Effects of a Digitally-Enabled Healthy Eating and Physical Activity Diabetes Prevention Peer Support Program on Weight over 6-Months
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Recruitment
2.3. Peer Support Program
2.4. Peer Support Facilitation
2.5. Data Collection
2.6. Statistical Analysis
3. Results
3.1. Peer Support Facilitators
3.2. Participant Demographics
3.3. Readiness to Change
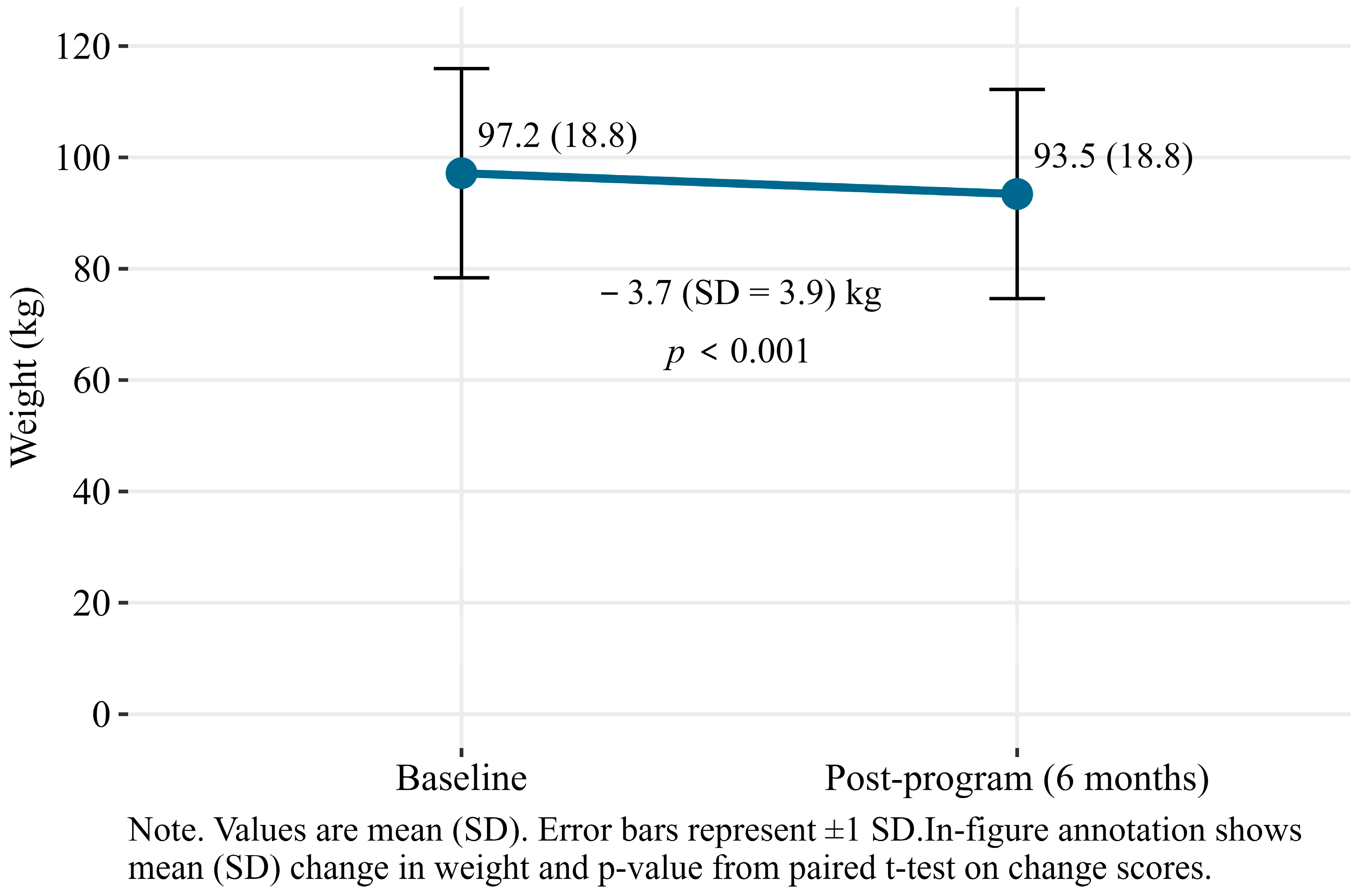
3.4. Change in Weight
3.5. Platform Activity
3.6. Program Feedback
3.6.1. Challenges Identified by the Participants and PSFs
3.6.2. Challenges Identified by the Research Team
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| T2D | Type 2 Diabetes |
| PSF | Peer support facilitator |
| GP | General practitioner |
| IGT | Impaired glucose tolerance |
| IFG | Impaired fasting glucose |
| AUSDRISK | Australian Diabetes Risk Assessment |
References
- International Diabetes Federation. IDF Diabetes Atlas, 11th ed.; International Diabetes Federation: Brussels, Belgium, 2025; Available online: https://diabetesatlas.org (accessed on 31 July 2025).
