Changes in Children’s Adherence to Sustainable Healthy Diets During the Implementation of Chile’s Food Labelling and Advertising Law: A Longitudinal Study (2016–2019)
Abstract
1. Introduction
2. Materials and Methods
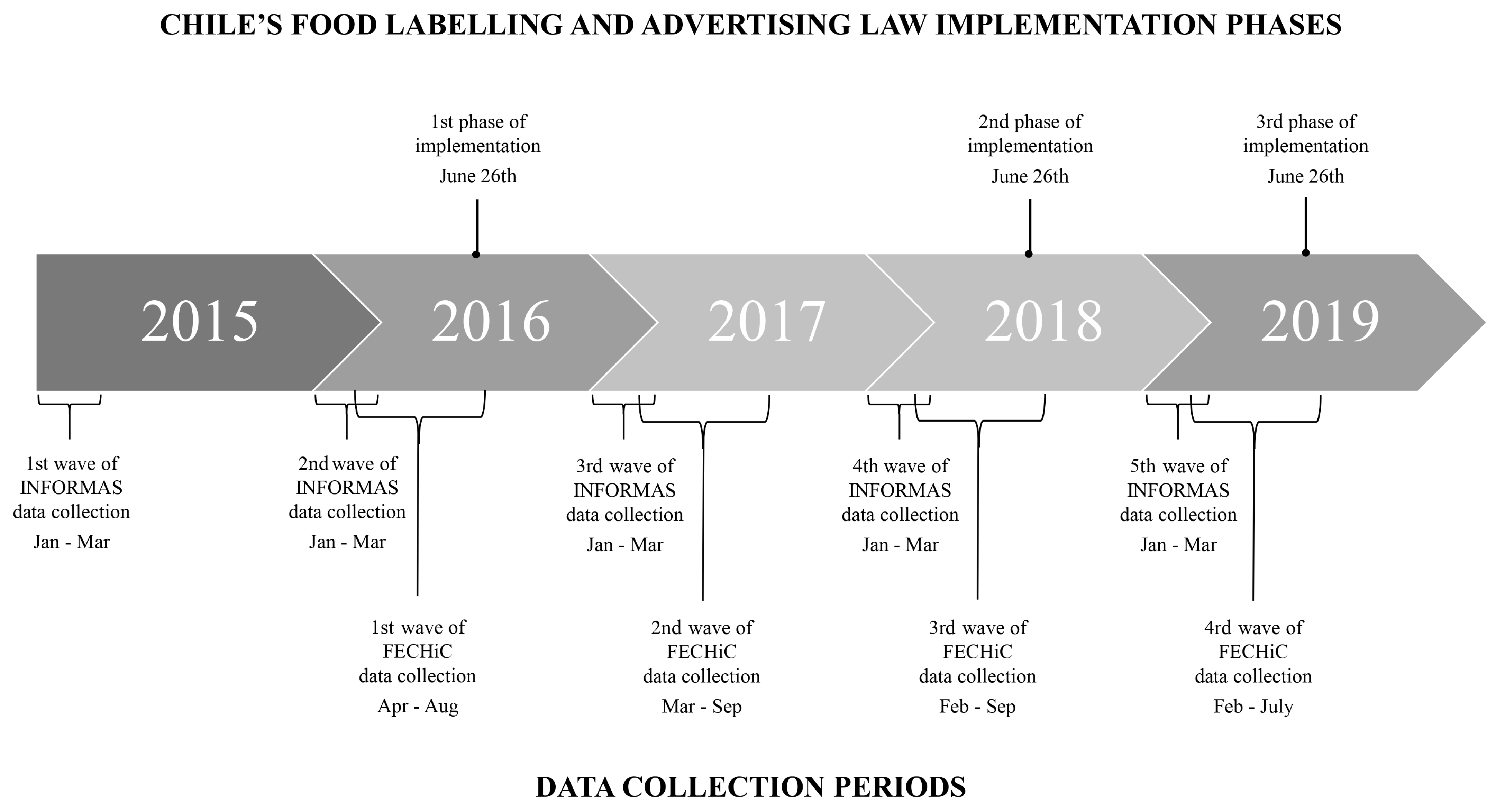
2.1. Study Design
2.2. Participants and Setting
2.3. Data Collection
2.4. Merging Nutrient Information Panels and Ingredient Lists with Children’s Dietary Data
2.5. Outcomes of Interest
2.6. Covariates
2.7. Statistical Analysis
3. Results
3.1. Participants’ Baseline Characteristics (Table 1)
| Analytical Sample (n = 698) | |
|---|---|
| Sociodemographic characteristics | n (%) |
| Child gender | |
| Male | 351 (50.3) |
| Female | 347 (49.7) |
| Child age | |
| 3–4 years | 505 (72.4) |
| 5–6 years | 193 (27.6) |
| Maternal age | |
| <25 years | 123 (17.6) |
| ≥25 years | 575 (82.4) |
| Maternal level of education | |
| Incomplete secondary education | 108 (15.4) |
| Complete secondary education | 404 (57.9) |
| Complete tertiary education | 186 (26.7) |
| Anthropometric characteristics | n (%) |
| Child weight status a | |
| At risk of undernutrition | 21 (3.0) |
| Normal weight | 357 (51.2) |
| Overweight | 204 (29.2) |
| Obesity | 77 (11.0) |
| Severe obesity | 39 (5.6) |
| Maternal weight status b,c | |
| Underweight | 5 (0.8) |
| Normal weight | 188 (28.1) |
| Overweight | 241 (36.0) |
| Obesity class I | 155 (23.2) |
| Obesity class II | 53 (7.9) |
| Obesity class III | 27 (4.0) |
| Maternal abdominal obesity c,d | |
| Absence | 303 (45.3) |
| Presence | 366 (54.7) |
| Dietary recall characteristics | n (%) |
| Day of the dietary recall | |
| Weekday | 598 (85.7) |
| Weekend day/holiday | 100 (14.3) |
| Type of eating pattern on the day of the dietary recall e | |
| Typical | 586 (84.0) |
| Atypical | 112 (16.0) |
| Type of diet on the day of the dietary recall f | |
| Normal | 661 (94.7) |
| Special | 37 (5.3) |
| Reliability of the dietary recall g | |
| Reliable | 654 (93.7) |
| Unreliable | 44 (6.3) |
3.2. Changes in Children’s Dietary Intake and PHDI-C Scores
3.2.1. Changes in Adequacy Components
3.2.2. Changes in Ratio Components
3.2.3. Changes in Optimum Components
3.2.4. Changes in Moderation Components
3.2.5. Sensitivity Analysis
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CIAPEC | Center for Research in Food Environments and Prevention of Nutrition-related Chronic Diseases |
| FECHiC | Food Environment Chilean Cohort |
| GLOBE | Global Centre for Preventive Health and Nutrition |
| INTA | Institute of Nutrition and Food Technology |
| NHANES | National Health and Nutrition Examination Survey |
| PHDI | Planetary Health Diet Index |
| PHDI-C | Planetary Health Diet Index for Children andAdolescents |
| STROBE-Nut | Strengthening the Reporting of Observational Studies in Epidemiology—Nutritional Epidemiology |
| USDA | US Department of Agriculture |
References
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- OECD. OECD Reviews of Public Health: Chile; Organisation for Economic Co-Operation and Development (OECD): Paris, France, 2019. [Google Scholar]
