National Trends and Disparities in Complementary Food Diversity Among Infants: A 12-Year Cross-Sectional Birth Cohort Study
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Dietary Practices
2.3. Definitions
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics of the Study Population
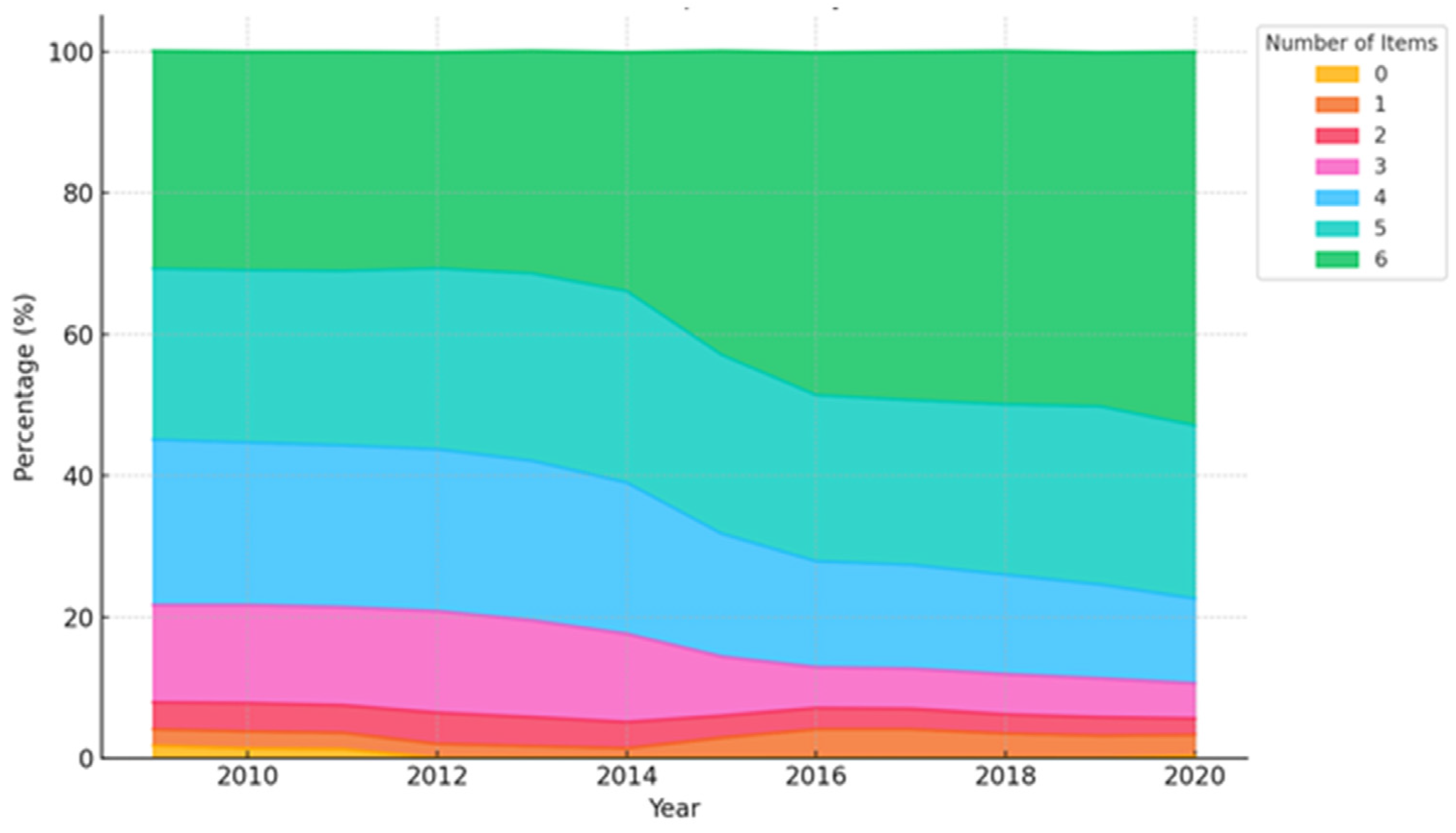
3.2. Trends in Complementary Food Diversity in Infancy from 2009 to 2020
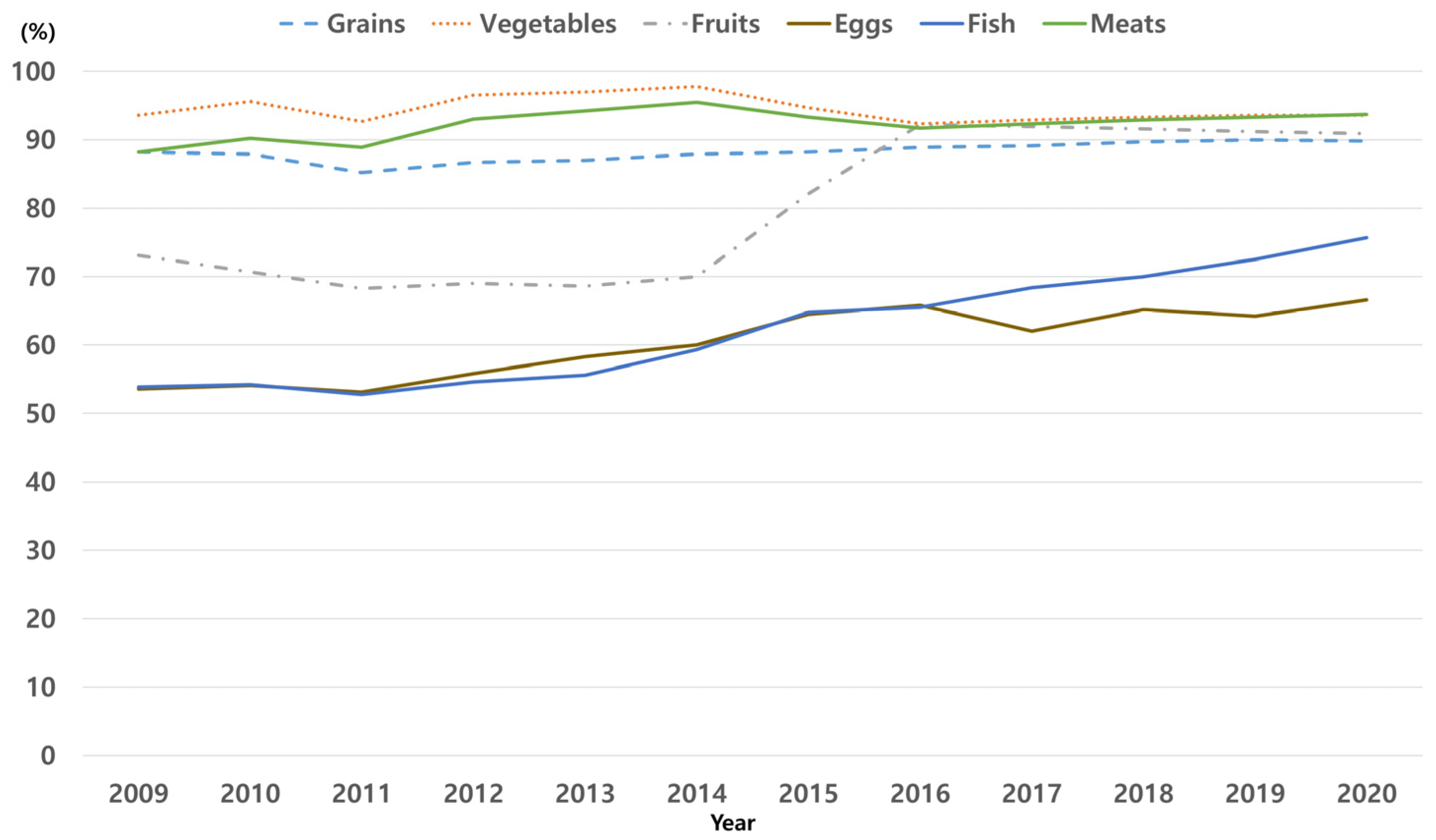
3.3. Consumption Trend of Each Complementary Food Item by Year
3.4. Factors Associated with the Introduction of Low Complementary Food Diversity in Infancy
3.5. Interaction Effects Between Birth Year and Complementary Food Diversity Across Vulnerable Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AAP | American Academy of Pediatrics |
| AD | Atopic dermatitis |
| aORs | Adjusted odds ratios |
| CIs | Confidence intervals |
| FA | Food allergy |
| ICD-10 | International Classification of Diseases, 10th Revision |
| NICK | National Investigation of Birth Cohort in Korea |
| OR | Odds ratio |
References
- Martin-Rodriguez, A.; Bustamante-Sanchez, A.; Martinez-Guardado, I.; Navarro-Jimenez, E.; Plata-SanJuan, E.; Tornero-Aguilera, J.F.; Clemente-Suarez, V.J. Infancy Dietary Patterns, Development, and Health: An Extensive Narrative Review. Children 2022, 9, 1072. [Google Scholar] [CrossRef] [PubMed]
- Fewtrell, M.; Bronsky, J.; Campoy, C.; Domellof, M.; Embleton, N.; Fidler Mis, N.; Hojsak, I.; Hulst, J.M.; Indrio, F.; Lapillonne, A.; et al. Complementary Feeding: A Position Paper by the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Krebs, N.F.; Westcott, J.E.; Butler, N.; Robinson, C.; Bell, M.; Hambidge, K.M. Meat as a first complementary food for breastfed infants: Feasibility and impact on zinc intake and status. J. Pediatr. Gastroenterol. Nutr. 2006, 42, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Agostoni, C.; Decsi, T.; Fewtrell, M.; Goulet, O.; Kolacek, S.; Koletzko, B.; Michaelsen, K.F.; Moreno, L.; Puntis, J.; Rigo, J.; et al. Complementary feeding: A commentary by the ESPGHAN Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2008, 46, 99–110. [Google Scholar] [CrossRef]
