Nutritional Issues in Children with Congenital Heart Diseases (CHDs)
Abstract
1. Introduction
2. Methods
3. Pathophysiology of Nutritional Disorders in Paediatric CHDs
3.1. Increased Metabolic Demands
3.2. Reduced Nutritional Intake
3.3. Malabsorption and Inefficient Nutrient Utilization
3.4. Clinical Implications
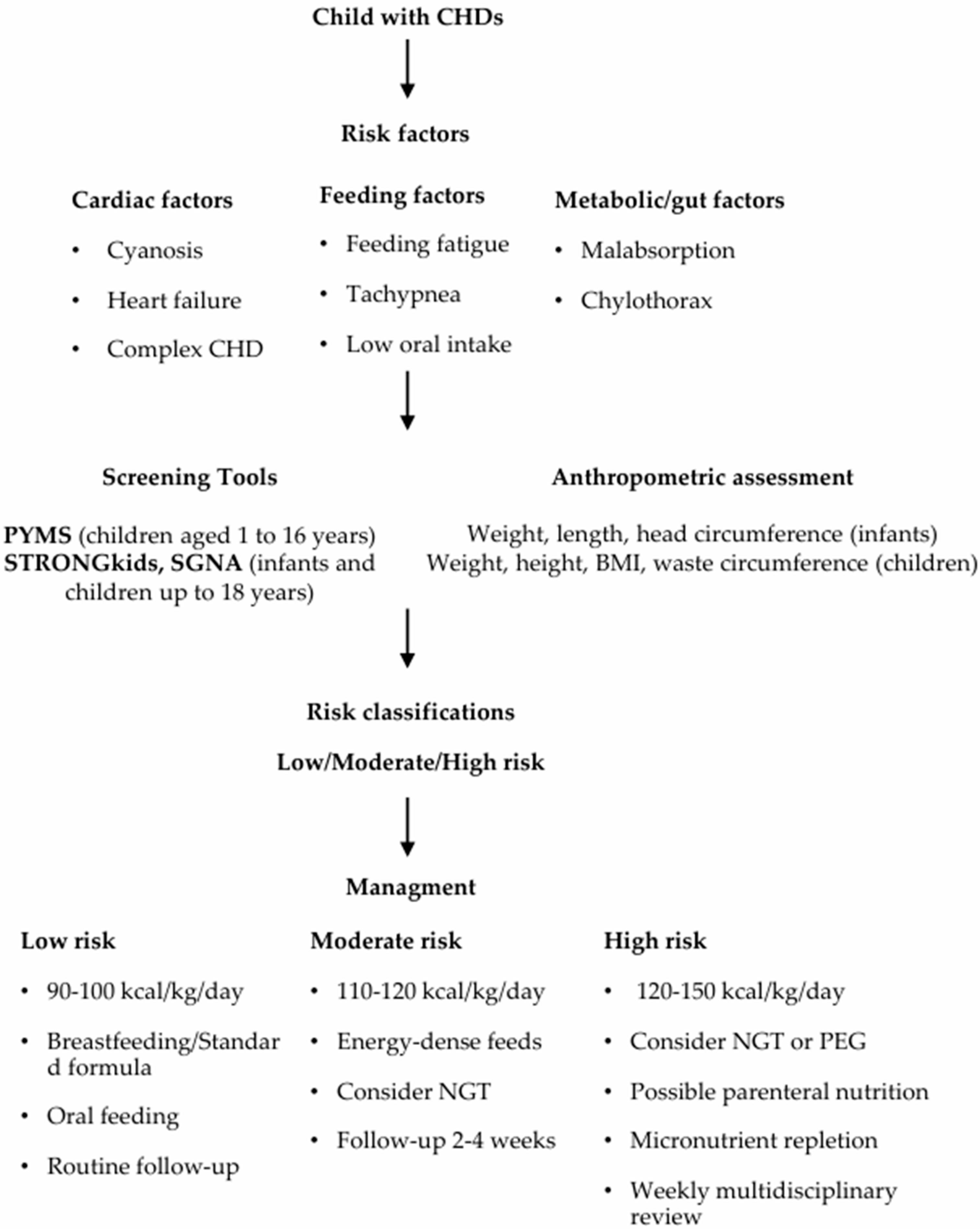
4. Nutritional Screening and Assessment Tools in Children with CHDs
4.1. Timing and Screening Tools
4.2. Anthropometric Assessment
4.3. Clinical Evaluation
4.4. Laboratory Investigations and Micronutrient Assessment
5. Nutritional Requirements and Intervention Strategies
5.1. Energy and Protein Requirements
5.2. Feeding Modalities and Strategies
5.3. Fluid and Electrolyte Management
5.4. Micronutrient Deficiencies and Supplementation
6. Special Considerations
6.1. Cyanotic Versus Non-Cyanotic CHDs
6.2. Single-Ventricle and Fontan Physiology
7. Monitoring and Follow-Up
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CHDs | Congenital heart diseases |
| PYMS | Paediatric Yorkhill Malnutrition Score |
| STRONGkids | Screening Tool for Risk on Nutritional status and Growth in Kids |
| STAMP | Screening Tool for the Assessment of Malnutrition in Pediatrics |
| PNSS | Paediatric Nutrition Screening Tool |
| SGNA | Subjective Global Nutritional Assessment |
| WHO | World Health Organization |
| WAZ | Weight-for-age Z-score |
| WLZ/WHZ | Weight-for-length Z-score |
| MUAC | Mid-upper arm circumference |
| REE | Resting energy expenditure |
| NGT | Nasogastric tube |
| PEG | Percutaneous endoscopic gastrostomy |
| PLE | Protein-losing enteropathy |
References
- Mills, K.I.; Kim, J.H.; Fogg, K.; Goldshtrom, N.; Graham, E.M.; Kataria-Hale, J.; Osborne, S.W.; Figueroa, M. Nutritional Considerations for the Neonate with Congenital Heart Disease. Pediatrics 2022, 150, e2022056415G. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Van der Linde, D.; Konings, E.E.; Slager, M.A.; Witsenburg, M.; Helbing, W.A.; Takkenberg, J.J.M.; Roos-Hesselink, J.W. Birth prevalence of congenital heart disease worldwide: A systematic review and meta-analysis. J. Am. Coll. Cardiol. 2011, 58, 2241–2247. [Google Scholar] [CrossRef] [PubMed]
- Wernovsky, G.; Licht, D.J. Neurodevelopmental outcomes in children with congenital heart disease: What can we impact? Pediatr. Crit. Care Med. 2016, 17, S232–S242. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Larson-Nath, C.; Goday, P. Malnutrition in children with chronic disease. Nutr. Clin. Pract. 2019, 34, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Diao, J.; Chen, L.; Wei, J.; Shu, J.; Li, Y.; Li, J.; Zhang, S.; Wang, T.; Qin, J. Prevalence of malnutrition in children with congenital heart disease: A systematic review and meta-analysis. J. Pediatr. 2022, 242, 39–47.e4. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Xu, B.; Zhu, C.; Pu, K.; Bian, L. Risk factors of malnutrition in children with congenital heart disease: A meta-analysis. Front. Pediatr. 2024, 12, 1258725. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mignot, M.; Huguet, H.; Cambonie, G.; Guillaumont, S.; Vincenti, M.; Blanc, J.; Ovaert, C.; Picot, M.-C.; Karsenty, C.; Amedro, P.; et al. Risk factors for early occurrence of malnutrition in infants with severe congenital heart disease. Eur. J. Pediatr. 2023, 182, 1261–1269. [Google Scholar] [CrossRef] [PubMed]
