Impact of L-Citrulline Supplementation and HIIT on Lipid Profile, Arterial Stiffness, and Fat Mass in Obese Adolescents with Metabolic-Dysfunction-Associated Fatty Liver Disease: A Randomized Clinical Trial
Highlights
- High-intensity interval training plus L-citrulline supplementation for 12 weeks improved the aerobic capacity and lipid profile in obese adolescents with metabolic dysfunction-associated fatty liver disease (MASLD).
- High-intensity interval training plus L-citrulline supplementation for 12 weeks did not improve vascular function and blood pressure in obese adolescents with MASLD.
- L-citrulline supplementation alone for 12 weeks decreased the degree of hepatic steatosis in obese adolescents with MASLD.
- The main findings demonstrated that high-intensity interval training plus L-citrulline supplementation could be a complementary therapy for MASLD.
Abstract
1. Introduction
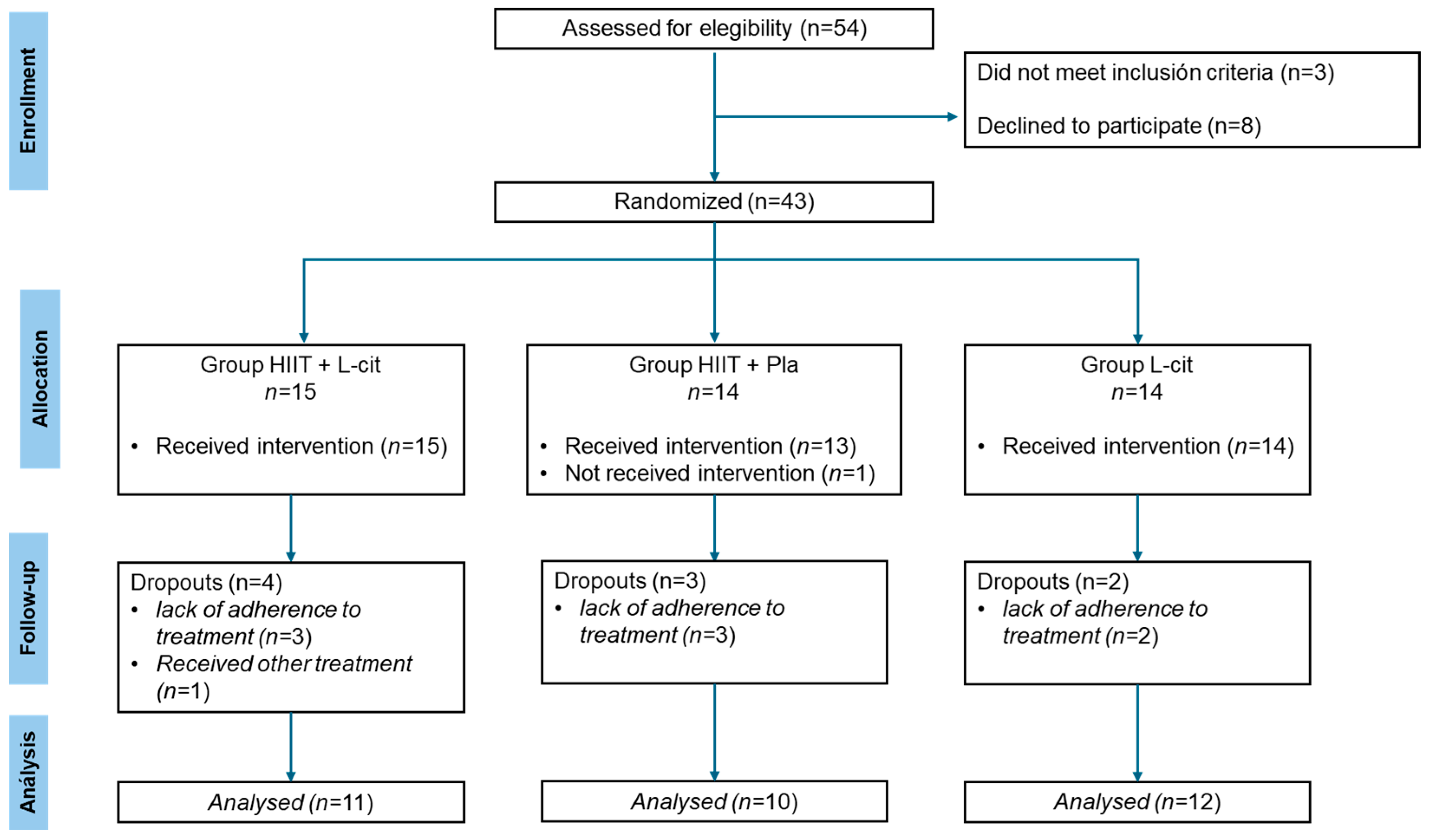
2. Materials and Methods
2.1. Subjects
2.2. Study Design
2.3. Biochemical Analyses
2.4. Peak Oxygen Consumption (VO2peak)
2.5. Blood Pressure and Arterial Function
2.6. Body Composition
2.7. Dietary Assessment
2.8. Interventions
2.9. Ethics Approval
2.10. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. World Health Organization (WHO): Obesity and Overweight. Available online: https://www.who.int/es/news-room/fact-sheets/detail/obesity-and-overweight# (accessed on 13 June 2024).
