Abstract
Mangiferin (MF), a natural component widely found in fruits, vegetables, and herbs, has garnered increasing attention for its potent antioxidative properties and therapeutic potential. This bioactive xanthone compound plays a crucial role in mitigating oxidative stress, which is a key factor in the pathogenesis of various diseases, including liver diseases. As a powerful natural antioxidant, MF exhibits a wide range of hepatoprotective effects, making it a promising candidate for liver disease therapy. In this review, we systematically examine the source and chemical properties, synthetic pathways, pharmacokinetic characteristics, and bioavailability enhancement strategies of MF. Furthermore, we explore its mechanisms of action in treating liver diseases, with a focus on its antioxidative properties and their role in modulating liver disease progression. Given the growing burden of liver disease and the limitations of current therapies, this review aims to promote the clinical application of MF as a therapeutic candidate, paving the way for innovative therapeutic strategies for liver diseases.
1. Introduction
Mangiferin (MF), a bioactive xanthone compound widely found in a variety of fruits, vegetables, and herbs, has attracted growing interest due to its remarkable antioxidative effects and therapeutic versatility. The core pharmacological feature of MF lies in its potent broad-spectrum antioxidant activity. By precisely regulating tissue-specific antioxidant signaling pathways, it provides comprehensive protection against damage to the kidneys, cardiovascular system, nervous system, skeletal system, reproductive metabolic system, and diabetes-related organs. For the kidneys, it offers antioxidant protection against diabetic nephropathy, renal ischemia–reperfusion injury, and hypertensive nephropathy [1,2,3]. In the cardiovascular system, it counteracts myocardial apoptosis [4]. In the nervous system, it ameliorates depression, neuronal injury, and Parkinson’s-related damage [5,6,7]. It also protects bones, alleviates oxidative damage in polycystic ovary syndrome [8,9], and supports protection of diabetes-related organs [10]. This multidimensional mechanism has been thoroughly validated. This compound plays a critical role in counteracting oxidative stress, which is a key contributor to the onset and progression of numerous diseases, including liver disorders. The unique structure of MF, characterized by its glucosyl-modified xanthone skeleton (C2-β-D-glucoside), provides the molecular basis for its ability to modulate multiple cellular pathways, offering a multi-target approach to therapeutic intervention. Recent studies have demonstrated that MF can alleviate lipotoxicity, restore redox balance, inhibit pro-fibrotic signaling, and block tumor cell cycles, positioning it as a promising pleiotropic hepatoprotective agent in the context of liver disease [11,12,13,14].
Liver disease, one of the most pressing global health concerns, continues to rise, with viral hepatitis, alcoholic liver disease (ALD), and metabolic-associated fatty liver disease (MAFLD) leading to millions of deaths annually. Despite significant advances in the understanding of liver pathology, current treatments remain limited, with antiviral drugs, immunomodulatory therapies, and the development of drugs for metabolic liver diseases still facing challenges. ALD, for example, lacks approved therapies, and although Resmetirom will soon be approved for MAFLD, the overall number of newly approved liver disease drugs remains low across the US, China, Japan, and the EU. The urgent need for multi-target, low-toxicity therapies is critical [15].
In this context, the antioxidant and hepatoprotective properties of MF offer a promising avenue for innovative treatments targeting the oxidative mechanisms underlying liver disease pathology. Its ability to target multiple pathways involved in liver injury, including oxidative stress, inflammation, and fibrosis, positions it as a leading candidate for further clinical exploration. However, its clinical application has been limited by challenges typical of natural products, such as low oral bioavailability and poor metabolic stability. To overcome these obstacles, ongoing research is focused on enhancing its pharmacokinetic profile through structural modifications, novel drug delivery systems, and biotransformation strategies [16,17,18,19].
This review aims to synthesise recent research advances concerning the chemical properties, biological activity, pharmacokinetics, and structural modifications of MF, with particular emphasis on its translational significance as a nutritional supplement in the treatment of liver disease. By examining its molecular mechanisms and potential applications in liver disease, this paper provides a theoretical foundation for the development of precision therapies based on natural products, with a particular focus on the antioxidant properties of MF and their role in liver disease intervention.
2. Method
We conducted literature retrieval of MF using electronic databases, including PubMed, CNKI, Web of Science, SpecialSciDBS, Elsevier, and academic papers, to conduct a comprehensive analysis and summary. We used mangiferin, pharmacological activity, hepatoprotection, oxidative stress, bioavailability, antioxidant, biosynthesis and chemical synthesis as keywords to review the information about source, phytochemical properties, synthesis, pharmacokinetics, pharmacology analysis and bioavailability studies of MF.
3. Source and Phytochemical Properties of MF
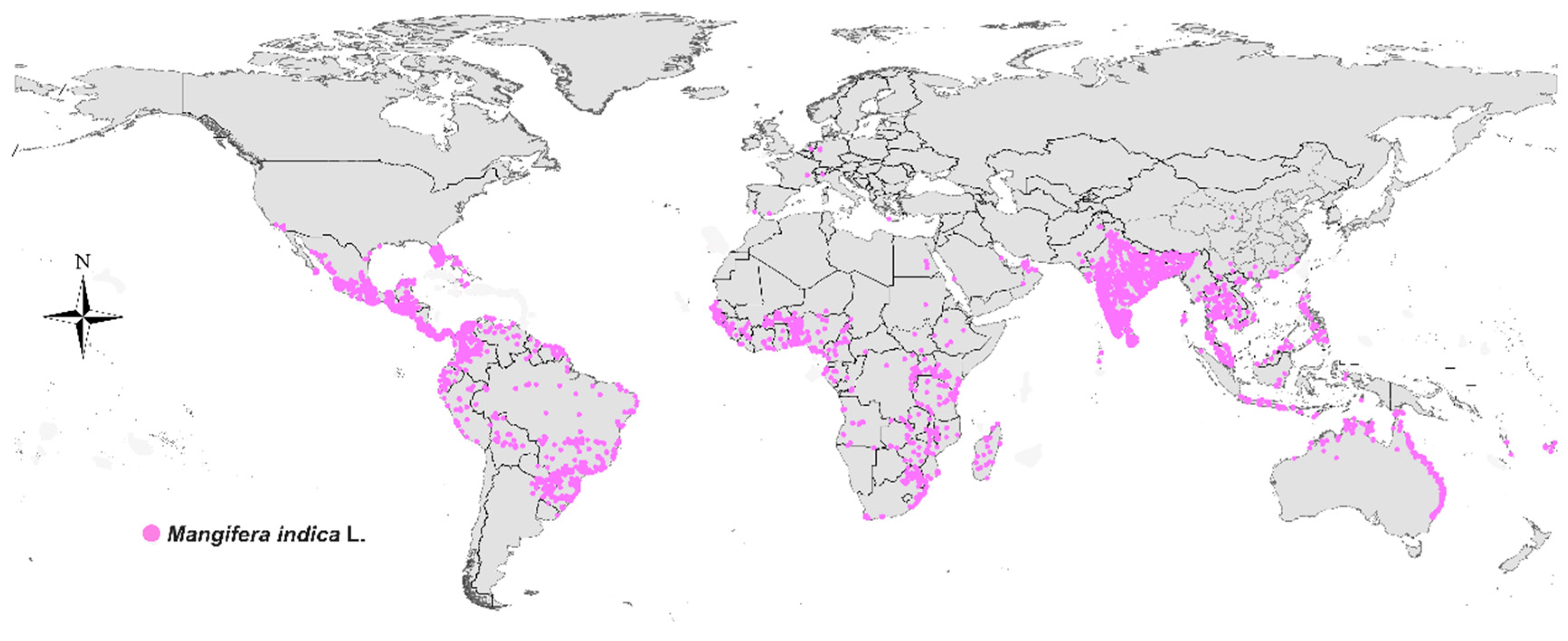
MF is a natural polyphenolic xanthone with a remarkably broad botanical distribution. It has been identified in over 180 species spanning more than 51 plant families, encompassing ferns, monocotyledons, and dicotyledons. The compound is not uniformly distributed across the plant kingdom but is particularly concentrated in several key families. Among these, the Gentianaceae, Iridaceae, and Anacardiaceae families are recognized as major sources. Notably, within the Gentianaceae family, certain species such as Gentianella caucasica have been reported to contain MF levels as high as 2.34% in their dried aerial parts. The mango tree (Mangifera indica L.), a member of the Anacardiaceae family, is another rich reservoir, with the highest concentrations typically found in the bark, leaves, and fruit peel (Figure 1). Furthermore, MF is a principal bioactive component in the rhizome of Anemarrhena asphodeloides, a plant widely used in traditional medicine. It is important to note that the MF content in any given plant is highly variable and influenced by factors such as the species, genetic cultivar, specific plant organ, and the methods of extraction and analysis. This diverse and widespread occurrence in the plant kingdom underscores its significance as a readily accessible phytochemical for pharmacological research and development [20,21,22,23] (Table 1 and Figure 2).
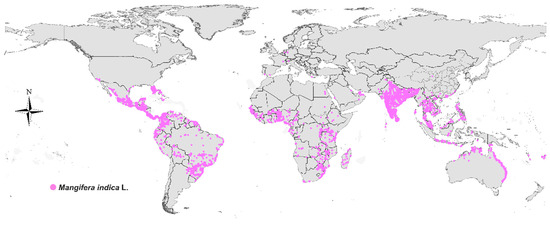
Figure 1.
The global distribution of mangoes.

Figure 2.
Some species containing mangiferin. Species images are reproduced from the POWO (Plants of the World Online) website (https://powo.science.kew.org/) with permission from [Royal Botanic Gardens, Kew], copyright [2025] and reproduced from the GBIF (Global Biodiversity Information Facility) website (https://powo.science.kew.org; https://www.gbif.org/) with permission from [www.GBIF.org], copyright [2025].
MF, a natural polyphenolic compound with the molecular formula C19H18O11, is a xanthone derivative [24,25,26]. Its core structure contains multiple reactive hydroxyl groups (notably at the C-2 and C-4 positions) and a glucose moiety linked via a β-glycosidic bond at the C-7 position. This compound appears as a yellow-to-light-brown crystalline powder, slightly soluble in water but readily soluble in polar solvents such as methanol and ethanol, with a melting point of 271~273 °C [27,28,29,30,31]. Its chemical stability is highly pH-dependent: under acidic conditions, the glycosidic bond undergoes hydrolysis to release the aglycone norathyriol [32,33,34]. Additionally, it is sensitive to light and heat, requiring storage in dark, low-temperature conditions to minimize oxidative degradation [35,36,37,38]. MF can be identified through colorimetric reactions and spectroscopic analysis (characteristic UV absorption peaks at 258 nm and 316 nm) [39,40,41]. Its polyhydroxy structure confers strong antioxidant activity, enabling free radical scavenging and metal ion chelation. However, while the glucose moiety enhances water solubility, it also limits bioavailability [23,42,43,44,45].

Table 1.
Sources of MF [23,41].
Table 1.
Sources of MF [23,41].
| No. | Scientific Name | Common Name | Source Parts in Plants |
|---|---|---|---|
| 1 | Mangifera indica | Mango | Fruits, leaves, bark |
| 2 | Mangifera persiciformis | Peach-shaped Mango | Fruits, leaves, bark |
| 3 | Mangifera sylvatica | Forest Mango | Fruits, leaves, bark |
| 4 | Hiptage benghalensis | Hiptage | Leaves; Flowers |
| 5 | Mammea americana | Mammee Apple | Branch; Leaves |
| 6 | Carica papaya | Papaya | Leaves |
| 7 | Citrus limon | Lemon | Fruit peel |
| 8 | Terminalia chebula | Chebulae Fructus | Fruit pulp |
| 9 | Cydonia oblonga | quince | Fruits; Seeds |
| 10 | Prunus amygdalus | European plum | Fruits |
| 11 | Garcinia mangostana | Mangosteen | Fruit peel |
| 12 | Coffea arabica | Arabian coffee | Leaves |
| 13 | Phaleria capitata | - | Seeds |
| 14 | Phaleria macrocarpa | - | Seeds |
| 15 | Aspalathus linearis | Rooibos | Leaves |
| 16 | Gypsophila pacifica | - | Roots; Leaves |
| 17 | Curio radicans | - | Roots; Stem |
| 18 | Penthorum chinense | all-grass of Chinese Penthorum | Leaves; Fruits |
| 19 | Swertia macrosperma | - | Whole herb |
| 20 | Swertia mussotii | Herba Swertiae Mussotii | Whole herb |
| 21 | Swertia punicea | - | Whole herb |
| 22 | Swertia kingii | - | Whole herb |
| 23 | Swertia franchetiana | - | Whole herb |
| 24 | Gentianella turkestanorum | - | Leaves |
| 25 | Gentiana algida | Alpine Gentian | Leaves; Flowers; Whole herb |
| 26 | Gentiana rhodantha | - | Leaves; Flowers; Whole herb |
| 27 | Hedysarum alpinum | - | Rhizome; Leaves |
| 28 | Hedysarum flavescens | - | Rhizome; Leaves |
| 29 | Astragalus membranaceus | Astragali Radix | Rhizome; Leaves |
| 30 | Anemarrhena asphodeloides | Anemarrhenae Rhizoma | Rhizome |
| 31 | Aquilaria sinensis | Chinese Eaglewood | Resin-containing heartwood |
| 32 | Aquilaria crassna | Eaglewood | Resin-containing heartwood |
| 33 | Sesamum indicum | sesame | Seeds |
| 34 | Dobinea delavayi | - | Rhizome |
| 35 | Reynoutria japonica | Giant Knotweed Rhizome | Rhizome; Leaves |
| 36 | Polygala tenuifolia | Thinleaf Milkwort Root-bark | Roots; Stem; Leaves |
4. Extraction and Separation Methods of MF
The extraction and separation methods for mangiferin have developed into a relatively mature process system. Common extraction strategies include solvent extraction (such as ethanol-water systems) combined with physical assistance technologies like ultrasonication and microwaving to enhance efficiency. For raw materials with high gum content, such as mango leaves, pretreatment steps like ester extraction for impurity removal are often employed. During the separation and purification stage, macroporous resin chromatography serves as an effective method for obtaining high-purity products, often supplemented by crystallization techniques (such as recrystallization exploiting solubility differences in hot and cold methanol) for final refinement. The integrated application of these methods enables the efficient extraction of high-purity mangiferin from diverse plant sources including mango leaves and mango peel [38,39,45].