- Norman, V.; Zühlke, L.; Murray, K.; Morrow, B. Prevalence of feeding and swallowing disorders in congenital heart disease: A scoping review. Front. Pediatr. 2022, 10, 843023. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vaisman, N.; Leigh, T.; Voet, H.; Westerterp, K.; Abraham, M.; Duchan, R. Malabsorption in infants with congenital heart disease under diuretic treatment. Pediatr. Res. 1994, 36, 545–549. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Centeno-Malfaz, F.; Moráis-López, A.; Caro-Barri, A.; Peña-Quintana, L.; Gil-Villanueva, N.; Redecillas-Ferreiro, S.; Marcos-Alonso, S.; Ros-Arnal, I.; Tejero, M.Á.; Sánchez, C.S.; et al. Nutrition in congenital heart disease: Consensus document. An. Pediatr. 2023, 98, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Kołodziej, M.; Skulimowska, J. A systematic review of clinical practice guidelines on the management of malnutrition in children with congenital heart disease. Nutrients 2024, 16, 2778. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Luca, A.C.; Miron, I.C.; Mîndru, D.E.; Curpăn, A.Ș.; Stan, R.C.; Țarcă, E.; Luca, F.-A.; Pădureț, A.I. Optimal nutrition parameters for neonates and infants with congenital heart disease. Nutrients 2022, 14, 1671. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Itkin, M.; Piccoli, D.A.; Nadolski, G.; Rychik, J.; DeWitt, A.; Pinto, E.; Rome, J.; Dori, Y. Protein-losing enteropathy in patients with congenital heart disease. J. Am. Coll. Cardiol. 2017, 69, 2929–2937. [Google Scholar] [CrossRef] [PubMed]
- Mo, X.; Cai, W.; Qi, J.; Xu, Z.; Wang, Y.; Yan, W.; Li, S.; Dong, N.; Chen, X.; Liu, J.; et al. Expert consensus on nutritional support for children with congenital heart disease (2023 edition). Congenit. Heart Dis. 2023, 18, 571–593. [Google Scholar] [CrossRef]
- Daymont, C.; Neal, A.; Prosnitz, A.; Cohen, M.S. Growth in children with congenital heart disease. Pediatrics 2013, 131, e236–e242. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.B.; Beekman, R.H.; Border, W.L.; Kalkwarf, H.J.; Khoury, P.R.; Uzark, K.; Eghtesady, P.; Marino, B.S. Lower weight-for-age z-score adversely affects hospital length of stay after the bidirectional Glenn procedure in 100 infants with a single ventricle. J. Thorac. Cardiovasc. Surg. 2009, 138, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.B.; Beekman, R.H., 3rd; Eghtesady, P.; Kalkwarf, H.J.; Uzark, K.; Kehl, J.E.; Marino, B.S. Predictors of poor weight gain in infants with a single ventricle. J. Pediatr. 2010, 157, 407–413.e1. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.B.; Kalkwarf, H.J.; Kehl, J.E.; Eghtesady, P.; Marino, B.S. Low weight-for-age z-score and infection risk after the Fontan procedure. Ann. Thorac. Surg. 2011, 91, 1460–1466. [Google Scholar] [CrossRef] [PubMed]
- Ratanachu-Ek, S.; Pongdara, A. Nutritional status of pediatric patients with congenital heart disease: Pre- and post cardiac surgery. J. Med. Assoc. Thai. 2011, 94, S133–S137. [Google Scholar] [PubMed]
- Varan, B.; Tokel, K.; Yilmaz, G. Malnutrition and growth failure in cyanotic and acyanotic congenital heart disease with and without pulmonary hypertension. Arch. Dis. Child. 1999, 81, 49–52. [Google Scholar] [CrossRef] [PubMed]
- Katsagoni, C.N.; Cheirakaki, O.; Hatzoglou, A.; Zerva, O.; Koulieri, A.; Loizou, K.; Vasileiadi, E.; Toilou, M.; Poulia, K.-A.; Kontogianni, M.D. Malnutrition in Hospitalised Children-An Evaluation of the Efficacy of Two Nutritional Screening Tools. Nutrients 2021, 13, 1279. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Klanjsek, P.; Pajnkihar, M.; Marcun Varda, N.; Brzan, P.P. Screening and assessment tools for early detection of malnutrition in hospitalised children: A systematic review of validation studies. BMJ Open 2019, 9, e025444. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jimenez, E.Y.; Lamers-Johnson, E.; Long, J.M.; Woodcock, L.; Bliss, C.; Steiber, A.L. Predictive Validity of the Academy of Nutrition and Dietetics/American Society for Parental Nutrition Indicators to Diagnose Malnutrition and the Screening Tool for Risk on Nutritional Status and Growth among Hospitalized Children Relative to Medical Outcomes. J. Pediatr. 2025, 276, 114288. [Google Scholar] [CrossRef] [PubMed]