- Brown, C.L.; Halvorson, E.E.; Cohen, G.M.; Lazorick, S.; Skelton, J.A. Addressing Childhood Obesity. Opportunities for Prevention. Pediatr. Clin. N. Am. 2015, 62, 1241–1261. [Google Scholar] [CrossRef] [PubMed]
- Shamah-Levy, T.; Cuevas-Nasu, L.; Humarán, I.M.G.; Morales-Ruán, C.; Valenzuela-Bravo, D.G.; Gaona-Pineda, E.B.; Ávila-Arcos, M.A.; Rivera-Dommarco, J. Prevalencia y Predisposición a La Obesidad En Una Muestra Nacional de Niños y Adolescentes En México. Salud Publica Mex. 2020, 62, 725–733. [Google Scholar] [CrossRef]
- Jakab, A.E.; Hidvégi, E.V.; Illyés, M.; Cziráki, A.; Kalmár, T.; Maróti, Z.; Bereczki, C. Childhood Obesity: Does It Have Any Effect on Young Arteries? Front. Pediatr. 2020, 8, 389. [Google Scholar] [CrossRef]
- Rtveladze, K.; Marsh, T.; Barquera, S.; Sanchez Romero, L.M.; Levy, D.; Melendez, G.; Webber, L.; Kilpi, F.; McPherson, K.; Brown, M. Obesity Prevalence in Mexico: Impact on Health and Economic Burden. Public Health Nutr. 2014, 17, 233–239. [Google Scholar] [CrossRef]
- Güngör, N.K. Overweight and Obesity in Children and Adolescents. JCRPE J. Clin. Res. Pediatr. Endocrinol. 2014, 6, 129. [Google Scholar] [CrossRef]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Gómez, J.M.; Heitmann, B.L.; Kent-Smith, L.; Melchior, J.C.; Pirlich, M.; et al. Bioelectrical Impedance Analysis—Part I: Review of Principles and Methods. Clin. Nutr. 2004, 23, 1226–1243. [Google Scholar] [CrossRef]
- Mann, J.P.; Goonetilleke, R.; McKiernan, P. Paediatric Non-Alcoholic Fatty Liver Disease: A Practical Overview for Non-Specialists. Arch. Dis. Child. 2015, 100, 673–677. [Google Scholar] [CrossRef]
- Eslam, M.; Alkhouri, N.; Vajro, P.; Baumann, U.; Weiss, R.; Socha, P.; Marcus, C.; Lee, W.S.; Kelly, D.; Porta, G.; et al. Defining Paediatric Metabolic (Dysfunction)-Associated Fatty Liver Disease: An International Expert Consensus Statement. Lancet Gastroenterol. Hepatol. 2021, 6, 864–873. [Google Scholar] [CrossRef]
- Eslam, M.; Newsome, P.N.; Sarin, S.K.; Anstee, Q.M.; Targher, G.; Romero-Gomez, M.; Zelber-Sagi, S.; Wai-Sun Wong, V.; Dufour, J.-F.; Schattenberg, J.M.; et al. A New Definition for Metabolic Dysfunction-Associated Fatty Liver Disease: An International Expert Consensus Statement. J. Hepatol. 2020, 73, 202–209. [Google Scholar] [CrossRef]
- Ramírez-Mejía, M.M.; Díaz-Orozco, L.E.; Barranco-Fragoso, B.; Méndez-Sánchez, N. A Review of the Increasing Prevalence of Metabolic-Associated Fatty Liver Disease (MAFLD) in Children and Adolescents Worldwide and in Mexico and the Implications for Public Health. Med. Sci. Monit. 2021, 27, 341. [Google Scholar] [CrossRef]
- Tran, V.; De Silva, T.M.; Sobey, C.G.; Lim, K.; Drummond, G.R.; Vinh, A.; Jelinic, M. The Vascular Consequences of Metabolic Syndrome: Rodent Models, Endothelial Dysfunction, and Current Therapies. Front. Pharmacol. 2020, 11, 148. [Google Scholar] [CrossRef] [PubMed]
- Curis, E.; Nicolis, I.; Moinard, C.; Osowska, S.; Zerrouk, N.; Bénazeth, S.; Cynober, L. Almost All about Citrulline in Mammals. Amino Acids 2005, 29, 177–205. [Google Scholar] [CrossRef]
- Moinard, C.; MacCario, J.; Walrand, S.; Lasserre, V.; Marc, J.; Boirie, Y.; Cynober, L. Arginine Behaviour after Arginine or Citrulline Administration in Older Subjects. Br. J. Nutr. 2016, 115, 399–404. [Google Scholar] [CrossRef]
- Breuillard, C.; Cynober, L.; Moinard, C. Citrulline and Nitrogen Homeostasis: An Overview. Amino Acids 2015, 47, 685–691. [Google Scholar] [CrossRef]
- Papaioannou, T.G.; Thymis, J.; Benas, D.; Triantafyllidi, H.; Kostelli, G.; Pavlidis, G.; Kousathana, F.; Katogiannis, K.; Vlastos, D.; Lambadiari, V.; et al. Measurement of Central Augmentation Index by Three Different Methods and Techniques: Agreement among Arteriograph, Complior, and Mobil-O-Graph Devices. J. Clin. Hypertens. 2019, 21, 1386–1392. [Google Scholar] [CrossRef]