5. Synthesis of MF
5.1. Biosynthesis
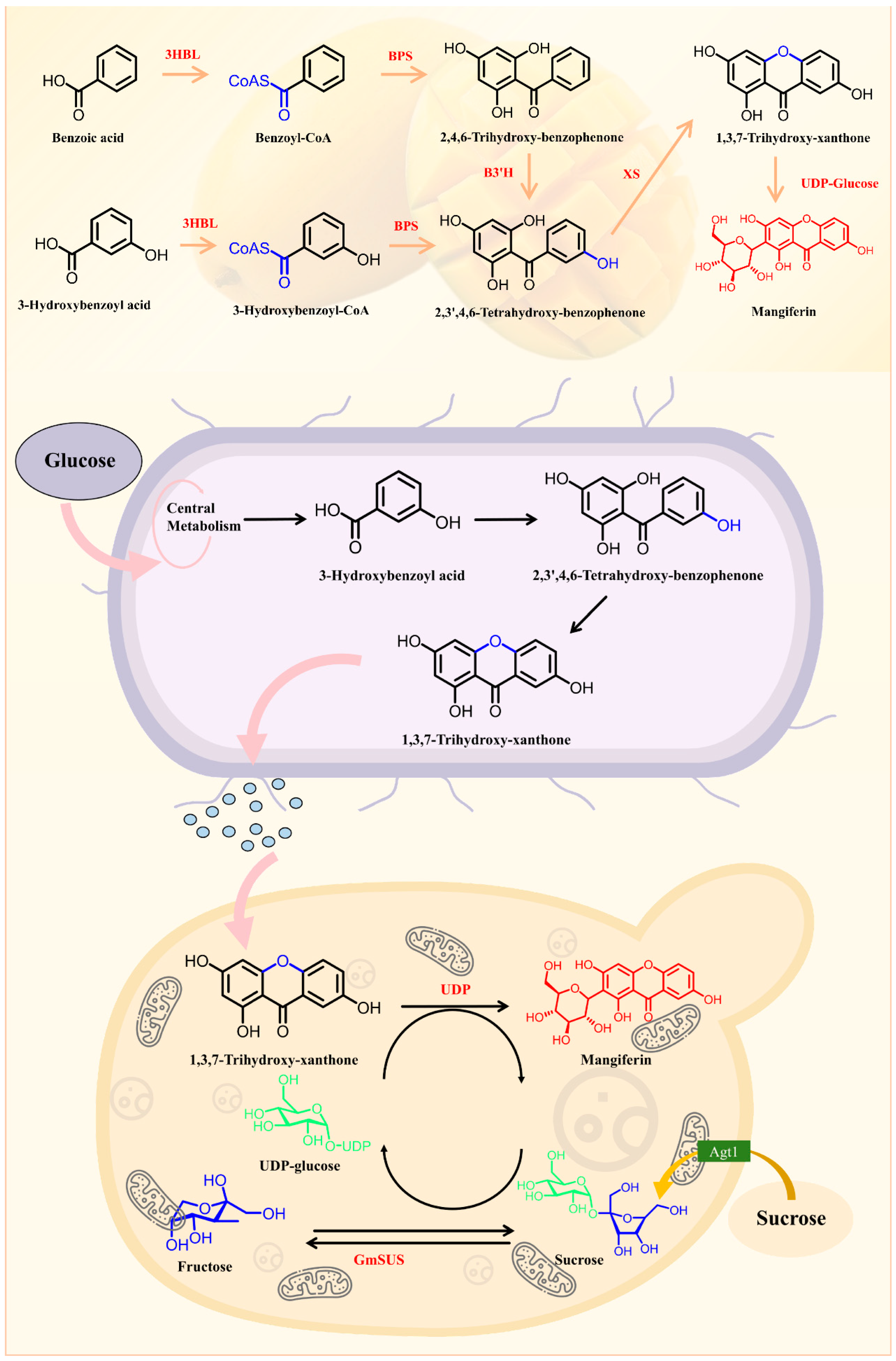
MF, a bioactive xanthonoid with antioxidant and anti-inflammatory properties, is biosynthesized through the integration of phenylpropanoid and polyketide pathways. Starting from phenylalanine, phenylalanine ammonia-lyase generates p-coumaric acid, which is converted to benzoyl-CoA. A type III polyketide synthase then extends the polyketide chain using malonyl-CoA, followed by cyclization and oxidation via cytochrome P450 enzymes to form the xanthone core. Subsequent hydroxylation and methylation modify the skeleton, while a UDP-glycosyltransferase attaches glucose to the C-2 hydroxyl group to complete glycosylation. The synthesis is regulated by developmental stages, environmental stresses, and jasmonic acid signaling. Heterologous expression of key enzymes enables metabolic engineering for production, though challenges remain in pathway elucidation, enzyme activity optimization, and intermediate toxicity. Deciphering these mechanisms holds promise for natural drug development and synthetic biology applications [44,46] (Figure 3).
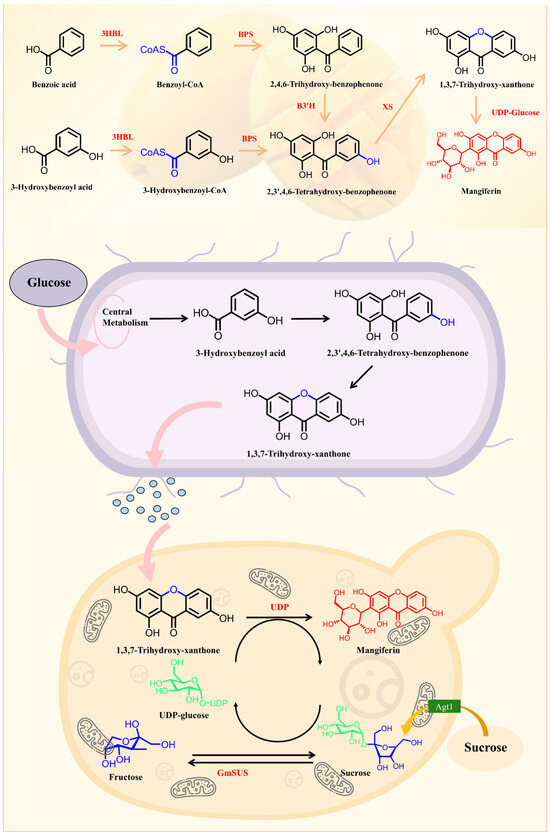
Figure 3.
Mangiferin biosynthesis and heterologous synthesis hypothetical pathway.
5.2. Chemosynthesis
5.2.1. Total Synthesis of MF
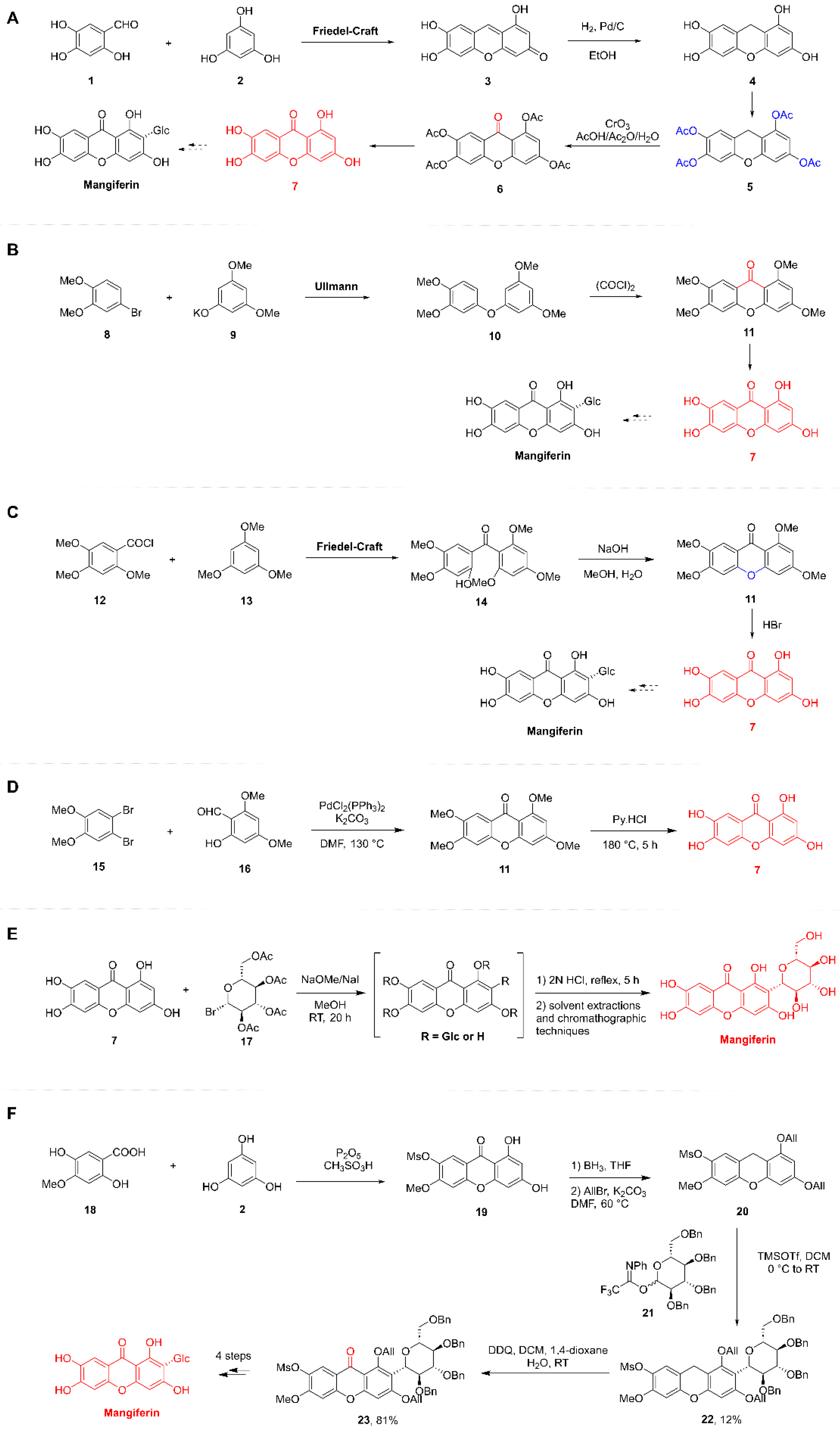
Synthesis of the Xanthone Moiety
The chemical synthesis of xanthones has attracted considerable interest from organic chemists due to their inherent biological significance. Starting from the original substrates 2,4,5-trihydroxybenzaldehyde (1) and phloroglucinol (2), compound 3 was obtained via a Friedel-Crafts reaction. Compound 4 was then obtained via hydrogenation, compound 5 was obtained via complete acetylation, compound 6 was obtained by oxidizing the C-9 position of compound 5 with CrO3, and it was hydrolyzed under acidic conditions to compound 7, which is tetrahydroxyoxazolone (Figure 4A). Additionally, they also employed 4-bromoveratrole (8) and potassium 3,5-dimethoxyphenoxide (9) to obtain the coupling product 10 via an Ullmann reaction. Subsequently, compound 10 underwent a Friedel-Crafts reaction in the presence of oxalyl chloride to afford compound 11. Demethylation of compound 11 then yielded compound 7 [37] (Figure 4B). Researcher synthesized tetrahydroxyxanthone using a Friedel-Crafts reaction, developed by Shah, as the key step. This involved the reaction of 2,4,5-trimethoxybenzoyl chloride (12) with 1,3,5-trimethoxybenzene (13) under ZnCl2-POCl3 conditions to afford the corresponding benzophenone intermediate 14 [47] (Figure 5C). Thus, 2,4,5-trimethoxybenzoyl chloride (12) and 1,3,5-trimethoxybenzene (13) were subjected to a Friedel-Crafts reaction in the presence of AlCl3 to yield compound 14. Subsequent intramolecular cyclization of 14 in aqueous methanolic NaOH furnished compound 11. Demethylation of 11 under refluxing HBr then afforded compound 7 (Figure 4C). Thus, 2,4,5-trimethoxybenzoyl chloride (12) and 1,3,5-trimethoxybenzene (13) were subjected to a Friedel-Crafts reaction in the presence of AlCl3 to yield compound 14. Subsequent intramolecular cyclization of 14 in aqueous methanolic NaOH furnished compound 11. Demethylation of 11 under refluxing HBr then afforded compound 7 [47,48] (Figure 4D).
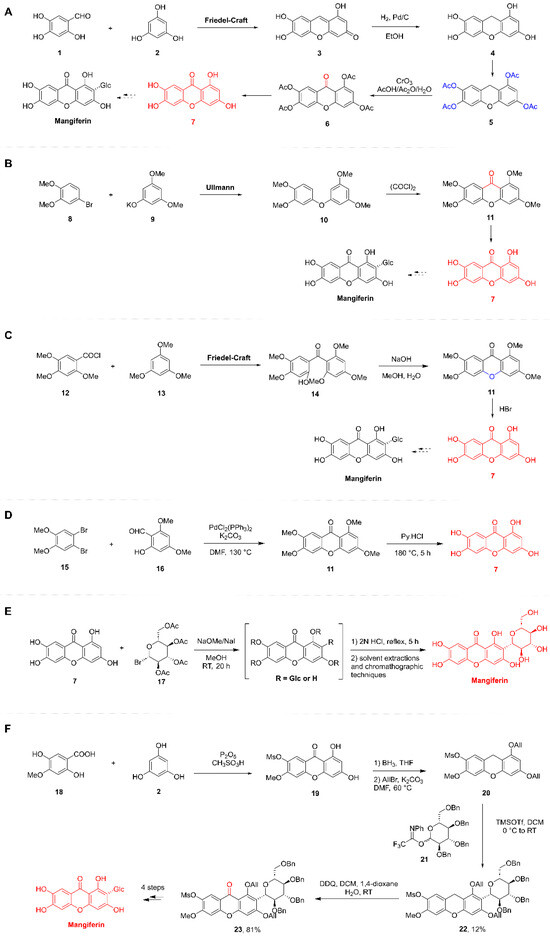
Figure 4.
Total synthetic route of Mangiferin. (A,B): The Tanase research group conducted a study on the synthesis of tetrahydroxyxanthone (1941). (C): The Scheinmann research group reported the synthesis of tetrahydroxyxanthone (1973). (D): The Yang group developed an efficient synthesis of tetrahydroxyxanthone (2014). (E): The research team of Nott and Roberts achieved the synthesis of MF (1967). (F): The Yu group devised an efficient synthetic route to MF (2010).
