An Overview of Essential Nutritional Strategies and Products in the Treatment of Endometriosis
Abstract
1. Introduction
- First-degree endometriosis (minimal)—small foci of endometriosis are located on the uterus, ovaries, fallopian tubes, and peritoneum, and there may be small adhesions.
- Second-degree of endometriosis (mild)—more extensive foci of endometriosis appear, and endometrial cysts of the ovaries (also known as chocolate cysts) may be present; changes may be located behind the uterus, in the rectouterine pouch.
- Third-degree endometriosis (moderate)—extensive adhesions are present, and the disease process also affects the sacrouterine ligaments.
- Fourth-degree endometriosis (severe)—due to the presence of numerous adhesions, deformation of the surrounding organs occurs. For example, the uterus may be immobile, bent backwards, or attached to the intestinal loops. Endometriosis lesions may also occur in other organs, including the appendix, bladder, intestines, vagina, and cervix.
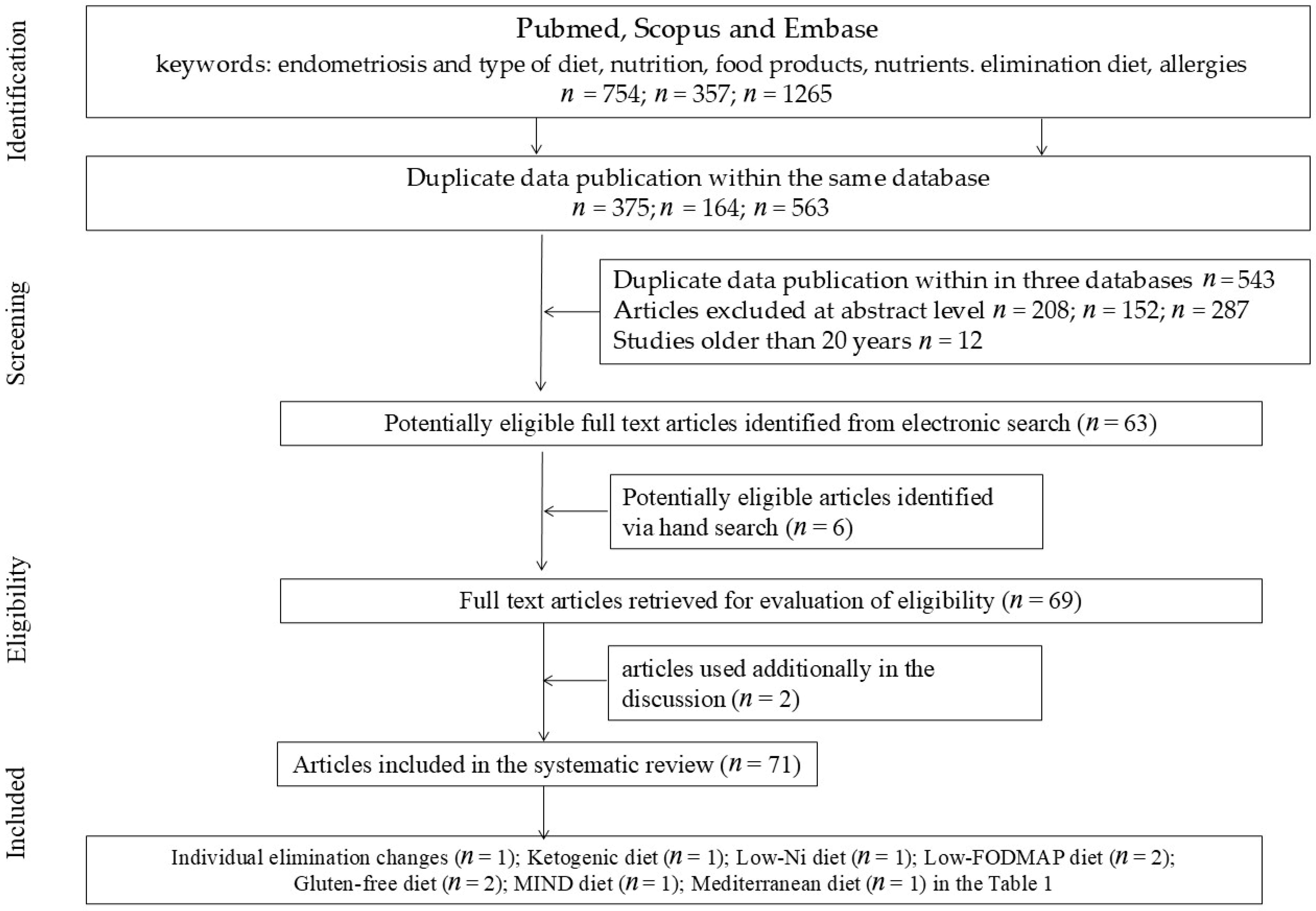
2. Materials and Methods
3. High-Fat and/or High-Protein Diets
3.1. Red Meat
3.2. Dairy Products
4. A Diet Low in Fermentable Oligo-, Di-, Monosaccharides and Polyols (Low-FODMAP Diet)
5. Gluten-Free Diet
6. Low-Nickel Diet
7. Mediterranean Diet
8. MIND Diet (Mediterranean-DASH Diet Intervention for Neurological Delay)
9. High-Fiber Diet
10. Antioxidant (Anti-Inflammatory) Diet
| The Type of Elimination | Number of Subjects | Materials and Methods | Period | Effect | Authors | Research Project |
|---|---|---|---|---|---|---|
| Individual elimination changes | 12 cases | Reducing consumption of dairy products and gluten Increasing consumption of fruit, vegetables, and fish | Minimum 1 year | Experience reduced pain and a regulated menstrual cycle | Vennberg et al., 2020 [2] | Quasi-experimental studies |
| Ketogenic diet with MCT supplement | 19 cases/25 placebo | The modified MCT ketogenic diet contains 70–80% fat, 15–20% protein, and 5–10% carbohydrates. | 12 weeks | dyspareunia and dyschezia significantly decreased marginally significant reduction in final pelvic pain scores | Naeini et al., 2025 [14] | Randomized Controlled Trial |
| Low-FODMAP diet | 59 cases IBS/101 controls Endometriosis and IBS | Rome III criteria for IBS two groups: individuals with concurrent endometriosis and IBS, and individuals diagnosed solely with IBS. | 4 weeks | improvement in intestinal symptoms in over 75% of patients | Moore et al., 2017 [38] | Randomized Controlled Trial |
| Low-FODMAP diet | 50 cases/50 controls | 7-day meal planning FODMAP intake < 5 g/day | 28 days | Significant: improved stool consistency, improved overall quality of life, reduced intestinal gas production, relief of pain symptoms, relief of depression symptoms. | Varney et al., 2025 [40] | Randomized Controlled Trial |
| Gluten-free diet | 207 patients | - | 12 months | 75%—statistically significant reduction in pain symptoms 25%—no improvement in symptoms 100%—significant improvement in quality of life | Marziali et al., 2012 [43] | Quasi-experimental studies |
