Abstract
Background: The complementary food introduction and consumption guidelines for atopic dermatitis and food allergy prevention have evolved; however, their impact on infant feeding practices remains unclear. This study aimed to analyze complementary food diversity trends in infants, identify vulnerable infants with limited food diversity, and examine the trends in infants with or without vulnerable factors over time. Methods: This study analyzed infants aged 9–12 months who participated in the food diversity survey, conducted as part of the National Health Screening Program in Korea from 2009 to 2020. The complementary food items included grains, vegetables, fruits, eggs, fish, and meats. Infants consuming “six” and “less than six” complementary food items were categorized into high- and low-food-diversity groups, respectively. The study employed logistic regression models to examine the trends in food diversity and vulnerable factors with an assessment of the interaction effects. Results: This study included 3,425,301 participants (51.5% male) aged 11.3 months (standard deviation, 0.8). The high-food-diversity prevalence significantly increased over time, from 30.8% in 2009 to 52.9% in 2020 (p < 0.001). Vulnerable infants included those with preterm birth, low birth weight, non-breastfeeding status, high socioeconomic status, non-Seoul residence at birth, any perinatal conditions, hospitalization due to wheezing, atopic dermatitis and food allergies. The high-diversity proportion increased significantly over the study period across all vulnerable factors (p for interaction < 0.001). However, no significant interactions were observed between the study years and vulnerable factors, except for food allergy (β Coefficient, −0.0117, p for interaction = 0.004). Conclusions: The increasing trends in high-complementary-food-diversity proportions highlight the substantial progress over the study period. However, persistent disparities in vulnerable populations underline the importance of targeted interventions, including tailored nutritional education and policies, that promote equitable dietary practices during early life.
1. Introduction
Complementary food diversity is essential for the nutritional and developmental outcomes of infants, significantly impacting their growth, immune function, and long-term health [1]. Food diversity during infancy can be shaped by various factors, including cultural practices, socioeconomic status, and parental perceptions. Vegetables and fruits supply essential vitamins, minerals, and fiber, contributing to immune health and digestion [2]. Protein-rich foods such as meats, fish, and eggs are critical for muscle development, iron supplementation, and the prevention of micronutrient deficiencies [2,3]. In particular, fish provides omega-3 fatty acids, which are essential for brain development, while eggs serve as a key source of high-quality protein and choline [4]. Although complementary foods provide essential nutrients, certain food groups, such as egg whites, were previously considered highly allergenic and were recommended for delayed introduction [5].
In 2000, the American Academy of Pediatrics (AAP) issued a key guideline recommending the delay of the introduction of allergenic foods (e.g., eggs) until after 1 year of age to mitigate the risk of allergic disease [5]. This recommendation has long influenced feeding practices, despite subsequent evidence challenging its efficacy in allergy prevention [6]. Introducing diverse complementary foods during infancy not only supports optimal growth and development but also serves a critical role in immune system maturation [1]. Consequently, the AAP later revised its guidelines, advising against food restrictions and advocating for the early introduction of assorted foods [6,7].
Despite the updated guidelines on complementary food practice and education, caregivers of infants with vulnerable factors, such as the presence of allergic diseases and premature birth, often encounter heightened anxiety regarding the introduction of multiple complementary foods, leading to delayed or restricted dietary diversity [8,9]. The hesitation, compounded by limited access to reliable information or the fear of potential adverse reactions, reportedly contributes to disparities in food diversity between infants with and without vulnerable factors [10]. In addition, socioeconomic, geographic, and clinical factors may further affect complementary food introduction patterns in infancy [10,11]. However, research on these patterns during infancy is lacking, and comprehensive data on the real-world implementation of these guideline revisions are scarce.
Therefore, we aimed to investigate the temporal consumption trends of six major complementary foods, namely, vegetables, meats, grains, fruits, fish, and eggs, in terms of food diversity in infants aged 9–12 months between 2009 and 2020, following the transition in dietary guidelines. In addition, we sought to elucidate the determinants of complementary food diversity in early life. Determining the consumption trends, along with their associated factors, of diverse complementary foods can aid in improving dietary practices and formulating targeted intervention strategies that promote healthy and diversified dietary practice patterns in early life.