- Kleinman, R.E. American Academy of Pediatrics recommendations for complementary feeding. Pediatrics 2000, 106, 1274. [Google Scholar] [CrossRef]
- Greer, F.R.; Sicherer, S.H.; Burks, A.W.; American Academy of Pediatrics Committee on Nutrition and Section on Allergy and Immunology. Effects of early nutritional interventions on the development of atopic disease in infants and children: The role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas. Pediatrics 2008, 121, 183–191. [Google Scholar] [CrossRef]
- Abrams, E.M.; Shaker, M.; Stukus, D.; Mack, D.P.; Greenhawt, M. Updates in Food Allergy Prevention in Children. Pediatrics 2023, 152, e2023062836. [Google Scholar] [CrossRef]
- Howe, L.; Franxman, T.; Teich, E.; Greenhawt, M. What affects quality of life among caregivers of food-allergic children? Ann. Allergy Asthma Immunol. 2014, 113, 69–74.e62. [Google Scholar] [CrossRef]
- Casale, T.B.; Warren, C.; Gupta, S.; Schuldt, R.; Wang, R.; Iqbal, A.; Seetasith, A.; Gupta, R. The mental health burden of food allergies: Insights from patients and their caregivers from the Food Allergy Research & Education (FARE) Patient Registry. World Allergy Organ. J. 2024, 17, 100891. [Google Scholar] [CrossRef]
- Fernandez-Alvira, J.M.; Bornhorst, C.; Bammann, K.; Gwozdz, W.; Krogh, V.; Hebestreit, A.; Barba, G.; Reisch, L.; Eiben, G.; Iglesia, I.; et al. Prospective associations between socio-economic status and dietary patterns in European children: The Identification and Prevention of Dietary- and Lifestyle-induced Health Effects in Children and Infants (IDEFICS) Study. Br. J. Nutr. 2015, 113, 517–525. [Google Scholar] [CrossRef]
- Meneghelli, M.; Toniazzo, S.; Priante, E.; Cavicchiolo, M.E.; De Terlizzi, F.; Gaio, P.; Spinella, P.; Verlato, G. Complementary feeding in infants born preterm: Aspects needing improvement. JPGN Rep. 2024, 5, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Lee, J.E.; Shim, S.M.; Ha, E.K.; Yon, D.K.; Kim, O.H.; Baek, J.H.; Koh, H.Y.; Chae, K.Y.; Lee, S.W.; et al. Cohort profile: National Investigation of Birth Cohort in Korea study 2008 (NICKs-2008). Clin. Exp. Pediatr. 2021, 64, 480–488. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Lee, E.; Ha, E.K.; Shin, J.; Lee, G.C.; Rha, Y.H.; Han, M.Y. Cascade of atopic dermatitis comorbidities in children after birth for 15 years. Allergy 2024, 79, 153–163. [Google Scholar] [CrossRef]