| Gluten-free diet | 204/114/56 controls | 3 groups: 1–3 months; Less than 1 month Control group | 1–3 months | Patients who avoided wheat, experienced greater improvements in well-being and reduced pain. | Mills et al., 2011 [46] | Randomized Controlled Trial |
| Low-Ni diet | 31 cases | oral mucosal patch test Ni (omPT), | 3 months | gastrointestinal, parenteral, and gynecological symptoms were statistically significantly reduced | Borghini et al., 2020 [50] | Quasi-experimental studies |
| Mediterranean diet | 68 | Doctors should recommend as a long-term solution for endometriosis | 5 months | Significant reduction in pain and improvement in quality of life | Ott et al., 2012 [52] | Quasi-experimental studies |
| MIND diet | 115 cases/230 controls | The MIND diet calculations were based on food intake in the form of FFQ. | 8 months | A significant reduction in the risk of endometriosis was observed in the group consuming the most green leafy vegetables, other vegetables, nuts, legumes, berries, and fish. A higher risk of endometriosis was found in the group consuming the most red meat, butter, and margarine. | Noormohammadi et al., 2025 [58] | Randomized Controlled Trial |
11. Discussion
12. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACM | allergic contact mucositis |
| BMI | Body mass index |
| DHA | docosahexaenoic acid |
| EPA | eicosapentaenoic acid |
| FODMAP | fermentable oligo-, di-, monosaccharides and polyols |
| IBS | irritable bowel syndrome |
| IGF-1 | insulin-like growth factor 1 |
| MUFA | monounsaturated fatty acids |
| PRISMA | preferred reporting Items for systematic reviews and meta-analyses |
| PUFA | polyunsaturated fatty acids |
| SFA | saturated fatty acids |
References
- Brouns, F.; Van Haaps, A.; Keszthelyi, D.; Venema, K.; Bongers, M.; Maas, J.; Mijatovic, V. Diet associations in endometriosis: A critical narrative assessment with special reference to gluten. Front. Nutr. 2023, 10, 1166929. [Google Scholar]
- Vennberg Karlsson, J.; Patel, H.; Premberg, A. Experiences of health after dietary changes in endometriosis: A qualitative interview study. BMJ Open 2020, 10, e032321. [Google Scholar] [CrossRef]
- Nabi, M.Y.; Nauhria, S.; Reel, M.; Londono, S.; Vasireddi, A.; Elmiry, M.; Ramdass, P.V.A.K. Endometriosis and irritable bowel syndrome: A systematic review and meta-analyses. Front. Med. 2022, 9, 914356. [Google Scholar] [CrossRef]
- Abulughod, N.; Valakas, S.; El-Assaad, F. Dietary and Nutritional Interventions for the Management of Endometriosis. Nutrients 2024, 16, 3988. [Google Scholar] [CrossRef]
- Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil. Steril. 1997, 67, 817–821. [CrossRef]
- Ek, M.; Roth, B.; Ekström, P.; Valentin, L.; Bengtsson, M.; Ohlsson, B. Gastrointestinal Symptoms Among Endometriosis Patients—A Case-Cohort Study. BMC Women’s Health 2015, 15, 59. [Google Scholar] [CrossRef]