- Bahadoran, Z.; Mirmiran, P.; Kashfi, K.; Ghasemi, A. Endogenous Flux of Nitric Oxide: Citrulline Is Preferred to Arginine. Acta Physiol. 2021, 231, e13572. [Google Scholar] [CrossRef]
- Maharaj, A.; Fischer, S.M.; Dillon, K.N.; Kang, Y.; Martinez, M.A.; Figueroa, A. Effects of L-Citrulline Supplementation on Endothelial Function and Blood Pressure in Hypertensive Postmenopausal Women. Nutrients 2022, 14, 4396. [Google Scholar] [CrossRef]
- Darabi, Z.; Darand, M.; Yari, Z.; Hedayati, M.; Faghihi, A.; Agah, S.; Hekmatdoost, A. Inflammatory Markers Response to Citrulline Supplementation in Patients with Non-Alcoholic Fatty Liver Disease: A Randomized, Double Blind, Placebo-Controlled, Clinical Trial. BMC Res. Notes 2019, 12, 89. [Google Scholar] [CrossRef]
- Tovar-Villegas, V.I.; Kang, Y.; Ibarra-Reynoso, L.d.R.; Olvera-Juárez, M.; Gomez-Ojeda, A.; Bosquez-Mendoza, V.M.; Maldonado-Ríos, M.L.; Garay-Sevilla, M.E.; Figueroa, A. Oral L-Citrulline Supplementation Improves Fatty Liver and Dyslipidemia in Adolescents with Abdominal Obesity: A Parallel, Double-Blind, Randomized Clinical Trial. Gastroenterol. Insights 2024, 15, 354–365. [Google Scholar] [CrossRef]
- Wong, A.; Alvarez Alvarado, S.; Jaime, S.J.; Kinsey, A.W.; Spicer, M.T.; Madzima, T.A.; Figueroa, A. Combined Whole-Body Vibration Training and L-Citrulline Supplementation Improves Pressure Wave Reflection in Obese Postmenopausal Women. Appl. Physiol. Nutr. Metab. 2015, 41, 292–297. [Google Scholar] [CrossRef]
- Figueroa, A.; Alvarez-Alvarado, S.; Ormsbee, M.J.; Madzima, T.A.; Campbell, J.C.; Wong, A. Impact of L-Citrulline Supplementation and Whole-Body Vibration Training on Arterial Stiffness and Leg Muscle Function in Obese Postmenopausal Women with High Blood Pressure. Exp. Gerontol. 2015, 63, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Ross, L.M.; Porter, R.R.; Durstine, J.L. High-Intensity Interval Training (HIIT) for Patients with Chronic Diseases. J. Sport Health Sci. 2016, 5, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Eather, N.; Riley, N.; Miller, A.; Smith, V.; Poole, A.; Vincze, L.; Morgan, P.J.; Lubans, D.R. Efficacy and Feasibility of HIIT Training for University Students: The Uni-HIIT RCT. J. Sci. Med. Sport 2019, 22, 596–601. [Google Scholar] [CrossRef] [PubMed]
- Chuensiri, N.; Suksom, D.; Tanaka, H. Effects of High-Intensity Intermittent Training on Vascular Function in Obese Preadolescent Boys. Child. Obes. 2018, 14, 41–49. [Google Scholar] [CrossRef]
- Heydari, M.; Boutcher, Y.N.; Boutcher, S.H. The Effects of High-Intensity Intermittent Exercise Training on Cardiovascular Response to Mental and Physical Challenge. Int. J. Psychophysiol. 2013, 87, 141–146. [Google Scholar] [CrossRef]
- De Lira, C.T.; dos Santos, M.A.; Gomes, P.P.; Fidelix, Y.L.; dos Santos, A.C.; Tenório, T.R.; Lofrano-Prado, M.C.; do Prado, W.L. Aerobic Training Performed at Ventilatory Threshold Improves Liver Enzymes and Lipid Profile Related to Non-Alcoholic Fatty Liver Disease in Adolescents with Obesity. Nutr. Health 2017, 23, 281–288. [Google Scholar] [CrossRef]
- Hallsworth, K.; Thoma, C.; Hollingsworth, K.G.; Cassidy, S.; Anstee, Q.M.; Day, C.P.; Trenell, M.I. Modified High-Intensity Interval Training Reduces Liver Fat and Improves Cardiac Function in Non-Alcoholic Fatty Liver Disease: A Randomized Controlled Trial. Clin. Sci. 2015, 129, 1097–1105. [Google Scholar] [CrossRef]
- Abdelbasset, W.K.; Tantawy, S.A.; Kamel, D.M.; Alqahtani, B.A.; Soliman, G.S. A Randomized Controlled Trial on the Effectiveness of 8-Week High-Intensity Interval Exercise on Intrahepatic Triglycerides, Visceral Lipids, and Health-Related Quality of Life in Diabetic Obese Patients with Nonalcoholic Fatty Liver Disease. Medicine 2019, 98, e14918. [Google Scholar] [CrossRef]