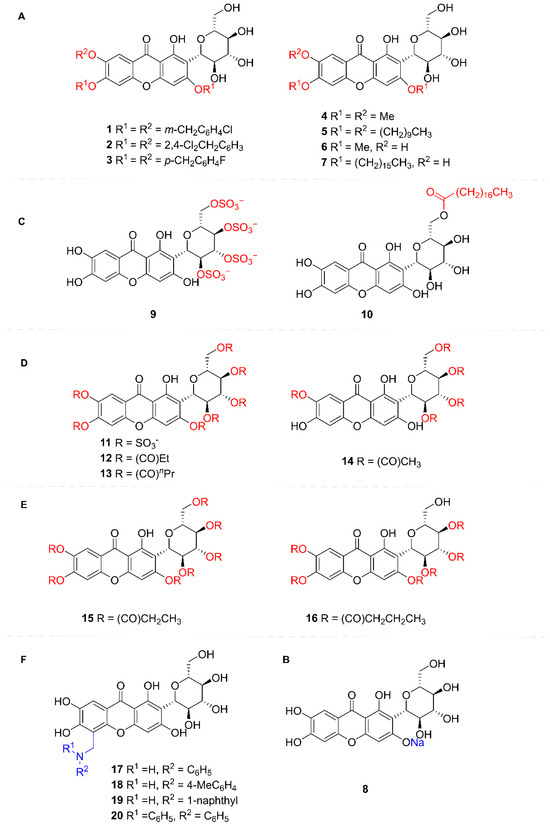
Figure 5.
Structural Modification Schematic of Mangiferin. (A) Hydroxy groups on the xanthone nucleus; (B) Sodium phenolate salts on the xanthone nucleus; (C) Hydroxy groups of glucose; (D) Hydroxy groups of mangiferin; (E) Oxygenated xanthone core’s C-8 position; (F) Nitrogen-containing derivatives of mangiferin.
This was followed by the stereoselective construction of the C-glycosidic bond. In traditional carbohydrate chemistry, the stereoselective formation of C-glycosidic bonds presents significantly greater challenges than that of O-glycosidic bonds. The total synthesis required implementation via either Friedel-Crafts glycosylation or Lewis acid-catalyzed C-glycosylation reactions. However, these reactions can be accompanied by the formation of byproducts and pose difficulties in stereochemical control.
This pioneering work established the C-glycosidic bond via Friedel-Crafts glycosylation, utilizing the electron-rich flavonoid nucleus (xanthone core) as the acceptor and glucose as the donor, culminating in the total synthesis of MF. Specifically, compound 7 was reacted with an excess of α-acetobromoglucose (17) in anhydrous methanol containing sodium methoxide/sodium iodide, yielding a mixture of C- and O-glucosylated xanthones. Acidic treatment with diluted hydrochloric acid selectively cleaved the O-glucosidic bond while leaving the C-glucosidic bond intact. Subsequent extraction and chromatographic separation finally afforded MF, albeit in a yield of only 0.1% (Figure 4E). Researchers have also conducted studies using such methods. However, the yield remained similarly low at merely 0.05%. Despite the extremely low yields, this strategy achieved the selective construction of the C-glycosidic bond, laying the essential groundwork for the subsequent optimization of the synthetic route [49] (Figure 4E).
Researchers have also conducted studies on the total synthesis of MF. Recognizing that the electron-withdrawing effect of the C-9 carbonyl group diminishes the nucleophilicity of the xanthone nucleus, researchers opted to perform the C-glycosylation on a xanthone precursor prior to introducing the carbonyl group at C-9. The synthesis commenced with the construction of the xanthone nucleus (20), and achieved in three steps: (a) Condensation of 4-methoxy-2,5-dihydroxybenzoic acid (18) with phloroglucinol (2) using P2O5/CH3SO3H afforded xanthone 19, (b) Reduction in the C-9 carbonyl group in 19 with BH3 yielded the corresponding xanthene intermediate, (c) Allylation of the 1,3-dihydroxy groups furnished the desired xanthone nucleus 20. Subsequently, glycosylation of xanthone nucleus 20 with 2,3,4,6-tetra-O-benzyl-D-glucopyranosyl N-phenyl trifluoroacetimidate (21) under TMSOTf/DCM conditions afforded the target C-glycoside 22 in 12% yield. This was followed by oxidation of glycoside 22 with DDQ to introduce the carbonyl group at C-9, providing the benzylated xanthone glycoside 23 in 81% yield. Finally, sequential removal of the allyl, mesyl (methylsulfonyl), methyl, and benzyl protecting groups delivered MF. Notably, the allyl protecting group proved indispensable for successful glycosylation, as analogous attempts using benzyl or methoxy protecting groups under similar conditions failed to afford the desired glycoside [50] (Figure 4F).
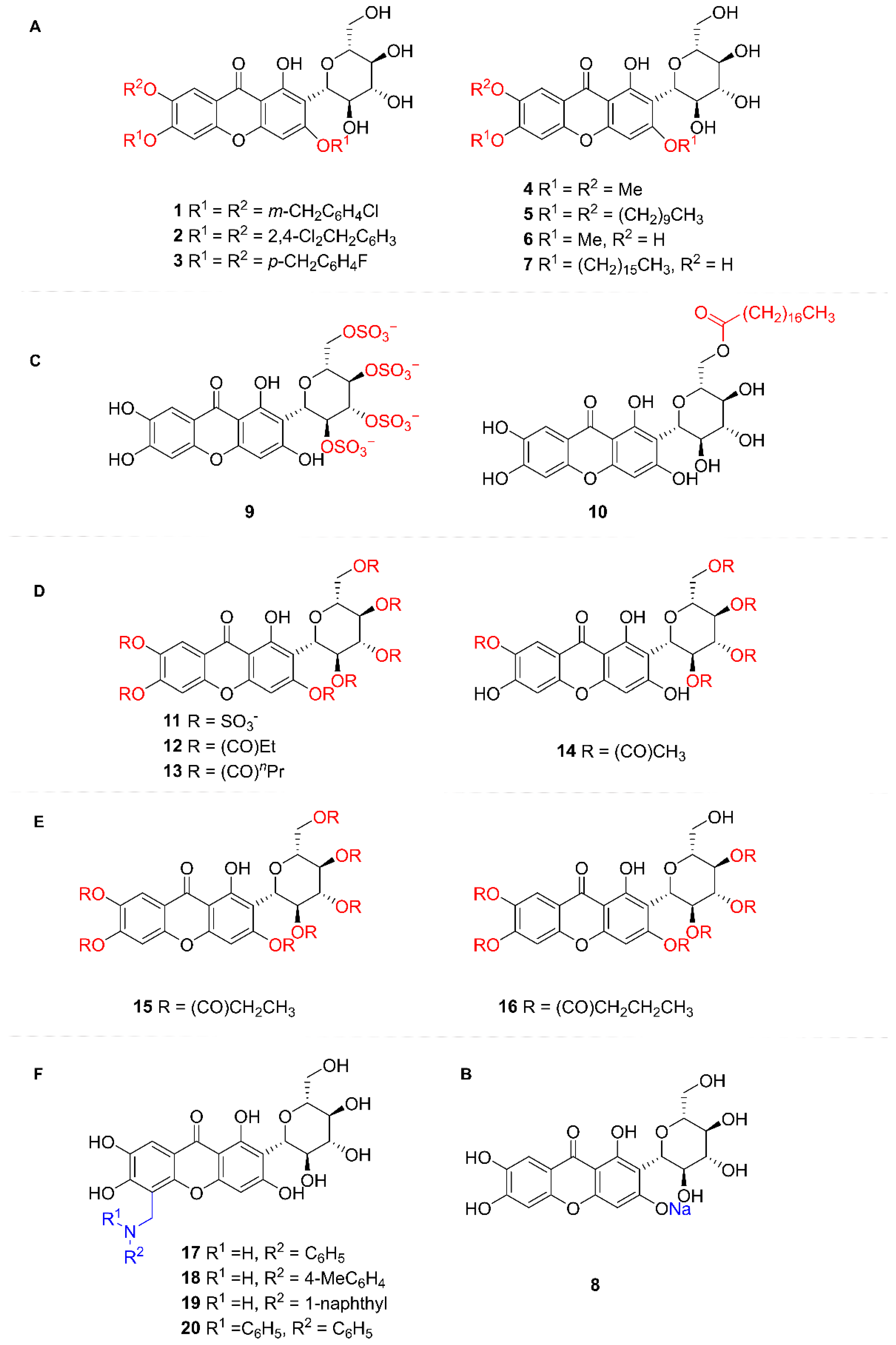
5.2.2. Structural Modification of MF
MF is a naturally occurring flavonoid C-glycoside. Its core structure consists of a chromone scaffold bearing a glucosyl group attached at the C-2 position via a C-glycosidic bond. Structural modifications of its derivatives are primarily focused on the hydroxy groups and the aglycone scaffold, aiming to optimize solubility, pharmacological activity, and targeting specificity.
- (1)
- Hydroxy groups on the xanthone nucleus (Benzyl, alkyl, and other groups)
Studies revealed that introducing long-chain alkyl groups and bulky lipophilic substituents onto the MF core in compounds 4–7 significantly enhanced their inhibitory activity against protein tyrosine phosphatase 1B. Notably, compound 5 achieved complete (100%) inhibition of this enzyme at a concentration of 50 μmol/L [51] (Figure 5A).
- (2)
- Sodium phenolate salts on the xanthone nucleus
Synthesis of MF monosodium salt was achieved under alkaline conditions by selective conversion of the 3-phenolic hydroxy group to its sodium phenolate salt. This modification significantly enhanced the aqueous solubility of the resulting product. Studies revealed that MF monosodium salt exhibits marked antitussive, expectorant, antiasthmatic, and anti-inflammatory activities. Notably, its antitussive, expectorant, and anti-inflammatory effects were significantly superior to those of MF. Subsequent research further demonstrated the ameliorative effects of MF sodium salt on alcoholic hepatitis [52,53,54,55] (Figure 5B).
- (3)
- Hydroxy groups of glucose (Sulfonic group, acyl group)
MF was esterified with benzoic acid, stearic acid, and phenylalanine to yield amphiphilic MF ester derivatives. These derivatives exhibited significantly enhanced solubility compared to MF, facilitating improved cellular uptake and augmenting their antioxidant activity. They demonstrated superior efficacy in inhibiting adipocyte differentiation and lipid droplet formation, suppressing leptin, pro-inflammatory cytokines, and oxidative stress responses, while promoting adiponectin secretion. These properties suggest their potential to delay obesity onset and mitigate obesity-associated precocious puberty. Notably, the stearic acid-modified MF derivative 10 displayed the most potent effects, positioning it as a promising therapeutic candidate for ameliorating obesity and preventing precocious puberty [56] (Figure 5C).
- (4)
- Hydroxy groups of MF (sulfonic acid and acyl group)
The polysulfation of hydroxyl groups in MF yielded heptasulfated MF. The key modification lies in the introduction of sulfate groups, which enhances molecular negative charge and target binding capacity. Studies demonstrate that sulfated MF derivatives exhibit significantly improved solubility, stability, and anticoagulant/antiplatelet activities compared to the parent compound. These findings provide a theoretical foundation for the development of novel antithrombotic agents [57] (Figure 5D).
- (5)
- Oxygenated xanthone core’s C-8 position
The introduction of various aromatic amine groups significantly alters the physicochemical properties of MF derivatives. Incorporation of lipophilic substituents potentially enhances membrane permeability, thereby improving bioavailability. Experimental data indicates that these analogs exhibit superior antipyretic activity to MF at 200 mg/kg doses, with naphthyl- and bis-phenylamino-containing derivatives demonstrating the most pronounced effects. This enhanced efficacy is hypothesized to correlate with improved antioxidant capacity and inhibition of TNF-α synthesis. Structural modifications through strategic manipulation of molecular polarity and steric effects successfully balance solubility characteristics with target engagement efficiency, offering a novel paradigm for developing highly efficient, low-toxicity antipyretic agents [58,59] (Figure 5E).
6. Pharmacokinetics of MF
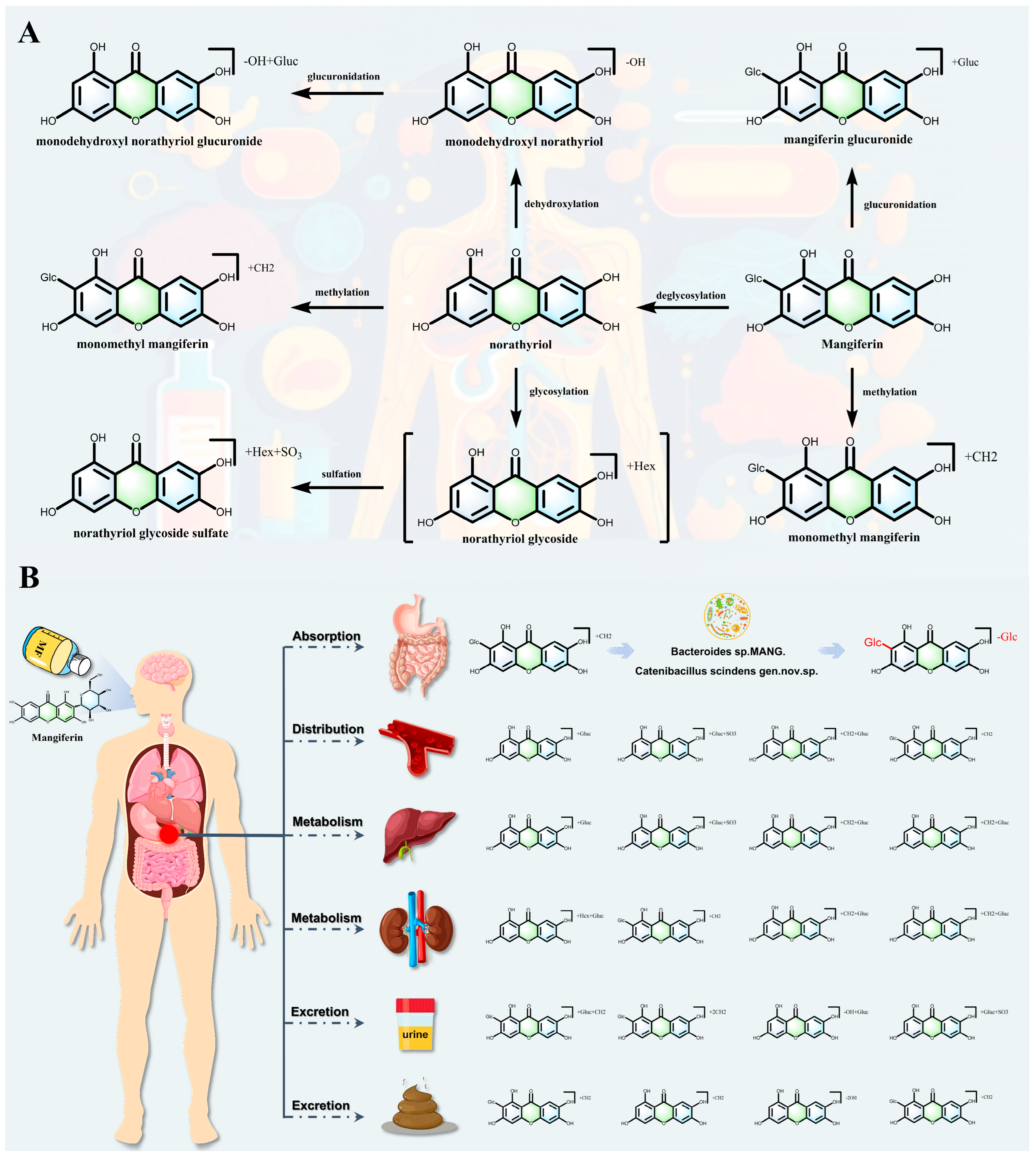
The pharmacokinetic process of MF involves a multi-stage biotransformation via multiple reactions, including glycosylation, deglycosylation, methylation, glucuronidation, sulfation, and dehydroxylation, and the intestinal flora plays a key regulatory role in the early stages of metabolism [60,61] (Figure 6A). This process can be divided into three sequential phases: initial activation by gut microbiota, systemic modification in the liver, and final excretion with potential recirculation.