- Carter, L.; Hulst, J.M.; Afzal, N.; Jeejeebhoy, K.; Brunet-Wood, K. Update to the pediatric Subjective Global Nutritional Assessment (SGNA). Nutr. Clin. Pract. 2022, 37, 1448–1457. [Google Scholar] [CrossRef] [PubMed]
- Cameron, J.W.; Rosenthal, A.; Olson, A.D. Malnutrition in hospitalized children with congenital heart disease. Arch. Pediatr. Adolesc. Med. 1995, 149, 1098–1102. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Wang, L.; Huang, R.; Sun, C.; Bao, N.; Xu, Z. Risk factors of malnutrition in Chinese children with congenital heart defect. BMC Pediatr. 2020, 20, 213. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kelleher, D.K.; Laussen, P.; Teixeira-Pinto, A.; Duggan, C. Growth and correlates of nutritional status among infants with hypoplastic left heart syndrome (HLHS) after stage 1 Norwood procedure. Nutrition 2006, 22, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Villar, J.; Cheikh Ismail, L.; Victora, C.G.; Ohuma, E.O.; Bertino, E.; Altman, D.G.; Lambert, A.; Papageorghiou, A.T.; Carvalho, M.; Jaffer, Y.A.; et al. International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH-21st). International standards for newborn weight, length, and head circumference by gestational age and sex: The Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet 2014, 384, 857–868. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, I.M.; Logan, R.W.; Pollock, J.C.; Jamieson, M.P. Nutritional status of children with congenital heart disease. Br. Heart J. 1995, 73, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Boullata, J.I.; Carrera, A.L.; Harvey, L.; Escuro, A.A.; Hudson, L.; Mays, A.; McGinnis, C.; Wessel, J.J.; Bajpai, S.; Beebe, M.L.; et al. ASPEN Safe Practices for Enteral Nutrition Therapy Task Force, American Society for Parenteral and Enteral Nutrition. ASPEN Safe Practices for Enteral Nutrition Therapy. JPEN J. Parenter. Enter. Nutr. 2017, 41, 15–103. [Google Scholar] [CrossRef] [PubMed]
- Okoromah, C.A.N.; Ekure, E.N.; Lesi, F.E.A.; Okunowo, W.O.; Tijani, B.O.; Okeiyi, J.C. Prevalence, profile and predictors of malnutrition in children with congenital heart defects: A case–control observational study. Arch. Dis. Child. 2011, 96, 354–360. [Google Scholar] [CrossRef] [PubMed]
- Schuurmans, F.M.; Pulles-Heintzberger, C.F.; Gerver, W.J.; Kester, A.D.; Forget, P.P. Long-term growth of children with congenital heart disease: A retrospective study. Acta Paediatr. 1998, 87, 1250–1255. [Google Scholar] [CrossRef] [PubMed]
- Radman, M.; Mack, R.; Barnoya, J.; Castañeda, A.; Rosales, M.; Azakie, A.; Mehta, N.; Keller, R.; Datar, S.; Oishi, P.; et al. The effect of preoperative nutritional status on postoperative outcomes in children undergoing surgery for congenital heart defects in San Francisco (UCSF) and Guatemala City (UNICAR). J. Thorac. Cardiovasc. Surg. 2014, 147, 442–450. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nydegger, A.; Bines, J.E. Energy metabolism in infants with congenital heart disease. Nutrition 2006, 22, 697–704, Erratum in Nutrition 2006, 22, 1073–1074. [Google Scholar] [CrossRef] [PubMed]