2. Methods
2.1. Study Population
This study was performed as part of the National Investigation of Birth Cohort in Korea 2008 (NICKs-2008), a nationwide, population-based health screening program initiated in 2008 [12]. A total of 3,518,398 infants born between 2008 and 2021 who had undergone regular check-ups at 9–12 months of age were initially considered for the study. Owing to the relatively small number of participants who had completed surveys on complementary food introduction patterns during infancy in 2008 (n = 18,804) and 2021 (n = 74,293), participants born in 2008 and 2021 were excluded from the analysis. Resultantly, 3,425,301 infants born in 2009–2020 who had participated in the surveys on complementary food introduction patterns at 9–12 months were included in the final analysis. Dietary information was collected through caregiver- and parent-reported questionnaires during clinic visits for regular check-ups at 9–12 months of age. This study utilized de-identified individual data authorized for research purposes under the National Health Insurance Act. Ethical approval for the research was obtained in accordance with the Act and relevant guidelines and regulations. The study protocol was reviewed and approved by the Institutional Review Board of the Korea National Institute for Bioethics Policy (P01-201603-21-005). As the study used anonymized, publicly available data, patient consent was not mandatory. The Institutional Review Board of the Korea National Institute for Bioethics Policy waived the requirement for informed consent.
2.2. Dietary Practices
The dietary practices during the complementary feeding introduction period were obtained at 9–12 months of age using the following questionnaire item: “Which types of food do you provide as complementary foods to your baby? (1) grains, (2) vegetables, (3) fruits, (4) eggs, (5) fish, and/or (6) meats”. Caregivers or parents could select all that apply upon completing the questionnaire. The participants were categorized into high- (introduction of six complementary food items) and low- (introduction of less than six complementary food items) food-diversity cohorts based on the number of introduced complementary food items at check-up.
2.3. Definitions
Atopic dermatitis (AD) was defined as having five or more principal diagnoses based on the International Classification of Diseases, 10th Revision, (ICD-10) code for AD (L20.9), reflecting its chronic, relapsing, and remitting inflammatory nature to ensure a more accurate identification of AD cases [13]. Food allergy (FA) was identified based on a principal diagnosis with any of the following ICD-10 codes: T78.0, T78.1, L23.6, L24.6, L25.4, L27.2, and/or K52.294. A wheezing episode was defined as hospital admission with a principal diagnosis based on any of the following ICD-10 codes: J45.X, J46.X, and/or J21.X. All three conditions were restricted to participants diagnosed before the administration of the solid food survey.
The preterm status, defined as birth before 37 weeks of pregnancy, and birth weight were determined based on caregiver-reported questionnaire responses. The breastfeeding status was assessed using survey items inquiring about feeding practices within the first 4 months of life, with participants categorized into the “exclusive breastfeeding” group if they had received breastmilk only. Perinatal conditions were identified using ICD-10 codes ranging from P10 to P96, which include congenital malformations and chromosomal anomalies. Socioeconomic status was determined using insurance income quintiles and categorized into three groups: low (≤25th percentile), intermediate (25th–75th percentile), and high (>75th percentile). Birth residence was classified as Seoul, metropolitan, city, or rural, following the regional classification system of South Korea.
2.4. Statistical Analysis
The demographic characteristics and clinical variables of the study population are summarized as frequencies and percentages for categorical variables and means with standard deviations for continuous variables. To more effectively elucidate the prevalence trend of each demographic variable from 2009 to 2020, the study period was divided into three intervals: 2009–2012, 2013–2016, and 2017–2020.
Reversed stacked area plots were utilized to visually present the cumulative fraction of individuals across complementary food diversity categories. The changes in prevalence rates over time were analyzed by dividing the population into two groups: those who consumed all six types of complementary foods at 9–12 months and those who consumed less than six. To evaluate the trends in the consumption of each complementary food item over time, a logistic regression analysis was performed. The year (2009–2020) was used as an independent variable, whereas the consumption of each complementary food item (grains, vegetables, fruit, eggs, fish, and meats) was treated as a binary dependent variable. The adjusted odds ratios (aORs) and their 95% confidence intervals (CIs) were calculated to assess the direction and magnitude of each trend. All models were adjusted for potential covariates, including sex (male or female), birth weight (continuous), breastfeeding during the first 4 months (yes or no), prematurity (yes or no), AD or FA (yes or no), wheezing episodes (yes or no), birth residence (Seoul or rural), socioeconomic status (tertile: low, intermediate, or high), and certain conditions originating in the perinatal period (yes or no).
