese | 2 unit (240 g)/60 g | Mix of vegetables | 2 spoon |
| Margarine | 2 slides (600 g) | Margarine | 2 slides (60 g) | Onion | 1 cup (80 g) |
| Coffe with milk | 1 cup | Soda | 1 glass (240 cc) | Tomato | 1 cup (80 g) |
| Sugar | 1 spoon (12 g) | Capsicum | 1 cup (170 g) | ||
| Fish or tuna | 1 slide or 1 cup (170 g) | ||||
| Arepa | 1 unit (100 g) | ||||
| Whole fruit | 1 cup (150 g) | ||||
| Menu Composition | Menu Composition | Menu Composition | |||
| Nutrient | Content | Nutrient | Content | Nutrient | Content |
| Energy (kcal) | 2785 | Energy (kcal) | 3174 | Energy (kcal) | 1734 |
| Carbs (g/% of Energy ) | 366.5/46 | Carbs (g/% of Energy ) | 356/44 | Carbs (g/% of Energy ) | 220.7/50 |
| Lipid (g/% of Energy) | 147.2/41 | Lipid (g/% of Energy) | 155/44 | Lipid (g/% of Energy) | 41.0 /29 |
| Protein (g/% of Energy) | 104/13 | Protein (g/% of Energy) | 93/12 | Protein (g/% of Energy) | 126.0/21 |
| Fiber (g) | 17.4 | Fiber (g) | 18.6 | Fiber (g) | 46.2 |
| Cholesterol (mg) | 277 | Cholesterol (mg) | 244 | Cholesterol (g) | 221 |
| Sodium (mg) | 1643 | Sodium (mg) | 1551 | Sodium (mg) | 839 |
| Carbohydrate Foods | Glycemic Index | Carbohydrate Foods | Glycemic Index |
|---|---|---|---|
| Glucose | 100 | Fruits | |
| Common foods | Banana | 59 | |
| Casabe | 118 | Papaya | 50 |
| Tapioca (yuca) | 108 | Pineapple | 41 |
| Bread | 98 | Mango | 36 |
| Arepa | 74 | Tangerine | 36 |
| Brown sugar cane | 71 | Watermelon | 34 |
| Pasta | 59 | Vegetables | |
| Legumes | Potato | 93 | |
| Black beans | 51 | Platain | 78 |
2.7. Body Composition and Cardio-Metabolic Risk, Genetic, and Ethnic Particularities in Venezuelan Population
| Category | BMI, kg/m2 | Obesity Class | Disease Risk | |
|---|---|---|---|---|
| WC: M ≤ 94 cm F ≤ 90 cm | WC: M > 94 cm F > 90 cm | |||
| Underweight | <18.5 | |||
| Normal | 18.5–24.9 | |||
| Overweight | 25.0–27.4 | Increased | High | |
| Obesity | 27.5–34.9 | I | High | Very high |
| 35.0–39.9 | II | Very high | Very high | |
| ≥40 | III | Extremely high | Extremely high | |
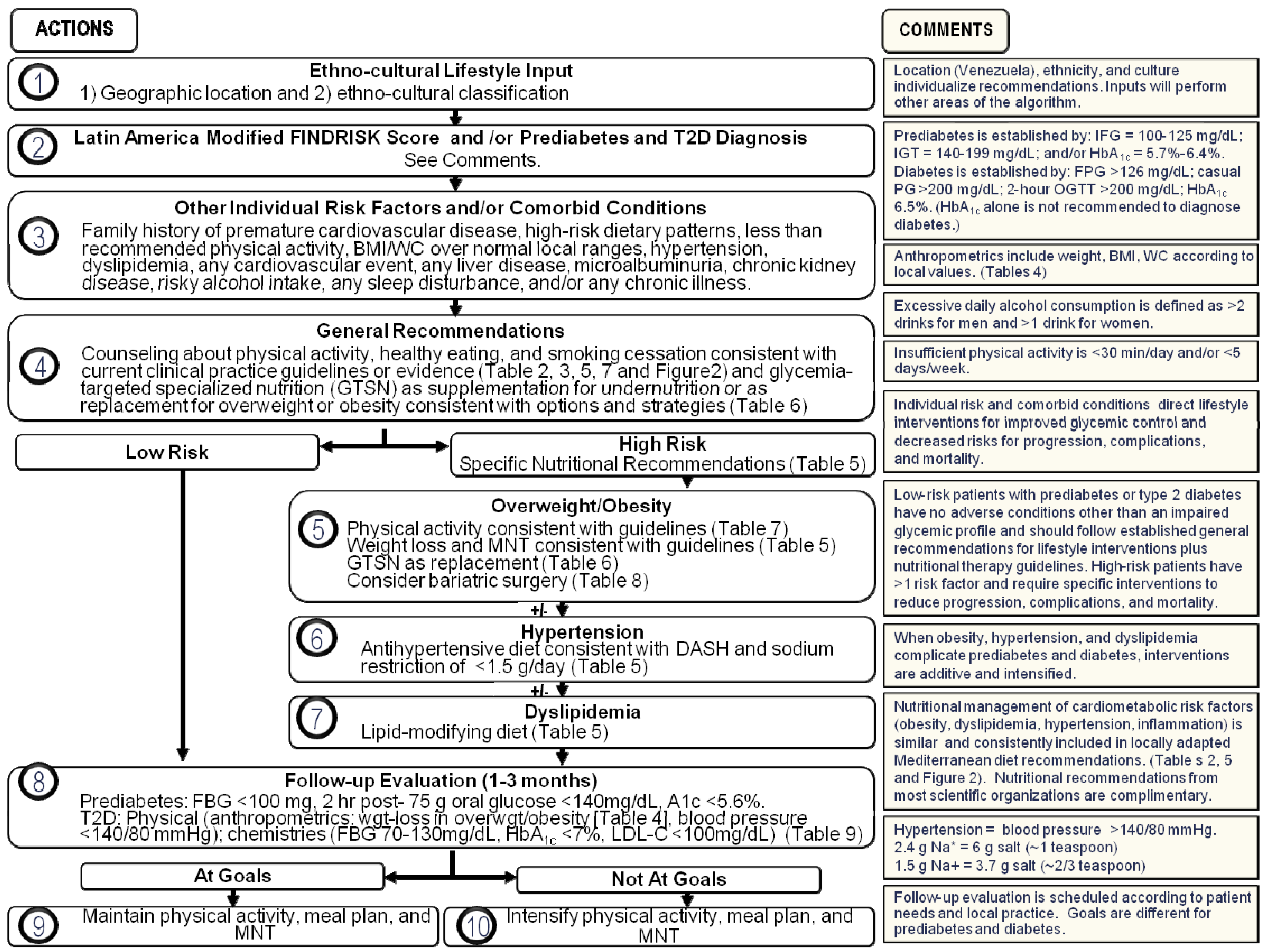
3. Current Local CPG and Proposed Recommendations
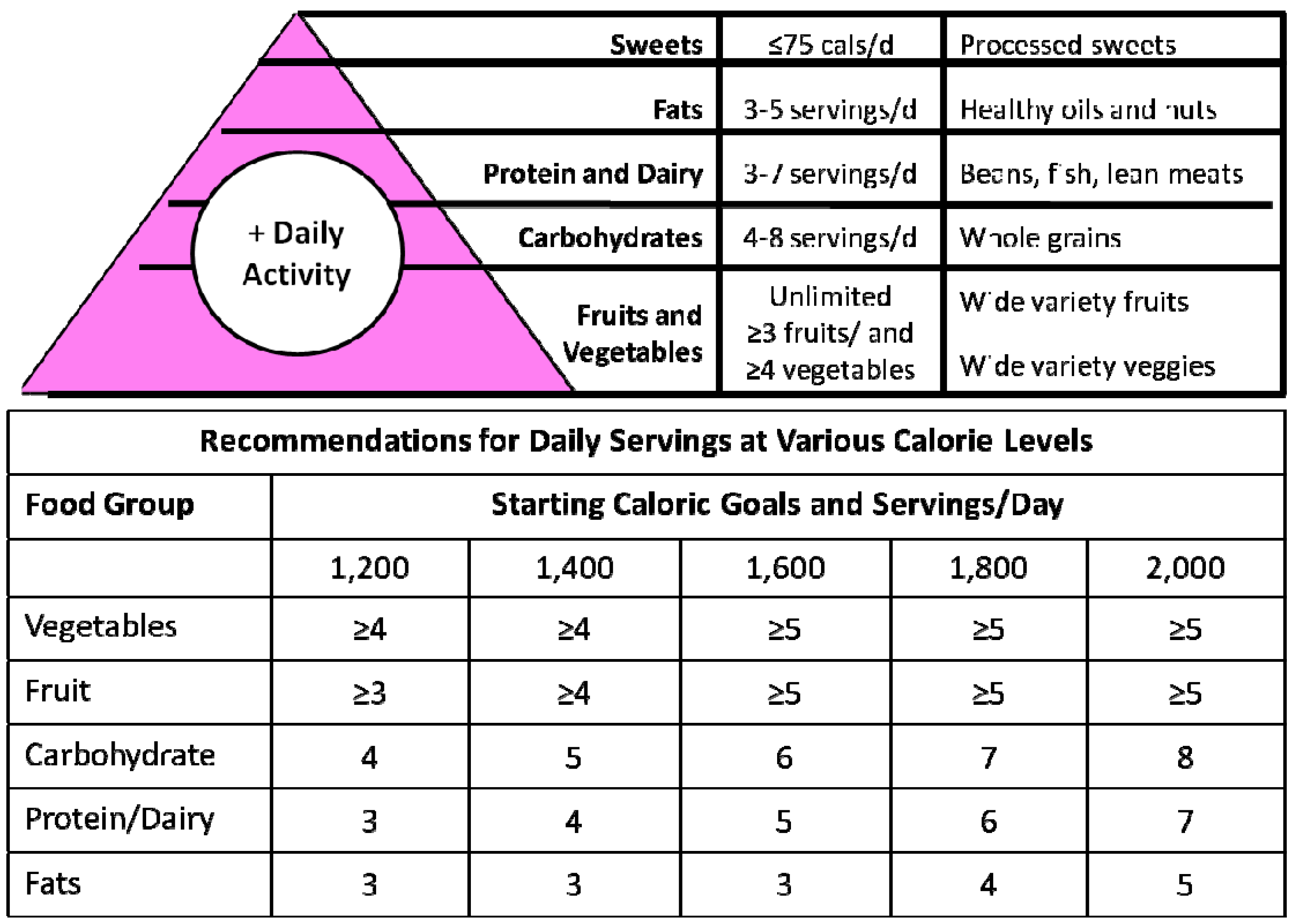
3.1. Medical Nutrition Therapy (MNT) Recommendations in T2D and Co-Morbidities
| Nutrient a | ADA b/AACE [85,86] | ALAD [8] | FENADIABETES [87] | Proposed recommendations |
|---|---|---|---|---|
| Calories | Deficit: 500–1000 kcal/day; Target: decrease weight by 5%–10% for overweight and obese individuals | Restriction: 25–30; Maintenance: 30–35 | Deficit: 500–1000 kcal/day; Target: weight loss of 5% in 3 months or 10% in 6 months for overweight and obese individuals | |
| Carbohydrate | 45%–65% daily energy intake and not <130 g/day | 40%–60% | 45%–65% | 45%–55% |
| Protein | 15%–20% daily energy intake | 15%–30%No less than <1 g/kg | 0.8–1 g (80% HBV) | 15%–20% 0.8%–1.2 g/kg (80% HBV) |
| Fat | 20%–35% daily energy intake | 30%–45% | 25%–35% | 25%–30% |
| Saturated fat | <7% daily energy intake | ˂7% | 7–10 g/day | <7% 7–10 g/day |
| Cholesterol | <200 mg/day | ≤200 mg/day | <200 mg/day | |
| Fiber | 25–50 g/day | 14 g/1000 cal | 25–35 g/1000 cal (5%–10% soluble fiber) | |
| Trans fat | Minimize or eliminate | <1% | Minimize or eliminate | |
| Sodium c | <2300 mg/day | 1 g/1000 cal | 1 g/1000 cal |
3.2. Diabetes-Specific Formulas to Facilitate Metabolic Control