- Eskedal, L.; Hagemo, P.; Eskild, A.; Aamodt, G.; Seiler, K.S.; Thaulow, E. A population-based study of extra-cardiac anomalies in children with congenital cardiac malformations. Cardiol. Young 2004, 14, 600–607. [Google Scholar] [CrossRef] [PubMed]
- Vaidyanathan, B.; Nair, S.B.; Sundaram, K.R.; Babu, U.K.; Shivaprakasha, K.; Rao, S.G.; Kumar, R.K. Malnutrition in children with congenital heart disease (CHD) determinants and short term impact of corrective intervention. Indian Pediatr. 2008, 45, 541–546. [Google Scholar] [PubMed]
- van der Kuip, M.; Hoos, M.B.; Forget, P.P.; Westerterp, K.R.; Gemke, R.J.; de Meer, K. Energy expenditure in infants with congenital heart disease, including a meta-analysis. Acta Paediatr. 2003, 92, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Indramohan, G.; Pedigo, T.P.; Rostoker, N.; Cambare, M.; Grogan, T.; Federman, M.D. Identification of Risk Factors for Poor Feeding in Infants with Congenital Heart Disease and a Novel Approach to Improve Oral Feeding. J. Pediatr. Nurs. 2017, 35, 149–154. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Medoff-Cooper, B.; Irving, S.Y.; Hanlon, A.L.; Golfenshtein, N.; Radcliffe, J.; Stallings, V.A.; Marino, B.S.; Ravishankar, C. The Association among Feeding Mode, Growth, and Developmental Outcomes in Infants with Complex Congenital Heart Disease at 6 and 12 Months of Age. J. Pediatr. 2016, 169, 154–159.e1. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Abqari, S.; Gupta, A.; Shahab, T.; Rabbani, M.U.; Ali, S.M.; Firdaus, U. Profile and risk factors for congenital heart defects: A study in a tertiary care hospital. Ann. Pediatr. Cardiol. 2016, 9, 216–221. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Marino, B.S.; Lipkin, P.H.; Newburger, J.W.; Peacock, G.; Gerdes, M.; Gaynor, J.W.; Mussatto, K.A.; Uzark, K.; Goldberg, C.S.; Johnson, W.H.; et al. Neurodevelopmental outcomes in children with congenital heart disease: Evaluation and management: A scientific statement from the American Heart Association. Circulation 2012, 126, 1143–1172. [Google Scholar] [CrossRef] [PubMed]
- Marino, B.S.; Shera, D.; Wernovsky, G.; Tomlinson, R.S.; Aguirre, A.; Gallagher, M.; Lee, A.; Cho, C.J.; Stern, W.; Davis, L.; et al. The development of the pediatric cardiac quality of life inventory: A quality of life measure for children and adolescents with heart disease. Qual. Life Res. 2008, 17, 613–626. [Google Scholar] [CrossRef] [PubMed]
- Mitting, R.; Marino, L.; Macrae, D.; Shastri, N.; Meyer, R.; Pathan, N. Nutritional status and clinical outcome in postterm neonates undergoing surgery for congenital heart disease. Pediatr Crit Care Med. 2015, 16, 448–452. [Google Scholar] [CrossRef] [PubMed]
- Toole, B.J.; Toole, L.E.; Kyle, U.G.; Cabrera, A.G.; Orellana, R.A.; Coss-Bu, J.A. Perioperative nutritional support and malnutrition in infants and children with congenital heart disease. Congenit. Heart Dis. 2014, 9, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Kyle, U.G.; Kossovsky, M.P.; Karsegard, V.L.; Pichard, C. Comparison of tools for nutritional assessment and screening at hospital admission: A population study. Clin. Nutr. 2006, 25, 409–417. [Google Scholar] [CrossRef] [PubMed]
- Becker, P.; Carney, L.N.; Corkins, M.R.; Monczka, J.; Smith, E.; Smith, S.E.; Spear, B.A.; White, J.V. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: Indicators recommended for the identification and documentation of pediatric malnutrition (undernutrition). Nutr. Clin. Pract. 2015, 30, 147–161. [Google Scholar] [CrossRef] [PubMed]