The factors associated with low food diversity in early life were analyzed using logistic regression models. AORs with 95% CIs were calculated for each variable after adjusting for confounding factors, such as sex, birth weight, prematurity, breastfeeding during the first 4 months, birth residence, household income level, and any perinatal conditions. The interaction terms (e.g., year × vulnerable factor) were included in the regression models to ascertain whether the relationships between vulnerable factors and high food diversity altered over time. The statistical significance was set at p < 0.05, and all analyses were conducted using SAS (version 9.4; SAS Institute, Inc., Cary, NC, USA).
3. Results
3.1. Baseline Characteristics of the Study Population
The study population comprised 3,425,301 infants whose demographic characteristics are summarized in Table 1. Their median age at the time of the survey was 12 months. The sex distribution was consistent across time periods: 51.5% males and 48.5% females. Birth weight slightly decreased over time (3.2 kg in 2009–2012, 3.18 kg in 2013–2016, and 3.17 kg in 2017–2020). The prevalence of prematurity increased over time from 5.61% (2009–2012) to 7.16% (2017–2020). The breastfeeding rate in the first 4 months exhibited a notable decrease (32.5% in 2009–2012, 30.2% in 2013–2016, and 19.2% in 2017–2020). Most infants were born in cities (48.3%), followed by metropolitan areas (24.5%), Seoul (19.7%), and rural areas (6.8%). Socioeconomic status (income quintiles) remained stable across the three periods. Conditions originating in the perinatal period increased over time. The prevalence of AD displayed a decreasing trend from 24.7% (2009–2012) to 11.0% (2017–2020). The prevalence of hospitalization owing to wheezing or FA diagnosis remained stable over time.

Table 1.
Demographic characteristics of the study population.
3.2. Trends in Complementary Food Diversity in Infancy from 2009 to 2020
Figure 1 illustrates the longitudinal trends in the number of introduced complementary food items in the total population, demonstrating a significantly increasing trend of infants exposed to a greater number of complementary food items (p < 0.0001). The proportion of infants introduced to all six complementary food items markedly increased from 30.8% in 2009 to 52.9% in 2020 (p for trend < 0.001). However, the proportion of infants introduced to three or four types of complementary foods significantly decreased, while no statistically significant changes were observed for those introduced to two or five types of complementary foods over the same period (Figure 1 and Supplementary Table S1).
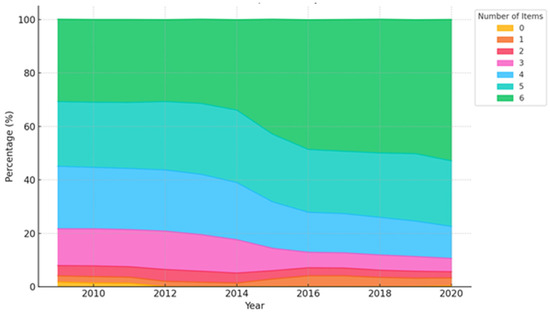
Figure 1.
Trends in the number of consumed complementary food items between 2009 and 2020 in the total population.
3.3. Consumption Trend of Each Complementary Food Item by Year
There was a steady increase in the consumption rates of grains, fruits, eggs, fish, and meats, with fish and fruits showing the most pronounced increase (Figure 2). Conversely, vegetable consumption exhibited a slight decline, despite being consistently high. Table 2 presents the aORs and 95% CIs for the consumption of each complementary food item by year. The odds of consuming fish (aOR = 1.0374; 95% CI: 1.0369–1.0379; p < 0.0001), fruits (aOR = 1.0345; 95% CI: 1.0341–1.0349; p < 0.0001), eggs (aOR = 1.0207; 95% CI: 1.0202–1.0212; p < 0.0001), meats (aOR = 1.0019; 95% CI: 1.0015–1.0023; p < 0.0001), and grains (aOR = 1.0034; 95% CI: 1.003–1.0038; p < 0.0001) increased significantly over time in infants during the study period. However, the odds of vegetable (aOR = 0.9973; 95% CI: 0.9969–0.9977; p < 0.0001) consumption decreased significantly over time, although vegetables exhibited the highest consumption rate among the six complementary food items (Figure 2 and Supplementary Table S2).
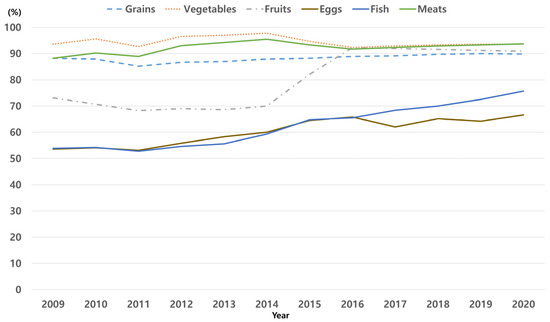
Figure 2.