| Overweight/Obese | Use 2–3 GTSN a as part of a reduced calorie meal plan, as a calorie replacement for meal, partial meal or snack Calorie goals: <113 kg b = 1200 to 1500 cal; >113 kg b = 1500 to 1800 cal; Calories from GTSN. Calories from other healthy dietary source | |
| Normal Weight | Uncontrolled diabetes c A1c > 7% | 1–2 GTSN per day to be incorporated into a meal plan, as a calorie replacement for meal, partial meal or snack |
| Controlled diabetes c A1c < 7% | Use of GTSN should be based on clinical judgment and individual assessment d | |
| Under weight | Use GTSN supplements e 1–3 units/day per clinical judgment based on desired rate of weight gain and clinical tolerance | |
3.3. Physical Activity Recommendations
3.4. Bariatric Surgery Indications
| Type of exercise: Aerobic Resistance Stretching (Flexibility) Balance General physical activity | Intensity Level | |||||
|---|---|---|---|---|---|---|
| Low | Medium | High | ||||
| Aerobic | Resistance | Aerobic | Resistance | Aerobic | Resistance | |
| (<40% of HRmax, or <2.9 METS) | 3 Big Muscle Groups | (40%–59% of HRmax, or 3.0–5.9 METS) | 5 Big Muscle Groups | (≥60% of HRmax, or ≥6.0 METS) | 10 Muscle Groups | |
| Activity | Slow walking, swimming, stationary cycling, dancing | Bands (Quadriceps, biceps, triceps) | Vigorous walking, jogging, stair climbing, swimming, cycling, elliptical, fast dancing | Bands, weightlifting (dumbbells) (Quadriceps, biceps, triceps, calves, hamstrings ) | Running, stair climbing, hill walking or more intense cycling, dancing, swimming | Bands, Weightlifting(dumbbells and/or gym machines)(Ten muscle groups a ) |
| Duration | ≥10 min | - | ≥30 min | - | ≥60 min | - |
| Set × reps × rest (min) | - | 2 × 10 × 2 | - | 3 × 15 × (1–2) | - | 3 × 15 × 2 |
| Frequency | 3×/week | 2×/week | (3–4)×/week | 3×/week | ≥5×/week | (3–4)×/week |
| Stretching for maintaining flexibility and range of motion of joints is recommended after each exercise session. This can be achieved by passively (with the aid of the opposite limb, or by another person) or actively (using the agonist-antagonist muscle contraction). | ||||||
| General physical activity: Use the stairs in the workplace. Subjects, who have practiced a sport in the past should be encouraged to take up this activity again after achieving an acceptable fitness level. Pedometer: 3000 to 7000 steps per day (individualized) | ||||||
| Place: Select safer places to exercise. Walking or jogging on treadmills, stationary cycling, dancing, elliptical, bands, and weight lifting with dumbbells can be performed at home. Outdoor exercises such as jogging and cycling should be performed in organized groups. Only few options such as weight lifting using machines could require a gym. | ||||||
| The initial intensity level should be selected based on age, presence of comorbidities and/or musculoskeletal limitations and fitness level of each subject. Older, less trained and/or subjects with limited mobility should start exercising at a low intensity level. | ||||||
| BMI ≥ 40 kg/m2 |
| BMI 35–39.9 kg/m2 and an obesity-related comorbidity, such as T2D, coronary heart disease, or severe sleep apnea. |
| BMI 30–34.9 kg/m2 under special circumstances —When diabetes is not adequately controlled by a medical regimen and especially when there are cardiovascular disease risk factors. |