- Cho, N.H.; Shaw, J.E.; Karuranga, S.; Huang, Y.; da Rocha Fernandes, J.D.; Ohlrogge, A.W.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Magliano, D.J.; Shaw, J.; Shortreed, S.M.; Nusselder, W.J.; Liew, D.; Barr, E.L.; Zimmet, P.Z.; Peeters, A. Lifetime risk and projected population prevalence of diabetes. Diabetologia 2008, 51, 2179–2186. [Google Scholar] [CrossRef][Green Version]
- Lee, C.M.Y.; Colagiuri, R.; Magliano, D.J.; Cameron, A.J.; Shaw, J.; Zimmet, P.; Colagiuri, S. The cost of diabetes in adults in Australia. Diabetes Res. Clin. Pract. 2013, 99, 385–390. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Diabetes: Australian Facts; Australian Institute of Health and Welfare: Canberra, Australia, 2024. [Google Scholar]
- Li, M.; Fan, Y.; Zhang, X.; Hou, W.; Tang, Z. Fruit and vegetable intake and risk of type 2 diabetes mellitus: Meta-analysis of prospective cohort studies. BMJ Open 2014, 4, e005497. [Google Scholar] [CrossRef]
- Smith, A.D.; Crippa, A.; Woodcock, J.; Brage, S. Physical activity and incident type 2 diabetes mellitus: A systematic review and dose-response meta-analysis of prospective cohort studies. Diabetologia 2016, 59, 2527–2545. [Google Scholar] [CrossRef] [PubMed]
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.M.; Walker, E.A.; Nathan, D.M.; Watson, P.G.; Mendoza, J.T.; Smith, K.A.; et al. Diabetes Prevention Program Research Group. Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [CrossRef] [PubMed]
- Johnson, G.; Martin, J.E.; Timoshanko, A. Preventing type 2 diabetes: Scaling up to create a prevention system. Med. J. Aust. 2015, 202, 24. [Google Scholar] [CrossRef]
- Hamman, R.F.; Wing, R.R.; Edelstein, S.L.; Lachin, J.M.; Bray, G.A.; Delahanty, L.; Hoskin, M.; Kriska, A.M.; Mayer-Davis, E.J.; Pi-Sunyer, X.; et al. Effect of Weight Loss With Lifestyle Intervention on Risk of Diabetes. Diabetes Care 2006, 29, 2102–2107. [Google Scholar] [CrossRef]
- Wing, R.R.; Lang, W.; Wadden, T.A.; Safford, M.; Knowler, W.C.; Bertoni, A.G.; Hill, J.O.; Brancati, F.L.; Peters, A.; Wagenknecht, L.; et al. Benefits of Modest Weight Loss in Improving Cardiovascular Risk Factors in Overweight and Obese Individuals With Type 2 Diabetes. Diabetes Care 2011, 34, 1481–1486. [Google Scholar] [CrossRef]
- Uusitupa, M.; Lindi, V.; Louheranta, A.; Salopuro, T.; Lindström, J.; Tuomilehto, J.; Finnish Diabetes Prevention Study Group. Long-term improvement in insulin sensitivity by changing lifestyles of people with impaired glucose tolerance: 4-year results from the Finnish Diabetes Prevention Study. Diabetes 2003, 52, 2532–2538. [Google Scholar] [CrossRef]
- Ndwiga, D.W.; MacMillan, F.; McBride, K.A.; Thompson, R.; Reath, J.; Alofivae-Doorbinia, O.; Abbott, P.; McCafferty, C.; Aghajani, M.; Rush, E. Outcomes of a church-based lifestyle intervention among Australian Samoans in Sydney–Le Taeao Afua diabetes prevention program. Diabetes Res. Clin. Pract. 2020, 160, 108000. [Google Scholar] [CrossRef] [PubMed]