- Mehta, N.M.; Skillman, H.E.; Irving, S.Y.; Coss-Bu, J.A.; Vermilyea, S.; Farrington, E.A.; McKeever, L.; Hall, A.M.; Goday, P.S.; Braunschweig, C. Guidelines for the provision and assessment of nutrition support therapy in the pediatric critically ill patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition. JPEN J. Parenter. Enter. Nutr. 2017, 41, 706–742. [Google Scholar] [CrossRef] [PubMed]
- Elgersma, K.M.; Wolfson, J.; Fulkerson, J.A.; Georgieff, M.K.; Looman, W.S.; Spatz, D.L.; Shah, K.M.; Uzark, K.; McKechnie, A.C. Human milk feeding and direct breastfeeding improve outcomes for infants with single ventricle congenital heart disease: Propensity score–matched analysis of the NPC-QIC registry. J. Am. Heart Assoc. 2023, 12, e030756. [Google Scholar] [CrossRef] [PubMed]
- Russel, S.M.; Lessen, R.; Rovner, A.J.; Delahanty, M.; Hollowell, C.M.; Trabulsi, J.C.P. Breastfeeding characteristics and duration of feeding human milk in infants with congenital heart disease. J. Perinat. Neonatal Nurs. 2024, 38, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.M.; Qian, S.Y.; Lu, G.P.; Xu, F.; Wang, Y.; Liu, C.F.; Ren, X.X.; Zhang, Y.C.; Gao, H.M.; Zhou, T.; et al. Chinese guidelines for the assessment and provision of nutrition support therapy in critically ill children. World J. Pediatr. 2018, 14, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Kronborg, J.R.; Lindhardt, R.B.; Vejlstrup, N.; Holst, L.M.; Juul, K.; Smerup, M.H.; Gjedsted, J.; Ravn, H.B. Impact of acute kidney injury and dysnatremia on length of stay in infants after cardiac surgery. Pediatr. Nephrol. 2025, 40, 3281–3291. [Google Scholar] [CrossRef] [PubMed]
- Homan, M.; Hauser, B.; Romano, C.; Tzivinikos, C.; Torroni, F.; Gottrand, F.; Hojsak, I.; Dall’Oglio, L.; Thomson, M.; Bontems, P.; et al. Percutaneous Endoscopic Gastrostomy in Children: An Update to the ESPGHAN Position Paper. J. Pediatr. Gastroenterol. Nutr. 2021, 73, 415–426. [Google Scholar] [CrossRef] [PubMed]
- Sochet, A.A.; Grindy, A.K.; Son, S.; Barrie, E.K.; Hickok, R.L.; Nakagawa, T.A.; Wilsey, M.J. Percutaneous Endoscopic Gastrostomy After Cardiothoracic Surgery in Children Less Than 2 Months Old: An Assessment of Long-Term Malnutrition Status and Gastrostomy Outcomes. Pediatr. Crit. Care Med. 2020, 21, 50–58. [Google Scholar] [CrossRef] [PubMed]
- McKay, K.G.; Huang, E.Y.; Robinson, J.R. Enteral Access in Pediatric Cardiac Patients: A Survey of Pediatric Surgeons at the Top 50 Cardiac Hospitals. J. Pediatr. Surg. 2025, 60, 162513. [Google Scholar] [CrossRef] [PubMed]
- Avasarala, V.; Aitharaju, V.; Encisco, E.M.; Rymeski, B.; Ponsky, T.A.; Huntington, J.T. Enteral access and reflux management in neonates with severe univentricular congenital heart disease: Literature review and proposed algorithm. Eur. J. Pediatr. 2023, 182, 3375–3383. [Google Scholar] [CrossRef] [PubMed]
- Zook, N.; Schultz, L.; Rizzuto, S.; Aufdermauer, A.; Hollander, A.M.; Almond, C.S.; Hollander, S.A. Supplemental nutrition, feeding disorders, and renourishment in pediatric heart failure through transplantation. Pediatr. Transplant. 2023, 27, e14601. [Google Scholar] [CrossRef] [PubMed]
- Teng, C.; Shu, D.; Faerber, J.A.; Goldenring, J.; Butto, A.; Tam, V.; Olsen, R.; Glatz, A.C.; Cohen, M.S. Factors Associated with Growth in a Cohort of Children with Complex Biventricular Congenital Heart Disease. J. Pediatr. 2024, 267, 113901. [Google Scholar] [CrossRef] [PubMed]
- Ricci, Z.; Iacoella, C.; Cogo, P. Fluid management in critically ill pediatric patients with congenital heart disease. Minerva Pediatr. 2011, 63, 399–410. [Google Scholar] [PubMed]