| —Consideration may be given to laparoscopic-assisted gastric sleeve in patients with T2D who have a BMI > 30 kg/m2 or Roux-en-Y gastric bypass for patients with a body BMI > 35 kg/m2 to achieve at least short-term weight reduction. —And for each of the above: Failure to achieve and sustain weight loss after attempts at supervised lifestyle modification for at least six months; Tolerable operative risks; Understanding of operation; Commitment to treatment and long-term follow-up; Acceptance of required lifestyle changes; Diagnostic of psychiatric conditions; Suitable life expectancy. |
3.5. Follow-Up Evaluation
4. Factors Affecting TDNA Implementation
4.1. Changes in Food Intake, Medical Appointments, and Treatment Adherence during Holidays
4.2. Misconception of Obesity as an Esthetic Problem
4.3. Misconceptions Surrounding Insulin
4.4. Misuse of Metformin and Other Drugs in the Treatment of Obesity
| Category | Current Situations and Behaviors | Proposed tDNA Recommendations |
|---|---|---|
| Health system | Fragmented | Utilization of integrated health service delivery networks to educate primary care physicians to implement tDNA |
| Nutrition |
|
|
| Physical activity |
|
|
| Anthropometry and body composition |
|
|
| Diagnosis and risk identification |
|
|
| Pharmacologic treatment |
|
|
| Obesity |
|
|
| Bariatric surgery |
|
|
| Other general considerations |
|
|
5. Conclusions
Acknowledgments
Disclosures
Conflicts of Interest
References
- IDF (2011) International Diabetes Federation Diabetes Atlas. Diabetes Estimates Excel Tables. 2011. Available online: http://www.idf.org (accessed on 14 October 2012).
- Escobedo, J.; Buitrón, L.V.; Velasco, M.F.; Ramírez, J.C.; Hernández, R.; Macchia, A.; Pellegrini, F.; Schargrodsky, H.; Boissonnet, C.; Champagne, B.M.; et al. High prevalence of diabetes and impaired fasting glucose in urban Latin America: The CARMELA Study. Diabet. Med. 2009, 26, 864–871. [Google Scholar] [CrossRef]
- Florez, H.; Silva, E.; Fernández, V.; Ryder, E.; Sulbarán, T.; Campos, G.; Calmón, G.; Clavel, E.; Castillo-Florez, S.; Goldberg, R. Prevalence and risk factors associated with the metabolic syndrome and dyslipidemia in White, Black, Amerindian and Mixed Hispanics in Zulia State, Venezuela. Diabetes Res. Clin. Pract. 2005, 69, 63–77. [Google Scholar] [CrossRef]
- González, J.P.; Nieto-Martínez, R.; Molina, T.; García, R.J.; Ugel, E.; Osuna, D.; Salazar, L. Prevalencia de síndrome metabólico, obesidad y alteración de la glucemia en ayunas en adultos del páramo del Estado Mérida, Venezuela (estudio VEMSOLS). Med. Int. 2012, 28, 262–267. [Google Scholar]
- Duarte-Moreira, E.D., Jr.; Neves, R.C.; Nunes, Z.O.; de Almeida, M.C.; Mendes, A.B.; Fittipaldi, J.A.; Ablan, F.; Venezuelan Diabetes Investigators’ Group. Glycemic control and its correlates in patients with diabetes in Venezuela: Results from a nationwide survey. Diabetes Res. Clin. Pract. 2010, 87, 407–414. [Google Scholar] [CrossRef]
- Mechanick, J.I.; Marchetti, A.E.; Apovian, C.; Benchimol, A.K.; Bisschop, P.H.; Bolio-Galvis, A.; Hegazi, R.A.; Jenkins, D.; Mendoza, E.; Sanz, M.L.; et al. Diabetes-specific nutrition algorithm: A transcultural program to optimize diabetes and prediabetes care. Curr. Diabetes Rep. 2012, 12, 180–194. [Google Scholar]
- INE, Instituto Nacional de Estadísticas. República Bolivariana de Venezuela. Censo 2011. Available online: http://www.ine.gov.ve/ (accessed on 12 September 2012).