- Werner, J.J.; Ufholz, K.; Yamajala, P. Recent Findings on the Effectiveness of Peer Support for Patients with Type 2 Diabetes. Curr. Cardiovasc. Risk Rep. 2024, 18, 65–79. [Google Scholar] [CrossRef]
- Pollard, C.M.; Landrigan, T.J.; Ellies, P.L.; Kerr, D.A.; Underwood Lester, M.L.; Goodchild, S.E. Geographic factors as determinants of food security: A Western Australian food pricing and quality study. Asia Pac. J. Clin. Nutr. 2014, 23, 703–713. [Google Scholar] [PubMed]
- Eley, R.; Bush, R.; Brown, W. Opportunities, barriers, and constraints to physical activity in rural Queensland, Australia. J. Phys. Act. Health 2014, 11, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Sushames, A.; Engelberg, T.; Gebel, K. Perceived barriers and enablers to participation in a community-tailored physical activity program with Indigenous Australians in a regional and rural setting: A qualitative study. Int. J. Equity Health 2017, 16, 172. [Google Scholar] [CrossRef]
- Kim, C.; MacMillan, F.; Osuagwu, U.L.; Simmons, D. Peer support facilitator and peer perspectives of an inner-regional Australian diabetes prevention and self-management peer support program. Health Soc. Care Community 2022, 30, e4051–e4064. [Google Scholar] [CrossRef]
- Kerr, D.; Ahn, D.; Waki, K.; Wang, J.; Breznen, B.; Klonoff, D.C. Digital Interventions for Self-Management of Type 2 Diabetes Mellitus: Systematic Literature Review and Meta-Analysis. J. Med. Internet Res. 2024, 26, e55757. [Google Scholar] [CrossRef]
- Golovaty, I.; Wadhwa, S.; Fisher, L.; Lobach, I.; Crowe, B.; Levi, R.; Seligman, H. Reach, engagement and effectiveness of in-person and online lifestyle change programs to prevent diabetes. BMC Public Health 2021, 21, 1314. [Google Scholar] [CrossRef]
- Zarora, M.R.; Jani, D.R.; MacMillan, D.F.; Pham, D.A.; Dench, M.A.; Simmons, D. Challenges to introducing integrated diabetes care to an inner-regional area in South Western Sydney, Australia. Int. J. Integr. Care 2020, 20, 6. [Google Scholar] [CrossRef]
- Zarora, R.; MacMillan, F.; Piya, M.K.; Fernandes, B.; Simmons, D. Effectiveness of a locality-based integrated diabetes care service on clinical outcomes. Intern. Med. J. 2022, 52, 975–981. [Google Scholar] [CrossRef]
- Chen, L.; Magliano, D.J.; Balkau, B.; Colagiuri, S.; Zimmet, P.Z.; Tonkin, A.M.; Mitchell, P.; Phillips, P.J.; Shaw, J.E. AUSDRISK: An Australian Type 2 Diabetes Risk Assessment Tool based on demographic, lifestyle and simple anthropometric measures. Med. J. Aust. 2010, 192, 197–202. [Google Scholar] [CrossRef]
- Coventry, P.A.; Bower, P.; Blakemore, A.; Baker, L.; Hann, M.; Paisley, A.; Renwick, C.; Li, J.; Ugajin, A.; Gibson, M. Comparison of active treatments for impaired glucose regulation: A Salford Royal Foundation Trust and Hitachi collaboration (CATFISH): Study protocol for a randomized controlled trial. Trials 2016, 17, 424. [Google Scholar] [CrossRef]