- Junta Nacional de Auxilio Escolar y Becas (JUNAEB); Departamento de Planificación y Estudios; Ministerio de Educación. Informe Mapa Nutricional 2016 [Nutritional Map Report 2016]; JUNAEB: Santiago, Chile, 2016. [Google Scholar]
- Junta Nacional de Auxilio Escolar y Becas (JUNAEB); Departamento de Planificación y Estudios; Ministerio de Educación. Informe Mapa Nutricional 2023 [Nutritional Map Report 2023]; JUNAEB: Santiago, Chile, 2024. [Google Scholar]
- Castillo-Valenzuela, O.; Duarte, L.; Arredondo, M.; Iñiguez, G.; Villarroel, L.; Pérez-Bravo, F. Childhood Obesity and Plasma Micronutrient Deficit of Chilean Children between 4 and 14 Years Old. Nutrients 2023, 15, 1707. [Google Scholar] [CrossRef] [PubMed]
- Myers, S.S.; Smith, M.R.; Guth, S.; Golden, C.D.; Vaitla, B.; Mueller, N.D.; Dangour, A.D.; Huybers, P. Climate Change and Global Food Systems: Potential Impacts on Food Security and Undernutrition. Annu. Rev. Public Health 2017, 38, 259–277. [Google Scholar] [CrossRef] [PubMed]
- Swinburn, B.A.; Kraak, V.I.; Allender, S.; Atkins, V.J.; Baker, P.I.; Bogard, J.R.; Brinsden, H.; Calvillo, A.; De Schutter, O.; Devarajan, R.; et al. The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission report. Lancet 2019, 393, 791–846. [Google Scholar] [CrossRef]
- Venegas Hargous, C.; Strugnell, C.; Allender, S.; Orellana, L.; Corvalan, C.; Bell, C. Double- and triple-duty actions in childhood for addressing the global syndemic of obesity, undernutrition, and climate change: A scoping review. Obes. Rev. 2023, 24, e13555. [Google Scholar] [CrossRef] [PubMed]
- Burgaz, C.; Gorasso, V.; Achten, W.M.J.; Batis, C.; Castronuovo, L.; Diouf, A.; Asiki, G.; Swinburn, B.A.; Unar-Munguía, M.; Devleesschauwer, B.; et al. The effectiveness of food system policies to improve nutrition, nutrition-related inequalities and environmental sustainability: A scoping review. Food Secur. 2023, 15, 1313–1344. [Google Scholar] [CrossRef]
- Ministerio de Salud; Subsecretaría de Salud Pública. LEY 20606 Sobre Composición Nutricional de los Alimentos y su Publicidad; Ministerio de Salud, Ed.: Santiago, Chile, 2012. [Google Scholar]
- Reyes, M.; Smith Taillie, L.; Popkin, B.; Kanter, R.; Vandevijvere, S.; Corvalan, C. Changes in the amount of nutrient of packaged foods and beverages after the initial implementation of the Chilean Law of Food Labelling and Advertising: A nonexperimental prospective study. PLoS Med. 2020, 17, e1003220. [Google Scholar] [CrossRef]
- Quintiliano Scarpelli, D.; Pinheiro Fernandes, A.C.; Rodriguez Osiac, L.; Pizarro Quevedo, T. Changes in Nutrient Declaration after the Food Labeling and Advertising Law in Chile: A Longitudinal Approach. Nutrients 2020, 12, 2371. [Google Scholar] [CrossRef]
- Zancheta Ricardo, C.; Corvalán, C.; Smith Taillie, L.; Quitral, V.; Reyes, M. Changes in the Use of Non-nutritive Sweeteners in the Chilean Food and Beverage Supply After the Implementation of the Food Labeling and Advertising Law. Front. Nutr. 2021, 8, 773450. [Google Scholar] [CrossRef]