- Guías ALAD Sobre el Diagnóstico, Control y Tratamiento de la Diabetes Mellitus Tipo 2 con Medicina Basada en Evidencia. Available online: http://issuu.com/alad-diabetes/docs/guias_alad_2013 (accessed on 12 February 2014).
- OPS. Salud en la Américas. Organización Panamericana de la Salud; Publicación Científica y Técnica No. 622 II-Países: Washington, DC, USA, 2006; pp. 770–784. [Google Scholar]
- Pan American Health Organization. Technical Reference Document on Non-communicable Disease Prevention and Control. July 2011. Available online: http://new.paho.org/hq/index.php?option=com_docman&task=doc_view&gid=14815&Itemid= (accessed on 6 October 2012).
- Health in the Americas. Scientific and Technical Publication No. 636. 2012 Edition. Available online: http://health-equity.blogspot.com/2012/09/eq-paho-health-in-americas-2012-edition.html (accessed on 14 October 2012).
- Prevention and Control of Non-Communicable Diseases. Report of the Secretary-General. Follow-Up to the Outcome of the Millennium Summit A/66/83. Available online: http://www.un.org/ga/search/view_doc.asp?symbol=A/66/83&Lang=E (accessed on 1 September 2012).
- WHO. World Health Statistics 2012, Part III: Global Health Indicators. Available online: http://www.who.int/gho (accessed on 2 September 2012).
- Rodriguez, T.; Malvezzi, M.; Chatenoud, L.; Bosetti, C.; Levi, F.; Negri, E.; La Vecchia, C. Trends in mortality from coronary heart and cerebrovascular diseases in the Americas: 1970–2000. Heart 2006, 92, 453–460. [Google Scholar]
- Ciruzzi, M.; Schargrodsky, H.; Pramparo, P.; Rivas Estany, E.; Rodriguez Naude, L.; de la Noval Garcia, R.; Gaxiola Cazarez, S.; Meaney, E.; Nass, A.; Finizola, B.; et al. Attributable risks for acute myocardial infarction in four countries of Latin America. Medicina 2003, 63, 697–703. [Google Scholar]
- Lanas, F.; Avezum, A.; Bautista, L.E.; Diaz, R.; Luna, M.; Islam, S.; Yusuf, S. Risk factors for acute myocardial infarction in Latin America: The INTERHEART Latin American study. Circulation 2007, 115, 1067–1074. [Google Scholar] [CrossRef]
- Case, C.; Brito, S.; Palma, A.; Lares, M.; Pérez, E. Factores de riesgo asociados a diabetes mellitus tipo 2 en indios waraos del delta amacuro, Venezuela. Interciencia 2006, 31, 309–311. [Google Scholar]
- Garcia-Araujo, M.; Semprún-Fereira, M.; Sulbarán, T.A.; Silva, E.; Calmón, G.; Campos, G. Nutritional and metabolic factors as risk factors for cardiovascular diseases in an adult population in the city of Maracibo, Estado Zulia, Venezuela. Investig. Clin. 2001, 42, 23–42. [Google Scholar]
- Ryder, E.; Hernández-Hernández, R.; Champagne, B.M.; Silva, H.; Vinueza, R.; Silva Ayçaguer, L.C.; Touboul, P.J.; Boissonnet, C.P.; Escobedo, J.; Pellegrini, F.; et al. Black Hispanics have a worse cardiovascular risk profile than mixed Hispanics in Venezuela. Investig. Clin. 2007, 48, 45–55. [Google Scholar]
- Schargrodsky, H.; Hernández-Hernández, R.; Champagne, B.M.; Silva, H.; Vinueza, R.; Silva Ayçaguer, L.C.; Touboul, P.J.; Boissonnet, C.P.; Escobedo, J.; Pellegrini, F.; et al. CARMELA: Assessment of cardiovascular risk in seven Latin American cities. Am. J. Med. 2008, 121, 58–65. [Google Scholar] [CrossRef]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T.; Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U.; Lancet Physical Activity Series Working Group. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- Granero, R.; Poni, E.; Sánchez, Z. Patrones de actividad física durante tiempo de ocio entre estudiantes del séptimo al noveno grado en el Estado Lara, Venezuela. Av. Cardiol. 2007, 27, 160–167. [Google Scholar]
- Brajkovich, I.; Arismendi, Z.; Benedetti, P.; Crocce, N.; Escudero, P.; Escauriza, M.; España, M.; González, R.; Khawan, R.; Márquez, M.; et al. Prevalencia de sobrepeso y obesidad en una población de Catia La Mar (Edo. Vargas) y Municipio Sucre Distrito Metropolitano de Caracas. Rev. Venezol. Endocrinol. Metab. 2006, 4, 32. [Google Scholar]
- Brajkovich, I.; González, R.; Peña, N.; Suarez, M.; Terrones, O.; Crocce, N.; Rizquez, A.; Millán, A. Prevalencia de Síndrome Metabólico en una muestra poblacional del Estado Vargas. Noviembre 2005–Enero 2006 (Ambulatorio de Vía Eterna, Catia La Mar; Sector I, Parroquia Raúl Leoni. Estado Vargas). Rev. Venezol. Endocrinol. Metab. 2006, 4, 31. [Google Scholar]
- Brajkovich, I.; Arismendi, Z.; Benedetti, P.; Escudero, P.; Escauriza, M.; España, M.; Khawan, R.; Marquez, M.; Megadja, M.; Millán, A.; et al. Prevalencia de síndrome metabólico en el Municipio Sucre, Estado Miranda, distrito metropolitano de Caracas. Rev. Venezol. Endocrinol. Metab. 2006, 4, 31. [Google Scholar]
- De Oliveria, L.; García, E.; Torres, J.; Rivas, A. Prevalencia de síndrome metabólico en el sector Olivett. El Junquito. Rev. Venezol. Endocrinol. Metab. 2006, 4, 3. [Google Scholar]