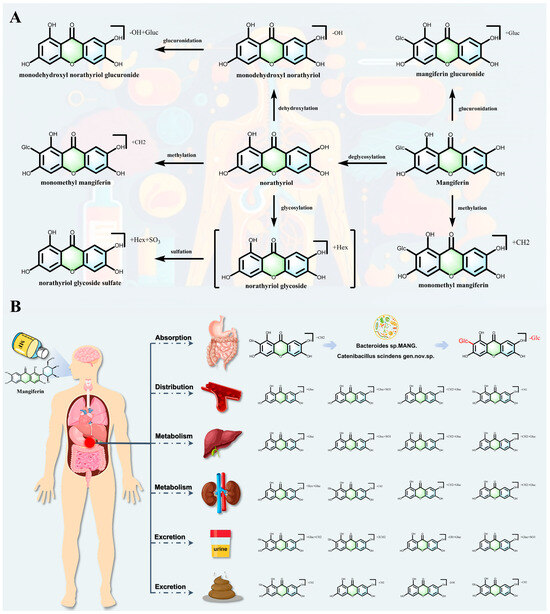
Figure 6.
(A,B): The process of absorption, distribution, metabolism and excretion pattern of Mangiferin.
In the intestinal flora-mediated metabolism, MF (C-glycoside) is specifically hydrolyzed by C-glycosidase secreted by intestinal commensal bacteria to produce the aglycone norathyriol. Additionally, some bacterial strains further catalyze the removal of secondary glycosidic bonds via β-glucosidase, resulting in low-glycosylated products [21,62,63,64]. This initial deglycosylation process is accompanied by in situ methylation, and colony metabolizing enzymes catalyze the methylation of phenolic hydroxyl groups to generate mono-or di-methylated derivatives, which significantly enhances the lipid-solubility of the metabolite and the efficiency of transmembrane absorption [65,66]. This microbial preprocessing is a crucial step that enables the efficient absorption of MF-derived metabolites.
Upon entry into the systemic circulation, the liver systematically regulates metabolite properties through phase II conjugation reactions: uridine diphosphate glucuronosyltransferases mediate glucuronidation, sulfotransferases catalyze sulfation, and glycosyltransferases may reintroduce secondary sugar groups to form novel O-glycoside derivatives. Furthermore, cytochrome P450 enzymes regulate the strength and targeting of activity by dehydroxylating to produce low-hydroxyl metabolites. In the excretion and recirculation chain, the resulting conjugates are excreted via bile or urine, and some of them can be hydrolyzed anew by intestinal flora to form an enterohepatic cycle, thereby prolonging their systemic exposure. Metabolomics studies based on UHPLC-Q-Exactive orbitrap HRMS have identified a variety of metabolites, revealing the complexity of the intestinal flora-hepatic synergistic metabolic network, among which the competitive relationship between methylation and glucuronidation, and the discovery of new metabolites of trihydroxyflavonoids provide a key basis for the optimization of the design of prodrugs and the evaluation of individualized therapeutic efficacy (Figure 6B). In conclusion, the metabolic kinetics of MF covers deglycosylation, methylation, glucuronidation, sulfation, glycosylation and dehydroxylation pathways, and its multi-organ synergistic mechanism not only elucidates the causes of low bioavailability, but also lays a theoretical foundation for the development of targeted metabolites [67,68,69].
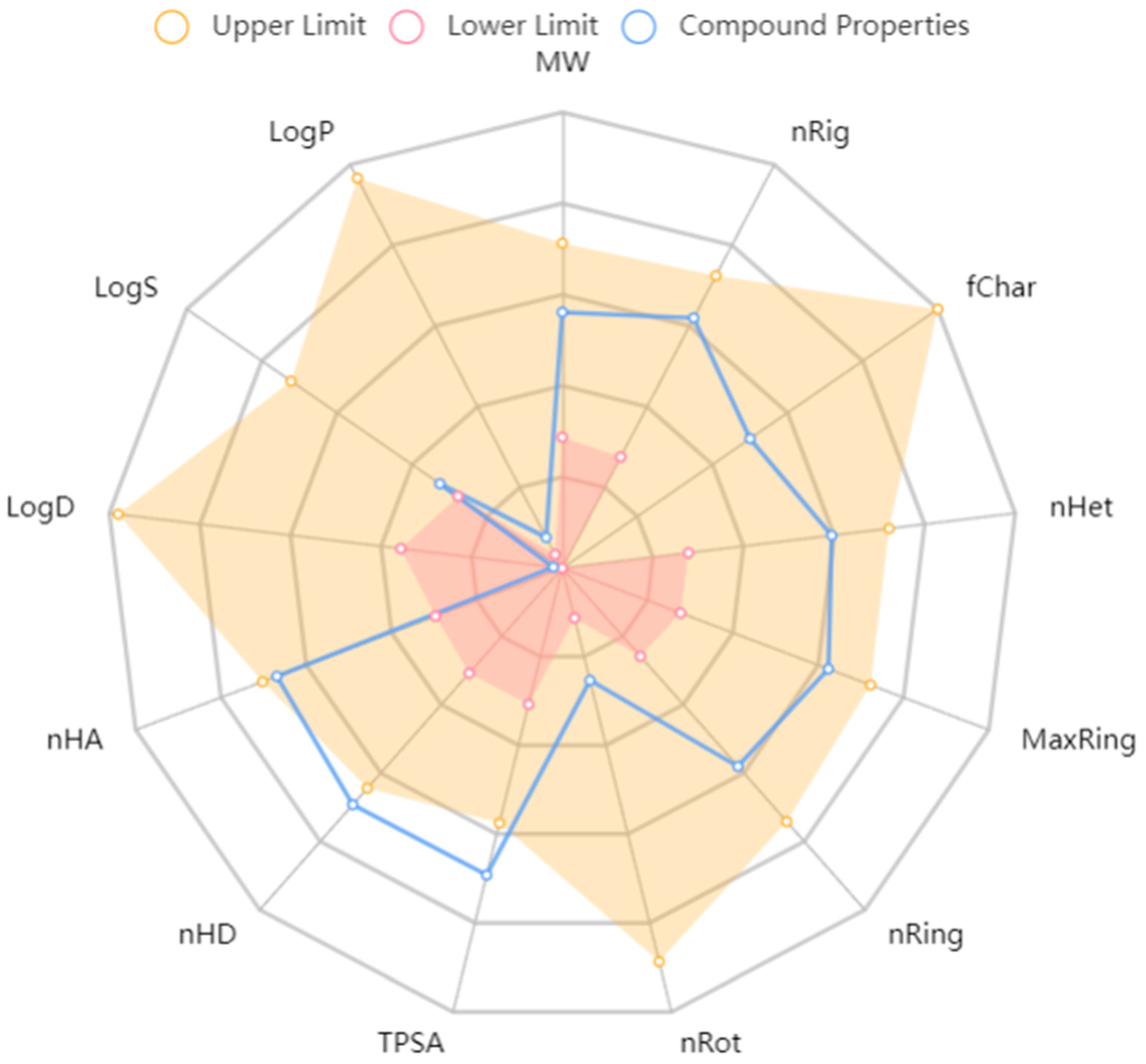
Complementing the experimental findings, in silico predictions provide a theoretical perspective on MF’s ADME properties. The ADME process of MF was predicted by the ADMETLab 3.0 platform and Deep ToxLab platform (Figure 7). According to the ADME prediction results, MF exhibits poor oral absorption (low bioavailability), difficulty in penetrating cell membranes and the blood–brain barrier, and limited distribution in the body due to its large molecular weight (approximately 422 g/mol), strong hydrophilicity (extremely low LogP/LogD), high polar surface area, and abundant hydroxyl groups (multiple hydrogen bond donors). Additionally, its polyphenolic hydroxyl structure is prone to phase II metabolism, leading to rapid metabolism and primarily excretion via the kidneys and bile, which aligns with the extensive conjugation observed experimentally.
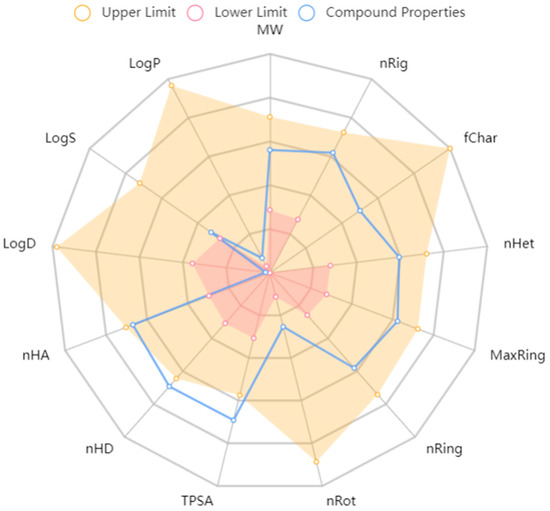
Figure 7.
Radar chart involved in ADMET properties of mangiferin and relevant metabolites compared with the thresholds. Het, heteroatoms; fChar, formal charge; Rot, rotatable bonds; HD, hydrogen bond donors; MaxRing, atoms in the biggest ring; TPSA, topological polar surface area; LogS, solubility.
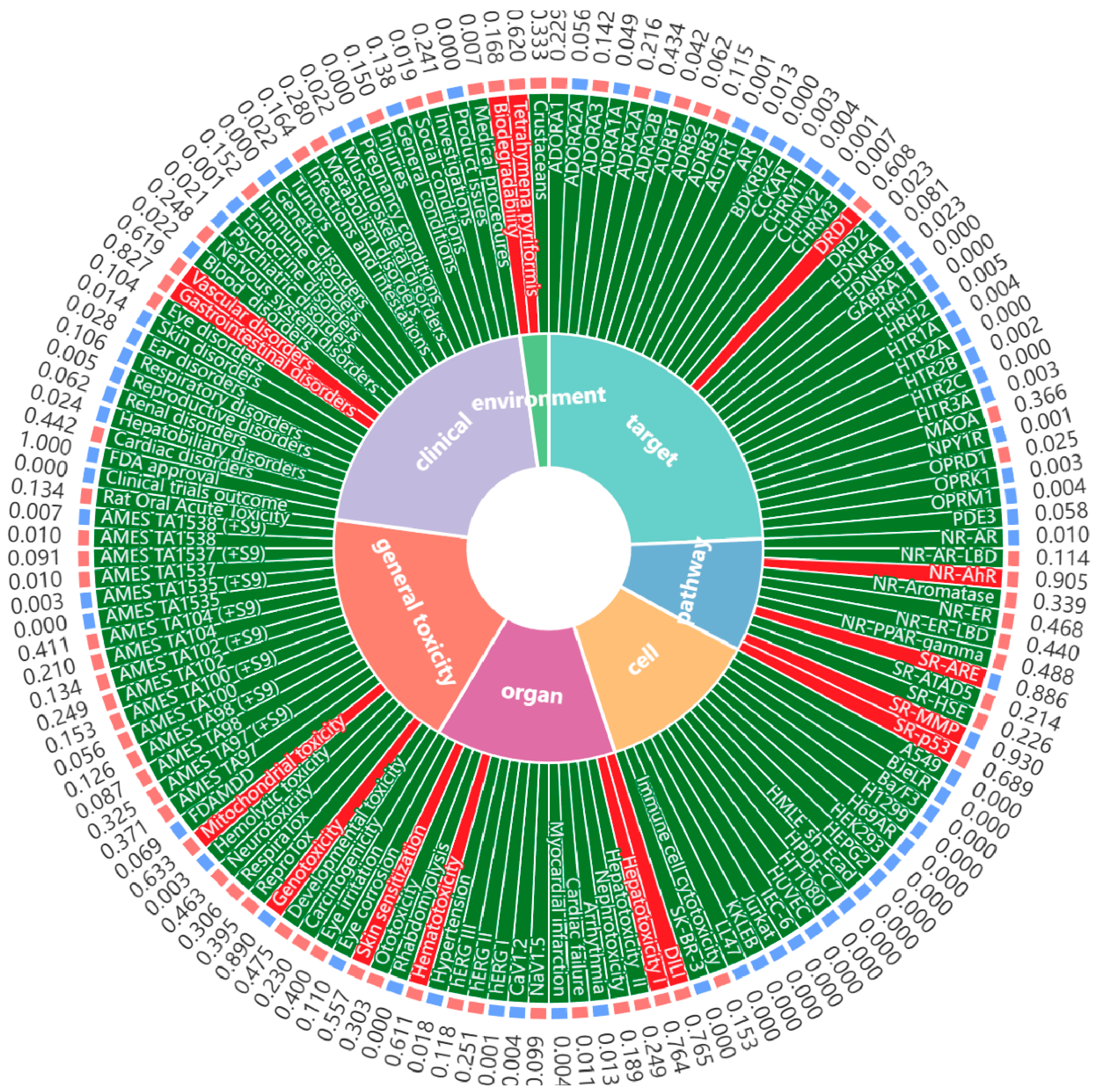
7. Safety of MF
The toxicology of MF was predicted by Deep ToxLab platform (Figure 8). Toxicological predictive analysis indicates that MF exhibits no significant toxicity risks across seven dimensions: target toxicity, pathway toxicity, cellular toxicity, organ toxicity, animal toxicity, clinical toxicity, and environmental toxicity, demonstrating good safety characteristics. This computational prediction is strongly supported by evidence from pre-clinical in vivo studies. Acute toxicity assessments have established that MF is practically non-toxic following oral administration, with a median lethal dose (LD50) reported to be as high as 4984 mg/kg body weight in mice. In sub-chronic toxicity studies, oral administration of MF at doses ranging from 250 to 1000 mg/kg for 28 days did not induce any abnormal clinical signs or hematological alterations in rats, indicating a wide safety margin for medium-term use [41]. These results further highlight MF’s favorable safety profile as a natural antioxidant, reinforcing its potential for therapeutic use with minimal toxicological concerns, thus enhancing its appeal as a viable candidate for clinical application.