- Rebolledo, N.; Ferrer-Rosende, P.; Reyes, M.; Smith Taillie, L.; Corvalán, C. Changes in the critical nutrient content of packaged foods and beverages after the full implementation of the Chilean Food Labelling and Advertising Law: A repeated cross-sectional study. BMC Med. 2025, 23, 46. [Google Scholar] [CrossRef]
- Taillie, L.S.; Reyes, M.; Colchero, M.A.; Popkin, B.; Corvalan, C. An evaluation of Chile’s Law of Food Labeling and Advertising on sugar-sweetened beverage purchases from 2015 to 2017: A before-and-after study. PLoS Med. 2020, 17, e1003015. [Google Scholar] [CrossRef]
- Smith Taillie, L.; Bercholz, M.; Popkin, B.; Reyes, M.; Colchero, M.A.; Corvalan, C. Changes in food purchases after the Chilean policies on food labelling, marketing, and sales in schools: A before and after study. Lancet Planet. Health 2021, 5, e526–e533. [Google Scholar] [CrossRef]
- Barahona, N.; Otero, C.; Otero, S. Equilibrium Effects of Food Labeling Policies. Econometrica 2023, 91, 839–868. [Google Scholar] [CrossRef]
- Taillie, L.S.; Bercholz, M.; Popkin, B.; Rebolledo, N.; Reyes, M.; Corvalán, C. Decreases in purchases of energy, sodium, sugar, and saturated fat 3 years after implementation of the Chilean food labeling and marketing law: An interrupted time series analysis. PLOS Med. 2024, 21, e1004463. [Google Scholar] [CrossRef]
- Massri, C.; Sutherland, S.; Källestål, C.; Peña, S. Impact of the Food-Labeling and Advertising Law Banning Competitive Food and Beverages in Chilean Public Schools, 2014–2016. Am. J. Public Health 2019, 109, 1249–1254. [Google Scholar] [CrossRef]
- Fretes, G.; Corvalán, C.; Reyes, M.; Taillie, L.S.; Economos, C.D.; Wilson, N.L.W.; Cash, S.B. Changes in children’s and adolescents’ dietary intake after the implementation of Chile’s law of food labeling, advertising and sales in schools: A longitudinal study. Int. J. Behav. Nutr. Phys. Act. 2023, 20, 40. [Google Scholar] [CrossRef] [PubMed]
- FAO; WHO. Sustainable Healthy Diets–Guiding Principles; FAO and WHO: Rome, Italy, 2019. [Google Scholar]
- Lachat, C.; Hawwash, D.; Ocké, M.C.; Berg, C.; Forsum, E.; Hörnell, A.; Larsson, C.; Sonestedt, E.; Wirfält, E.; Åkesson, A.; et al. Strengthening the Reporting of Observational Studies in Epidemiology-Nutritional Epidemiology (STROBE-nut): An Extension of the STROBE Statement. PLoS Med. 2016, 13, e1002036. [Google Scholar] [CrossRef] [PubMed]
- Departamento de Nutrición; Escuela de Nutrición; Escuela de Salud Pública; Centro de Microdatos. Informe Final Encuesta Nacional de Consumo Alimentario; Universidad de Chile: Santiago, Chile, 2010. [Google Scholar]
- Venegas Hargous, C.; Reyes, M.; Smith Taillie, L.; Gonzalez, C.G.; Corvalan, C. Consumption of non-nutritive sweeteners by pre-schoolers of the food and environment Chilean cohort (FECHIC) before the implementation of the Chilean food labelling and advertising law. Nutr. J. 2020, 19, 69. [Google Scholar] [CrossRef]
- SEREMI de Desarrollo Social Metropolitana. Pobreza y Distribución del Ingreso en la Región Metropolitana de Santiago: Resultados Encuesta Casen 2015. Available online: https://www.gobiernosantiago.cl/wp-content/uploads/2014/12/DOCUMENTO-POBREZA-Y-DISTR-ING-RMS-CASEN-2015.pdf (accessed on 26 May 2023).