- Coventry, P.; Bower, P.; Blakemore, A.; Baker, E.; Hann, M.; Li, J.; Paisley, A.; Gibson, M. Satisfaction with a digitally-enabled telephone health coaching intervention for people with non-diabetic hyperglycaemia. NPJ Digit. Med. 2019, 2, 5. [Google Scholar] [CrossRef]
- Simmons, D.; Mesui, J. Decisional balance and stage of change in relation to weight loss, exercise and dietary fat reduction among Pacific Islands people. Asia Pac. J. Clin. Nutr. 1999, 8, 39–45. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation on Obesity, Geneva, 3–5 June 1997; World Health Organization: Geneva, Switzerland, 1998. [Google Scholar]
- R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2024; Available online: https://www.R-project.org/ (accessed on 10 November 2025).
- Berelson, B. Content Analysis in Communication Research; American Psychological Association: Washington, DC, USA, 1952. [Google Scholar]
- Donkin, L.; Christensen, H.; Naismith, S.L.; Neal, B.; Hickie, I.B.; Glozier, N. A Systematic Review of the Impact of Adherence on the Effectiveness of e-Therapies. J. Med. Internet Res. 2011, 13, e52. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.H.; Bahniwal, R.; Laupacis, A.; Leung, E.; Orr, M.S.; Straus, S.E. Systematic review and evaluation of web-accessible tools for management of diabetes and related cardiovascular risk factors by patients and healthcare providers. J. Am. Med. Inform. Assoc. Assoc. 2012, 19, 514–522. [Google Scholar] [CrossRef] [PubMed]
- Croker, J.E.; Swancutt, D.R.; Roberts, M.J.; Abel, G.A.; Roland, M.; Campbell, J.L. Factors affecting patients’ trust and confidence in GPs: Evidence from the English national GP patient survey. BMJ Open 2013, 3, e002762. [Google Scholar] [CrossRef]
- Keyworth, C.; Epton, T.; Goldthorpe, J.; Calam, R.; Armitage, C.J. Perceptions of receiving behaviour change interventions from GPs during routine consultations: A qualitative study. PLoS ONE 2020, 15, e0233399. [Google Scholar] [CrossRef]
- Tarrant, C.; Stokes, T.; Baker, R. Factors associated with patients’ trust in their general practitioner: A cross-sectional survey. Br. J. Gen. Pract. 2003, 53, 798–800. [Google Scholar]
- Gucciardi, E. A Systematic Review of Attrition from Diabetes Education Services: Strategies to Improve Attrition and Retention Research. Can. J. Diabetes 2008, 32, 53–65. [Google Scholar] [CrossRef]
- Lie, S.S.; Karlsen, B.; Oord, E.R.; Graue, M.; Oftedal, B. Dropout From an eHealth Intervention for Adults With Type 2 Diabetes: A Qualitative Study. J. Med. Internet Res. 2017, 19, e187. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Coughlin, J.F. PERSPECTIVE: Older Adults’ Adoption of Technology: An Integrated Approach to Identifying Determinants and Barriers. J. Prod. Innov. Manag. 2015, 32, 747–759. [Google Scholar] [CrossRef]
- van Genugten, L.; Dusseldorp, E.; Webb, T.L.; van Empelen, P. Which Combinations of Techniques and Modes of Delivery in Internet-Based Interventions Effectively Change Health Behavior? A Meta-Analysis. J. Med. Internet Res. 2016, 18, e155. [Google Scholar] [CrossRef] [PubMed]