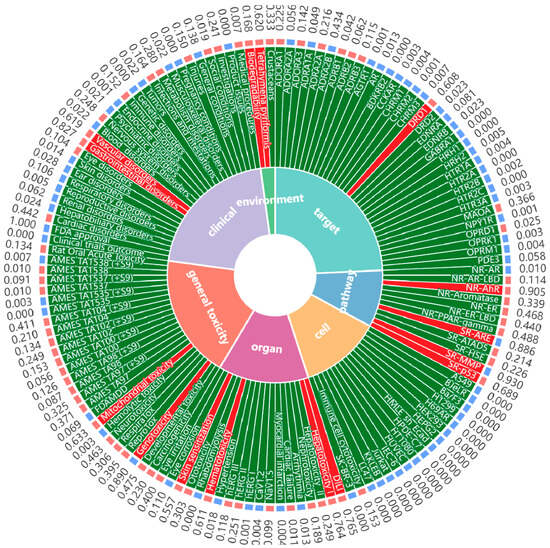
Figure 8.
Toxicity prediction of mangiferin via Deep ToxLab.
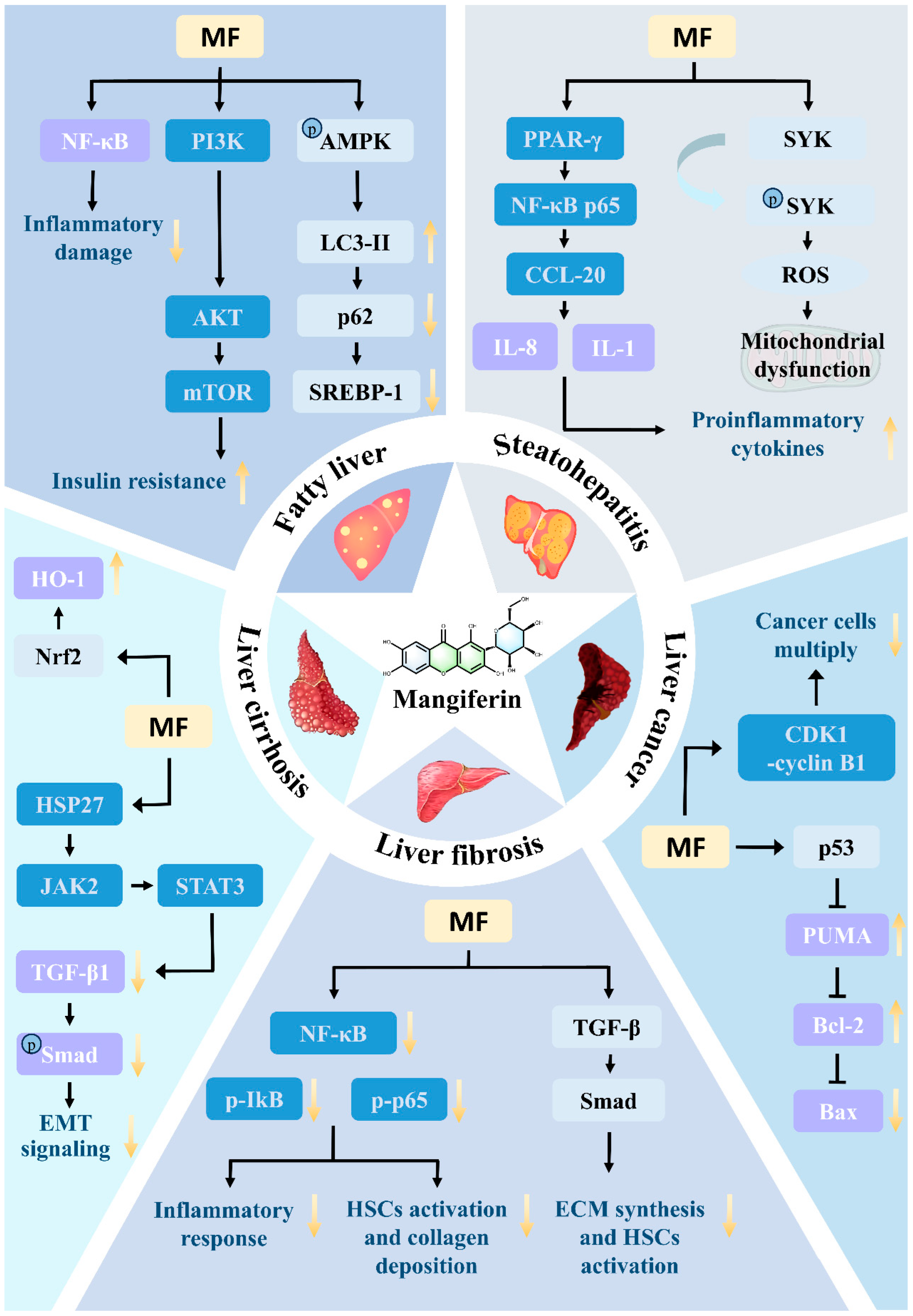
8. Mechanism of MF in the Treatment of Liver Disease
According to the World Health Organization, about 20% of the global disease burden is related to liver disease. As the core organ of human metabolism and detoxification, the dynamic evolution of pathological injury in the liver is often characterized by multiple stages, covering acute liver injury, non-alcoholic fatty liver disease (including simple fatty liver and steatohepatitis), liver fibrosis, cirrhosis, and up to the malignant transformation of hepatocellular carcinoma [70,71,72]. In this pathological continuum, molecular mechanisms such as oxidative stress, mitochondrial dysfunction, inflammatory cascade and abnormal deposition of extracellular matrix are intertwined to drive the disease towards end-stage. Although some progress has been made in clinical intervention strategies, their efficacy is mostly limited to a single pathology, and there are problems such as low bioavailability, insufficient targeting, and toxicity of long-term drug use [73,74].
In recent years, natural product multi-target intervention strategies have attracted much attention due to both pharmacological activity and safety advantages. MF, a C-glucosylxanthones isolated from Mangifera indica, has been shown to be effective in regulating the nuclear factor E2-related factor 2 (Nrf2)/antioxidant response element pathway, inhibiting the activation of nucleotide-binding oligomerization structural domain-like receptor protein 3 (NLRP3) inflammatory vesicles, and antagonizing the activation of transforming factor-β. Growth factor-β/Smad signaling and other key mechanisms have shown multidimensional regulatory potential, providing an important direction for the development of novel therapeutic strategies for liver disease [75,76].
In the field of liver disease research, there are various modeling methods for different stages of liver disease, and MF has demonstrated unique mechanisms and pharmacological activities in the treatment of various stages of liver disease [77].
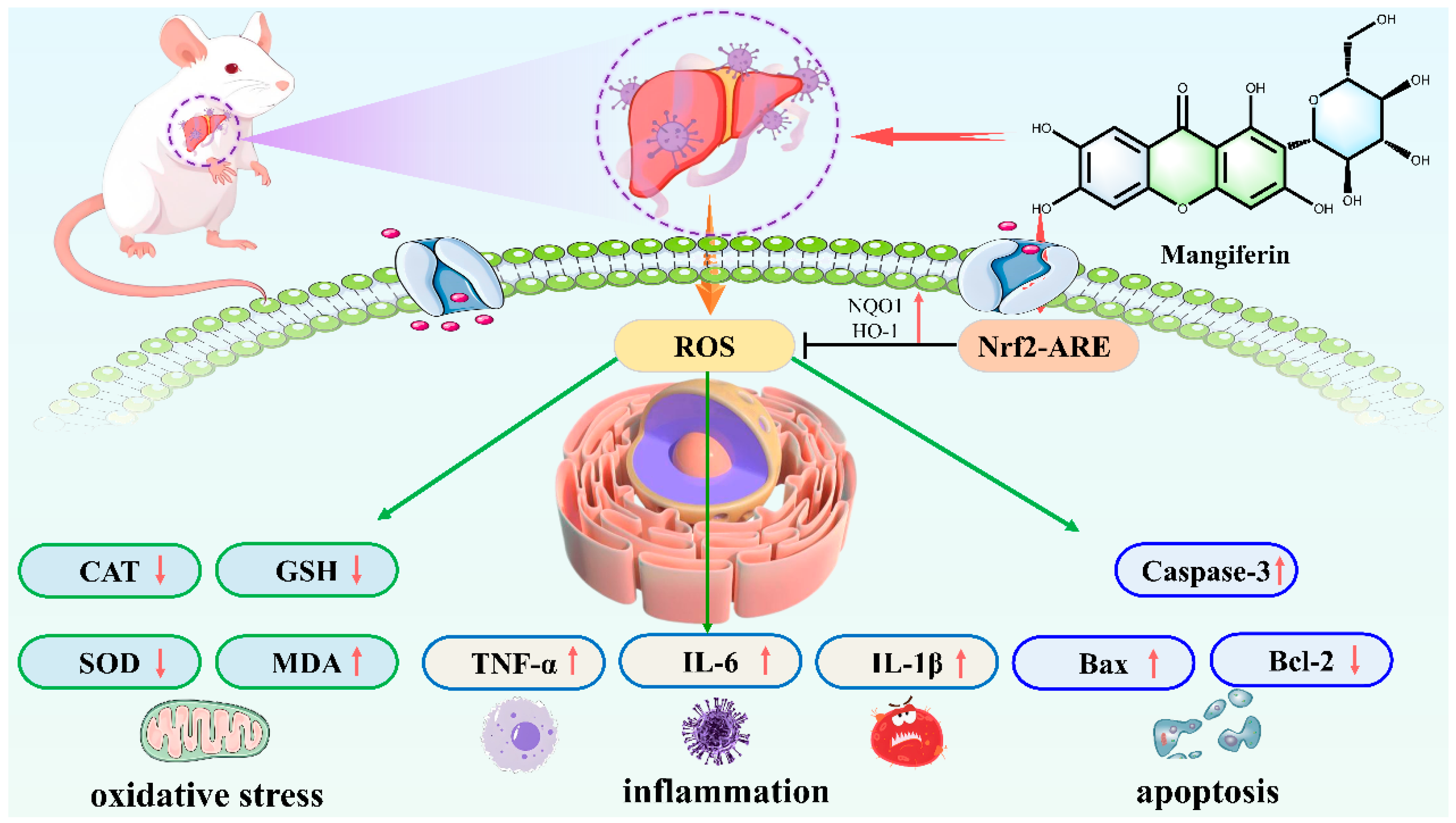
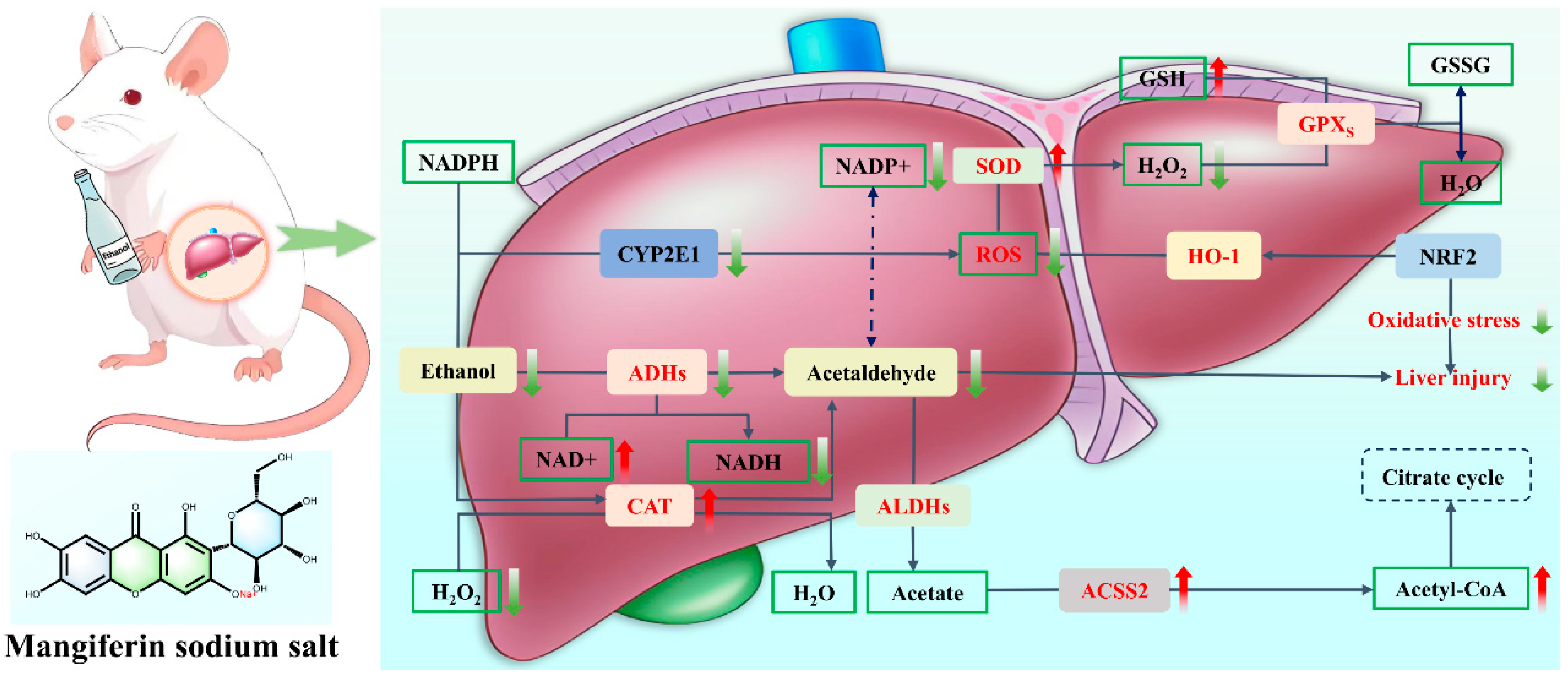
8.1. Acute Liver Injury
In acute liver injury, lipopolysaccharide combined with D-galactosamine, acetaminophen, and carbon tetrachloride (CCl4) are often used to induce modeling. The mechanism of MF treatment of acute liver injury mainly involves the regulation of multiple signaling pathways and intracellular processes, which promotes the expression of antioxidant enzymes and enhances the body’s antioxidant capacity to inhibit oxidative stress injury by activating the Nrf2 pathway, inhibits the activation of NLRP3 inflammatory vesicles, and regulates the endoplasmic reticulum stress-related miR-20a/miR-101a-Nrf2 axis to maintain endoplasmic reticulum homeostasis [78]. It can also promote the expression of heme oxygenase-1 (HO-1) in Kupffer cells, inhibit the production of inflammatory factors such as TNF-α, and exert hepatoprotective effects. Its pharmacological activity is manifested in significantly reducing the serum levels of liver injury markers such as alanine aminotransferase and azelaic transaminase and alleviating pathological changes such as hepatocyte degeneration and necrosis [79] (Figure 9).