- World Health Organization (WHO). WHO STEPS Surveillance Manual: The WHO STEPwise Approach to Chronic Disease Risk Factor Surveillance; World Health Organization: Ginebra, Switzerland, 2006. [Google Scholar]
- World Health Organization. WHO Child Growth Standards. Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-Forage. Methods and Development; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- de Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Body Mass Index-BMI. Available online: https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle---who-recommendations (accessed on 26 May 2023).
- Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef]
- Raper, N.; Perloff, B.; Ingwersen, L.; Steinfeldt, L.; Anand, J. An overview of USDA’s Dietary Intake Data System. J. Food Compos. Anal. 2004, 17, 545–555. [Google Scholar] [CrossRef]
- Moshfegh, A.; Rhodes, D.; Baer, D.; Murayi, T.; Clemens, J.; Rumpler, W.; Paul, D.; Sebastian, R.; Kuczynski, K.; Ingwersen, L.; et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J. Clin. Nutr. 2008, 88, 324–332. [Google Scholar] [CrossRef]
- Universidad de Chile; Ministerio de Salud de Chile. Atlas Fotográfico de Alimentos y Preparaciones Típicas Chilenas: Encuesta Nacional de Consumo Alimentario 2010; Ministerio de Salud: Santiago, Chile, 2010. [Google Scholar]
- Rebolledo, N.; Reyes, M.; Popkin, B.; Adair, L.; Avery, C.; Corvalán, C.; Ng, S.; Smith Taillie, L. Changes in nonnutritive sweetener intake in a cohort of preschoolers after the implementation of Chile’s Law of Food Labelling and Advertising. Pediatr. Obes. 2022, 17, e12895. [Google Scholar] [CrossRef]
- United States Department of Agriculture (USDA); Agricultural Research Service. FoodData Central. Available online: https://fdc.nal.usda.gov// (accessed on 12 November 2020).
- INFORMAS. Chile|INFORMAS. Available online: https://www.informas.org/chile/ (accessed on 16 March 2020).
- Kanter, R.; Reyes, M.; Corvalán, C. Photographic Methods for Measuring Packaged Food and Beverage Products in Supermarkets. Curr. Dev. Nutr. 2017, 1, e001016. [Google Scholar] [CrossRef]
- Venegas Hargous, C.; Orellana, L.; Strugnell, C.; Corvalan, C.; Allender, S.; Bell, C. Adapting the Planetary Health Diet Index for children and adolescents. Int. J. Behav. Nutr. Phys. Act. 2023, 20, 146. [Google Scholar] [CrossRef] [PubMed]
- Cacau, L.T.; De Carli, E.; de Carvalho, A.M.; Lotufo, P.A.; Moreno, L.A.; Bensenor, I.M.; Marchioni, D.M. Development and Validation of an Index Based on EAT-Lancet Recommendations: The Planetary Health Diet Index. Nutrients 2021, 13, 1698. [Google Scholar] [CrossRef]
- Sirin, S. Socioeconomic Status and Academic Achievement: A Meta-Analytic Review of Research. Rev. Educ. Res. 2005, 75, 417–453. [Google Scholar] [CrossRef]
- Venegas Hargous, C.; Orellana, L.; Corvalan, C.; Strugnell, C.; Allender, S.; Bell, C. Chilean children’s adherence to sustainable healthy diets and its associations with sociodemographic and anthropometric factors: A cross-sectional study. Eur. J. Nutr. 2024, 63, 2459–2475. [Google Scholar] [CrossRef] [PubMed]