Trends in the consumption rates of complementary food items among infants aged 9–12 months during the study period.

Table 2.
Adjusted odds ratio and 95% confidence interval for the consumption of each complementary food item over time.
3.4. Factors Associated with the Introduction of Low Complementary Food Diversity in Infancy
Compared with infants exhibiting high complementary food diversity (introduction of all six complementary food items), those displaying low food diversity (five or fewer items) were associated with several demographic, socioeconomic, and clinical factors (Table 3). Infants with a birth weight below 2.5 kg (aOR = 1.018, 95% CI: 1.009–1.027) and preterm birth (aOR = 1.009, 95% CI: 1.001–1.017) were more likely to have low food diversity. Socioeconomic factors also played a role, with infants from high-income families (aOR = 1.027, 95% CI: 1.018–1.063) and those born in metropolitan regions (aOR = 1.088, 95% CI: 1.080–1.097), cities (aOR = 1.054, 95% CI: 1.044–1.063), and rural areas (aOR = 1.045, 95% CI: 1.034–1.057) having higher odds of low food diversity compared with those born in Seoul. Clinically, infants with FA (aOR = 1.156, 95% CI: 1.138–1.174), wheezing (aOR = 1.029, 95% CI: 1.025–1.032), or AD (aOR = 1.085, 95% CI: 1.080–1.089) were significantly associated with low food diversity. Breastfeeding for <4 months was also a contributing factor (aOR = 1.041, 95% CI: 1.038–1.045). Food diversity demonstrated an improving trend over time, as indicated by a significant decrease in the odds of low food diversity in later years (aOR = 0.9554, 95% CI: 0.9549–0.9559).

Table 3.
Factors associated with low food diversity in infancy.
3.5. Interaction Effects Between Birth Year and Complementary Food Diversity Across Vulnerable Factors
The high diversity proportion increased significantly over the study period across all vulnerable factors (p for interaction < 0.001). After identifying the vulnerable factors associated with low food diversity (Table 3), the interaction effects between “year” and “each vulnerable factor” were analyzed to examine the trends in high complementary food diversity over time (Table 4). An analysis of the interaction effects between birth year and high complementary food diversity revealed no significant interactions for most of the vulnerable factors, including sex, birth weight, prematurity, breastfeeding in the first 4 months, birth residence, socioeconomic status, wheezing, and AD. However, a significant negative interaction was observed for FA (β = −0.0117, p = 0.004).

Table 4.
Interaction effects between birth year and high complementary food diversity rate depending on vulnerable factors.
4. Discussion
This study provides comprehensive data on complementary food diversity trends from 2009 to 2020 in infants aged 9–12 months, highlighting the overall improvements while identifying persistent disparities across sociodemographic and health-related factors. The rate of improvement in complementary food consumption in infancy varied across food items; the consumption of grains, fruits, eggs, fish, and meats exhibited increasing trends over the study period, with substantial increases in fish and fruit intakes. Infants with preterm birth, low birth weight, lack of breastfeeding, high socioeconomic status, residence outside Seoul at birth, perinatal conditions, hospitalization for wheezing, atopic dermatitis, and food allergy were associated with low complementary food diversity in infancy. This study highlights the steady increase in high complementary food diversity rates across most vulnerable groups over the study period with slower improvements in dietary diversity in infants with FA. The findings emphasize the importance of tailored interventions for vulnerable populations, particularly those with food allergies, to ensure equitable improvements in dietary diversity.
A comprehensive investigation of the consumption trends of each complementary food item provides insight into how specific food items have been incorporated into infant diets. Over the study period, the consumption of grains, fruits, eggs, fish, and meats significantly increased. Notably, the substantial increase in fish and egg consumption during infancy suggests a shift toward dietary diversity in infancy that aligns with public health guidelines promoting healthy nutrition for infants. This trend potentially reflects enhanced nutrition education, greater food accessibility, and evolving parental practices [14]. Vegetables exhibited the highest consumption rate during the study period, although the odds of vegetable consumption declined slightly over the same period. Although the absolute vegetable intake levels during infancy may remain comparatively high, barriers to vegetable consumption, such as taste preference, accessibility, and socioeconomic factors, need to continue being addressed. Continued efforts are required to sustain high complementary food diversity in infancy, thus ensuring balanced nutrition during early life.