- Leone, L.; Mazzocchi, A.; Maffeis, L.; De Cosmi, V.; Agostoni, C. Nutritional management of food allergies: Prevention and treatment. Front. Allergy 2022, 3, 1083669. [Google Scholar] [CrossRef] [PubMed]
- Greer, F.R.; Sicherer, S.H.; Burks, A.W.; Committee On, N.; Committee on Nutrition and Section on Allergy and Immunology. The Effects of Early Nutritional Interventions on the Development of Atopic Disease in Infants and Children: The Role of Maternal Dietary Restriction, Breastfeeding, Hydrolyzed Formulas, and Timing of Introduction of Allergenic Complementary Foods. Pediatrics 2019, 143, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Group, N.S. Timing of initiation, patterns of breastfeeding, and infant survival: Prospective analysis of pooled data from three randomised trials. Lancet Glob. Health 2016, 4, e266–e275. [Google Scholar] [CrossRef]
- Panjwani, A.; Heidkamp, R. Complementary Feeding Interventions Have a Small but Significant Impact on Linear and Ponderal Growth of Children in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis. J. Nutr. 2017, 147, 2169S–2178S. [Google Scholar] [CrossRef]
- van der Burg, M.P.; Scheringa, M.; Basir, I.; Bouwman, E. Assessment of isolated islet equivalents. Transplant. Proc. 1997, 29, 1971–1973. [Google Scholar] [CrossRef]
- Jin, J.H.; Lee, S.A.; Yoon, S.W. Medical Utilization and Costs in Preterm Infants in the First 6 Years of Life After Discharge From Neonatal Intensive Care Unit: A Nationwide Population-Based Study in Korea. J. Korean Med. Sci. 2022, 37, e93. [Google Scholar] [CrossRef]
- Gatica-Dominguez, G.; Neves, P.A.R.; Barros, A.J.D.; Victora, C.G. Complementary Feeding Practices in 80 Low- and Middle-Income Countries: Prevalence of and Socioeconomic Inequalities in Dietary Diversity, Meal Frequency, and Dietary Adequacy. J. Nutr. 2021, 151, 1956–1964. [Google Scholar] [CrossRef]