- Buckinx, F.; Carvalho, L.P.; Marcangeli, V.; Dulac, M.; Hajj Boutros, G.; Gouspillou, G.; Gaudreau, P.; Noirez, P.; Aubertin-Leheudre, M. High Intensity Interval Training Combined with L-Citrulline Supplementation: Effects on Physical Performance in Healthy Older Adults. Exp. Gerontol. 2020, 140, 111036. [Google Scholar] [CrossRef]
- Kang, Y.; Dillon, K.N.; Martinez, M.A.; Maharaj, A.; Fischer, S.M.; Figueroa, A. Combined L-Citrulline Supplementation and Slow Velocity Low-Intensity Resistance Training Improves Leg Endothelial Function, Lean Mass, and Strength in Hypertensive Postmenopausal Women. Nutrients 2023, 15, 74. [Google Scholar] [CrossRef]
- Ketelhut, S.; Kirchenberger, T.; Ketelhut, R.G. Hemodynamics in Young Athletes Following High-Intensity Interval or Moderate-Intensity Continuous Training. J. Sports Med. Phys. Fit. 2020, 60, 1202–1208. [Google Scholar] [CrossRef] [PubMed]
- Csendes, P.; Paolinelli, P.; Busel, D.; Venturelli, V.; Rodríguez, J. HIGADO GRASO: ULTRASONIDO Y CORRELACION ANATOMOPATOLOGICA. Rev. Chil. Radiol. 2004, 10, 50–52. [Google Scholar] [CrossRef]
- Haskell, W.L.; Lee, I.M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; MacEra, C.A.; Heath, G.W.; Thompson, P.D.; Bauman, A. Physical Activity and Public Health: Updated Recommendation for Adults from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007, 116, 1981. [Google Scholar] [CrossRef]
- Magalhães, J.P.; Santos, D.A.; Correia, I.R.; Hetherington-Rauth, M.; Ribeiro, R.; Raposo, J.F.; Matos, A.; Bicho, M.D.; Sardinha, L.B. Impact of Combined Training with Different Exercise Intensities on Inflammatory and Lipid Markers in Type 2 Diabetes: A Secondary Analysis from a 1-Year Randomized Controlled Trial. Cardiovasc. Diabetol. 2020, 19, 169. [Google Scholar] [CrossRef]
- Figueroa, A.; Trivino, J.A.; Sanchez-Gonzalez, M.A.; Vicil, F. Oral L-Citrulline Supplementation Attenuates Blood Pressure Response to Cold Pressor Test in Young Men. Am. J. Hypertens. 2010, 23, 12–16. [Google Scholar] [CrossRef]
- Schwedhelm, E.; Maas, R.; Freese, R.; Jung, D.; Lukacs, Z.; Jambrecina, A.; Spickler, W.; Schulze, F.; Böger, R.H. Pharmacokinetic and Pharmacodynamic Properties of Oral L-Citrulline and L-Arginine: Impact on Nitric Oxide Metabolism. Br. J. Clin. Pharmacol. 2008, 65, 51–59. [Google Scholar] [CrossRef]
- Figueroa, A.; Sanchez-Gonzalez, M.A.; Perkins-Veazie, P.M.; Arjmandi, B.H. Effects of Watermelon Supplementation on Aortic Blood Pressure and Wave Reflection in Individuals with Prehypertension: A Pilot Study. Am. J. Hypertens. 2011, 24, 40–44. [Google Scholar] [CrossRef]
- Meng, C.; Yucheng, T.; Shu, L.; Yu, Z. Effects of School-Based High-Intensity Interval Training on Body Composition, Cardiorespiratory Fitness and Cardiometabolic Markers in Adolescent Boys with Obesity: A Randomized Controlled Trial. BMC Pediatr. 2022, 22, 112. [Google Scholar] [CrossRef]
- Youssef, L.; Durand, S.; Aprahamian, F.; Lefevre, D.; Bourgin, M.; Maiuri, M.C.; Dulac, M.; Hajj-Boutros, G.; Marcangeli, V.; Buckinx, F.; et al. Serum Metabolomic Adaptations Following a 12-Week High-Intensity Interval Training Combined to Citrulline Supplementation in Obese Older Adults. Eur. J. Sport Sci. 2023, 23, 2157–2169. [Google Scholar] [CrossRef]
- Kudo, M.; Yoshitomi, H.; Momoo, M.; Suguro, S.; Yamagishi, Y.; Gao, M. Evaluation of the Effects and Mechanism of L-Citrulline on Anti-Obesity by Appetite Suppression in Obese/Diabetic KK-Ay Mice and High-Fat Diet Fed SD Rats. Biol. Pharm. Bull. 2017, 40, 524–530. [Google Scholar] [CrossRef]
- Azizi, S.; Mahdavi, R.; Mobasseri, M.; Aliasgharzadeh, S.; Abbaszadeh, F.; Ebrahimi-Mameghani, M. The Impact of L-Citrulline Supplementation on Glucose Homeostasis, Lipid Profile, and Some Inflammatory Factors in Overweight and Obese Patients with Type 2 Diabetes: A Double-Blind Randomized Placebo-Controlled Trial. Phytother. Res. 2021, 35, 3157–3166. [Google Scholar] [CrossRef] [PubMed]