The overall increase in complementary food diversity reflects positive progress in nutritional practices over time, as evidenced by a significant rise in the introduction of diverse food items, such as fish, fruits, and eggs. In particular, the increase in complementary food diversity in infants with AD or FA over time is attributable to evolving nutritional guidelines and their practical implementation. However, despite this progress, infants with FA demonstrated a significantly slower improvement in the prevalence of high complementary food diversity over the study period. In addition, infants with FA exhibited the lower prevalence of high complementary food diversity among all groups, displaying a persistent disparity over time. Caregivers of these infants may avoid introducing complementary foods owing to the risk of exacerbating symptoms or triggering allergic reactions, despite emerging evidence corroborating early and diverse food introduction to prevent allergic disease development [6,7,15]. In addition, infants with wheezing before check-up at 9–12 months exhibited a significantly lower prevalence of high complementary food diversity compared with those without wheezing, and this disparity demonstrated minimal improvement over time. Wheezing episodes are often associated with respiratory infections or early signs of asthma, potentially leading to conservative feeding practices among caregivers, including the delayed introduction of complementary foods owing to fears of triggering allergic or adverse reactions. The persistent inequality suggests a need for improved education on desirable complementary dietary practices for infants with allergic diseases or those at high risk of allergic disease. Collaborative efforts among pediatricians, allergists, and nutritionists can empower caregivers to navigate dietary challenges and promote diverse feeding practices, even in the context of allergic disease.
While the overall trend in complementary food diversity reflects progress, the lack of significant interaction effects between study years and most of the vulnerable factors suggests that improvements were experienced uniformly rather than disproportionately benefiting specific high-risk groups. However, the observed disparity in food diversity trends for infants with FA underscores the unique challenges faced by this group. Despite evolving nutritional guidelines encouraging early allergen introduction, caregivers of FA infants may remain cautious, leading to slower improvements in dietary diversity. The significant negative interaction effect observed for FA supports this concern, indicating that the gap in food diversity between FA and non-FA infants persisted over time. This suggests that general improvements in nutritional practices may not be equally effective for all subpopulations, necessitating more targeted public health efforts. Beyond FA, the absence of significant interaction effects for other vulnerable factors suggests that while food diversity improved, existing disparities in feeding practices were not necessarily reduced. Future research should investigate whether specific barriers, such as misinformation, access to allergen-safe dietary options, or healthcare guidance, contribute to these trends and explore strategies to enhance the effectiveness of dietary interventions for at-risk infants.
Infants with perinatal conditions demonstrated consistently low complementary food diversity compared with those without complications, with the disproportion slightly widening over time. This trend suggests that infants with perinatal issues may encounter unique challenges, such as delayed feeding initiation, medical complications, and prolonged hospital stays [16], potentially impacting early complementary dietary practices. Enhanced medical care and caregiver education over the study period may explain the improvement in complementary food diversity in infancy. Nevertheless, efforts to improve complementary food diversity in infants with perinatal conditions are still warranted.
Infant diet quality with respect to complementary food diversity is important in infant growth and development [17]. A previous cross-sectional study with a smaller sample size reported a lack of dietary diversity in preterm infants during the second half of infancy, especially in those of a low socioeconomic status [18]. In the present study, preterm infants demonstrated a consistently low prevalence of high complementary food diversity compared with full-term infants throughout the study period. Despite the overall improvements in complementary food diversity for both groups, preterm infants lagged behind, underlining ongoing disparities in dietary practices. Prematurity may also be associated with feeding difficulties in early life, developmental delays, and increased parental anxiety regarding complementary food introduction, which may collectively hinder the achievement of high complementary food diversity. The findings of the present study underscore the burgeoning need for targeted nutritional education and support for caregivers of preterm infants, especially considering the increasing prevalence of preterm births in recent years [19]. Socioeconomic factors, including income level and residence area at birth, can significantly influence complementary food diversity in infants owing to a complex interplay between socioeconomic status and complementary feeding practices. Therefore, comprehensive strategies that address economic, educational, and cultural factors to improve complementary dietary diversity are requisite to enhancing nutritional practice in infancy [20]. In this study, a high socioeconomic status was defined as having a household income in the upper 25th percentile. However, income alone may not fully capture dietary practices, as factors such as caregiver education, cultural influences, and food accessibility also play critical roles [20,21]. Future research should consider integrating these dimensions to provide a more comprehensive understanding of the relationship between socioeconomic status and complementary food diversity in infants.