- Rauber, F.; Hoffman, D.J.; Vitolo, M.R. Diet quality from pre-school to school age in Brazilian children: A 4-year follow-up in a randomised control study. Br. J. Nutr. 2014, 111, 499–505. [Google Scholar] [CrossRef]
- Mannino, M.L.; Lee, Y.; Mitchell, D.C.; Smiciklas-Wright, H.; Birch, L.L. The quality of girls’ diets declines and tracks across middle childhood. Int. J. Behav. Nutr. Phys. Act. 2004, 1, 5. [Google Scholar] [CrossRef]
- da Costa, M.; Durão, C.; Lopes, C.; Vilela, S. Adherence to a healthy eating index from pre-school to school age and its associations with sociodemographic and early life factors. Br. J. Nutr. 2019, 122, 220–230. [Google Scholar] [CrossRef] [PubMed]
- Welsh, J.A.; Wang, Y.; Figueroa, J.; Brumme, C. Sugar intake by type (added vs. naturally occurring) and physical form (liquid vs. solid) and its varying association with children’s body weight, NHANES 2009–2014. Pediatr. Obes. 2018, 13, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Neri, D.; Martinez-Steele, E.; Monteiro, C.A.; Levy, R.B. Consumption of ultra-processed foods and its association with added sugar content in the diets of US children, NHANES 2009–2014. Pediatr. Obes. 2019, 14, e12563. [Google Scholar] [CrossRef]
- Rebolledo, N.; Bercholz, M.; Adair, L.; Corvalán, C.; Ng, S.W.; Taillie, L.S. Sweetener Purchases in Chile before and after Implementing a Policy for Food Labeling, Marketing, and Sales in Schools. Curr. Dev. Nutr. 2023, 7, 100016. [Google Scholar] [CrossRef] [PubMed]
- Bellisle, F.; Hébel, P.; Colin, J.; Reyé, B.; Hopkins, S. Consumption of whole grains in French children, adolescents and adults. Br. J. Nutr. 2014, 112, 1674–1684. [Google Scholar] [CrossRef]
- O’Neil, C.E.; Nicklas, T.A.; Zanovec, M.; Cho, S.S.; Kleinman, R. Consumption of whole grains is associated with improved diet quality and nutrient intake in children and adolescents: The National Health and Nutrition Examination Survey 1999–2004. Public Health Nutr. 2011, 14, 347–355. [Google Scholar] [CrossRef]
- Pinheiro, A.; Quintiliano-Scarpelli, D.; Flores, J.; Álvarez, C.; Suárez-Reyes, M.; Palacios, J.; Quevedo, T.; de Oliveira, M. Food Availability in Different Food Environments Surrounding Schools in a Vulnerable Urban Area of Santiago, Chile: Exploring Socioeconomic Determinants. Foods 2022, 11, 901. [Google Scholar] [CrossRef]
- Poti, J.M.; Popkin, B.M. Trends in energy intake among US children by eating location and food source, 1977–2006. J. Am. Diet. Assoc. 2011, 111, 1156–1164. [Google Scholar] [CrossRef]
- Burrows, T.L.; Martin, R.J.; Collins, C.E. A systematic review of the validity of dietary assessment methods in children when compared with the method of doubly labeled water. J. Am. Diet. Assoc. 2010, 110, 1501–1510. [Google Scholar] [CrossRef]
- Naska, A.; Lagiou, A.; Lagiou, P. Dietary assessment methods in epidemiological research: Current state of the art and future prospects. F1000Research 2017, 6, 926. [Google Scholar] [CrossRef]
- Ministerio de Salud. Guías Alimentarias Para Chile; Ministerio de Salud: Santiago, Chile, 2022. [Google Scholar]
- FAO. Food-Based Dietary Guidelines-Chile. Available online: https://www.fao.org/nutrition/education/food-dietary-guidelines/regions/countries/chile/en/ (accessed on 13 November 2023).