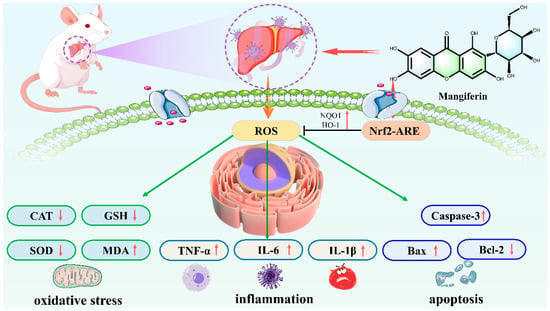
Figure 9.
Mangiferin against Polar Liver Injury mechanism diagram.
8.2. Fatty Liver
For fatty liver, a model is usually constructed using high-fat-diet-fed animals. MF can regulate fat metabolism-related signaling pathways, activate the AMPK pathway, inhibit the activity of fatty acid synthase and other key enzymes of lipid synthesis, promote fatty acid oxidation, and reduce hepatic fat accumulation [80]. Meanwhile, it can inhibit inflammatory responses, reduce the expression of inflammatory factors such as TNF-α and IL-6, and improve the hepatic inflammatory microenvironment, thus alleviating fatty liver symptoms.
By improving lipid metabolism through AMPK activation and inhibition of fatty acid synthase, MF alleviates hepatic lipotoxicity and steatosis, thereby establishing a metabolic link between its systemic lipid-regulatory actions and liver protection.
8.3. Steatohepatitis
The modeling method for steatohepatitis is often alcohol gavage combined with high-fat diet-treated animals [81,82]. MF not only regulates lipid metabolism and reduces the accumulation of triglycerides and free fatty acids in the liver at this stage, but also reduces the level of inflammatory factors by inhibiting the inflammatory signaling pathway, such as NF-κB, to reduce the inflammatory injury of hepatocytes and to improve liver function [83].
8.4. Liver Fibrosis
Hepatic fibrosis models are mostly induced by repeated intraperitoneal injections of CCl4. The mechanism of hepatic fibrosis treatment with MF is more complex. On the one hand, it inhibits the activation and proliferation of hepatic stellate cells by inhibiting the TGF-β1/Smad pathway and reducing the synthesis and deposition of extracellular matrix. On the other hand, MF can target the HSP27-mediated JAK2/STAT3 and TGF-β1/Smad pathways, preventing the hepatocyte epithelial–mesenchymal transition, maintaining the normal morphology and function of hepatocytes [84,85]. In addition, MF can activate Nrf2, protect DNase 2 abundance, prevent inflammatory reactions triggered by cytoplasmic mtDNA accumulation, and thus reduce the degree of liver fibrosis [86].
8.5. Liver Cirrhosis
Cirrhosis modeling can be done by long-term induction of CCl4 and bile duct ligation combined with infection [87,88]. MF plays a therapeutic role in cirrhosis by regulating the metabolic function of the liver, improving the microcirculation of hepatic tissues, promoting the regeneration of hepatocytes, and inhibiting the process of inflammation and fibrosis.
8.6. Liver Cancer
In liver cancer research, diethylnitrosamine is commonly used to induce rat liver cancer model. MF has the effect of inhibiting the proliferation of hepatocellular carcinoma cells and inducing apoptosis, which can regulate cell cycle-related proteins and block the progression of the cancer cell cycle. Meanwhile, it inhibits the migration and invasive ability of cancer cells and down-regulates the expression of related proteins, such as MMP-9. It can also alleviate the damage of hepatocellular carcinoma cells on the liver by altering the pathways of oxidative stress and apoptosis [87,89].
In summary, MF has demonstrated multi-pathway and multi-target therapeutic potentials in all stages of liver disease, providing a new direction and hope for the treatment of liver disease, but most of the studies are still in the stage of animal experiments, and its wide application in the clinic requires further in-depth research and validation (Table 2 and Figure 10).

Table 2.
The pharmacological effects and mechanisms of MF in different stages of liver disease.
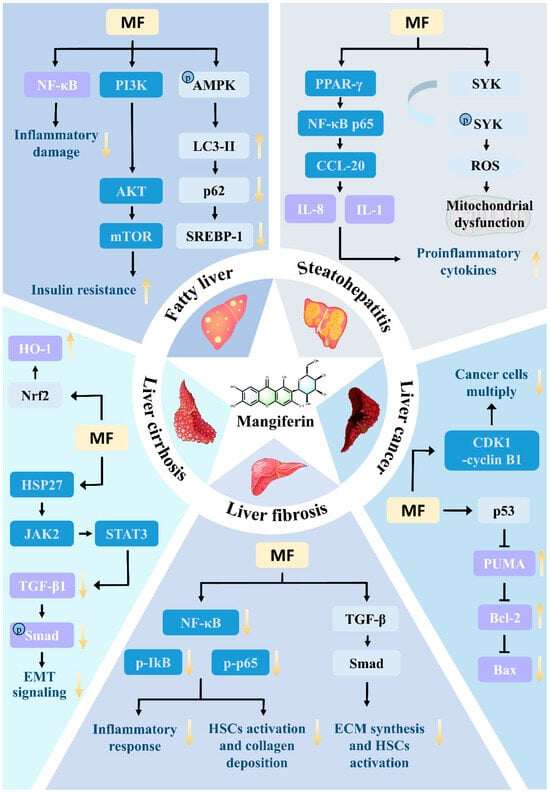
Figure 10.
Mechanism of mangiferin in treating liver diseases.
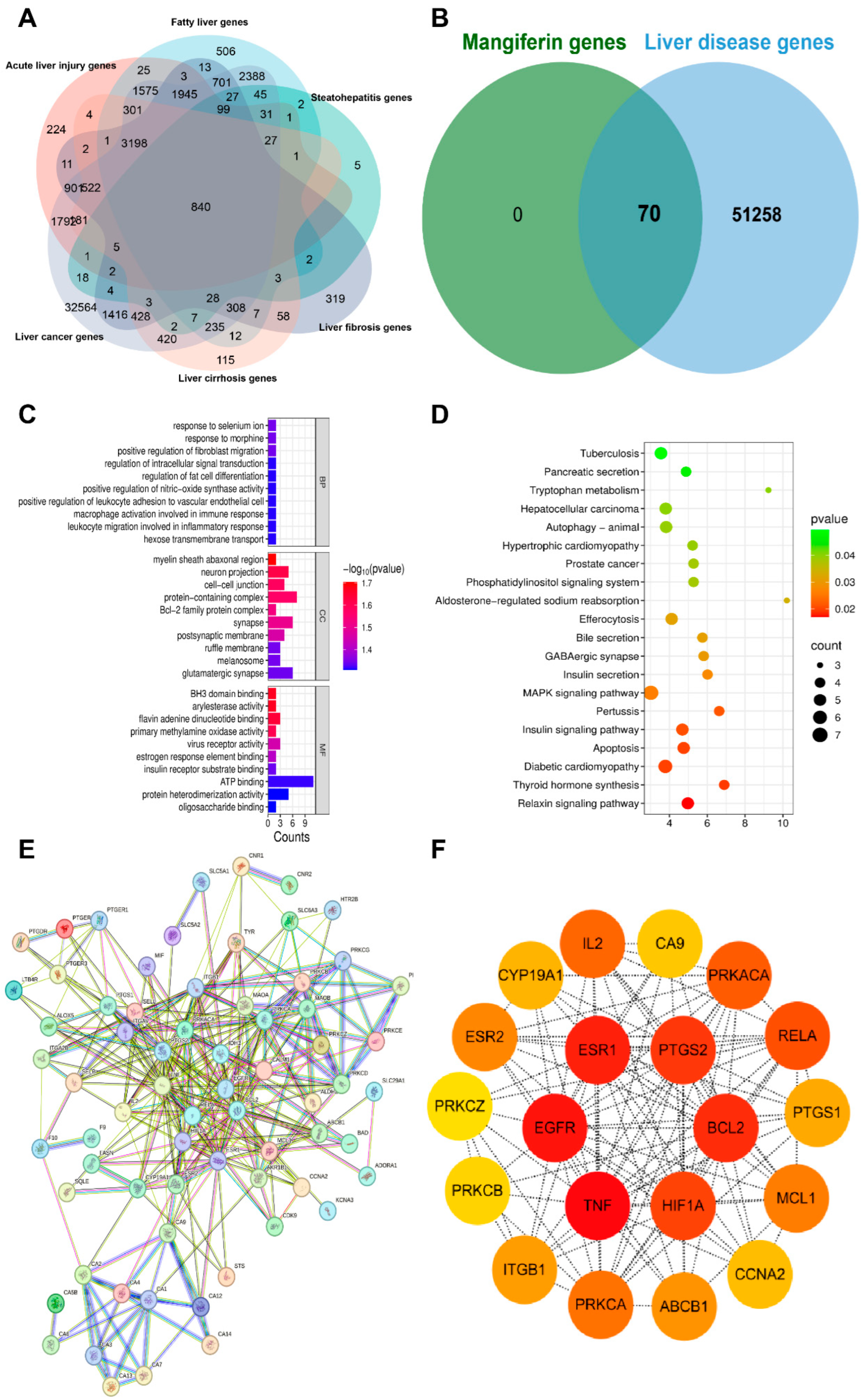
9. Network Pharmacology Analysis of MF
9.1. Collection Targets of Liver Disease Genes
By using the online platform Draw Venn Diagram to find the intersection between the screened ingredient targets and disease targets, and plotting a Venn diagram, we obtained 70 targets for the therapeutic effect of MF in liver disease genes (Figure 11A,B).
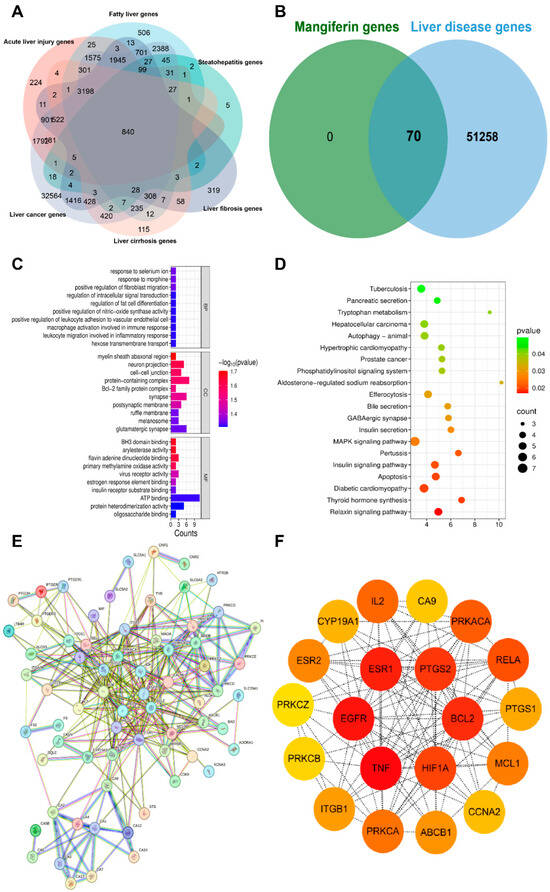
Figure 11.
(A). Venn diagram of liver diseases. (B). Venn diagram of liver disease targets and mangiferin therapeutic targets. (C,D). KEGG and GO Enrichment Analysis Plots (E,F). Protein–protein interaction in network of Targets.
9.2. GO and KEGG Pathway Enrichment Analysis
The findings from the enrichment analysis revealed a total of 183 BPs, 46 CCs, 49 MFs, and 112 KEGG pathways, with a significance level of p < 0.01. The illustration presents enriched GO, KEGG categories and component-target-pathway. Molecular functions encompass various activities such as oligosaccharide binding, protein heterodimerization activity, and ATP binding, among others. The cellular components identified glutamatergic synapse, ruffle membrane, and melanosome. Additionally, the biological processes involve hexose transmembrane transport, positive regulation of leukocyte adhesion to vascular endothelial cell, and macrophage activation involved in immune response, among other functions. The twenty most prevalent KEGG pathways are presented, which include pathways related to tuberculosis, pancreatic secretion, tryptophan metabolism, hepatocellular carcinoma and autophagy-animal, among others (Figure 11C,D).
9.3. Protein–Protein Interaction (PPI) Network Construction
The potential targets of MF for the treatment of liver diseases were imported into the STRING database to obtain the PPI network, and the topological analysis showed that the PPI network contained 70 nodes and 301 edges. The data were imported into Cytoscape 3.8.0 software, and the topological analysis was performed by using CytoNCA plug-in in Cytoscape 3.8.0 software, and 20 core targets were screened by using the median of the degree value as the standard, including ESR1, PTGS2, BCL2, HIF1A, TNF, EGFR, IL2, PRKACA, RELA, PRKCA and other core targets, of which the top six targets were TNF, EGFR, ESR1, BCL2, PTGS2 and HIF1A (Figure 11E,F).