- Heard, M.E.; Melnyk, S.B.; Simmen, F.A.; Yang, Y.; Pabona, J.M.P.; Simmen, R.C.M. High-fat diet promotion of endometriosis in an immunocompetent mouse model is associated with altered peripheral and ectopic lesion redox and inflammatory status. Endocrinology 2016, 157, 2870–2882. [Google Scholar] [CrossRef] [PubMed]
- Minihane, A.M.; Vinoy, S.; Russell, W.R.; Baka, A.; Roche, H.M.; Tuohy, K.M.; Teeling, J.L.; Blaak, E.E.; Fenech, M.; Vauzour, D.; et al. Low-grade inflammation, diet composition and health: Current research evidence and its translation. Br. J. Nutr. 2015, 114, 999–1012. [Google Scholar] [CrossRef] [PubMed]
- Saini, R.K.; Keum, Y.S. Omega-3 and omega-6 polyunsaturated fatty acids: Dietary sources, metabolism, and significance—A review. Life Sci. 2018, 203, 255–267. [Google Scholar] [CrossRef]
- Guo, L.; Nan, Y.; Liang, K.; Yao, L.; Li, J. Association between polyunsaturated fatty acid intake estradiol levels among, U.S. women. Front. Nutr. 2024, 11, 1500705. [Google Scholar] [CrossRef] [PubMed]
- Kotowska, M.; Różańska-Smuszkiewicz, G.; Smuszkiewicz-Różański, P.; Zamirska, W.; Zygmunt, A.; Zięba, K.; Koszyczarek, K.; Ziemiański, A. Nutritional interventions in the management of endometriosis—Review of the literature. J. Educ. Health Sport 2024, 52, 87–97. [Google Scholar] [CrossRef]
- Forsythe, C.E.; Phinney, S.D.; Fernandez, M.L.; Quann, E.E.; Wood, R.J.; Bibus, D.M.; Kraemer, W.J.; Feinman, R.D.; Volek, J.S. Comparison of low fat and low carbohydrate diets on circulating fatty acid composition and markers of inflammation. Lipids 2008, 43, 65–77. [Google Scholar] [CrossRef]
- Masino, S.A.; Ruskin, D.N. Ketogenic diets and pain. J. Child Neurol. 2013, 28, 993–1001. [Google Scholar] [CrossRef]
- Naeini, F.; Tanha, F.D.; Mahmoudi, M.; Ansar, H.; Hosseinzadeh-Attar, M.J. MCT-modified ketogenic diet as an adjunct to standard treatment regimen could alleviate clinical symptoms in women with endometriosis. BMC Women’s Health 2025, 25, 232. [Google Scholar] [CrossRef] [PubMed]
- Parazzini, F.; Chiaffarino, F.; Surace, M.; Chatenoud, L.; Cipriani, S.; Chiantera, V.; Benzi, G.; Fedele, L. Selected food intake and risk of endometriosis. Hum. Reprod. 2004, 19, 1755–1759. [Google Scholar] [CrossRef] [PubMed]
- Jurkiewicz-Przondziono, J.; Lemm, M.; Kwiatkowska-Pamuła, A.; Ziółko, E.; Wójtowicz, M.K. Influence of diet on the risk of developing endometriosis. Ginekol. Pol. 2017, 88, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Demezio da Silva, C.V.; Felipe, V.L.; Shivappa, N.; Hebert, J.R.; Perini, J.A.; de Brito, P.D.; Cardoso, J.V.; Ferrari, R.; de Almeida Filho, G.L. Dietary Inflammatory Index score and risk of developing endometriosis: A case-control study. J. Endometr. Pelvic Pain Disord. 2021, 13, 32–39. [Google Scholar] [CrossRef]
- Yamamoto, A.; Harris, H.R.; Vitonis, A.F.; Chavarro, J.E.; Missmer, S.A. A prospective cohort study of meat and fish consumption and endometriosis risk. Am. J. Obstet. Gynecol. 2018, 219, e171–e178. [Google Scholar] [CrossRef]
- Trabert, B.; Peters, U.; De Roos, A.J.; Scholes, D.; Holt, V.L. Diet and risk of endometriosis in a population-based case-control study. Br. J. Nutr. 2011, 105, 459–467. [Google Scholar] [CrossRef]