- Fernandez-Alvira, J.M.; Bammann, K.; Eiben, G.; Hebestreit, A.; Kourides, Y.A.; Kovacs, E.; Michels, N.; Pala, V.; Reisch, L.; Russo, P.; et al. Prospective associations between dietary patterns and body composition changes in European children: The IDEFICS study. Public Health Nutr. 2017, 20, 3257–3265. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Garcia, A.L.; Huang, J.; Wright, C.M. Associations between breastfeeding duration and adherence to complementary feeding recommendations in Scotland. Matern. Child. Nutr. 2024, 20, e13633. [Google Scholar] [CrossRef] [PubMed]
- Woo, J.G.; Herbers, P.M.; McMahon, R.J.; Davidson, B.S.; Ruiz-Palacios, G.M.; Peng, Y.M.; Morrow, A.L. Longitudinal Development of Infant Complementary Diet Diversity in 3 International Cohorts. J. Pediatr. 2015, 167, 969–974.e1. [Google Scholar] [CrossRef] [PubMed]
| n (%) or Mean (SD) | Total | 2009–2012 | 2013–2016 | 2017–2020 | ||||
|---|---|---|---|---|---|---|---|---|
| Total number | 3,425,301 | 100.0% | 975,997 | 28.5% | 1,299,823 | 37.9% | 1,152,481 | 33.6% |
| Male | 1,764,310 | 51.5% | 502,486 | 51.5% | 668,782 | 51.5% | 593,042 | 51.5% |
| Female | 1,660,991 | 48.5% | 470,511 | 48.2% | 631,041 | 48.5% | 559,439 | 48.5% |
| Age at check-up, median (Q1–Q3) months | 12.0 | (11–12) | 11.0 | (10–12) | 12.0 | (11–12) | 12.0 | (11–13) |
| Birth weight, mean (SD), kg | 3.18 | (0.45) | 3.2 | (0.44) | 3.18 | (0.44) | 3.17 | (0.46) |
| Body weight upon first examination, mean (SD), kg | 8.12 | (1.62) | 8.13 | (1.52) | 8.09 | (1.48) | 8.14 | (1.83) |
| Body weight upon second examination, mean (SD), kg | 9.88 | (1.67) | 9.83 | (1.48) | 9.84 | (1.36) | 9.98 | (2.1) |
| Prematurity | 204,309 | 5.96% | 54,787 | 5.61% | 67,037 | 5.16% | 82,485 | 7.16% |
| Breastfeeding in the first 4 months | 930,724 | 27.17% | 317,166 | 32.50% | 392,549 | 30.20% | 221,009 | 19.18% |
| Residence at birth | ||||||||
| Seoul | 674,397 | 19.7% | 211,772 | 21.7% | 251,113 | 19.3% | 211,512 | 18.4% |
| Metropolitan | 840,215 | 24.5% | 232,252 | 23.8% | 324,745 | 25.0% | 283,218 | 24.6% |
| City | 1,655,396 | 48.3% | 450,748 | 46.2% | 627,122 | 48.2% | 577,526 | 50.1% |