| PHDI-C Components | PHDI-C Recommended Percentage of Total Caloric Intake for Children a | Children’s Percentage of Total Caloric Intake a,b | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2016 | 2017 | 2018 | 2019 | 2017 vs. 2016 | 2018 vs. 2016 | 2019 vs. 2016 | |||||
| Optimal Value (Range) | Mean (95%CI) | Mean (95%CI) | Mean (95%CI) | Mean (95%CI) | Diff (95%CI) | p-Value | Diff (95%CI) | p-Value | Diff (95%CI) | p-Value | |
| Adequacy components | |||||||||||
| Nuts and peanuts | ≥11.6 (0, 100) | 0.34 (0.19, 0.49) | 0.39 (0.24, 0.54) | 0.44 (0.29, 0.59) | 0.27 (0.12, 0.42) | 0.05 (−0.16, 0.25) | 0.654 | 0.1 (−0.11, 0.3) | 0.349 | −0.07 (−0.28, 0.13) | 0.489 |
| Legumes | ≥11.3 (0, 100) | 2.23 (1.89, 2.57) | 2.05 (1.71, 2.39) | 1.56 (1.22, 1.9) | 1.06 (0.72, 1.40) | −0.18 (−0.66, 0.29) | 0.456 | −0.67 (−1.14, −0.20) | 0.005 | −1.18 (−1.65, −0.7) | <0.001 |
| Fruits | ≥5.0 (0, 100) | 4.93 (4.55, 5.32) | 4.8 (4.41, 5.19) | 4.5 (4.11, 4.89) | 4.49 (4.10, 4.88) | −0.14 (−0.64, 0.37) | 0.596 | −0.43 (−0.93, 0.07) | 0.091 | −0.44 (−0.94, 0.06) | 0.083 |
| Vegetables | ≥3.1 (0, 100) | 1.43 (1.32, 1.54) | 1.46 (1.35, 1.57) | 1.28 (1.17, 1.39) | 1.48 (1.37, 1.59) | 0.03 (−0.12, 0.17) | 0.715 | −0.15 (−0.29, −0.01) | 0.041 | 0.05 (−0.09, 0.19) | 0.490 |
| Ratio components | |||||||||||
| DGV ratio | 29.5 (0, 100) | 5.66 (4.4, 6.91) | 4.99 (3.73, 6.26) | 4.62 (3.36, 5.88) | 4.49 (3.24, 5.75) | −0.66 (−2.41, 1.09) | 0.46 | −1.03 (−2.78, 0.71) | 0.246 | −1.16 (−2.9, 0.58) | 0.191 |
| ReV ratio | 38.5 (0, 100) | 40.25 (37.86, 42.64) | 39.81 (37.41, 42.22) | 36.77 (34.38, 39.16) | 38.58 (36.19, 40.96) | −0.44 (−3.71, 2.84) | 0.794 | −3.48 (−6.74, −0.23) | 0.036 | −1.67 (−4.92, 1.58) | 0.313 |
| WC ratio | 75.0 (0, 100) | 4.89 (3.74, 6.04) | 7.62 (6.46, 8.77) | 6.19 (5.04, 7.33) | 9.3 (8.16, 10.45) | 2.73 (1.18, 4.27) | 0.001 | 1.3 (−0.24, 2.84) | 0.098 | 4.41 (2.88, 5.95) | <0.001 |
| Optimum components | |||||||||||
| Cereals | 30.0 (0, 60.0) | 25.32 (24.57, 26.08) | 27.09 (26.33, 27.85) | 28.69 (27.94, 29.45) | 29.44 (28.69, 30.20) | 1.76 (0.74, 2.78) | 0.001 | 3.37 (2.36, 4.38) | <0.001 | 4.12 (3.11, 5.13) | <0.001 |
| Tubers and potatoes | 1.6 (0, 3.1) | 3.4 (3, 3.79) | 3.71 (3.31, 4.11) | 3.72 (3.33, 4.12) | 3.68 (3.28, 4.07) | 0.31 (−0.24, 0.87) | 0.272 | 0.33 (−0.23, 0.88) | 0.249 | 0.28 (−0.27, 0.83) | 0.318 |
| Dairy products | 12.2 (0, 24.4) | 19.95 (19.17, 20.73) | 18.75 (17.97, 19.53) | 16.49 (15.71, 17.27) | 16.07 (15.29, 16.84) | −1.2 (−2.16, −0.24) | 0.014 | −3.46 (−4.42, −2.51) | <0.001 | −3.89 (−4.84, −2.93) | <0.001 |
| Eggs and white meats | 6.2 (0, 12.2) | 5.74 (5.2, 6.29) | 6.01 (5.46, 6.56) | 6.62 (6.07, 7.16) | 6.61 (6.07, 7.15) | 0.27 (−0.47, 1.01) | 0.474 | 0.87 (0.14, 1.61) | 0.019 | 0.87 (0.14, 1.60) | 0.020 |
| Vegetable oils | 14.1 (0, 28.3) | 10.41 (9.91, 10.92) | 10.31 (9.80, 10.82) | 9.83 (9.32, 10.33) | 10.00 (9.49, 10.50) | −0.1 (−0.79, 0.59) | 0.770 | −0.59 (−1.27, 0.1) | 0.094 | −0.41 (−1.1, 0.27) | 0.236 |