- Heilier, J.-F.; Donnez, J.; Nackers, F.; Rousseau, R.; Verougstraete, V.; Rosenkranz, K.; Donnez, O.; Grandjean, F.; Lison, D.; Tonglet, R. Environmental and host-associated risk factors in endometriosis and deep endometriotic nodules: A matched case–control study. Environ. Res. 2007, 103, 121–129. [Google Scholar] [CrossRef]
- Khan, K.N.; Fujishita, A.; Hiraki, K.; Kitajima, M.; Nakashima, M.; Fushiki, S.; Kitawaki, J. Bacterial contamination hypothesis: A new concept in endometriosis. Reprod. Med. Biol. 2018, 17, 125–133. [Google Scholar] [CrossRef]
- Jiang, I.; Yong, P.J.; Allaire, C.; Bedaiwy, M.A. Intricate connections between the microbiota and endometriosis. Int. J. Mol. Sci. 2021, 22, 5644. [Google Scholar] [CrossRef]
- Wang, Y.; Beydoun, M.A. Meat consumption is associated with obesity and central obesity among us adults. Int. J. Obes. 2009, 33, 621–628. [Google Scholar] [CrossRef] [PubMed]
- Calder, P.C.; Ahluwalia, N.; Brouns, F.; Buetler, T.; Clement, K.; Cunningham, K.; Esposito, K.; Jönsson, L.S.; Kolb, H.; Lansink, M.; et al. Dietary factors and low-grade inflammation in relation to overweight and obesity. Br. J. Nutr. 2011, 106, S5–S78. [Google Scholar] [CrossRef]
- Montonen, J.; Boeing, H.; Fritsche, A.; Schleicher, E.; Joost, H.-G.; Schulze, M.B.; Steffen, A.; Pischon, T. Consumption of red meat and whole-grain bread in relation to biomarkers of obesity, inflammation, glucose metabolism and oxidative stress. Eur. J. Nutr. 2013, 52, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Peterson, C.M.; Johnstone, E.B.; Hammoud, A.O.; Stanford, J.B.; Varner, M.W.; Kennedy, A.; Chen, Z.; Sun, L.; Fujimoto, V.Y.; Hediger, M.L.; et al. Risk factors associated with endometriosis: Importance of study population for characterizing disease in the ENDO study. Am. J. Obstet. Gynecol. 2013, 208, 451.e1–451.e11. [Google Scholar] [CrossRef]
- Gao, M.; Allebeck, P.; Mishra, G.D.; Koupil, I. Developmental origins of endometriosis: A Swedish cohort study. J. Epidemiol. Community Health 2019, 73, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Hetemäki, N.; Mikkola, T.S.; Tikkanen, M.J.; Wang, F.; Hämäläinen, E.; Turpeinen, U.; Haanpää, M.; Vihma, V.; Savolainen-Peltonen, H. Adipose tissue estrogen production and metabolism in premenopausal women. J. Steroid Biochem. Mol. Biol. 2021, 209, 105849. [Google Scholar] [CrossRef]
- Brinkman, M.T.; Baglietto, L.; Krishnan, K.; English, D.R.; Severi, G.; Morris, H.A.; Hopper, J.L.; Giles, G.G. Consumption of animal products, their nutrient components and postmenopausal circulating steroid hormone concentrations. Eur. J. Clin. Nutr. 2010, 64, 176–183. [Google Scholar] [CrossRef]
- Harris, H.R.; Chavarro, J.E.; Malspeis, S.; Willett, W.C.; Missmer, S.A. Dairy-food, calcium, magnesium, and vitamin D intake and endometriosis: A prospective cohort study. Am. J. Epidemiol. 2013, 177, 420–430. [Google Scholar] [CrossRef]