- García, R.S.; Roa, M.; Zavala, N.; Nuñez, R.; Alfieri, A.B.; Cubeddu, L.X.; Hoffman, I.S. Niveles de LDL-colesterol, HDL-colesterol y triglicéridos en una muestra poblacional de la Gran Caracas, distribuidos por sexo y por edad. Rev. Venezol. Endocrinol. Metab. 2006, 4, 27. [Google Scholar]
- Lunar, L.; Serafin, M.; da Silva, R. Prevalencia del síndrome metabólico en Venezuela: El estudio sind-Met Venezuela. Rev. Venezol. Endocrinol. Metab. 2006, 4, 33. [Google Scholar]
- Moya-Sifontes, M.; García-Avendaño, P.; Lucena, N.; Casañas, R.; Brito, P.; Rodríguez, A.; Flores, Z.; Cordero, R. Hipocinetismo: Un problema de salud entre jóvenes ucevistas? Rev. Fac. Med. 2006, 29, 74–79. [Google Scholar]
- Pérez-Correa, N.G.; Moya-Sifontes, M.; Bauce, G.; García, P.; Cueva, E.; Peña, R.; Flores, Z. Patrones alimentarios y niveles de actividad física en estudiantes de la Universidad Central de Venezuela. Rev. Esp. Nutr. Comun. 2009, 15, 129–144. [Google Scholar]
- Ruiz-Fernández, N.; Espinoza, M.; Barrios, E.; Reigosa, A. Factores cardiometabólicos en una comunidad de Valencia, Venezuela. Rev. Salud Públ. 2009, 11, 383–394. [Google Scholar]
- Nieto-Martínez, R.; González, J.P.; Ugel, E. Estudio Venezolano de Síndrome Metabólico, Obesidad y Estilo de Vida (Estudio VEMSOLS). Unplublished work. 2013. [Google Scholar]
- Hernández, R.; Chacón-Ramírez, L.A.; Hernández-Farazo, A.; Aguero, R.E.; Hernández-Faraco, G.; Armas-Hernández, M.J.; Armas-Padilla, M.C.; Guerrero-Puente, J. Estudio de la prevalencia de la hipertensión arterial en Barquisimeto, Venezuela. Bol. Méd. Postgrado 1994, 10, 1–11. [Google Scholar]
- Granero, R.; Finizola, B.; Infante, E. Tendencias en hipertension arterial en el Estudio de la Salud Cardiovascular del Estado Lara (ESCEL), Venezuela 1987 y 1997. Av. Cardiol. 2004, 24, 85–89. [Google Scholar]
- Nieto-Martínez, R.E.; González, J.P.; García, R.J.; Ugel, E.; Osuna, D.; Salazar, L. Prevalencia de hipertensión arterial y dislipidemias en adultos del páramo del Estado Mérida y su relación con obesidad. Resultados preliminares del estudio VEMSOLS. Av. Cardiol. 2011, 31, 193–200. [Google Scholar]
- Becerra-Leal, A.V.; Lenin-Valery, A.; Arata-Bellabarba, G.; Velásquez-Maldonado, E.M. Prevalencia de síndrome metabólico en la población urbana de Mucuchíes, Mérida-Venezuela. Rev. Venez. Endocrinol. Metab. 2009, 7, 16–22. [Google Scholar]
- Uzcátegui Pinto, E.; Baptista, T.; Carrizo, E.; Valeri, L.; Uzcátegui, L.R.; Gómez Pérez, R. Prevalencia del síndrome metabólico en sujetos de la población general, área metropolitana, Municipio Libertador de la ciudad de Mérida, Venezuela 2006. Rev. Venez. Endocrinol. Metab. 2009, 7, 40. [Google Scholar]
- Sulbaran, T.; Silva, E.; Calmón, G.; Vegas, A. Epidemiologic aspects of arterial hypertension in Maracaibo, Venezuela. J. Hum. Hypertens. 2000, 14, S6–S9. [Google Scholar]
- Sirit, Y.; Acero, C.; Bellorin, M.; Portillo, R. Metabolic syndrome and other factors cardiovascular risk in workers of a plant of vinyl polychloride. Rev. Salud Publ. 2008, 10, 239–249. [Google Scholar] [CrossRef]
- Campos, G.; Ryder, E.; Diez-Ewald, M.; Rivero, F.; Fernández, V.; Raleigh, X.; Arocha-Piñango, C.L.; y Grupo para el Estudio del Fibrinógeno como Factor de Riesgo Coronario en Venezuela (FRICVE). Prevalencia de obesidad e hiperinsulinemia en una población aparentemente sana de Maracaibo, Venezuela y su relación con las concentraciones de lípidos y lipoproteínas del suero. Investig. Clin. 2003, 44, 15. [Google Scholar]
- Astrup, A.; Dyerberg, J.; Selleck, M.; Stender, S. Nutrition transition and its relationship to the development of obesity and related chronic diseases. Obes. Rev. 2008, 9, 48–52. [Google Scholar] [CrossRef]
- Joshi, S.R.; Mohan, V.; Joshi, S.S.; Mechanick, J.I.; Marchetti, A. Transcultural diabetes nutrition therapy algorithm: The Asian Indian application. Curr. Diabetes Rep. 2012, 12, 204–212. [Google Scholar]
- INE. Instituto Nacional de Estadística. Available online: http://www.noticias24.com/venezuela/noticia/8401/ine-presento-los-resultados-de-la-encuesta-de-seguimiento-al-consumo-de-alimentos-desde-2003-a-2010 (accessed on 12 September 2012).
- Montilva, M.; Berné, Y.; Papale, J.; García-Casal, M.N.; Ontiveros, Y.; Durán, L. Perfil de alimentación y nutrición de mujeres en edad fértil de un Municipio del Centroccidente de Venezuela. Anal. Venez. Nutr. 2010, 23, 67–74. [Google Scholar]
- Calanche Morales, J.B. Influencias culturales en el régimen alimentario del venezolano. Anal. Venez. Nutr. 2009, 22, 32–40. [Google Scholar]
- Suárez, M.M.; Bosch, V.; Aliaga, C.; García, N. La empanada en Venezuela: Importancia social y nutricional. Anal. Venez. Nutr. 2010, 23, 88–99. [Google Scholar]
- Lago-Moneo, J. El Consumo de Comida Rápida. Situación en el Mundo y Acercamiento Autonómico. Available online: http://www.abc.es/gestordocumental/uploads/Sociedad/comida-rapida.pdf (accessed on 13 December 2013).