| Moderation components | |||||||||||
| Palm oil | 0.0 (0, 2.4) | 3.37 (3.02, 3.72) | 3.78 (3.42, 4.13) | 4.5 (4.15, 4.85) | 4.67 (4.32, 5.02) | 0.4 (−0.07, 0.87) | 0.094 | 1.13 (0.66, 1.60) | <0.001 | 1.30 (0.83, 1.77) | <0.001 |
| Red meats | 0.0 (0, 2.4) | 4.43 (3.89, 4.97) | 5.33 (4.79, 5.87) | 5.78 (5.24, 6.32) | 5.62 (5.08, 6.16) | 0.9 (0.17, 1.63) | 0.016 | 1.35 (0.63, 2.08) | <0.001 | 1.19 (0.47, 1.92) | 0.001 |
| Animal fats | 0.0 (0, 1.4) | 1.77 (1.53, 2.01) | 2.22 (1.98, 2.46) | 2.41 (2.17, 2.65) | 2.41 (2.17, 2.66) | 0.45 (0.12, 0.79) | 0.008 | 0.64 (0.31, 0.98) | <0.001 | 0.64 (0.31, 0.97) | <0.001 |
| Added sugars | 0.0 (0, 4.8) | 16.3 (15.73, 16.87) | 13.46 (12.89, 14.03) | 13.87 (13.3, 14.43) | 13.92 (13.36, 14.49) | −2.84 (−3.58, −2.1) | <0.001 | −2.43 (−3.17, −1.7) | <0.001 | −2.38 (−3.12, −1.64) | <0.001 |
| PHDI-C Components | PHDI-C Possible Scores | Participants’ PHDI-C Scores a | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2016 | 2017 | 2018 | 2019 | 2017 vs. 2016 | 2018 vs. 2016 | 2019 vs. 2016 | |||||
| Points | Mean (95%CI) | Mean (95%CI) | Mean (95%CI) | Mean (95%CI) | Diff (95%CI) | p-Value | Diff (95%CI) | p-Value | Diff (95%CI) | p-Value | |
| Adequacy components | |||||||||||
| Nuts and peanuts | 0–10 | 0.23 (0.13, 0.32) | 0.29 (0.19, 0.39) | 0.34 (0.24, 0.44) | 0.21 (0.11, 0.31) | 0.07 (−0.07, 0.2) | 0.327 | 0.11 (−0.02, 0.25) | 0.102 | −0.01 (−0.15, 0.12) | 0.845 |
| Legumes | 0–10 | 1.46 (1.25, 1.67) | 1.42 (1.21, 1.63) | 1.09 (0.88, 1.3) | 0.75 (0.54, 0.96) | −0.04 (−0.33, 0.25) | 0.803 | −0.37 (−0.66, −0.08) | 0.013 | −0.71 (−1.00, −0.42) | <0.001 |
| Fruits | 0–10 | 5.97 (5.67, 6.27) | 5.72 (5.42, 6.03) | 5.6 (5.29, 5.9) | 5.30 (5.00, 5.60) | −0.25 (−0.64, 0.15) | 0.220 | −0.37 (−0.76, 0.02) | 0.064 | −0.67 (−1.06, −0.28) | 0.001 |
| Vegetables | 0–10 | 4.2 (3.96, 4.44) | 4.07 (3.82, 4.31) | 3.69 (3.45, 3.94) | 4.11 (3.87, 4.35) | −0.14 (−0.45, 0.17) | 0.388 | −0.51 (−0.82, −0.2) | 0.001 | −0.09 (−0.4, 0.22) | 0.566 |
| Ratio components | |||||||||||
| DGV ratio | 0–5 | 0.37 (0.29, 0.44) | 0.34 (0.27, 0.42) | 0.23 (0.16, 0.3) | 0.25 (0.18, 0.32) | −0.02 (−0.12, 0.08) | 0.663 | −0.14 (−0.23, −0.04) | 0.006 | −0.11 (−0.21, −0.02) | 0.024 |
| ReV ratio | 0–5 | 2.37 (2.23, 2.5) | 2.19 (2.05, 2.32) | 1.89 (1.75, 2.02) | 2.07 (1.93, 2.2) | −0.18 (−0.37, 0.01) | 0.057 | −0.48 (−0.67, −0.29) | <0.001 | −0.3 (−0.49, −0.12) | 0.001 |
| WC ratio | 0–10 | 0.59 (0.46, 0.72) | 0.86 (0.73, 0.99) | 0.81 (0.67, 0.94) | 1.1 (0.97, 1.23) | 0.27 (0.1, 0.45) | 0.002 | 0.22 (0.04, 0.39) | 0.015 | 0.52 (0.34, 0.69) | <0.001 |
| Optimum components | |||||||||||
| Cereals | 0–10 | 7.05 (6.9, 7.21) | 7.22 (7.06, 7.38) | 7.17 (7.01, 7.32) | 7.18 (7.03, 7.34) | 0.17 (−0.05, 0.39) | 0.136 | 0.11 (−0.11, 0.33) | 0.318 | 0.13 (−0.09, 0.35) | 0.250 |
| Tubers and potatoes | 0–10 | 0.46 (0.35, 0.57) | 0.31 (0.2, 0.43) | 0.35 (0.24, 0.47) | 0.32 (0.21, 0.43) | −0.14 (−0.3, 0.01) | 0.071 | −0.1 (−0.26, 0.05) | 0.192 | −0.14 (−0.3, 0.01) | 0.074 |