- Bagheripour, F.; Jeddi, S.; Kashfi, K.; Ghasemi, A. Anti-Obesity and Anti-Diabetic Effects of L-Citrulline Are Sex-Dependent. Life Sci. 2024, 339, 122432. [Google Scholar] [CrossRef] [PubMed]
- Julian, V.; Costa, D.; O’Malley, G.; Metz, L.; Fillon, A.; Miguet, M.; Cardenoux, C.; Dutheil, F.; Boirie, Y.; Duclos, M.; et al. Bone Response to High-Intensity Interval Training versus Moderate-Intensity Continuous Training in Adolescents with Obesity. Obes. Facts 2022, 15, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Tong, T.K.; Kong, Z.; Shi, Q.; Liu, Y.; Nie, J. Exercise Training-Induced Visceral Fat Loss in Obese Women: The Role of Training Intensity and Modality. Scand. J. Med. Sci. Sports 2021, 31, 30–43. [Google Scholar] [CrossRef]
- Abassi, W.; Ouerghi, N.; Feki, M.; Jebabli, N.; Andrade, M.S.; Bouassida, A.; Sousa, C.V.; Nikolaidis, P.T.; Weiss, K.; Knechtle, B. Effects of Moderate- vs. High-Intensity Interval Training on Physical Fitness, Enjoyment, and Affective Valence in Overweight/Obese Female Adolescents: A Pre-/Post-Test Study. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 3809–3822. [Google Scholar] [CrossRef]
- Babu, A.F.; Csader, S.; Männistö, V.; Tauriainen, M.M.; Pentikäinen, H.; Savonen, K.; Klåvus, A.; Koistinen, V.; Hanhineva, K.; Schwab, U. Effects of Exercise on NAFLD Using Non-Targeted Metabolomics in Adipose Tissue, Plasma, Urine, and Stool. Sci. Rep. 2022, 12, 6485. [Google Scholar] [CrossRef]
- Maillard, F.; Pereira, B.; Boisseau, N. Effect of High-Intensity Interval Training on Total, Abdominal and Visceral Fat Mass: A Meta-Analysis. Sports Med. 2018, 48, 269–288. [Google Scholar] [CrossRef]
- Bouillanne, O.; Melchior, J.C.; Faure, C.; Paul, M.; Canouï-Poitrine, F.; Boirie, Y.; Chevenne, D.; Forasassi, C.; Guery, E.; Herbaud, S.; et al. Impact of 3-Week Citrulline Supplementation on Postprandial Protein Metabolism in Malnourished Older Patients: The Ciproage Randomized Controlled Trial. Clin. Nutr. 2019, 38, 564–574. [Google Scholar] [CrossRef]
- Moinard, C.; Le Plénier, S.; Cynober, L.; Raynaud-Simon, A. Long-Term Effect of Citrulline Suplementation in Healthy Aged Rats: Effect of Body Composition. Clin. Nutr. Suppl. 2009, 4, 12. [Google Scholar] [CrossRef]
- Luo, P.; Wu, R.; Gao, W.; Yan, W.; Wang, R.; Ye, Y. Effects of High-Intensity Interval Exercise on Arterial Stiffness in Individuals at Risk for Cardiovascular Disease: A Meta-Analysis. Front. Cardiovasc. Med. 2024, 11, 1376861. [Google Scholar] [CrossRef]
- Ochiai, M.; Hayashi, T.; Morita, M.; Ina, K.; Maeda, M.; Watanabe, F.; Morishita, K. Short-Term Effects of L-Citrulline Supplementation on Arterial Stiffness in Middle-Aged Men. Int. J. Cardiol. 2012, 155, 257–262. [Google Scholar] [CrossRef]
- Figueroa, A.; Alvarez-Alvarado, S.; Jaime, S.J.; Kalfon, R. L-Citrulline Supplementation Attenuates Blood Pressure, Wave Reflection and Arterial Stiffness Responses to Metaboreflex and Cold Stress in Overweight Men. Br. J. Nutr. 2016, 116, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Hametner, B.; Wassertheurer, S.; Kropf, J.; Mayer, C.; Eber, B.; Weber, T. Oscillometric Estimation of Aortic Pulse Wave Velocity: Comparison with Intra-Aortic Catheter Measurements. Blood Press. Monit. 2013, 18, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Salvi, P.; Scalise, F.; Rovina, M.; Moretti, F.; Salvi, L.; Grillo, A.; Gao, L.; Baldi, C.; Faini, A.; Furlanis, G.; et al. Noninvasive Estimation of Aortic Stiffness Through Different Approaches. Hypertension 2019, 74, 117–129. [Google Scholar] [CrossRef] [PubMed]
- Golabi, P.; Locklear, C.T.; Austin, P.; Afdhal, S.; Byrns, M.; Gerber, L.; Younossi, Z.M. Effectiveness of Exercise in Hepatic Fat Mobilization in Nonalcoholic Fatty Liver Disease: Systematic Review. World J. Gastroenterol. 2016, 22, 6318–6327. [Google Scholar] [CrossRef]