- BCV. IV Encuesta Nacional de Presupuestos Familiares y Hábitos Alimenticios del Venezolano: Principales Resultados. Available online: http://iies.faces.ula.ve/IV_ENPF/enpf.htm (accessed on 12 September 2012).
- Marin, M.; Vivas de Vegas, J. Elaboración de una estrategia para manejo nutricional de diabetes lipo 2 basada en tablas de Índice Glicémico. Rev. Venezol. Endocrinol. Metab. 2006, 4, 24. [Google Scholar]
- Izquierdo, M.; Oráa, E.; de los Ríos, V.; Drayer, R.; Urbina, D. Índice glucémico e insulinémico de alimentos ricos en carbohidratos. Rev. Venezol. Endocrinol. Metab. 2006, 4, 25. [Google Scholar]
- Herrera, N.; Reif, B.; Suárez, A.; Malo, M.; Castillo, H.A.; Ayala, A.; Melkon, R.; Negrín, S. El Alcohol y las Políticas Públicas en Venezuela; Organización Panamericana de la Salud: Caracas, Venezuela, 2009. [Google Scholar]
- Seale, J.P.; Seale, J.D.; Alvarado, M.; Vogel, R.L.; Terry, N.E. Prevalence of problem drinking in a Venezuelan native American population. Alcohol Alcohol. 2002, 37, 198–204. [Google Scholar] [CrossRef]
- WHO. United Nations, Data Range 1990–2006; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Negretti de Bratter, V.E.; Bratter, P.; Oliver, W.; Alvarez, N. Study of the Trace Element Status and the Dietary Intake of Mineral and Trace Elements in Relation to the Gastric Cancer Incidence in Tachira, Venezuela. Metal Ions in Biology and Medicine; Collery, P., Negretti de Bratter, V.E., Khassanova, L., Etienne, J.-C., Eds.; John Libbet Eurotext: Paris, France, 1998; pp. 557–565. [Google Scholar]
- Hoffmann, I.S.; Cubeddu, L.X. Increased blood pressure reactivity to dietary salt in patients with the metabolic syndrome. J. Hum. Hypertens. 2007, 21, 438–444. [Google Scholar]
- Aschner, P.; Buendía, R.; Brajkovich, I.; Gonzalez, A.; Figueredo, R.; Juarez, X.E.; Uriza, F.; Gomez, A.M.; Ponte, C.I. Determination of the cutoff point for waist circumference that establishes the presence of abdominal obesity in Latin American men and women. Diabetes Res. Clin. Pract. 2011, 93, 243–247. [Google Scholar] [CrossRef]
- Romero-Corral, A.; Somers, V.K.; Sierra-Johnson, J.; Thomas, R.J.; Collazo-Clavell, M.L.; Korinek, J.; Allison, T.G.; Batsis, J.A.; Sert-Kuniyoshi, F.H.; Lopez-Jimenez, F. Accuracy of body mass index in diagnosing obesity in the adult general population. Int. J. Obes. 2008, 32, 959–966. [Google Scholar] [CrossRef]
- Nieto-Martínez, R.; Pérez, Y.; Suárez, M.A.; Ugel, E. A BMI of 27.5 can improve the detection of obesity in a Venezuelan population. Diabetes 2013, 62, A750. [Google Scholar]
- Molero-Conejo, E.; Morales, L.M.; Fernández, V.; Raleigh, X.; Gómez, M.E.; Semprún-Fereira, M.; Campos, G.; Ryder, E. Lean adolescents with increased risk for metabolic syndrome. Arch. Latioam Nutr. 2003, 53, 39–46. [Google Scholar]
- Zambrano, M.; Fernández, E.; López, M.; Rangel, A.; de Romero, P.; Fernández, V.; Marina Morales, L.; Molero-Conejo, E.; Connell, L.; Raleigh, X.; et al. Gly482Ser polymorphism of the coactivator-1alpha of the activated receptor of peroxisome gamma proliferation in individuals from Maracaibo, Venezuela. Investig. Clin. 2009, 50, 285–294. [Google Scholar]
- Almarza, J.; Arráiz, N.; Bermúdez, V.; Prieto, C.; Escalona, C. Polimorfismos del gen UCP-3 en individuos con síndrome metabólico del Municipio Maracaibo-Venezuela. Rev. Venezol. Endocrinol. Metab. 2012, 10, 65–71. [Google Scholar]
- Ryder, E.; Gómez, M.E.; Fernández, V.; Campos, G.; Morales, L.M.; Valbuena, H.; Raleigh, X. Glucose/insulin response to a glucose overload in subjects at risk for type 2 diabetes. Investig. Clin. 2001, 42, 269–281. [Google Scholar]
- Ryder, E.; Gómez, M.E.; Fernández, V.; Campos, G.; Morales, L.M.; Valbuena, H.; Raleigh, X. Presence of impaired insulin secretion and insulin resistance in normoglycemic male subjects with family history of type 2 diabetes. Diabetes Res. Clin. Pract. 2003, 60, 95–103. [Google Scholar] [CrossRef]
- López, J.E.; Urbaneja, H. Tolerancia a la glucosa e insulinemia en hermanos asintomáticos de pacientes diabéticos tipo 2. Gac. Méd. Caracas 2006, 114, 305–317. [Google Scholar]
- Lindstrom, J.; Tuomilehto, J. The diabetes risk score: A practical tool to predict type 2 diabetes risk. Diabetes Care 2003, 26, 725–731. [Google Scholar] [CrossRef]
- Aschner, P.; Nieto-Martínez, R.; Marín, A.; Ríos, M. Validation of the Findrisk score as a screening tool for people with impaired glucose regulation in Latin America using modified score points for waist circumference according to the validated regional cutoff values for abdominal obesity. Minerva Endocrinol. 2012, 37, 114. [Google Scholar]
- Chiuve, S.E.; McCullough, M.L.; Sacks, F.M.; Rimm, E.B. Healthy lifestyle factors in primary prevention of coronary heart disease among men. Circulation 2006, 114, 160–167. [Google Scholar] [CrossRef]
- Reeves, M.J.; Rafferty, A.P. Healthy lifestyle characteristics among adults in the United States 2000. Arch. Intern. Med. 2005, 165, 854–857. [Google Scholar] [CrossRef]