- Nodler, J.L.; Harris, H.R.; Chavarro, J.E.; Frazier, A.L.; Missmer, S.A. Dairy consumption during adolescence and endometriosis risk. Am. J. Obstet. Gynecol. 2020, 222, e251–e257. [Google Scholar] [CrossRef] [PubMed]
- Nieman, K.M.; Anderson, B.D.; Cifelli, C.J. The Effects of Dairy Product and Dairy Protein Intake on Inflammation: A Systematic Review of the Literature. J. Am. Coll. Nutr. 2021, 40, 571–582. [Google Scholar] [CrossRef]
- Crowe, F.L.; Key, T.J.; Allen, N.E.; Appleby, P.N.; Roddam, A.; Overvad, K.; Grønbaek, H.; Tjønneland, A.; Halkjaer, J.; Dossus, L.; et al. The association between diet and serum concentrations of IGF-I, IGFBP-1, IGFBP-2, and IGFBP-3 in the European Prospective Investigation into Cancer and Nutrition. Cancer Epidemiol. Biomark. Prev. 2009, 18, 1333–1340. [Google Scholar] [CrossRef]
- Salminen, A.; Kaarniranta, K.; Kauppinen, A. Insulin/IGF-1 signaling promotes immunosuppression via the STAT3 pathway: Impact on the aging process and age-related diseases. Inflamm. Res. 2021, 70, 1043–1061. [Google Scholar] [CrossRef]
- Forster, R.; Sarginson, A.; Velichkova, A.; Hogg, C.; Dorning, A.; Horne, A.W.; Saunders, P.T.K.; Greaves, E. Macrophage-derived insulin-like growth factor-1 is a key neurotrophic and nerve-sensitizing factor in pain associated with endometriosis. FASEB J. 2019, 33, 11210–11222. [Google Scholar] [CrossRef]
- RomoVentura, E.; Konigorski, S.; Rohrmann, S.; Schneider, H.; Stalla, G.K.; Pischon, T.; Linseisen, J.; Nimptsch, K. Association of dietary intake of milk and dairy products with blood concentrations of insulin-like growth factor 1 (IGF-1) in Bavarian adults. Eur. J. Nutr. 2020, 59, 1413–1420. [Google Scholar] [CrossRef]
- Deepak Kumar, K.; Appleby-Gunnill, B.; Maslin, K. Nutritional practices and dietetic provision in the endometriosis population, with a focus on functional gut symptoms. J. Hum. Nutr. Diet. 2023, 36, 1529–1538. [Google Scholar] [CrossRef] [PubMed]
- Moore, J.S.; Gibson, P.R.; Perry, R.E.; Burgell, R.E. Endometriosis in patients with irritable bowel syndrome: Specific symptomatic and demographic profile, and response to the low FODMAP diet. Aust. N. Z. J. Obstet. Gynaecol. 2017, 57, 201–205. [Google Scholar] [CrossRef]
- Armour, M.; Middleton, A.; Lim, S.; Sinclair, J.; Varjabedian, D.; Smith, C.A. Dietary Practices of Women with Endometriosis: A Cross-Sectional Survey. J. Altern. Complement. Med. 2021, 27, 771–777. [Google Scholar] [CrossRef] [PubMed]
- Varney, J.E.; So, D.; Gibson, P.R.; Rhys-Jones, D.; Lee, Y.S.J.; Fisher, J.; Moore, J.S.; Ratner, R.; Morrison, M.; Burgell, R.E.; et al. Clinical Trial: Effect of a 28-Day Low FODMAP Diet on Gastrointestinal Symptoms Associated with Endometriosis (EndoFOD)—A Randomised, Controlled Crossover Feeding Study. Aliment. Pharmacol. Ther. 2025, 61, 1889–1903. [Google Scholar] [CrossRef]
- Mazza, E.; Troiano, E.; Mazza, S.; Ferro, Y.; Abbinante, A.; Agneta, M.T.; Montalcini, T.; Pujia, A. The impact of endometriosis on dietary choices and activities of everyday life: A cross-sectional study. Front. Nutr. 2023, 10, 1273976. [Google Scholar] [CrossRef]