| Rural | 233,355 | 6.8% | 67,000 | 6.9% | 86,801 | 6.7% | 79,554 | 6.9% |
| Socioeconomic status | ||||||||
| Low (≤25 percentile) | 24.9% | 244,771 | 25.1% | 325,360 | 25.0% | 289,056 | 25.1% | |
| Intermediate (>25 percentile and ≤75 percentile) | 1,687,741 | 49.3% | 472,516 | 48.4% | 631,953 | 48.6% | 568,202 | 49.3% |
| High (>75 percentile) | 864,195 | 25.2% | 244,485 | 25.0% | 329,468 | 25.3% | 294,552 | 25.6% |
| Condition(s) originating in the perinatal period | 1,874,450 | 54.7% | 498,802 | 51.1% | 701,641 | 54.0% | 671,007 | 58.2% |
| Birth trauma (P10–P159) | 47,235 | 1.4% | 10,307 | 1.1% | 16,894 | 1.3% | 20,034 | 1.7% |
| Respiratory and cardiovascular disorder specific to the perinatal period (P20–P299) | 310,062 | 9.1% | 67,569 | 6.9% | 111,780 | 8.6% | 130,713 | 11.3% |
| Infections specific to the perinatal period (P35–P399) | 486,150 | 14.2% | 140,095 | 14.4% | 178,577 | 13.7% | 167,478 | 14.5% |
| Hemorrhagic and hematological disorders of fetus and newborn (P50–P619) | 1,255,963 | 36.7% | 331,304 | 33.9% | 476,984 | 36.7% | 447,675 | 38.8% |
| Transitory endocrine and metabolic disorders (P70–P749) | 238,494 | 7.0% | 45,673 | 4.7% | 93,120 | 7.2% | 99,701 | 8.7% |
| Digestive system disorders of fetus and newborn (P75–P789) | 67,085 | 2.0% | 26,136 | 2.7% | 24,600 | 1.9% | 16,349 | 1.4% |
| Conditions involving the integument and temperature regulation (P80–P849) | 138,876 | 4.1% | 39,379 | 4.0% | 49,735 | 3.8% | 49,762 | 4.3% |
| Congenital malformations, deformations, and other disorders originating in the perinatal period (P90–P969) | 207,166 | 6.0% | 60,596 | 6.2% | 75,128 | 5.8% | 71,452 | 6.2% |
| Chromosomal anomaly | 22,111 | 0.6% | 4385 | 0.4% | 6841 | 0.5% | 10,885 | 0.9% |
| Hospitalization owing to wheezing before check-up | 604,764 | 17.7% | 90,730 | 9.3% | 142,113 | 10.9% | 129,021 | 11.2% |
| Atopic dermatitis before check-up | 587,043 | 17.1% | 241,520 | 24.7% | 218,498 | 16.8% | 127,025 | 11.0% |
| Food allergy before check-up | 29,249 | 0.9% | 7965 | 0.8% | 10,846 | 0.8% | 10,438 | 0.9% |
| Food Item | aOR 1 | 95% Lower | 95% Upper | p Value |
|---|---|---|---|---|