- Ossei, I.; Buabeng, K.O.; Ossei, P.P.S.; Nguah, S.B.; Ayibor, W.G.; Anto, B.P.; Eric, A.-D.; Duwiejua, M. Iron-deficiency anaemia in children with congenital heart diseases at a teaching hospital in Ghana. Heliyon 2020, 6, e03408. [Google Scholar] [CrossRef] [PubMed]
- Kumsa, H.; Woldesenbet, R.; Mulugeta, F.; Murugan, R.; Moges, T. Anemia in children with congenital heart disease: A finding from low-resource setting hospitals. Int. J. Pediatr. 2024, 2024, 8095150. [Google Scholar] [CrossRef] [PubMed]
- Itiola, A.Y.; Animasahun, B.A.; Njokanma, O.F. Serum iron status of children with cyanotic congenital heart disease in Lagos, Nigeria. Sultan Qaboos Univ. Med. J. 2019, 19, e345–e351. [Google Scholar] [CrossRef] [PubMed]
- Mires, S.; Caputo, M.; Overton, T.; Skerritt, C. Maternal micronutrient deficiency and congenital heart disease risk: A systematic review of observational studies. Birth Defects Res. 2022, 114, 1079–1091. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Dong, S.; Deng, Y.; Jiang, C.; Kong, Y.; Tang, L.; Wang, Y.; Bei, F.; Hong, H. Preoperative vitamin D deficiency is associated with higher vasoactive–inotropic scores following pediatric cardiac surgery in Chinese children. Front. Pediatr. 2021, 9, 671289. [Google Scholar] [CrossRef] [PubMed]
- Dohain, A.M.; Almogati, J.; Al-Radi, O.O.; Elassal, A.A.; Zaher, Z.F.; Fatani, T.H.; Abdulgawad, A.; Abdelmohsen, G. Serum vitamin D status following pediatric cardiac surgery and association with clinical outcome. Eur. J. Pediatr. 2020, 179, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Trabulsi, J.C.; Irving, S.Y.; Papas, M.A.; Hollowell, C.; Ravishankar, C.; Marino, B.S.; Medoff-Cooper, B.; Schall, J.I.; Stallings, V.A. Total energy expenditure of infants with congenital heart disease who have undergone surgical intervention. Pediatr. Cardiol. 2015, 36, 1670–1679. [Google Scholar] [CrossRef] [PubMed]
- Modi, P.; Suleiman, M.S.; Reeves, B.C.; Pawade, A.; Parry, A.J.; Angelini, G.D.; Caputo, M. Basal metabolic state of hearts of patients with congenital heart disease: The effects of cyanosis, age, and pathology. Ann. Thorac. Surg. 2004, 78, 1710–1716. [Google Scholar] [CrossRef] [PubMed]
- Dong, S.; Wu, L.; Duan, Y.; Cui, H.; Chen, K.; Chen, X.; Sun, Y.; Du, C.; Ren, J.; Shu, S.; et al. Metabolic profile of heart tissue in cyanotic congenital heart disease. Am. J. Transl. Res. 2021, 13, 4224–4232. [Google Scholar] [PubMed]
- Blanche, C.; Alonso-Gonzalez, R.; Uribarri, A.; Kempny, A.; Swan, L.; Price, L.; Wort, S.J.; Beghetti, M.; Dimopoulos, K. Use of intravenous iron in cyanotic patients with congenital heart disease and/or pulmonary hypertension. Int. J. Cardiol. 2018, 267, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.N.; Driscoll, D.J.; O’Leary, P.W. Protein-losing enteropathy and the Fontan operation. Nutr. Clin. Pract. 2012, 27, 375–384. [Google Scholar] [CrossRef] [PubMed]
- Alsaied, T.; Lubert, A.M.; Goldberg, D.J.; Schumacher, K.; Rathod, R.; Katz, D.A.; Opotowsky, A.R.; Jenkins, M.; Smith, C.; Rychik, J.; et al. Protein-losing enteropathy after the Fontan operation. Int. J. Cardiol. Congenit. Heart Dis. 2022, 7, 100338. [Google Scholar] [CrossRef] [PubMed]
- Viswanathan, S.; Ong, K.J.F.; Kakavand, B. Prevalence and Risk Factors for Tube-Feeding at Discharge in Infants following Early Congenital Heart Disease Surgery: A Single-Center Cohort Study. Am. J. Perinatol. 2024, 41, e2832–e2841. [Google Scholar] [CrossRef] [PubMed]