| HIIT + L-cit (n = 15) | HIIT + Placebo (n = 14) | L-cit (n = 14) | p | ||||
|---|---|---|---|---|---|---|---|
| Age (y) | 16 ± 0.9 | 16.1 ± 0.9 | 16.3 ± 0.7 | 0.92 # | |||
| Male/Female (n) | 2/13 | 2/12 | 6/8 | ||||
| Anthropometry | |||||||
| Weight (kg) | 86 ± 8.6 | 89.4 ± 13.7 | 97.9 ± 20.1 | 0.09 # | |||
| Height (m) | 1.62 ± 0.05 | 1.64 ± 0.1 | 1.67 ± 0.1 | 0.35 # | |||
| BMI (kg/m2) | 32.7 (28.8, 35.3) | 31.75 (29.7, 4) | 32.6 (29.2, 48.6) | 0.78 † | |||
| Abdominal Circumference (cm) | 102 ± 6 | 105 ± 9.8 | 110 ± 12.9 | 0.11 # | |||
| Body Composition | |||||||
| Fat Mass (kg) | 37.9 (30.4, 45.1) | 37.4 (31.6, 60.9) | 38.8 (24.7, 63.7) | 0.86 † | |||
| Body Fat Mass (%) | 44.5 ± 4.1 | 44.4 ± 6.3 | 43 ± 7.3 | 0.74 # | |||
| Visceral Fat Area (cm2) | 178 ± 18.6 | 184 ± 39.6 | 185 ± 42 | 0.81 # | |||
| Muscle Mass | 24.7 (22.7, 37.2) | 26.7 (22.5, 43.9) | 29.2 (21.7, 47) | 0.15 † | |||
| Glucose Control | |||||||
| Glucose (mg/dL) | 93.4 ± 7.5 | 94.2 ± 7.8 | 96.4 ± 13.4 | 0.69 # | |||
| Insulin (µU/mL) | 49 ± 18.4 | 36.9 ± 19.8 | 45.7 ± 28.3 | 0.34 # | |||
| HOMA-IR | 10.4 (4.66, 25.6) | 7.2 (1.2, 21.4) | 8.6 ± 32.1 | 0.23 † | |||
| HbA1C (%) | 4.2 (4.2, 4.8) | 4.2 (4.2, 5.4) | 4.2 ± 0.9 | 0.61 † | |||
| Lipid Profile | |||||||
| Total-C (mg/dL) | 162.4 ± 30.3 | 150.1 ± 19.7 | 167.6 ± 34.3 | 0.26 # | |||
| HDL-C (mg/dL) | 45.1 ± 7.9 | 45.6 ± 12.6 | 43.1 ± 5.9 | 0.72 # | |||
| Non-HDL-C (mg/dL) | 117.3 ± 27.6 | 104.5 ± 15.2 | 124.5 ± 33.8 | 0.14 # | |||
| LDL-C (mg/dL) | 89.5 ± 24.1 | 85.9 ± 14.4 | 98.9 ± 28.1 | 0.30 # | |||
| VLDL-C (mg/dL) | 27.9 ± 13.1 | 18.5 ± 6.3 | 25.6 ± 10.9 | 0.06 # | |||
| Triglyceride (mg/dL) | 139.7 ± 65.8 | 91.1 ± 32.1 | 128.8 ± 54.9 | 0.06 # | |||
| Atherogenic Index | 3.7 ± 0.8 | 3.4 ± 0.7 | 3.9 ± 0.8 | 0.20 # | |||
| Vascular Function | |||||||
| PWV (m/s) | 4.86 ± 0.3 | 4.86 ± 0.3 | 4.92 ± 0.5 | 0.89 # | |||
| AIx75 (%) | 27.2 ± 7.2 | 29.7 ± 8.8 | 28.7 ± 6.4 | 0.67 # | |||
| Arginine (µU/dL) | 64.2 (0.65, 203) | 54.2 (0.3, 263) | 55.4 (0.70, 130.5) | 0.38 † | |||
| Blood Pressure | |||||||
| Systolic (mmHg) | 120 ± 8 | 120 ± 11 | 122 ± 14 | 0.91 # | |||
| Diastolic (mmHg) | 67 ± 6 | 66 ± 5 | 69 ± 9 | 0.62 # | |||
| Median (mmHg) | 85 ± 6 | 84 ± 6 | 86 ± 10 | 0.71 # | |||
| Systolic Central (mmHg) | 118 ± 9 | 115 ± 6 | 119 ± 12 | 0.39 # | |||
| Diastolic Central (mmHg) | 68 ± 6 | 69 ± 8 | 70 ± 10 | 0.89 # | |||
| Pulse Pressure (mmHg) | 53 ± 7 | 54 ± 10 | 53 ± 12 | 0.93 # | |||
| Cardiorespiratory Fitness | |||||||
| VO2peak (mL/kg/min) | 29.3 ± 2.8 | 28.3 ± 3.9 | 27.8 ± 4.5 | 0.55 # | |||
| Heart Rate (bpm) | 78.1 ± 11.7 | 80.1 ± 11.9 | 80.1 ± 14.7 | 0.88 # | |||
| HIIT + L-cit | HIIT + Pla | L-cit | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 11) | (n = 10) | (n = 12) | |||||||||||
| Baseline | Final | p-Value Within Group | ∆ | Baseline | Final | p-Value Within Group | ∆ | Baseline | Final | p-Value Within Group | ∆ | p-Value Between Group | |
| Age | 16 ± 0.89 | 16.10 ± 0.88 | 16.25 ± 0.75 | ||||||||||
| Male/Female | 2/9 | 1/9 | 5/7 | ||||||||||
| Antrhopometry | |||||||||||||
| Weight (kg) | 86.3 ± 9.9 | 85.3 ± 10.2 | 0.06 | −1.1 ± 1.7 | 89.9 ± 15.9 | 89.5 ± 15.3 | 0.69 | −0.4 ± 0.9 | 92.2 ± 15.7 | 92.4 ± 15 | 0.63 | 0.2 ± 1.3 | 0.23 # |
| Height (m) | 1.6 ± 0.1 | 1.6 ± 0.1 | 0.34 | 0 | 1.6 (1.49, 1.92) | 1.6 (1.49, 1.92) | 1 | 0 | 1.7 ± 0.1 | 1.7 ± 0.1 | 0.36 | 0 | 0.36 # |
| Abdominal Circumference (cm) | 101 ± 6.3 | 102 ± 6.7 | 0.68 | −0.5 ± 3.8 | 106 ± 11.1 | 105 ± 8.5 | 0.61 | −0.8 ± 5.2 | 107 ± 12.4 | 108 ± 11.7 | 0.39 | 0.4 ± 4.6 | 0.75 # |
| BMI (kg/m2) | 32.6 ± 2.2 | 32.2 ± 2.4 | 0.03 | −0.5 ± 0.6 | 33.6 ± 3.9 | 33.4 ± 3.4 | 0.69 | −0.1 ± 1.12 | 34.6 ± 5.5 | 34.8 ± 5.5 | 0.57 | 0.2 ± 0.4 | 0.15 # |
| Body Composition | |||||||||||||
| Fat Mass (kg) | 37.8 ± 3.8 | 36 ± 4 | 0.02 | −1.8 ± 2.2 | 40.8 ± 9.6 | 39.9 ± 8.2 | 0.47 | −0.9 ± 3.8 | 41.9 ± 10.8 | 41.7 ± 10.7 | 0.75 | −0.2 ± 2.1 | 0.36 # |