| Grains | 1.0034 | 1.0030 | 1.0038 | <0.0001 |
| Vegetables | 0.9973 | 0.9969 | 0.9977 | <0.0001 |
| Fruits | 1.0345 | 1.0341 | 1.0349 | <0.0001 |
| Eggs | 1.0207 | 1.0202 | 1.0212 | <0.0001 |
| Fish | 1.0374 | 1.0369 | 1.0379 | <0.0001 |
| Meats | 1.0019 | 1.0015 | 1.0023 | <0.0001 |
| Variables, n (%) or Mean (SD) | High Food Diversity 1 | Low Food Diversity 2 | aOR 3 | 95% Lower | 95% Upper | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Sex | |||||||
| Male | 716,513 | 40.6% | 1,047,797 | 59.4% | Ref | ||
| Female | 672,083 | 40.5% | 988,908 | 59.5% | 1.005 | 1.002 | 1.008 |
| Month at second check-up, mean (SD) | 6.37 | (3.39) | 6.44 | (3.35) | 1.002 | 1.0015 | 1.0024 |
| Birth weight, mean (SD), kg | |||||||
| ≥2.5 kg | 1,321,650 | 40.6% | 1,932,066 | 59.4% | Ref | ||
| <2.5 kg | 66,946 | 39.0% | 104,639 | 61.0% | 1.018 | 1.009 | 1.027 |
| Body weight at first check-up, mean (SD), kg | 8.14 | (1.60) | 8.11 | (1.64) | |||
| Body weight at second check-up, mean (SD), kg | 9.96 | (1.72) | 9.83 | (1.64) | |||
| Prematurity | |||||||
| No | 1,307,522 | 40.6% | 1,913,470 | 59.4% | Ref | ||
| Yes | 81,074 | 39.7% | 123,235 | 60.3% | 1.009 | 1.001 | 1.017 |
| Breastfeeding in the first 4 months | |||||||
| Yes | 385,326 | 41.4% | 545,398 | 58.6% | Ref | ||
| No | 808,473 | 42.7% | 1,086,711 | 57.3% | 1.041 | 1.038 | 1.045 |
| Birth residence | |||||||
| Seoul | 287,553 | 42.6% | 386,844 | 57.4% | Ref | ||
| Metropolitan | 330,195 | 39.3% | 510,020 | 60.7% | 1.088 | 1.080 | 1.097 |
| City | 672,576 | 40.6% | 982,820 | 59.4% | 1.054 | 1.044 | 1.063 |
| Rural | 91,201 | 39.1% | 142,154 | 60.9% | 1.045 | 1.034 | 1.057 |
| Socioeconomic factors | |||||||
| Low (≤25 P) | 355,438 | 41.7% | 495,989 | 58.3% | Ref | ||
| Intermediate (>25 P and ≤75 P) | 690,299 | 40.9% | 997,442 | 59.1% | 0.983 | 0.976 | 0.991 |
| High (>75 percentile) | 335,788 | 38.9% | 528,407 | 61.1% | 1.027 | 1.018 | 1.063 |
| Year of examination, mean (SD) | 2015.39 | 3.19 | 2014.29 | 3.22 | 0.9554 | 0.9549 | 0.9559 |
| Condition(s) originating in the perinatal period | |||||||
| No | 626,409 | 40.4% | 924,442 | 59.6% | Ref | ||