| Dairy products | 0–10 | 3.77 (3.52, 4.03) | 4.12 (3.86, 4.37) | 4.31 (4.06, 4.57) | 4.23 (3.97, 4.48) | 0.34 (−0.00, 0.69) | 0.051 | 0.54 (0.2, 0.88) | 0.002 | 0.46 (0.11, 0.80) | 0.009 |
| Eggs and white meats | 0–10 | 2.87 (2.62, 3.13) | 2.92 (2.67, 3.18) | 3 (2.75, 3.26) | 2.96 (2.70, 3.22) | 0.05 (−0.31, 0.42) | 0.773 | 0.13 (−0.23, 0.49) | 0.477 | 0.09 (−0.27, 0.45) | 0.629 |
| Vegetable oils | 0–10 | 5.57 (5.36, 5.78) | 5.33 (5.12, 5.54) | 5.17 (4.96, 5.38) | 5.01 (4.80, 5.22) | −0.24 (−0.53, 0.04) | 0.097 | −0.41 (−0.69, −0.12) | 0.006 | −0.56 (−0.85, −0.27) | <0.001 |
| Moderation components | |||||||||||
| Palm oil | 0–10 | 4.77 (4.44, 5.1) | 4.23 (3.9, 4.56) | 3.61 (3.28, 3.94) | 3.49 (3.17, 3.82) | −0.54 (−0.98, −0.09) | 0.019 | −1.16 (−1.6, −0.71) | <0.001 | −1.27 (−1.72, −0.83) | <0.001 |
| Red meats | 0–10 | 4.89 (4.53, 5.24) | 4.47 (4.11, 4.83) | 4.19 (3.83, 4.55) | 4.16 (3.8, 4.52) | −0.42 (−0.91, 0.07) | 0.095 | −0.69 (−1.19, −0.2) | 0.006 | −0.73 (−1.22, −0.24) | 0.004 |
| Animal fats | 0–10 | 5.38 (5.03, 5.74) | 4.71 (4.35, 5.06) | 4.47 (4.12, 4.82) | 4.41 (4.06, 4.76) | −0.68 (−1.16, −0.19) | 0.006 | −0.91 (−1.4, −0.43) | <0.001 | −0.97 (−1.45, −0.49) | <0.001 |
| Added sugars | 0–10 | 0.17 (0.06, 0.28) | 0.42 (0.31, 0.53) | 0.4 (0.29, 0.52) | 0.49 (0.38, 0.60) | 0.25 (0.1, 0.4) | 0.001 | 0.23 (0.08, 0.38) | 0.002 | 0.32 (0.17, 0.47) | <0.001 |
| Total PHDI-C score | 0–150 | 50.11 (49.08, 51.15) | 48.64 (47.6, 49.68) | 46.32 (45.28, 47.35) | 46.05 (45.01, 47.08) | −1.47 (−2.83, −0.12) | 0.033 | −3.79 (−5.14, −2.45) | <0.001 | −4.06 (−5.4, −2.72) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Venegas Hargous, C.; Orellana, L.; Corvalan, C.; Allender, S.; Bell, C. Changes in Children’s Adherence to Sustainable Healthy Diets During the Implementation of Chile’s Food Labelling and Advertising Law: A Longitudinal Study (2016–2019). Nutrients 2025, 17, 1041. https://doi.org/10.3390/nu17061041
Venegas Hargous C, Orellana L, Corvalan C, Allender S, Bell C. Changes in Children’s Adherence to Sustainable Healthy Diets During the Implementation of Chile’s Food Labelling and Advertising Law: A Longitudinal Study (2016–2019). Nutrients. 2025; 17(6):1041. https://doi.org/10.3390/nu17061041
Chicago/Turabian StyleVenegas Hargous, Carolina, Liliana Orellana, Camila Corvalan, Steven Allender, and Colin Bell. 2025. "Changes in Children’s Adherence to Sustainable Healthy Diets During the Implementation of Chile’s Food Labelling and Advertising Law: A Longitudinal Study (2016–2019)" Nutrients 17, no. 6: 1041. https://doi.org/10.3390/nu17061041
APA StyleVenegas Hargous, C., Orellana, L., Corvalan, C., Allender, S., & Bell, C. (2025). Changes in Children’s Adherence to Sustainable Healthy Diets During the Implementation of Chile’s Food Labelling and Advertising Law: A Longitudinal Study (2016–2019). Nutrients, 17(6), 1041. https://doi.org/10.3390/nu17061041