- Mick, I.; Freger, S.M.; van Keizerswaard, J.; Gholiof, M.; Leonardi, M. Comprehensive endometriosis care: A modern multimodal approach for the treatment of pelvic pain and endometriosis. Ther. Adv. Reprod. Health 2024, 18, 26334941241277759. [Google Scholar] [CrossRef]
- Marziali, M.; Venza, M.; Lazzaro, S.; Lazzaro, A.; Micossi, C.; Stolfi, V.M. Gluten-free diet: A new strategy for management of painful endometriosis related symptoms? Minerva Chir. 2012, 67, 499–504. [Google Scholar]
- Marziali, M.; Capozzolo, T. Role of gluten-free diet in the management of chronic pelvic pain of deep infiltranting endometriosis. J. Minim. Invasive Gynecol. 2015, 1, S51–S52. [Google Scholar] [CrossRef]
- Krabbenborg, I.; de Roos, N.; van der Grinten, P.; Nap, A. Diet quality and perceived effects of dietary changes in Dutch endometriosis patients: An observational study. Reprod. Biomed. Online 2021, 43, 952–961. [Google Scholar] [CrossRef]
- Mills, D.S. A conundrum: Wheat and gluten avoidance and its implication with endometriosis patients. Fertil. Steril. 2011, 96, S139. [Google Scholar] [CrossRef]
- Szczuko, M.; Syrenicz, A.; Szymkowiak, K.; Przybylska, A.; Szczuko, U.; Pobłocki, J.; Kulpa, D. Doubtful Justification of the Gluten-Free Diet in the Course of Hashimoto’s Disease. Rev. Nutr. 2022, 14, 1727. [Google Scholar] [CrossRef] [PubMed]
- Mania, M.; Rebeniak, M.; Postupolski, J. Food as a source of exposure to nickel. Rocz. Państw. Zakł. Hig. 2019, 70, 393–399. [Google Scholar]
- Yuk, J.S.; Kim, Y.J.; Yi, K.W.; Tak, K.; Hur, J.Y.; Shin, J.H. High rate of nickel allergy in women with endometriosis: A 3-year population-based study. J. Obstet. Gynaecol. Res. 2015, 41, 1255–1259. [Google Scholar] [CrossRef]
- Borghini, R.; Porpora, M.G.; Casale, R.; Marino, M.; Palmieri, E.; Greco, N.; Donato, G.; Picarelli, A. Irritable bowel syndrome-like disorders in endometriosis: Prevalence of nickel sensitivity and effects of a low-nickel diet. An open-label pilot study. Nutrients 2020, 12, 341. [Google Scholar] [CrossRef]
- Davis, C.; Bryan, J.; Hodgson, J.; Murphy, K. Definition of the Mediterranean diet; a literature review. Nutrients 2015, 7, 9139–9153. [Google Scholar] [CrossRef]
- Ott, J.; Nouri, K.; Hrebacka, D.; Gutschelhofer, S.; Huber, J.; Wenzl, R.J. Endometriosis and nutrition-recommending a Mediterranean diet decreases endometriosis-associated pain: An experimental observational study. J. Aging Res. Clin. Pract. 2012, 1, 162–166. [Google Scholar]
- Ashrafi, M.; Jahangiri, N.; Sadatmahalleh, S.J.; Aliani, F.; Akhoond, M. Diet and the risk of endometriosis in Iranian women: A case-control study. Int. J. Fertil. Steril. 2020, 14, 193–200. [Google Scholar] [PubMed]
- Barbouti, A.; Goulas, V. Dietary antioxidants in the Mediterranean diet. Antioxidants 2021, 10, 1213. [Google Scholar] [CrossRef] [PubMed]
- Zarbo, C.; Brugnera, A.; Compare, A.; Malandrino, C.; Candeloro, I.; Secomandi, R.; Betto, E.; Bellia, A.; Rabboni, M.; Bondi, E.; et al. Psychological and cognitive factors implicated in pain experience in women with endometriosis. Health Care Women Int. 2022, 43, 142–159. [Google Scholar] [CrossRef]