| Yes | 762,187 | 40.7% | 1,112,263 | 59.3% | 1.0121 | 1.0089 | 1.0153 |
| Hospitalization owing to wheezing before check-up | |||||||
| No | 993,240 | 41.6% | 1,394,788 | 58.4% | Ref | ||
| Yes | 395,356 | 38.1% | 641,917 | 61.9% | 1.029 | 1.025 | 1.032 |
| Atopic dermatitis before check-up | |||||||
| No | 1,187,243 | 41.8% | 1,651,015 | 58.2% | Ref | ||
| Yes | 201,353 | 34.3% | 385,690 | 65.7% | 1.085 | 1.080 | 1.089 |
| Food allergy before check-up | |||||||
| No | 1,378,930 | 40.6% | 2,017,122 | 59.4% | Ref | ||
| Yes | 9666 | 33.0% | 19,583 | 67.0% | 1.156 | 1.138 | 1.174 |
| Variables | % | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | p for Trend | β Coefficient | p for Interaction |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | male | 30.8 | 30.9 | 32.5 | 30.5 | 31.5 | 34.0 | 43.0 | 48.6 | 47.8 | 50.2 | 50.3 | 53.4 | <0.0001 | 0.0003 | 0.942 |
| female (ref) | 30.8 | 30.9 | 31.0 | 30.6 | 31.4 | 33.7 | 43.1 | 48.5 | 47.6 | 49.9 | 49.8 | 52.4 | ||||
| Birth weight | <2.5 kg | 29.2 | 29.6 | 28.4 | 28.5 | 30.0 | 32.2 | 40.6 | 45.7 | 44.6 | 47.2 | 46.7 | 50.3 | <0.0001 | −0.002 | 0.605 |
| ≥2.5 kg (ref) | 29.8 | 31.0 | 31.1 | 30.7 | 31.5 | 33.9 | 43.2 | 48.7 | 47.9 | 50.2 | 50.3 | 53.1 | ||||
| Prematurity | yes | 30.9 | 31.0 | 31.1 | 30.7 | 31.5 | 33.9 | 43.1 | 48.7 | 48.3 | 50.2 | 50.3 | 53.1 | <0.0001 | −0.0012 | 0.757 |
| no (ref) | 29.6 | 29.5 | 29.5 | 28.8 | 30.3 | 32.8 | 41.0 | 46.1 | 45.4 | 47.9 | 47.7 | 50.8 | ||||
| BMF in the first 4 months | no | 30.0 | 30.5 | 31.1 | 30.4 | 31.5 | 33.8 | 43.2 | 49.0 | 48.0 | 50.8 | 50.6 | 53.1 | <0.0001 | 0.0004 | 0.920 |
| yes (ref) | 33.3 | 32.9 | 32.9 | 33.4 | 33.8 | 36.8 | 46.2 | 51.3 | 51.1 | 52.9 | 53.1 | 56.1 | ||||
| Birth residence | rural | 30.4 | 30.5 | 30.3 | 30.0 | 30.8 | 33.3 | 42.3 | 47.8 | 47.1 | 49.4 | 49.4 | 52.1 | <0.0001 | 0.0004 | 0.928 |
| Seoul (ref) | 31.8 | 32.9 | 34.0 | 33.2 | 34.2 | 36.0 | 46.0 | 51.7 | 50.4 | 52.6 | 53.0 | 56.4 | ||||
| Socioeconomic status | Low (ref) | 31.5 | 32.1 | 33.0 | 32.3 | 33.0 | 35.0 | 44.9 | 50.4 | 49.3 | 51.6 | 52.2 | 55.4 | <0.0001 | 0.0014 | 0.724 |