Our study discovered that infants who had been breastfed during the first 4 months exhibited high complementary food diversity. Another study found that infants breastfed for >6 months tend to be introduced to complementary foods later, although their complementary food diversity does not significantly differ from that of formula-fed infants [22]. In contrast, another study reported lower dietary diversity among infants who were predominantly breastfed [23]. These studies suggest that complementary food diversity in breastfed infants is influenced by a combination of factors beyond breastfeeding itself, including regional variations, socioeconomic status, and the impact of nutritional education. These findings underscore the potential role of tailored nutritional strategies and education programs in improving complementary feeding practices, rather than solely attributing outcomes to breastfeeding duration.
Notwithstanding, this study has certain limitations. This study lacks detailed information on dietary patterns, including the introduction timing of each complementary food and frequency of complementary food consumption, limiting our ability to assess their impact on complementary food diversity trends. In addition, parental dietary preferences and family disease history, both of which can significantly influence complementary food introduction patterns, were not accounted for in our analysis. The reliance on self-reported questionnaires introduces short-term recall bias, which may affect the reporting of allergic food introduction and frequency of consumption. The results of the present study have limitations in the interpretation of causal relationships between complementary food introduction patterns and health-related conditions, such as wheezing, AD, or FA. This cross-sectional study provides valuable insights into national trends but does not allow for the assessment of individual changes in complementary feeding practices over time. A prospective cohort study would be needed to examine the evolution of early feeding behaviors and their impact on health outcomes, including allergic diseases.
External influences, including cultural shifts, economic fluctuations, and public health initiatives, were not explicitly accounted for in our analysis. The increasing trend in complementary food diversity may have been influenced by government nutrition programs, evolving infant feeding recommendations, changes in food marketing, and the COVID-19 pandemic, which altered household food availability and caregiver behaviors. Future research should integrate these external determinants into models assessing dietary trends. While this study provides a comprehensive analysis of complementary food diversity trends in South Korea, its findings may not be fully generalizable to other countries with different dietary habits, cultural attitudes, and socioeconomic structures. Furthermore, marginalized populations, including those with lower healthcare access, may be underrepresented in the National Health Screening Program dataset. Future research should prioritize data collection from underrepresented groups to ensure equitable policy recommendations. To address these limitations and reduce disparities in complementary feeding practices, targeted interventions are necessary. Educating caregivers on the benefits and safety of introducing diverse foods early, training healthcare professionals to offer evidence-based nutritional guidance, and implementing food accessibility programs for disadvantaged families could help improve dietary diversity across all socioeconomic groups.
5. Conclusions
Our findings indicate a significant improvement in complementary food diversity among Korean infants from 2009 to 2020. However, disparities persist, particularly among infants with FA and other vulnerable groups. To address these gaps, targeted interventions should include caregiver education on the benefits and safety of diverse complementary food introduction, improved training for healthcare providers to support caregivers in making informed feeding choices, and policies that improve food accessibility for socioeconomically disadvantaged families. Additionally, future research should incorporate external sociocultural and economic influences into dietary diversity trends and employ longitudinal designs to better understand the long-term impact of complementary feeding practices on health outcomes. These measures can promote equitable nutrition and better health outcomes for all infants, particularly those in vulnerable populations.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu17040636/s1, Table S1. Prevalence of the number of complementary food items introduced between 2009 and 2020 in the total population; Table S2. Prevalence of introduced complementary food items between 2009 and 2020 in the total population; Figure S1. Flowchart of the study population.
Author Contributions
E.L. and M.Y.H. formulated the concept and design of this study. E.L., S.R. and M.Y.H. had full access to all study data and assumed responsibility for data integrity and data analysis accuracy. M.Y.H., E.L. and B.H. analyzed the data. E.L., J.H.K., E.K.H., M.S.K., W.S.L., B.H., S.R. and M.Y.H. interpreted the data. E.L. drafted the manuscript. E.L., J.H.K., E.K.H., M.S.K., W.S.L., B.H., S.R. and M.Y.H. critically revised the manuscript for important intellectual content. E.L., S.R. and M.Y.H. sourced for funding. All authors have approved the final manuscript as submitted and agree to be accountable for all aspects of the work. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (grant number: HR22C1605) and a grant (BCRI-24082) given by the Chonnam National University Hospital Biomedical Research Institute. The funders played no role in the study’s design, data collection, interpretation, or the decision to submit the manuscript for publication.