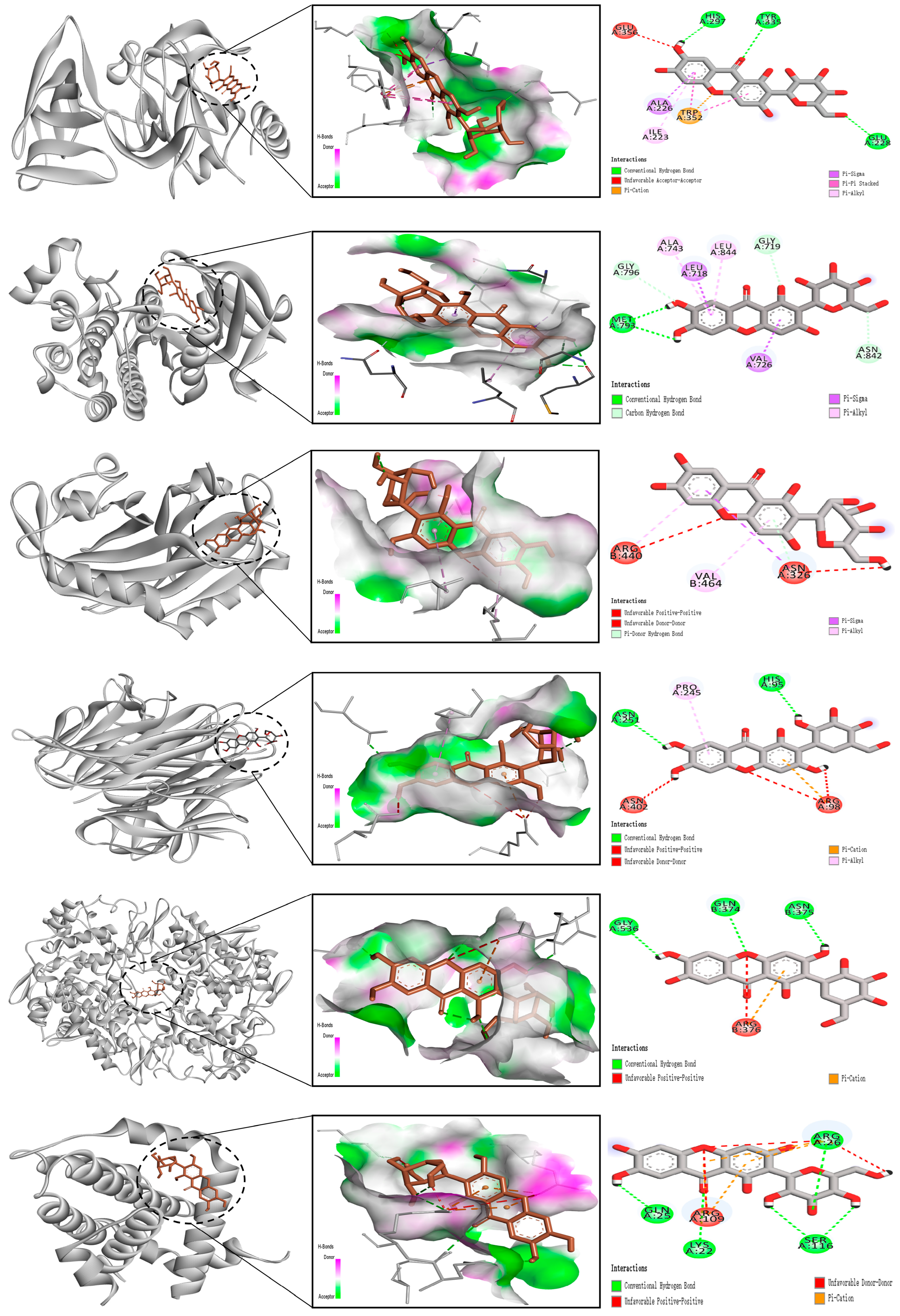
9.4. Molecular Docking Analysis
The receptor proteins were ESR1 (3cbp), PTGS2 (3poz), BCL2 (4h6j), HIF1A (4zch), TNF (5f19), and EGFR (8hts), and their 3D structure files were downloaded from the PDB database. PyMOL 2.3.0 software was used to check the protein structure for docking. The ligand small molecule is MF. Employ Auto Dock Vina (version 1.1.2) to perform docking of the compounds with the target. MF forms hydrogen bonds with the HIS, TYR, GLU, TRP, ILE, and ALA amino acid residues in ESR1, with bond lengths of 297, 335, 228, 352, 223, 226, and 356. MF forms hydrogen bonds with the ALA, LEU, GLY, ASN, VAL, and MET amino acid residues in PTGS2, with bond lengths of 743, 718, 844, 719, 842, 726, 793, and 796. MF forms hydrogen bonds with the ARG, VAL, and ASN amino acid residues in BCL2, with bond lengths of 440, 464, and 326. MF forms hydrogen bonds with the ASN, PRO, HIS, and ARG amino acid residues in HIF1A, with bond lengths of 251, 245, 95, 98, and 402. MF forms hydrogen bonds with the GLY, GLN, ASN, and ARG amino acid residues in TNF, with bond lengths of 536, 374, 375, and 376. MF forms hydrogen bonds with the ARG, SER, LYS, ARG, and GLN amino acid residues in EGFR, with bond lengths of 26, 116, 22, 109, and 25 (Figure 12).
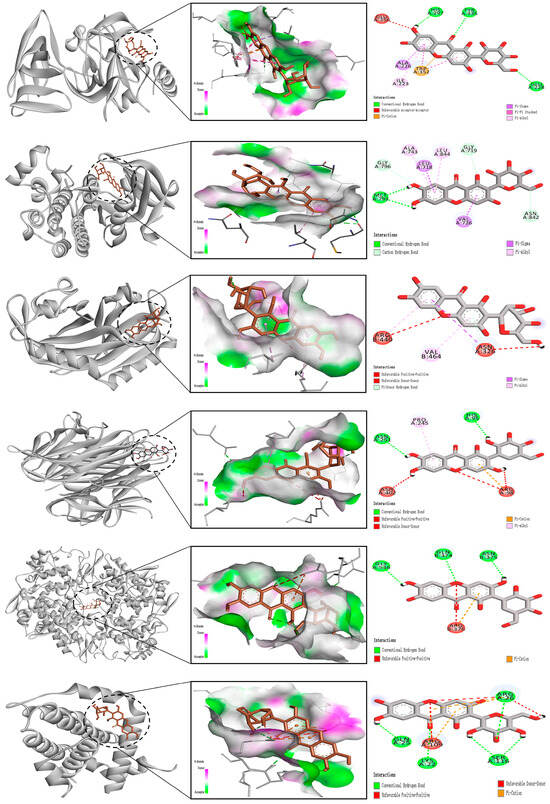
Figure 12.
Molecular docking diagram of mangiferin with key liver disease targets (ESR1, PTGS2, BCL2, HIF1A, TNF, EGFR).
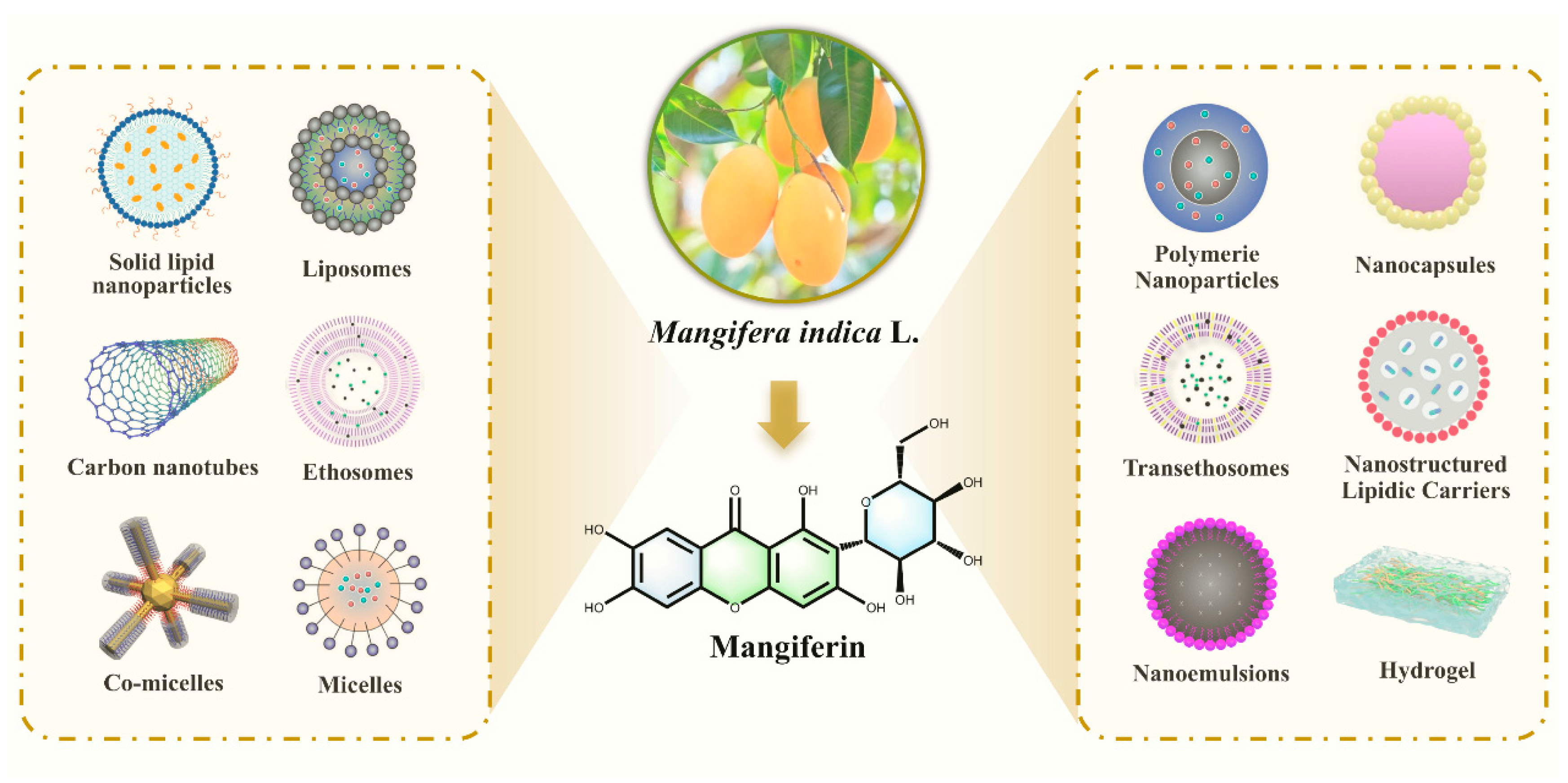
10. Study on the Bioavailability Enhancement Strategy of MF and Its Targeted Therapeutic Mechanism
MF exhibits limited solubility in water, which significantly contributes to its low oral bioavailability. Specifically, MF is described as being sparingly soluble in water (as well as in methanol), while it is insoluble in non-polar solvents such as diethyl ether, acetone, and n-hexane. This poor aqueous solubility, combined with its stability as a C-glycoside that resists hydrolysis in the gastrointestinal tract, limits its absorption in the small intestine. As a result, when MF is consumed orally, only a small fraction is absorbed via passive diffusion, leading to low systemic bioavailability. To address this issue, various strategies such as structural modification, nano/micro-encapsulation, and the use of solubility-enhancing carriers have been explored to improve its water solubility and overall bioavailability [41].
Due to the poor water solubility of MF, its bioavailability in the human body is also significantly limited. The oral bioavailability of MF in humans is very low, which is a major limitation for its efficacy. In a clinical study involving healthy male Chinese volunteers, a single high oral dose of 0.9 g of MF resulted in a maximum plasma concentration (Cmax) of only 38.64 ng/mL, which was reached after about 1 h (Tmax). The mean residence time (MRT) and elimination half-time (t1/2) were 13.87 h and 7.85 h, respectively. The very low plasma concentration achieved from a high dose clearly demonstrates the poor systemic availability of MF in humans [41].
This low bioavailability is attributed to its poor solubility, passive diffusion-based absorption in the intestine, and significant hepatic first-pass metabolism. Consequently, the biological effects observed after oral intake are likely due to its metabolites (such as norathyriol) produced by the gut microbiota, which have higher bioavailability, rather than the parent MF molecule itself.
10.1. New Dosage Form Development: Multimodal Carrier Systems Reshape Drug Delivery Characteristics
The new dosage form development systematically improves the solubility, membrane permeability and in vivo distribution characteristics of MF through the synergistic design of nanotechnology, colloidal carriers and extended release systems [90,91,92,93]. Nanoparticles based on amphiphilic polymers are formed into a core–shell structure by the method of complex emulsion-solvent evaporation, encapsulating the drug in a hydrophobic core, with an outer hydrophilic coating avoiding the body’s elimination, which improves the solubility by 1.79-fold, the oil-water partition coefficient by 2.04-fold, the rate of dissolution by 1.48-fold compared with that of active pharmaceutical ingredients (API), and significantly extends the in vivo residence time, with a relative bioavailability of 162.0-fold [94,95,96]. Solid dispersion technology utilizes water-soluble carriers to highly disperse the drug in an amorphous state, destroying the crystalline structure, increasing solubility by a maximum of 633 times, and increasing the cumulative release rate from 30.5% to 76.1% within 5 min. It can also reduce the contact of intestinal bacteria and slow down the metabolic degradation through the hydrogen bonding effect between carrier molecules [97,98,99]. Lipid-based carriers solubilize hydrophobic drugs with the help of phospholipid bilayers or self-assembly properties to optimize the transmembrane permeation efficiency, among which, the self-microemulsion drug delivery system increases the peak concentration by 7.7-fold and shortens the time to peak to 0.358 h, which significantly improves the oral absorption kinetics [100,101,102,103]. In addition, the porous microspheres and mesoporous silica nanoparticles control the drug release through the three-dimensional pore structure and delay the intestinal degradation. The residual concentration of the drug at 4 h is more than three times that of the raw material drug, which provides the carrier basis for the long-lasting delivery [104,105] (Figure 13).
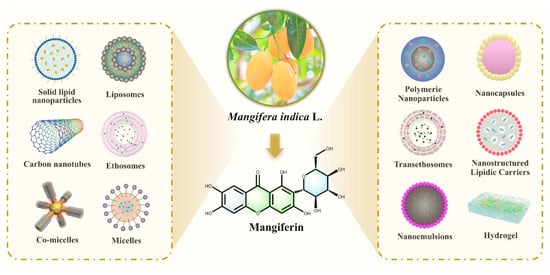
Figure 13.
Advanced delivery systems for mangiferin.