- Liu, Y.; Fowler, H.; Wang, D.D.; Barnes, L.L.; Cornelis, M.C. Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) Trial: Genetic Resource for Precision Nutrition. Nutrients 2025, 17, 2548. [Google Scholar] [CrossRef]
- Barber, T.M.; Kabisch, S.; Pfeiffer, A.F.; Weickert, M.O. The health benefits of dietary fibre. Nutrients 2020, 12, 3209. [Google Scholar] [CrossRef]
- Noormohammadi, M.; Ghoreishy, S.M.; Ghasemisedaghat, S.; Hasan-Rashedi, M.; Saeedirad, Z.; Eslamian, G.; Kazemi, S.N.; Nematifard, E.; Rashidkhani, B.; Taheripanahe, R.; et al. Association between MIND diet its components with endometriosis risk: Secondary results from a case-control study. Sci. Rep. 2025, 15, 19201. [Google Scholar] [CrossRef]
- Harris, H.; Eke, A.; Chavarro, J.; Missmer, S. Fruit and vegetable consumption and risk of endometriosis. Hum. Reprod. 2018, 33, 715–727. [Google Scholar] [CrossRef]
- Zheng, Y.F.; Guo, Y.M.; Song, C.J.; Liu, G.C.; Chen, S.Y.; Guo, X.G.; Lin, L.H. A cross-sectional study on the relationship between dietary fiber and endometriosis risk based on NHANES 1999–2006. Sci. Rep. 2024, 14, 28502. [Google Scholar] [CrossRef] [PubMed]
- Parazzini, F.; Vigano, P.; Candiani, M.; Fedele, L. Diet and endometriosis risk: A literature review. Reprod. Biomed. Online 2013, 26, 323–336. [Google Scholar] [CrossRef] [PubMed]
- Han, S.J.; Jung, S.Y.; Wu, S.P.; Hawkins, S.M.; Park, M.J.; Kyo, S.; O’Malley, B.W. Estrogen Receptor β Modulates Apoptosis Complexes and the Inflammasome to Drive the Pathogenesis of Endometriosis. Cell 2015, 163, 960–974. [Google Scholar] [CrossRef]
- Aubertin-Leheudre, M.; Gorbach, S.; Woods, M.; Dwyer, J.T.; Goldin, B.; Adlercreutz, H. Fat/fiber intakes and sex hormones in healthy premenopausal women in USA. J. Steroid Biochem. Mol. Biol. 2008, 112, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Kudesia, R.; Alexander, M.; Gulati, M.; Kennard, A.; Tollefson, M. Dietary Approaches to Women’s Sexual and Reproductive Health. Am. J. Lifestyle Med. 2021, 15, 414–424. [Google Scholar] [CrossRef] [PubMed]
- Aleksandrova, K.; Koelman, L.; Rodrigues, C.E. Dietary patterns and biomarkers of oxidative stress and inflammation: A systematic review of observational and intervention studies. Redox Biol. 2021, 42, 101869. [Google Scholar] [CrossRef]
- Mier-Cabrera, J.; Aburto-Soto, T.; Burrola-Méndez, S.; Jiménez-Zamudio, L.; Tolentino, M.C.; Casanueva, E.; Hernández-Guerrero, C. Women with endometriosis improved their peripheral antioxidant markers after the application of a high antioxidant diet. Reprod. Biol. Endocrinol. 2009, 7, 54. [Google Scholar] [CrossRef]
- Morales-Prieto, D.M.; Herrmann, J.; Osterwald, H.; Kochhar, P.S.; Schleussner, E.; Markert, U.R.; Oettel, M. Comparison of dienogest effects upon 3,3′-diindolylmethane supplementation in models of endometriosis and clinical cases. Reprod. Biol. 2018, 18, 252–258. [Google Scholar] [CrossRef]