- Tuomilehto, J.; Lindström, J.; Eriksson, J.G.; Valle, T.T.; Hämäläinen, H.; Ilanne-Parikka, P.; Keinänen-Kiukaanniemi, S.; Laakso, M.; Louheranta, A.; Rastas, M.; et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N. Engl. J. Med. 2001, 344, 1343–1350. [Google Scholar] [CrossRef]
- Knowler, W.C.; Fowler, S.E.; Hamman, R.F.; Christophi, C.A.; Hoffman, H.J.; Brenneman, A.T.; Brown-Friday, J.O.; Goldberg, R.; Venditti, E.; Nathan, D.M.; et al. 10-Year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009, 374, 1677–1686. [Google Scholar] [CrossRef]
- Liu, S.; Serdula, M.; Janket, S.J.; Cook, N.R.; Sesso, H.D.; Willett, W.C.; Manson, J.E.; Buring, J.E. A prospective study of fruit and vegetable intake and the risk of type 2 diabetes in women. Diabetes Care 2004, 27, 2993–2996. [Google Scholar] [CrossRef]
- Villegas, R.; Shu, X.O.; Gao, Y.T.; Yang, G.; Elasy, T.; Li, H.; Zheng, W. Vegetable but not fruit consumption reduces the risk of type 2 diabetes in Chinese women. J. Nutr. 2008, 138, 574–580. [Google Scholar]
- Priebe, M.G.; van Binsbergen, J.J.; de Vos, R.; Vonk, R.J. Whole grain foods for the prevention of type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2008, 23, CD006061. [Google Scholar]
- Baliunas, D.O.; Taylor, B.J.; Irving, H.; Roerecke, M.; Patra, J.; Mohapatra, S.; Rehm, J. Alcohol as a risk factor for type 2 diabetes: A systematic review and meta-analysis. Diabetes Care 2009, 32, 2123–2132. [Google Scholar] [CrossRef]
- Thomas, D.; Elliott, E.J. Low glycaemic index, or low glycaemic load, diets for diabetes mellitus. Cochrane Database Syst. Rev. 2009, 21, CD006296. [Google Scholar]
- Matusheski, N.V.; Bidel, S.; Tuomilehto, J. Coffee and Type 2 Diabetes Risk, Chapter 8 in Coffee Emerging Health Effects and Disease Prevention; Chu, Y.F., Ed.; John Wiley & Sons: Ames, IA, USA, 2012; pp. 141–179. [Google Scholar]
- Salas-Salvadó, J.; Bulló, M.; Babio, N.; Martínez-González, M.Á.; Ibarrola-Jurado, N.; Basora, J.; Estruch, R.; Covas, M.I.; Corella, D.; Arós, F.; et al. Reduction in the incidence of type 2 diabetes with the Mediterranean diet: Results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care 2011, 34, 14–19. [Google Scholar]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.E.A. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet. N. Engl. J. Med. 2013, 368, pp. 1279–1290. Available online: http://www.nejm.org/doi/full/10.1056/NEJMoa1200303 (accessed on 14 March 2013).[Green Version]
- Serra-Majem, L.; Roman, B.; Estruch, R. Scientific evidence of interventions using the Mediterranean diet: A systematic review. Nutr. Rev. 2006, 64, S27–S47. [Google Scholar] [CrossRef]
- Giugliano, D.; Esposito, K. Mediterranean diet and metabolic diseases. Curr. Opin. Lipidol. 2008, 19, 63–68. [Google Scholar]
- Willett, W.C.; Sacks, F.; Trichopoulou, A.; Drescher, G.; Ferro-Luzzi, A.; Helsing, E.; Trichopoulos, D. Mediterranean diet pyramid: A cultural model for healthy eating. Am. J. Clin. Nutr. 1995, 61, 1402S–1406S. [Google Scholar]
- Franz, M.J.; Monk, A.; Barry, B.E.A. Effectiveness of medical nutrition therapy provided by dietitians in the management of non-insulin-dependent diabetes mellitus: a randomized, controlled clinical trial. J. Am. Diet. Assoc. 1995, 95, 1009–1017. [Google Scholar] [CrossRef]
- Hensrud, D.D. Converting Knowledge to Action, Chapter 7. Mayo Clinicon Healthy Weight, 1st ed.; Kensington Publishing Corporation: New York, NY, USA, 2000; pp. 77–104. [Google Scholar]
- ADA. Standards of medical care in diabetes 2013. Diabetes Care 2013, 36, S11–S66. [Google Scholar] [CrossRef]
- Gonzalez-Campoy, J.M.; St Jeor, S.T.; Castorino, K.; Ebrahim, A.; Hurley, D.; Jovanovic, L.; Mechanick, J.I.; Petak, S.M.; Yu, Y.H.; Harris, K.A; et al. Clinical practice guidelines for healthy eating for the prevention and treatment of metabolic and endocrine diseases in adults: Cosponsored by the American Association of Clinical Endocrinologists/the American College of Endocrinology and the Obesity Society. Endocr. Pract. 2013, 19, 1–82. [Google Scholar]
- Fenadiabetes. Guía Práctica en Diabetes Mellitus; Gruber, E., Ablan, F., Arocha, J.I., Eds.; Smart Marketing: Caracas, CA, USA, 2012; p. 277. [Google Scholar]
- Lichtenstein, A.H.; Appel, L.J.; Brands, M.; Carnethon, M.; Daniels, S.; Franch, H.A.; Franklin, B.; Kris-Etherton, P.; Harris, W.S.; Howard, B.; et al. Diet and lifestyle recommendations revision 2006: A scientific statement from the American Heart Association Nutrition Committee. Circulation 2006, 114, 82–96. [Google Scholar] [CrossRef]
- Sacks, F.M.; Svetkey, L.P.; Vollmer, M.S.E.A.; DASH-sodium collaborative group. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. N. Engl. Med. 2001, 344, 3–10. [Google Scholar] [CrossRef]
- Bantle, J.P.; Wylie-Rosett, J.; Albright, A.L.; Apovian, C.M.; Clark, N.G.; Franz, M.J.; Hoogwerf, B.J.; Lichtenstein, A.H.; Mayer-Davis, E.; Mooradian, A.D.; et al. Nutrition recommendations and interventions for diabetes: A position statement of the American Diabetes Association. Diabetes Care 2008, 31, S61–S78. [Google Scholar] [CrossRef]