| high | 29.3 | 29.1 | 28.7 | 28.3 | 29.7 | 32.3 | 40.9 | 46.4 | 46.0 | 48.5 | 48.8 | 51.7 | ||||
| Any perinatal conditions | yes | 30.6 | 30.4 | 30.6 | 30.2 | 31.1 | 33.5 | 42.7 | 48.2 | 47.3 | 49.7 | 49.7 | 52.8 | <0.0001 | 0.0003 | 0.951 |
| no (ref) | 31.1 | 31.5 | 31.5 | 30.9 | 31.9 | 34.2 | 43.5 | 48.9 | 48.2 | 50.5 | 50.5 | 53.0 | ||||
| Wheezing | yes | 30.9 | 30.9 | 30.3 | 29.0 | 29.8 | 32.7 | 41.2 | 46.2 | 46.3 | 48.2 | 48.7 | 51.4 | <0.0001 | −0.0015 | 0.719 |
| no (ref) | 30.8 | 30.9 | 31.1 | 30.8 | 31.7 | 34.0 | 43.3 | 48.8 | 47.9 | 50.3 | 50.2 | 53.0 | ||||
| AD | yes | 27.7 | 28 | 28.7 | 28.3 | 28.9 | 31.5 | 39.2 | 43.7 | 42.6 | 45.3 | 44.5 | 46.5 | <0.0001 | −0.0018 | 0.644 |
| no (ref) | 32.1 | 31.9 | 31.8 | 31.2 | 32.1 | 34.3 | 43.8 | 49.3 | 48.4 | 50.7 | 50.7 | 50.2 | ||||
| FA | yes | 29.8 | 26.2 | 28.1 | 26.3 | 26.7 | 30 | 35.9 | 37.6 | 37.4 | 36.3 | 37.5 | 39.7 | <0.0001 | −0.0117 | 0.004 |
| no (ref) | 30.8 | 31 | 31 | 30.6 | 31.5 | 33.9 | 43.1 | 48.6 | 47.8 | 50.2 | 50.2 | 53.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, E.; Rhie, S.; Kim, J.H.; Ha, E.K.; Kim, M.S.; Lee, W.S.; Han, B.; Han, M.Y. National Trends and Disparities in Complementary Food Diversity Among Infants: A 12-Year Cross-Sectional Birth Cohort Study. Nutrients 2025, 17, 636. https://doi.org/10.3390/nu17040636
Lee E, Rhie S, Kim JH, Ha EK, Kim MS, Lee WS, Han B, Han MY. National Trends and Disparities in Complementary Food Diversity Among Infants: A 12-Year Cross-Sectional Birth Cohort Study. Nutrients. 2025; 17(4):636. https://doi.org/10.3390/nu17040636
Chicago/Turabian StyleLee, Eun, Seonkyeong Rhie, Ju Hee Kim, Eun Kyo Ha, Min Seo Kim, Won Suk Lee, Boeun Han, and Man Yong Han. 2025. "National Trends and Disparities in Complementary Food Diversity Among Infants: A 12-Year Cross-Sectional Birth Cohort Study" Nutrients 17, no. 4: 636. https://doi.org/10.3390/nu17040636
APA StyleLee, E., Rhie, S., Kim, J. H., Ha, E. K., Kim, M. S., Lee, W. S., Han, B., & Han, M. Y. (2025). National Trends and Disparities in Complementary Food Diversity Among Infants: A 12-Year Cross-Sectional Birth Cohort Study. Nutrients, 17(4), 636. https://doi.org/10.3390/nu17040636