| Body Fat Mass (%) | 43.9 ± 3.4 | 42.3 ± 4.1 | 0.02 | −1.6 ± 1.9 | 45.4 ± 6.32 | 44 ± 5.94 | 0.26 | −1.4 ± 3.8 | 42.9 ± 6.48 | 42.4 ± 6.94 | 0.49 | −0.5 ± 2.4 | 0.60 # |
| Visceral Fat Area (cm2) | 179 ± 17.15 | 168 ± 21.84 | 0.02 | −10.7 ± 13.9 | 192 ± 37.4 | 183 ± 38.2 | 0.18 | −9.1 ± 17.4 | 187 ± 37.3 | 185 ± 37.3 | 0.94 | −1.5 ± 11.4 | 0.21 # |
| Muscle Mass | 24.7 (23, 37.20) | 26.1 (23.1, 38.6) | 0.2 | 1.4 (−2.2, 4.7) | 25.6 (22.9, 43.9) | 25.7 (20.3, 44.9) | 0.26 | 0.1 (−2.6, 2.0) | 29.2 (21.7, 47) | 30.3 (20.3, 47.7) | 0.42 | 1.1 (−1.8, 2.6) | 0.83 † |
| Cardiorespiratory Fitness | |||||||||||||
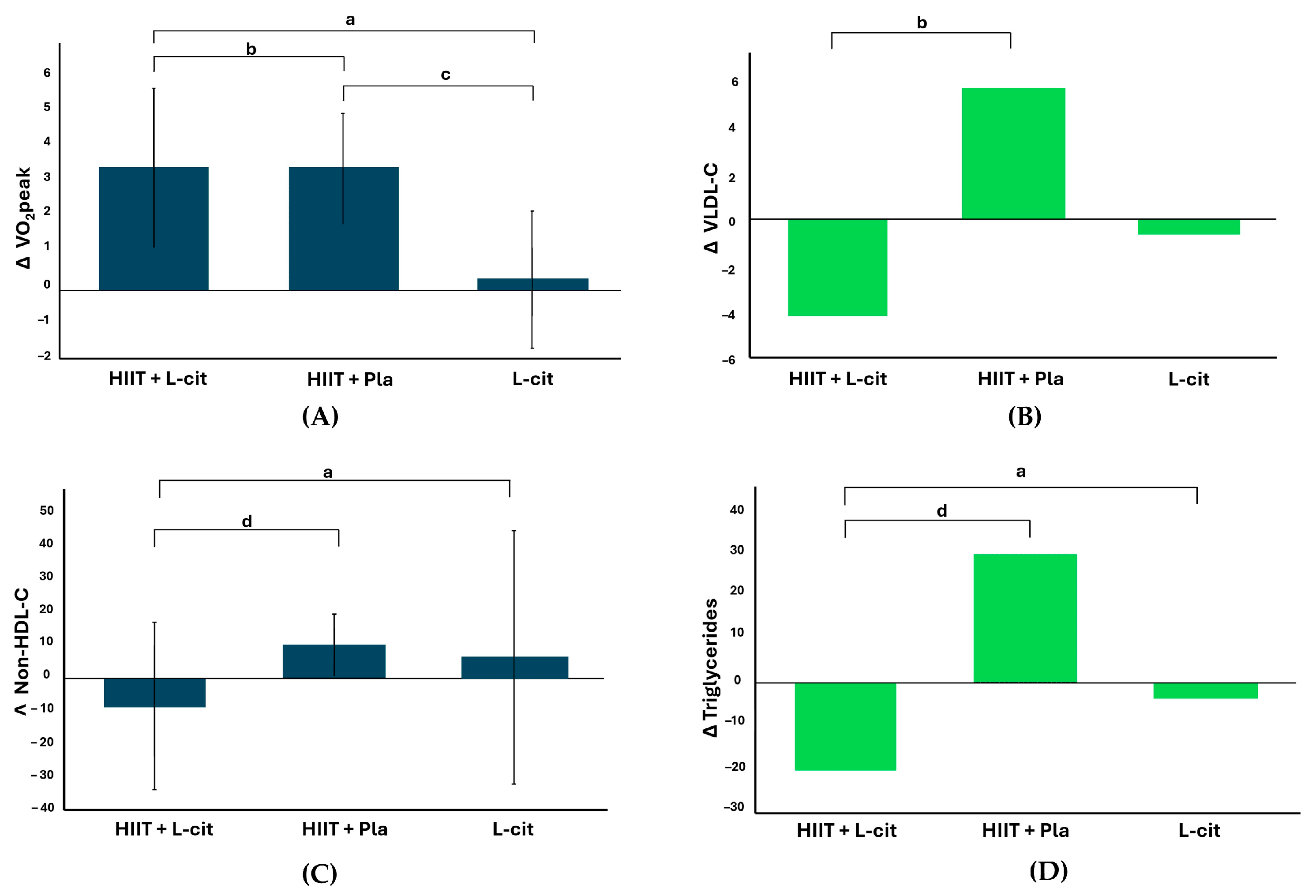
| VO2peak (ml/kg/min) | 29.8 ± 3.1 | 32.6 ± 3.4 | 0.002 | 3.4 ± 2.2 ab | 27.6 ± 3.8 | 30.9 ± 3.8 | <0.0001 | 3.4 ± 1.5 c | 26.8 ± 4.3 | 27.1 ± 4.9 | 0.6 | 0.3 ± 1.9 | 0.001 *# |
| Heart Rate (lpm) | 77.5 ± 12.1 | 75.8 ± 9.1 | 0.59 | −1.5 ± 9.7 | 79 ± 11.6 | 75.5 ± 10.7 | 0.37 | −3.3 ± 11.6 | 82.7 ± 12.4 | 82.5 ± 14.1 | 0.68 | −0.3 ± 9.4 | 0.76 # |
| Glucose Control | |||||||||||||
| Glucose (mg/dL) | 94.1 ± 7.3 | 96.1 ± 4.8 | 0.5 | 2 ± 9.6 | 93.4 ± 8 | 99.8 ± 9.1 | 0.06 | 6.4 ± 9.82 | 94.4 ± 9.8 | 104 ± 9.9 | 0.006 | 10.91 ± 8.43 | 0.08 # |
| Insulin (µU/mL) | 48.9 ± 20.8 | 38.1 ± 13.1 | 0.11 | −10.7 ± 20.6 a | 33.9 ± 17.6 | 33 ± 13.1 | 0.83 | −0.90 ± 13.11 | 46.6 ± 31 | 58.3 ± 37.8 | 0.52 | 11.70 ± 26.21 | 0.05 *# |
| HOMA-IR | 11.6 ± 5.7 | 9.1 ± 3.2 | 0.18 | −2.5 ± 5.9 a | 7.8 ± 3.9 | 8.1 ± 3.2 | 0.75 | 0.35 ± 3.48 | 12 ± 9.7 | 16.6 ± 13.4 | 0.28 | 4.56 ± 7.88 | 0.03 *# |
| HbA1C (%) | 4.2 (4.2, 4.8) | 4.2 (4.2, 5.4) | 0.68 | 0 (−0.6, 1.2) | 4.2 (4.2, 4.9) | 4.2 (4.2, 4.7) | 0.71 | 0 (−0.20, 0.50) | 4.2 (4.2, 4.5) | 4.2 (4.2, 5.8) | 0.71 | 0 (−0.30, 1.50) | 0.56 † |
| Lipid Profile | |||||||||||||
| Total-C (mg/dL) | 169 ± 31.1 | 163.6 ± 29.9 | 0.45 | −5.5 ± 23.1 | 149.3 ± 12.6 | 161.1 ± 14.2 | 0.008 | 11.8 ± 11 | 162.3 ± 32.6 | 173 ± 33.3 | 0.96 | 10.8 ± 39.1 | 0.28 # |
| HDL-C (mg/dL) | 45.6 ± 8.7 | 48.5 ± 10.5 | 0.26 | 2.8 ± 7.9 | 43.2 ± 9.1 | 44.9 ± 7.4 | 0.39 | 1.7 ± 6.1 | 42.8 ± 6.9 | 48.9 ± 7.3 | 0.01 | 4.4 ± 7.3 | 0.67 # |
| LDL-C (mg/dL) | 96.9 ± 21.8 | 96.4 ± 23.8 | 0.88 | 0.5 ± 12.4 | 87.4 ± 7.1 | 95 ± 11.2 | 0.07 | 7.6 ± 12 | 93.5 ± 23.8 | 99.4 ± 24.8 | 0.77 | 5.9 ± 29.7 | 0.62 # |
| VLDL-C (mg/dL) | 20 (12, 61) | 16 (10, 38) | 0.007 | −4 (−5, 2) b | 17 (12, 36) | 20.5 (15, 30) | 0.11 | 5.5 (−19, 11) | 23 (11, 52) | 21.5 (12, 49) | 0.29 | −0.5 (−19, 38) | 0.01 † |
| Non-HDL-C (mg/dL) | 123.4 ± 28.6 | 115.1 ± 27.1 | 0.29 | −8.3 ± 25.1 ad | 106.1 ± 8 | 116.2 ± 11.76 | 0.007 | 10.1 ± 9.3 | 119.3 ± 32.4 | 125.6 ± 32.8 | 0.41 | 6.3 ± 38.8 | 0.04 *# |
| Atherogenic Index | 3.8 ± 0.9 | 3.5 ± 0.9 | 0.39 | −0.3 ± 98 | 3.5 ± 0.6 | 3.7 ± 0.6 | 0.55 | 0.1 ± 0.6 | 3.8 ± 0.8 | 3.8 ± 0.9 | 0.16 | −0.1 ± 1. | 0.40 # |
| Triglyceride (mg/dL) | 98 (62, 306) | 82 (50, 189) | 0.01 | −20 (−250, 12) ad | 83 (59, 181) | 103 (75, 150) | 0.09 | 29.5 (−95, 55) | 117 (53, 260) | 108 (61, 246) | 0.25 | −3.5 (−96, 193) | 0.02 *† |
| Blood Pressure | |||||||||||||
| Systolic (mmHg) | 122 ± 7 | 119 ± 7 | 0.01 | −3 ± 4 | 121 ± 12 | 117 ± 8 | 0.22 | −4 ± 10 | 125 ± 14 | 122 ± 14 | 0.92 | −3 ± 8 | 0.84 # |
| Diastolic (mmHg) | 68 ± 4 | 68 ± 5 | 0.93 | 0 ± 4 | 64 ± 5 | 68 ± 6 | 0.29 | 4 ± 9 | 72 ± 8 | 72 ± 10 | 0.79 | 0 ± 9 | 0.63 # |
| Mean (mmHg) | 86 ± 4 | 85 ± 5 | 0.33 | −1 ± 4 | 83 ± 6 | 84 ± 6 | 0.78 | 1 ± 8 | 89 ± 9 | 89 ± 10 | 0.86 | 0 ± 8 | 0.75 # |
| Systolic Central (mmHg) | 120 ± 10 | 117 ± 9 | 0.08 | −3 ± 5 | 115 ± 6 | 116 ± 9 | 0.16 | 1 ± 7 | 121 ± 13 | 120 ± 12 | 0.59 | −1 ± 10 | 0.47 # |
| Diastolic Central (mmHg) | 69 ± 4 | 68 ± 6 | 0.72 | −1 ± 5 | 68 ± 10 | 69 ± 6 | 0.64 | 1 ± 11 | 73 ± 8 | 74 ± 9 | 0.31 | 1 ± 9 | 0.64 # |
| Pulse Pressure (mmHg) | 55 ± 8 | 51 ± 7 | 0.03 | −4 ± 5 | 57 ± 11 | 50 ± 6 | 0.03 | −7 ± 8 | 53 ± 13 | 52 ± 12 | 0.42 | −1 ± 9 | 0.25 # |