- Pettigrew, J.; Tzannes, G.; Swift, L.; Docking, K.; Osland, K.; Cheng, A.T. Surgically Acquired Vocal Cord Palsy in Infants and Children with Congenital Heart Disease (CHD): Description of Feeding Outcomes. Dysphagia 2022, 37, 1288–1304. [Google Scholar] [CrossRef] [PubMed]
- Hofner, G.; Behrens, R.; Koch, A.; Singer, H.; Hofbeck, M. Enteral nutritional support by percutaneous endoscopic gastrostomy in children with congenital heart disease. Pediatr. Cardiol. 2000, 21, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, R.; Irvine, T.; Dalzell, M. Indications for percutaneous endoscopic gastrostomy and procedure-related outcome. J. Pediatr. Gastroenterol. Nutr. 2009, 49, 584–588. [Google Scholar] [CrossRef] [PubMed]
- Slicker, J.; Hehir, D.A.; Horsley, M.; Monczka, J.; Stern, K.W.; Roman, B.; Ocampo, E.C.; Flanagan, L.; Keenan, E.; Lambert, L.M.; et al. Feeding Work Group of the National Pediatric Cardiology Quality Improvement Collaborative. Nutrition algorithms for infants with hypoplastic left heart syndrome; birth through the first interstage period. Congenit. Heart Dis. 2013, 8, 89–102. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hahn, S.; Willette, S.; Lay, A.; Schroeder, J.; Hazkani, I.; Valika, T.; Ghadersohi, S. Prevalence, Clinical Factors and Impact of Dysphagia After Cardiac Surgery for Congenital Heart Disease. Pediatr. Cardiol. 2025; ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Su, Z.; Zhang, Y.; Cai, X.; Li, Q.; Gu, H.; Luan, Y.; He, Y.; Li, S.; Chen, J.; Zhang, H. Improving long-term care and outcomes of congenital heart disease: Fulfilling the promise of a healthy life. Lancet Child Adolesc. Health 2023, 7, 502–518. [Google Scholar] [CrossRef] [PubMed]
- Ortinau, C.M.; Smyser, C.D.; Arthur, L.; Gordon, E.E.; Heydarian, H.C.; Wolovits, J.; Nedrelow, J.; Marino, B.S.; Levy, V.Y. Optimizing Neurodevelopmental Outcomes in Neonates with Congenital Heart Disease. Pediatrics 2022, 150, e2022056415L. [Google Scholar] [CrossRef] [PubMed]
- van Genuchten, W.J.; Averesch, H.; van Dieren, Q.M.; Bonnet, D.; Odermarsky, M.; Beghetti, M.; Roos-Hesselink, J.; Reinhardt, Z.; Male, C.; Naumburg, E.; et al. Clinical impact of circulating biomarkers in prediction of adverse cardiac events in patients with congenital heart disease. A systematic review. Int. J. Cardiol. 2025, 421, 132723. [Google Scholar] [CrossRef] [PubMed]
| Classification | Features | Common Examples | Risk of Malnutrition in Children |
|---|---|---|---|
| Cyanotic heart diseases | Right-to-left shunt; systemic hypoxemia; clinical cyanosis | Tetralogy of Fallot; Transposition of the Great Arteries; Tricuspid Atresia; Total Anomalous Pulmonary Venous Return; Pulmonary Atresia; Hypoplastic Left Heart Syndrome | High risk, especially with pulmonary hypertension, heart failure, or delayed diagnosis |
| Non-cyanotic heart diseases | Left-to-right shunt or obstructive lesions; absence of cyanosis | Ventricular Septal Defect; Atrial Septal Defect; Patent Ductus Arteriosus; Coarctation of the Aorta; Pulmonary Stenosis; Aortic Stenosis | Moderate to high risk; increases with heart failure, pulmonary hypertension, or significant structural disease |
| Infants and Toddlers | Children | |
|---|---|---|
| Recommended anthropometric measurements |
|
|
| Z-scores |
|
|
| Growth reference charts | WHO standards for term infants; Fenton charts for preterm infants until term-equivalent age. | |
| Supplementary anthropometry | MUAC (6–59 months) Triceps/subscapular skinfolds | |
| Cardiac and metabolic factors | Cardiac physiology, heart failure, pulmonary hypertension, feeding difficulties, and increased energy expenditure influence growth interpretation. | |