- Liu, P.; Maharjan, R.; Wang, Y.; Zhang, Y.; Zhang, Y.; Xu, C.; Geng, Y.; Miao, J. Association between dietary inflammatory index and risk of endometriosis: A population-based analysis. Front. Nutr. 2023, 10, 1077915. [Google Scholar] [CrossRef]
- Chen, W.; Xiao, K.; Zhou, C.; Cheng, J.; Zeng, Z.; Zhang, F. Association of composite dietary antioxidant index and endometriosis risk in reproductive-age women: A cross-sectional study using big data-machine learning approach. Front. Nutr. 2025, 12, 1572336. [Google Scholar] [CrossRef]
- Radowicka, M.M.; Warzecha, D. Endometriosis and diet—Can anti-inflammatory foods alleviate symptoms? Pediatr. Med. Rodz. 2025, 21, 41–45. [Google Scholar] [CrossRef]
- D’Alterio, M.N.; Saponara, S.; D’Ancona, G.; Russo, M.; Laganà, A.S.; Sorrentino, F.; Nappi, L.; Angioni, S. Role of surgical treatment in endometriosis. Minerva Obstet. Gynecol. 2021, 73, 317–332. [Google Scholar] [CrossRef] [PubMed]
- Laganà, A.S.; Garzon, S.; Götte, M.; Viganò, P.; Franchi, M.; Ghezzi, F.; Martin, D.C. The Pathogenesis of Endometriosis: Molecular and Cell Biology Insights. Int. J. Mol. Sci. 2019, 20, 5615. [Google Scholar] [CrossRef]
- Salmeri, N.; Sinagra, E.; Dolci, C.; Buzzaccarini, G.; Sozzi, G.; Sutera, M.; Candiani, M.; Ungaro, F.; Massimino, L.; Danese, S.; et al. Microbiota in Irritable Bowel Syndrome and Endometriosis: Birds of a Feather Flock Together—A Review. Microorganisms 2023, 11, 2089. [Google Scholar] [CrossRef]
- Kikut, J.; Drozd, A.; Mokrzycka, M.; Grzybowska-Chlebowczyk, U.; Ziętek, M.; Szczuko, M. Are EPA and DHA Derivatives Involved in IBD Remission? J. Clin. Med. 2022, 11, 2388. [Google Scholar] [CrossRef] [PubMed]
- Komorniak, N.; Szczuko, M.; Kowalewski, B.; Stachowska, E. Nutritional Deficiencies, Bariatric Surgery, and Serum Homocysteine Level: Review of Current Literature. Obes. Surg. 2019, 29, 3735–3742. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Szczuko, M.; Ziętek, M.; Janda-Milczarek, K.; Rębacz-Maron, E.; Nawrocka-Rutkowska, J.; Pokorska-Niewiada, K. An Overview of Essential Nutritional Strategies and Products in the Treatment of Endometriosis. Nutrients 2026, 18, 77. https://doi.org/10.3390/nu18010077
Szczuko M, Ziętek M, Janda-Milczarek K, Rębacz-Maron E, Nawrocka-Rutkowska J, Pokorska-Niewiada K. An Overview of Essential Nutritional Strategies and Products in the Treatment of Endometriosis. Nutrients. 2026; 18(1):77. https://doi.org/10.3390/nu18010077
Chicago/Turabian StyleSzczuko, Małgorzata, Maciej Ziętek, Katarzyna Janda-Milczarek, Ewa Rębacz-Maron, Jolanta Nawrocka-Rutkowska, and Kamila Pokorska-Niewiada. 2026. "An Overview of Essential Nutritional Strategies and Products in the Treatment of Endometriosis" Nutrients 18, no. 1: 77. https://doi.org/10.3390/nu18010077
APA StyleSzczuko, M., Ziętek, M., Janda-Milczarek, K., Rębacz-Maron, E., Nawrocka-Rutkowska, J., & Pokorska-Niewiada, K. (2026). An Overview of Essential Nutritional Strategies and Products in the Treatment of Endometriosis. Nutrients, 18(1), 77. https://doi.org/10.3390/nu18010077