- Webb, T.L.; Joseph, J.; Yardley, L.; Michie, S. Using the Internet to Promote Health Behavior Change: A Systematic Review and Meta-analysis of the Impact of Theoretical Basis, Use of Behavior Change Techniques, and Mode of Delivery on Efficacy. J. Med. Internet Res. 2010, 12, e4. [Google Scholar] [CrossRef]


| Characteristic | Responses | Mean (SD) or N (%) |
|---|---|---|
| Age | 78 | 58.5 (12.3) |
| Age group | 78 | |
| Under 35 years | 4 (5.1%) | |
| 35–44 years | 4 (5.1%) | |
| 45–54 years | 21 (26.9%) | |
| 55–64 years | 25 (32.1%) | |
| 65 years and over | 24 (30.8%) | |
| Gender (male) | 79 | 35 (44.3%) |
| Indigenous | 79 | 4 (5.1%) |
| Height (cm) | 68 | 169.6 (9.2) |
| Weight (kg) | 70 | 98.6 (19.7) |
| Waist circumference (cm) | 67 | 109.6 (15.0) |
| BMI | 68 | 34.4 (6.2) |
| BMI categories | 68 | |
| Normal (18.5–24.9) | 2 (2.9%) | |
| Overweight (25.0–29.9) | 15 (22.1%) | |
| Obese Class I (30.0–34.9) | 20 (29.4%) | |
| Obese Class II (35.0–39.9) | 16 (23.5%) | |
| Obese Class III (40 and above) | 15 (22.1%) | |
| WHO-5 Wellbeing (1–25) | 48 | 14.3 (5.0) |
| Alcohol consumption (>2 standard drinks/day) | 79 | 32 (40.5%) |
| High blood fats | 79 | 46 (58.2%) |
| Mental health issues | 79 | 31 (39.7%) |
| Highest level of education | 79 | |
| Postgraduate | 8 (10.1%) | |
| Graduate diploma or certificate | 5 (6.3%) | |
| Bachelor’s degree | 14 (17.7%) | |
| Advanced diploma or diploma | 18 (22.8%) | |
| Certificate | 14 (17.7%) | |
| Secondary school | 18 (22.8%) | |
| Other | 2 (2.5%) | |
| Occupation | 79 | |
| Manager | 12 (15.2%) | |
| Professional | 15 (19%) | |
| Technician or trade worker | 1 (1.3%) | |
| Community or personal service worker | 5 (6.3%) | |
| Clerical or administrative worker | 10 (12.7%) | |
| Sales worker | 3 (3.8%) | |
| Retired | 24 (30.4%) | |
| Other | 9 (11.4%) |
| Characteristic | N (%) |
|---|---|
| Dietary behaviour—readiness to change diet | |
| Do you drink water and other non-sugary drinks instead of sugary drinks/fruit juice? | 59 (74.7%) |
| Do you eat at least five or more servings of vegetables daily? | 31 (39.2%) |
| Do you eat at least two fruits every day? | 36 (45.6%) |
| Do you eat at least two servings of dairy foods every day? * | 50 (64.1%) |
| Do you eat at least three different protein foods every 1–2 days? | 37 (46.8%) |
| Do you eat less fat overall? | 41 (51.9%) |
| Have you reduced amount of food you eat at each sitting? | 49 (62.0%) |
| Do you eat more foods with fibre? | 48 (60.8%) |
| Do you eat less sugary foods and carbohydrates? | 46 (58.2%) |
| Do you eat at regular intervals? | 46 (58.2%) |
| Physical activity—readiness to change physical activity | |
| Are you making yourself stronger? * | 24 (30.8%) |
| Do you plan more activity in your day? | 30 (38.0%) |
| Do you plan more activity in weekends? ** | 33 (42.9%) |
| Have you increased the number of steps you take each day? * | 34 (43.6%) |