| Monitoring and follow-up | Serial assessments every 3–6 months; consider feeding modality and post-surgical recovery for “catch-up” growth. | |
| Nutritional Risk | Energy Requirements | Protein Requirements | Assessment Method | Clinical Considerations |
|---|---|---|---|---|
| Low risk | 90–100 kcal/kg/day | 1.5 g/kg/day | Predictive equations (Schofield, WHO) | Mild disease; stable growth; minor hemodynamic burden |
| Moderate risk | 110–120 kcal/kg/day | 2.5 g/kg/day | Indirect calorimetry preferred; predictive equations acceptable | Moderate disease severity; some feeding difficulties; increased energy expenditure |
| High risk/severe disease | 120–150 kcal/kg/day (up to 3× basal metabolic rate in some infants) | Up to 4 g/kg/day | Indirect calorimetry strongly recommended | Hemodynamically significant lesions; malnutrition; complex CHDs; requires intensive nutritional support |
| Feeding Strategy | Indications | Essential Considerations |
|---|---|---|
| Human Milk | Stable or postoperative infants | Preferred option; optimal tolerance and immune advantages |
| Standard/Follow-up Formula | When human milk is insufficient or unavailable | Suitable for most infants; monitor growth response |
| Semi-elemental/Hydrolysed Formula | Malabsorption or gastrointestinal compromise | Enhanced digestibility; supports nutrient absorption |
| High-Density Feeds | Fluid restriction; elevated caloric needs | ≥1 kcal/mL; monitor hydration and tolerance closely |
| Oral + NGT Feeding | Feeding fatigue, respiratory burden, inadequate weight gain | Oral intake supplemented by nocturnal NGT feeding |
| NGT | Temporary enteral support | Short-term solution; may cause irritation if prolonged |
| PEG | Persistent feeding difficulty or growth failure | Long-term stable access; supports growth; minor complications frequent |
| PN | Severe malabsorption or hemodynamic instability | Use when enteral feeding is not feasible; requires strict monitoring |
| Indicator | Key Recommendations |
|---|---|
| Fluid intake | Total daily fluid intake generally ≤165 mL/kg/day; careful titration required in neonates, infants, and post-operative patients to avoid overload or underperfusion. |
| Sodium intake | Limit to 2.2–3 mEq/kg/day to prevent fluid overload and worsening heart failure. |
| Monitoring | Daily weight, fluid balance, and electrolytes; adjust therapy based on hemodynamic status and renal function. |
| Electrolyte disturbances | Dysnatremias common post-cardiac surgery: hypernatremia linked to transfusions and low free water; hyponatremia associated with positive fluid balance and hypotonic fluids. |
| Fluid type considerations | Prefer isotonic solutions; individualized adjustments based on ADH secretion, cardiac output, and clinical status. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vazzana, G.F.; Romano, A.; Romano, C. Nutritional Issues in Children with Congenital Heart Diseases (CHDs). Nutrients 2025, 17, 3936. https://doi.org/10.3390/nu17243936
Vazzana GF, Romano A, Romano C. Nutritional Issues in Children with Congenital Heart Diseases (CHDs). Nutrients. 2025; 17(24):3936. https://doi.org/10.3390/nu17243936
Chicago/Turabian StyleVazzana, Giovanna Fernanda, Alessia Romano, and Claudio Romano. 2025. "Nutritional Issues in Children with Congenital Heart Diseases (CHDs)" Nutrients 17, no. 24: 3936. https://doi.org/10.3390/nu17243936
APA StyleVazzana, G. F., Romano, A., & Romano, C. (2025). Nutritional Issues in Children with Congenital Heart Diseases (CHDs). Nutrients, 17(24), 3936. https://doi.org/10.3390/nu17243936