- Elia, M.; Ceriello, A.; Laube, H.; Sinclair, A.J.; Engfer, M.; Stratton, R.J. Enteral nutritional support and use of diabetes-specific formulas for patients with diabetes: A systematic review and meta-analysis. Diabetes Care 2005, 28, 2267–2279. [Google Scholar] [CrossRef]
- Livesey, G.; Taylor, R.; Hulshof, T.; Howlett, J. Glycemic response and health—A systematic review and meta-analysis: Relations between dietary glycemic properties and health outcomes. Am. J. Clin. Nutr. 2008, 87, 258S–268S. [Google Scholar]
- Hamdy, O.; Zwiefelhofer, D. Weight management using a meal replacement strategy in type 2 diabetes. Curr. Diabetes Rep. 2010, 10, 159–164. [Google Scholar] [CrossRef]
- Wadden, T.A.; Neiberg, R.H.; Wing, R.R.; Clark, J.M.; Delahanty, L.M.; Hill, J.O.; Krakoff, J.; Otto, A.; Ryan, D.H.; Vitolins, M.Z.; et al. Four-year weight losses in the Look AHEAD study: Factors associated with long-term success. Obesity 2011, 19, 1987–1998. [Google Scholar] [CrossRef]
- Pozzilli, P.; Leslie, R.D.; Chan, J.; de Fronzo, R.; Monnier, L.; Raz, I.; Del Prato, S. The A1C and ABCD of glycaemia management in type 2 diabetes: A physician’s personalized approach. Diabetes Metab. Res. Rev. 2010, 26, 239–244. [Google Scholar] [CrossRef]
- Nieto-Martínez, R. Actividad física en la prevención y tratamiento de la diabetes. Rev. Venezol. Endocrinol. Metab. 2010, 8, 40–45. [Google Scholar]
- Florez, H.J.; Stepenka, V.; Castillo-Florez, S.; Rivas, Y.; Casal, J.; Ryder, E.; Silva, E.; Maestre, G.; Oropeza, L. Lifestyle intervention improves global cardiovascular health in latinos with prediabetes in Maracaibo, Venezuela. Circulation 2012, 125, AP162. [Google Scholar]
- US Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. 2008. Available online: http://www.health.gov/paguidelines/guidelines/summary.aspx (accessed on 22 June 2011). [Google Scholar]
- Leyba, J.L.; Aulestia, S.N.; Llopis, S.N. Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for the treatment of morbid obesity. A prospective study of 117 patients. Obes. Surg. 2011, 21, 212–216. [Google Scholar] [CrossRef]
- International Diabetes Federation. Bariatric Surgical Procedures and Interventions in the Treatment of Obese Patients with Type 2 Iabetes: A Position Statement from the International Diabetes Federation Taskforce on Epidemiology and Prevention. Available online: http://www.idf.org/webdata/docs/IDF-Position-Statement-Bariatric-Surgery.pdf (accessed on 3 March 2013).
- Navarrete, A.S.; Leyba, J.; Navarrete, L.L.S.; García Caballero, M.; Sánchez, N.; Pulgar, V.; Vivas, A. Roux-en-Y gastric bypass for treatment of patients with DM type 2 and BMI of 30 to 35 kg/m2. Nutr. Hosp. 2012, 27, 1160–1165. [Google Scholar]
- ASMBS. Bariatric surgery in class I obesity (body mass index 30–35 kg/m2). Surg. Obes. Relat. Dis. 2013, 9, 18. [Google Scholar] [CrossRef]
- Handelsman, Y.; Mechanick, J.I.; Blonde, L.E.A. American association of clinical endocrinologists medical guidelines for clinical practice for developing a diabetes mellitus comprehensive care plan. Endocr. Pract. 2011, 17, 1–53. [Google Scholar] [CrossRef]
- Mechanick, J.; Garber, A.J.; Handelsman, Y.; Garvey, W.T. American Association of Clinical Endocrinologists’ position statement on obesity and obesity medicine. Endocr. Pract. 2012, 18, 642–648. [Google Scholar] [CrossRef]
- Balkau, B.; Charles, M.A. Comment on the provisional report from the WHO consultation. European Group for the Study of Insulin Resistance (EGIR). Diabet. Med. 1999, 16, 442–443. [Google Scholar] [CrossRef]
- García, R.S.; Hoffmann, I.S. Utilizacion de la metformina en diferentes centros de salud del área metropolitana de Caracas. Rev. Venezol. Endocrinol. Metab. 2006, 4, 41–41. [Google Scholar]
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.M.; Walker, E.A.; Nathan, D.M.; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [CrossRef]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Nieto-Martínez, R.; Hamdy, O.; Marante, D.; Marulanda, M.I.; Marchetti, A.; Hegazi, R.A.; Mechanick, J.I. Transcultural Diabetes Nutrition Algorithm (tDNA): Venezuelan Application. Nutrients 2014, 6, 1333-1363. https://doi.org/10.3390/nu6041333
Nieto-Martínez R, Hamdy O, Marante D, Marulanda MI, Marchetti A, Hegazi RA, Mechanick JI. Transcultural Diabetes Nutrition Algorithm (tDNA): Venezuelan Application. Nutrients. 2014; 6(4):1333-1363. https://doi.org/10.3390/nu6041333
Chicago/Turabian StyleNieto-Martínez, Ramfis, Osama Hamdy, Daniel Marante, María Inés Marulanda, Albert Marchetti, Refaat A. Hegazi, and Jeffrey I. Mechanick. 2014. "Transcultural Diabetes Nutrition Algorithm (tDNA): Venezuelan Application" Nutrients 6, no. 4: 1333-1363. https://doi.org/10.3390/nu6041333
APA StyleNieto-Martínez, R., Hamdy, O., Marante, D., Marulanda, M. I., Marchetti, A., Hegazi, R. A., & Mechanick, J. I. (2014). Transcultural Diabetes Nutrition Algorithm (tDNA): Venezuelan Application. Nutrients, 6(4), 1333-1363. https://doi.org/10.3390/nu6041333