Institutional Review Board Statement
The study protocol was reviewed and approved by the Institutional Review Board of the Hallym University Kangnam Sacred Heart Hospital (No. 2022-10-002, approval date: 14 October 2022).
Informed Consent Statement
As the study used de-identified, publicly available data, patient consent was not required. The Institutional Review Board of the Korea National Institute for Bioethics Policy waived the need for informed consent.
Data Availability Statement
This study utilized data from the National Health Claims Database, maintained by the National Health Insurance Service (NHIS) of the Republic of Korea. The access to this database was granted following a review by the NHIS Research Support Inquiry Committee. Upon approval, the raw data were made available to researchers for a fee. Owing to the intellectual property rights held by the NHIS, we were unable to share the data, analytical methods, or research materials with other researchers. However, the database is available for research purposes, and interested investigators can access it to replicate our findings by following the outlined application process (https://nhiss.nhis.or.kr/, accessed on 12 June 2024).
Conflicts of Interest
The authors declare no competing interests.
Abbreviations
| AAP | American Academy of Pediatrics |
| AD | Atopic dermatitis |
| aORs | Adjusted odds ratios |
| CIs | Confidence intervals |
| FA | Food allergy |
| ICD-10 | International Classification of Diseases, 10th Revision |
| NICK | National Investigation of Birth Cohort in Korea |
| OR | Odds ratio |
References
- Martin-Rodriguez, A.; Bustamante-Sanchez, A.; Martinez-Guardado, I.; Navarro-Jimenez, E.; Plata-SanJuan, E.; Tornero-Aguilera, J.F.; Clemente-Suarez, V.J. Infancy Dietary Patterns, Development, and Health: An Extensive Narrative Review. Children 2022, 9, 1072. [Google Scholar] [CrossRef] [PubMed]
- Fewtrell, M.; Bronsky, J.; Campoy, C.; Domellof, M.; Embleton, N.; Fidler Mis, N.; Hojsak, I.; Hulst, J.M.; Indrio, F.; Lapillonne, A.; et al. Complementary Feeding: A Position Paper by the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Krebs, N.F.; Westcott, J.E.; Butler, N.; Robinson, C.; Bell, M.; Hambidge, K.M. Meat as a first complementary food for breastfed infants: Feasibility and impact on zinc intake and status. J. Pediatr. Gastroenterol. Nutr. 2006, 42, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Agostoni, C.; Decsi, T.; Fewtrell, M.; Goulet, O.; Kolacek, S.; Koletzko, B.; Michaelsen, K.F.; Moreno, L.; Puntis, J.; Rigo, J.; et al. Complementary feeding: A commentary by the ESPGHAN Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2008, 46, 99–110. [Google Scholar] [CrossRef]
- Kleinman, R.E. American Academy of Pediatrics recommendations for complementary feeding. Pediatrics 2000, 106, 1274. [Google Scholar] [CrossRef]
- Greer, F.R.; Sicherer, S.H.; Burks, A.W.; American Academy of Pediatrics Committee on Nutrition and Section on Allergy and Immunology. Effects of early nutritional interventions on the development of atopic disease in infants and children: The role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas. Pediatrics 2008, 121, 183–191. [Google Scholar] [CrossRef]
- Abrams, E.M.; Shaker, M.; Stukus, D.; Mack, D.P.; Greenhawt, M. Updates in Food Allergy Prevention in Children. Pediatrics 2023, 152, e2023062836. [Google Scholar] [CrossRef]
- Howe, L.; Franxman, T.; Teich, E.; Greenhawt, M. What affects quality of life among caregivers of food-allergic children? Ann. Allergy Asthma Immunol. 2014, 113, 69–74.e62. [Google Scholar] [CrossRef]
- Casale, T.B.; Warren, C.; Gupta, S.; Schuldt, R.; Wang, R.; Iqbal, A.; Seetasith, A.; Gupta, R. The mental health burden of food allergies: Insights from patients and their caregivers from the Food Allergy Research & Education (FARE) Patient Registry. World Allergy Organ. J. 2024, 17, 100891. [Google Scholar] [CrossRef]