| Vascular Function | |||||||||||||
| PWV (m/s) | 4.95 ± 0.2 | 4.76 ± 0.2 | <0.001 | −0.2 ± 0.1 | 4.9 ± 0.3 | 4.74 ± 0.3 | 0.06 | −0.2 ± 0.2 | 5.01 ± 0.5 | 4.92 ± 0.5 | 0.73 | −0.1 ± 0.3 | 0.57 # |
| AIx75 (%) | 26.5 ± 8.5 | 20.8 ± 10 | 0.06 | −5.7 ± 8.7 | 30.1 ± 8.5 | 26.3 ± 6.9 | 0.08 | −3.9 ± 6.2 | 27.4 ± 8.2 | 26.1 ± 10 | 0.57 | −1.3 ± 9 | 0.51 # |
| Arginine (µU/dL) | 39.5 (0, 69.8) | 50.1 (0, 100.5) | 0.45 | 16.5 (−69.7, 80.2) | 72 (−2.9, 198.9) | 62.4 (−1.9, 201.3) | 0.33 | −3.7 (−14.9, 59.1) | 55.4 (0.7, 103.5) | 64.2 (0, 76.7) | 0.76 | 7.1 (−71.8, 55) | 0.44 † |
| Macronutrients | |||||||||||||
| Calories (kcal) | 2095 ± 552.1 | 1779 ± 494 | 0.07 | 316 ± 529 | 2014 ± 248 | 2152 ± 688 | 0.5 | 139 ± 624 | 2322 ± 837 | 2294 ± 785 | 0.95 | −28.2 ± 423 | 0.14 # |
| Carbohydrates (g) | 266 ± 89.5 | 207 ± 59.7 | 0.02 | 59.5 ± 72.4 | 266 ± 35 | 265 ± 62.1 | 0.95 | −0.9 ± 52.9 | 292.8 ± 127 | 276 ± 118 | 0.68 | −16.6 ±73.6 | 0.13 # |
| Protein (g) | 78.5 ± 23.9 | 70.5 ± 24.3 | 0.32 | 8 ± 25.7 | 77.1 ± 21 | 77.6 ± 22.5 | 0.94 | 0.5 ± 23.4 | 91.1 ± 26.7 | 92.9 ± 29.8 | 0.54 | 1.8 ± 33.9 | 0.51 # |
| Fat (g) | 82.1 ± 25.5 | 77.2 ± 25.9 | 0.61 | −4.9 ± 31.9 | 73.8 ± 23.5 | 89.7 ± 44.6 | 0.26 | 15.9 ± 53.2 | 83.4 ± 31.6 | 89.5 ± 32.5 | 0.39 | 6.1 ± 37 | 0.36 # |
| HIIT + L-cit | Final Steatosis Grade | Total Baseline | X2 | p | |||
|---|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | |||||
| Basal Steatosis Grade | Mild | 0 | 1 | 0 | 1 | 3.841 | 0.43 |
| Moderate | 2 | 3 | 2 | 7 | |||
| Severe | 1 | 0 | 2 | 3 | |||
| Total Final | 3 | 4 | 4 | 11 | |||
| HIIT + Pla | |||||||
| Basal Steatosis Grade | Mild | 2 | 0 | 1 | 3 | 5.667 | 0.23 |
| Moderate | 2 | 4 | 0 | 6 | |||
| Severe | 0 | 1 | 0 | 1 | |||
| Total Final | 4 | 5 | 1 | 10 | |||
| L-cit | |||||||
| Basal Steatosis Grade | Mild | 3 | 0 | 0 | 3 | 6.514 | 0.038 |
| Moderate | 4 | 2 | 0 | 6 | |||
| Severe | 0 | 3 | 0 | 3 | |||
| Total Final | 7 | 5 | 0 | 12 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Carrillo, A.A.; Espinoza-Vargas, M.R.; Vargas-Ortiz, K.; Ibarra-Reynoso, L.d.R.; Olvera-Juárez, M.; Gómez-Ojeda, A.; Garay-Sevilla, M.E.; Figueroa, A. Impact of L-Citrulline Supplementation and HIIT on Lipid Profile, Arterial Stiffness, and Fat Mass in Obese Adolescents with Metabolic-Dysfunction-Associated Fatty Liver Disease: A Randomized Clinical Trial. Nutrients 2025, 17, 402. https://doi.org/10.3390/nu17030402
Rodríguez-Carrillo AA, Espinoza-Vargas MR, Vargas-Ortiz K, Ibarra-Reynoso LdR, Olvera-Juárez M, Gómez-Ojeda A, Garay-Sevilla ME, Figueroa A. Impact of L-Citrulline Supplementation and HIIT on Lipid Profile, Arterial Stiffness, and Fat Mass in Obese Adolescents with Metabolic-Dysfunction-Associated Fatty Liver Disease: A Randomized Clinical Trial. Nutrients. 2025; 17(3):402. https://doi.org/10.3390/nu17030402
Chicago/Turabian StyleRodríguez-Carrillo, Alan Arturo, Mario Ramón Espinoza-Vargas, Katya Vargas-Ortiz, Lorena del Rocío Ibarra-Reynoso, Monserrat Olvera-Juárez, Armando Gómez-Ojeda, Ma. Eugenia Garay-Sevilla, and Arturo Figueroa. 2025. "Impact of L-Citrulline Supplementation and HIIT on Lipid Profile, Arterial Stiffness, and Fat Mass in Obese Adolescents with Metabolic-Dysfunction-Associated Fatty Liver Disease: A Randomized Clinical Trial" Nutrients 17, no. 3: 402. https://doi.org/10.3390/nu17030402
APA StyleRodríguez-Carrillo, A. A., Espinoza-Vargas, M. R., Vargas-Ortiz, K., Ibarra-Reynoso, L. d. R., Olvera-Juárez, M., Gómez-Ojeda, A., Garay-Sevilla, M. E., & Figueroa, A. (2025). Impact of L-Citrulline Supplementation and HIIT on Lipid Profile, Arterial Stiffness, and Fat Mass in Obese Adolescents with Metabolic-Dysfunction-Associated Fatty Liver Disease: A Randomized Clinical Trial. Nutrients, 17(3), 402. https://doi.org/10.3390/nu17030402