| Have you reduced the amount of time you spend sitting? * | 35 (44.9%) |
| Weight—readiness to change weight | |
| Are you trying to reach your best weight? | 54 (68.4%) |
| Within-Group Δ, Mean (SD) | Between-Group Δ (95% CI) | p Value | ||
|---|---|---|---|---|
| Logged ≥ 1 | Did Not Log | |||
| Weight (yes n = 28) | −4.0 (4.1) | −2.6 (3.2) | −1.4 (−4.6, 1.7) | 0.398 |
| Achievements (yes n = 25) | −4.5 (3.9) | −1.7 (3.3) | −2.9 (−5.6, −0.1) | 0.049 |
| Steps (yes n = 19) | −4.3 (3.7) | −3.1 (4.2) | −1.2 (−3.9, 1.6) | 0.376 |
| Weight, achievement, or steps (yes n = 29) | −4.1 (4.1) | −1.7 (2.4) | −2.5 (−5.1, 0.2) | 0.164 |
| Weight, achievement, and steps (yes n = 18) | −4.1 (3.7) | −3.4 (4.2) | −0.7 (−3.4, 2.0) | 0.604 |
| Reported Challenge |
|---|
| Participant reported challenges |
| Low engagement due to lack of access to a computer |
| Difficulty in interpreting graphs |
| The action plan did not always align with achievements |
| Scheduling conflicts with PSFs Lack of encouragement from PSFs outside of the monthly scheduled check-in calls |
| PSF-reported challenges |
| Limited confidence post-training Maintaining their confidentiality |
| Researcher-reported challenges |
| Technology (password login issues, frequent timing out and logging out) |
| Website interaction difficulties, particularly with navigation using the ‘back’ button |
| Difficulty editing or undoing self-assessment activities Infrequent logins and engagement of participants Admin-intensive management of the platform Reaching participants for data collection, specifically for weight |
| PSFs were generally helpful but did not emphasise participant weight loss enough |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
MacMillan, F.; Hliounakis, H.; Jaye, K.; Mitlehner, K.; Pitt, C.; McBride, K.A.; Osuagwu, U.L.; Simmons, D. Effects of a Digitally-Enabled Healthy Eating and Physical Activity Diabetes Prevention Peer Support Program on Weight over 6-Months. Nutrients 2025, 17, 3599. https://doi.org/10.3390/nu17223599
MacMillan F, Hliounakis H, Jaye K, Mitlehner K, Pitt C, McBride KA, Osuagwu UL, Simmons D. Effects of a Digitally-Enabled Healthy Eating and Physical Activity Diabetes Prevention Peer Support Program on Weight over 6-Months. Nutrients. 2025; 17(22):3599. https://doi.org/10.3390/nu17223599
Chicago/Turabian StyleMacMillan, Freya, Holly Hliounakis, Kayla Jaye, Kimberly Mitlehner, Chris Pitt, Kate A. McBride, Uchechukwu Levi Osuagwu, and David Simmons. 2025. "Effects of a Digitally-Enabled Healthy Eating and Physical Activity Diabetes Prevention Peer Support Program on Weight over 6-Months" Nutrients 17, no. 22: 3599. https://doi.org/10.3390/nu17223599
APA StyleMacMillan, F., Hliounakis, H., Jaye, K., Mitlehner, K., Pitt, C., McBride, K. A., Osuagwu, U. L., & Simmons, D. (2025). Effects of a Digitally-Enabled Healthy Eating and Physical Activity Diabetes Prevention Peer Support Program on Weight over 6-Months. Nutrients, 17(22), 3599. https://doi.org/10.3390/nu17223599