- Fernandez-Alvira, J.M.; Bornhorst, C.; Bammann, K.; Gwozdz, W.; Krogh, V.; Hebestreit, A.; Barba, G.; Reisch, L.; Eiben, G.; Iglesia, I.; et al. Prospective associations between socio-economic status and dietary patterns in European children: The Identification and Prevention of Dietary- and Lifestyle-induced Health Effects in Children and Infants (IDEFICS) Study. Br. J. Nutr. 2015, 113, 517–525. [Google Scholar] [CrossRef]
- Meneghelli, M.; Toniazzo, S.; Priante, E.; Cavicchiolo, M.E.; De Terlizzi, F.; Gaio, P.; Spinella, P.; Verlato, G. Complementary feeding in infants born preterm: Aspects needing improvement. JPGN Rep. 2024, 5, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Lee, J.E.; Shim, S.M.; Ha, E.K.; Yon, D.K.; Kim, O.H.; Baek, J.H.; Koh, H.Y.; Chae, K.Y.; Lee, S.W.; et al. Cohort profile: National Investigation of Birth Cohort in Korea study 2008 (NICKs-2008). Clin. Exp. Pediatr. 2021, 64, 480–488. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Lee, E.; Ha, E.K.; Shin, J.; Lee, G.C.; Rha, Y.H.; Han, M.Y. Cascade of atopic dermatitis comorbidities in children after birth for 15 years. Allergy 2024, 79, 153–163. [Google Scholar] [CrossRef]
- Leone, L.; Mazzocchi, A.; Maffeis, L.; De Cosmi, V.; Agostoni, C. Nutritional management of food allergies: Prevention and treatment. Front. Allergy 2022, 3, 1083669. [Google Scholar] [CrossRef] [PubMed]
- Greer, F.R.; Sicherer, S.H.; Burks, A.W.; Committee On, N.; Committee on Nutrition and Section on Allergy and Immunology. The Effects of Early Nutritional Interventions on the Development of Atopic Disease in Infants and Children: The Role of Maternal Dietary Restriction, Breastfeeding, Hydrolyzed Formulas, and Timing of Introduction of Allergenic Complementary Foods. Pediatrics 2019, 143, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Group, N.S. Timing of initiation, patterns of breastfeeding, and infant survival: Prospective analysis of pooled data from three randomised trials. Lancet Glob. Health 2016, 4, e266–e275. [Google Scholar] [CrossRef]
- Panjwani, A.; Heidkamp, R. Complementary Feeding Interventions Have a Small but Significant Impact on Linear and Ponderal Growth of Children in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis. J. Nutr. 2017, 147, 2169S–2178S. [Google Scholar] [CrossRef]
- van der Burg, M.P.; Scheringa, M.; Basir, I.; Bouwman, E. Assessment of isolated islet equivalents. Transplant. Proc. 1997, 29, 1971–1973. [Google Scholar] [CrossRef]
- Jin, J.H.; Lee, S.A.; Yoon, S.W. Medical Utilization and Costs in Preterm Infants in the First 6 Years of Life After Discharge From Neonatal Intensive Care Unit: A Nationwide Population-Based Study in Korea. J. Korean Med. Sci. 2022, 37, e93. [Google Scholar] [CrossRef]
- Gatica-Dominguez, G.; Neves, P.A.R.; Barros, A.J.D.; Victora, C.G. Complementary Feeding Practices in 80 Low- and Middle-Income Countries: Prevalence of and Socioeconomic Inequalities in Dietary Diversity, Meal Frequency, and Dietary Adequacy. J. Nutr. 2021, 151, 1956–1964. [Google Scholar] [CrossRef]
- Fernandez-Alvira, J.M.; Bammann, K.; Eiben, G.; Hebestreit, A.; Kourides, Y.A.; Kovacs, E.; Michels, N.; Pala, V.; Reisch, L.; Russo, P.; et al. Prospective associations between dietary patterns and body composition changes in European children: The IDEFICS study. Public Health Nutr. 2017, 20, 3257–3265. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Garcia, A.L.; Huang, J.; Wright, C.M. Associations between breastfeeding duration and adherence to complementary feeding recommendations in Scotland. Matern. Child. Nutr. 2024, 20, e13633. [Google Scholar] [CrossRef] [PubMed]
- Woo, J.G.; Herbers, P.M.; McMahon, R.J.; Davidson, B.S.; Ruiz-Palacios, G.M.; Peng, Y.M.; Morrow, A.L. Longitudinal Development of Infant Complementary Diet Diversity in 3 International Cohorts. J. Pediatr. 2015, 167, 969–974.e1. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).