10.2. Structural Modification: Target Potentiation and Hepatic Injury Therapeutic Mechanism of MF Sodium Salt
The structural modification optimizes the physicochemical properties of MF through chemical modification, in which the sodium salt form significantly enhances the water solubility through phenolic hydroxyl salt formation, increasing the solubility from 0.123 mg/mL to more than 1.2 mg/mL, and at the same time regulates the molecular polarity to promote transmembrane transport and target enrichment in liver tissues. In the treatment of alcoholic liver injury, MF sodium salt can regulate the activity of key enzymes of alcohol metabolism, inhibit the over-activation of ethanol dehydrogenase and the accumulation of acetaldehyde, reduce the oxidative stress damage in the liver, lower the level of serum alanine aminotransferase and aspartate aminotransferase. Meanwhile, it enhances the antioxidant reserve of glutathione, inhibits the expression of inflammatory factors, and alleviates the lipid peroxidation of the hepatic tissues and the deposition of collagen fibers [106]. At the pharmacokinetic level, the negative charge property of sodium salt enhances the binding with anion receptor of liver cell membrane, so that the drug concentration in liver tissue reaches the peak within 1 h, which is 2.4 times higher than that of API; the plasma protein binding rate is increased from 65% to 82%, the circulation time is prolonged, the first-pass metabolism is reduced, and the clearance rate is reduced by 1.61 times, which significantly widens the therapeutic window. Mechanistic studies showed that the modified form promoted hepatocyte repair by regulating the glycerophospholipid metabolic pathway, inhibiting pro-inflammatory signaling, and reducing the degree of fibrosis by 50% in the CCl4-induced chronic liver injury model, demonstrating the advantages of structural modification in enhancing bioavailability while targeting and protecting against liver injury [55] (Figure 14).
Figure 14.
Molecular mechanism of mangiferin sodium salt against alcoholic fatty liver disease.
10.3. Biotransformation: Bacterial Colony Intervention and Metabolic Pathway Modulation to Enhance Drug Stability
At the biotransformation level, the C-glucosidic bond of MF is easily hydrolyzed by intestinal anaerobic flora, resulting in a significant first-pass effect, so the dosage form design can intervene in this process through physical barriers and biochemical modulation [107]. The amorphous dispersion and spatial site-blocking effect of solid dispersions and nanoparticles reduce the contact area between the drug and glycosidase, which reduces the metabolism rate by 40%. The concentration of unmetabolized drug in 4 h is 2 times higher than that of API, which prolongs the intestinal retention time. Phospholipid complex with surface-modified nanoparticles enhances the transmembrane transport efficiency by 1.8-fold by inhibiting the activity of intestinal P-glycoprotein efflux pumps, reducing the reverse drug excretion. The slow-release properties of microspheres and lipid carriers control the release rate of the drug, so that the metabolite norcoronarin is continuously generated, exerting synergistic antioxidant and anti-inflammatory effects. The concentration of active metabolites in liver tissue is increased 3-fold compared with that of the free drug, thus prolonging the duration of action. In addition, the carrier system indirectly protects the structural integrity of the drug by targeting and regulating the composition of the intestinal flora and inhibiting the expression of degradative enzymes in dominant bacteria such as Mycobacterium spp. The proportion of the prototypic drug entering the circulation is increased by 35%, which circumvents the first-pass metabolism depletion and enhances the bioavailability. By intervening in the key link of biotransformation, this strategy significantly enhances the stability of the drug in the gastrointestinal tract and liver without changing its molecular structure, providing an optimized pathway at the metabolic level for the development of oral formulations.
11. Future Perspectives
MF, a nutritional supplement widely distributed in various fruits, vegetables, and herbs, has garnered considerable attention for its remarkable antioxidative properties and therapeutic potential. As a potent bioactive compound, MF plays a crucial role in alleviating oxidative stress, a key contributor to the pathogenesis of many diseases, including liver disorders. Its strong antioxidant capabilities not only protect against oxidative damage but also promote liver health by mitigating lipid peroxidation and modulating inflammatory pathways.
While MF shows promise in preventing and treating liver diseases such as fatty liver and fibrosis, the therapeutic applications of MF are still constrained by its low bioavailability and poor solubility. Current strategies focus on enhancing its pharmacokinetic profile through structural modifications and novel delivery systems, which will facilitate its clinical application.
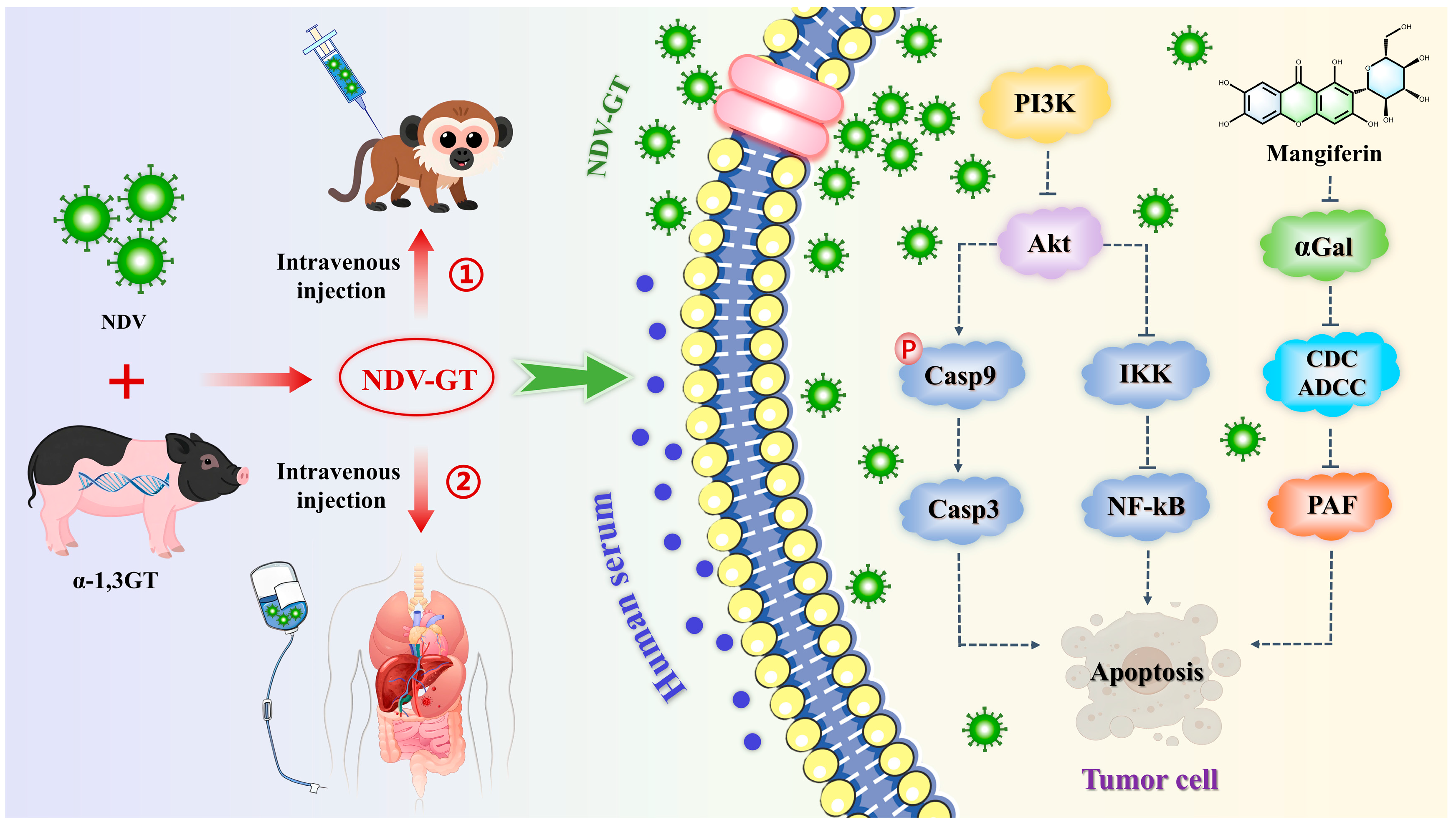
Hepatocellular carcinoma, a highly prevalent and poorly prognostic malignant tumor worldwide, remains primarily treated through surgical resection, liver transplantation, and systemic therapy. Liver transplantation is a critical means for advanced Hepatocellular carcinoma patients to achieve long-term survival. However, organ donor shortages, postoperative immune rejection reactions, and the risk of tumor recurrence significantly limit its widespread application [108,109,110]. Xenotransplantation offers a potential solution to the donor shortage, but the α1,3-galactosyl epitope triggers an ultra-acute rejection reaction mediated by the recipient’s natural anti-α1,3-galactosyl antibodies, leading to rapid graft necrosis [111]. To address these challenges, researchers have inserted the pig-derived α1,3-galactosyl transferase gene into Newcastle disease virus (NDV) to construct a recombinant oncolytic virus, Newcastle disease virus-pig-derived α1,3-galactosyl transferase gene. This virus selectively infects tumor cells and expresses the α1,3-galactosyl epitope, activating antibody-dependent cellular cytotoxicity mediated by anti-α1,3-galactosyl epitope antibodies, antibody-dependent cytolytic activity, and platelet-activating factor-induced tumor vascular thrombosis, as well as synergistically promoting CD4+/CD8+ T cell infiltration and other immune cascade reactions. This approach induced tumor regression in a CRISPR-mediated cynomolgus monkey hepatocellular carcinoma model and achieved a disease control rate of 90.00% in a clinical study involving 20 patients with refractory cancers, including hepatocellular carcinoma, with no severe adverse reactions. This technology leverages the immune mechanisms of hyperacute rejection, offering a novel approach for the clinical translation of oncolytic virus therapy and the regulation of xenograft rejection [112,113] (Figure 15). Future research may focus on optimizing viral vector design, exploring combination therapy with immune checkpoint inhibitors, and expanding indications. Further validation of long-term safety and immune memory effects is needed. Based on this, MF is increasingly being recognized for its potential role in regulating allograft rejection reactions. Studies have shown that MF can mitigate immune rejection reactions by inhibiting T cell activation, downregulating the secretion of pro-inflammatory cytokines, and blocking the activation of the classical complement pathway. In animal models, MF significantly reduces the infiltration levels of CD4+/CD8+ T cells in acute rejection reactions and inhibits antigen presentation by regulating the maturity of dendritic cells. For the hyperacute rejection response specific to xenotransplantation, MF may delay thrombosis formation in graft vessels by inhibiting the production of anti-α1,3-galactoside antibodies and the release of complement components C3a and C5a (Figure 15). However, current studies are primarily limited to in vitro experiments and rodent animal models [114,115,116]. The efficacy and pharmacokinetic characteristics of MF in non-human primate xenotransplantation models require further validation, particularly regarding its inhibitory mechanism against complement-dependent cytotoxicity mediated by natural antibodies and synergistic strategies when combined with immunosuppressive agents. These areas will become key research directions for overcoming the immune barriers in xenotransplantation.
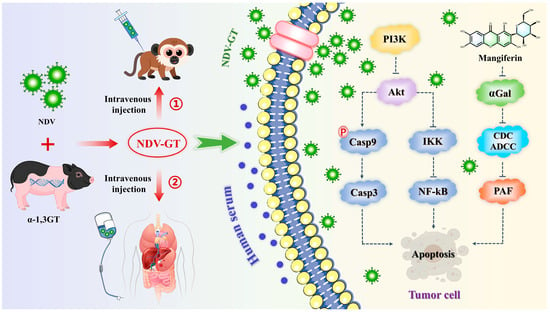
Figure 15.
Molecular mechanism of NDV-GT and mangiferin in the treatment of hepatocellular carcinoma (αGal: alpha-galactosidase, CDC: complement-mediated cytolysis, ADCC: antibody-dependent cell-mediated cytolysis, PAF: platelet-activating factor).
Under the backdrop of the deep integration of precision medicine and green pharmaceutical concepts, research on MF for liver disease treatment urgently needs to break away from traditional perspectives and expand into multidimensional interdisciplinary fields. Regarding the regulation mechanism of the gut-liver axis, given the central role of the gut microbiota-bile acid metabolism axis in the onset and progression of liver diseases, it is imperative to elucidate the molecular target network through which MF regulates the gut barrier function, inhibits the colonization of pathogenic bacteria, and regulates short-chain fatty acid and secondary bile acid metabolic pathways, particularly its bidirectional regulatory mechanism on the FXR/TGR5 signaling pathway and intestinal immune cells. This may reveal the new pharmacological basis for MF’s “gut-liver co-treatment” effect [117,118]. As a natural flavonoid glycoside compound, MF demonstrates potential anti-inflammatory, antioxidant, and anti-fibrotic effects in liver disease treatment. However, its limited water solubility and targeting capacity hinder clinical application. Based on structural modification research progress, introducing specific functional groups can significantly optimize its pharmacological properties. Hydrophilic groups: Drawing on the structural modification experience of sodium myricetin sulfate, introducing sulfonic acid groups or glycosylation modifications to the phenolic hydroxyl group of mango glycoside can improve its water solubility, promote liver-targeted delivery, and enhance regulation of lipid metabolism disorders in non-alcoholic fatty liver disease. Nitrogen-containing heterocycles: Similarly to the design of piperazine ring derivatives in the patent, such groups may enhance the binding affinity between the molecule and liver cell surface receptors, thereby improving the inhibitory efficiency of liver fibrosis-related pathways while enhancing transmembrane permeability. Alkoxy or halogen substituents: Introducing methoxy or fluorine atoms at specific positions on the thioxanthone skeleton can regulate molecular hydrophobicity and enhance interactions with inflammatory signaling pathways such as NF-κB, thereby inhibiting hepatic stellate cell activation and delaying the progression of liver fibrosis. In the field of microbial heterologous synthesis pathways, cutting-edge synthetic biology technologies can be leveraged to reconstruct the metabolic pathways of chassis cells via CRISPR-Cas9-mediated editing, overcoming the carbon flux allocation limitations of natural MF synthesis. Combined with directed evolution techniques to optimize the catalytic efficiency of key enzymes, this approach enables the construction of an efficient whole-cell biosynthetic system, providing a green manufacturing solution to address resource acquisition bottlenecks. The application prospects of organ-on-a-chip technology lie in constructing a 3D liver micro-organism model containing hepatic sinusoidal endothelial cells, hepatic stellate cells, and Kupffer cells based on microfluidic chips, combined with an intestinal epithelial chip to build a liver-intestine axis serial system. This can precisely simulate the in vivo pharmacokinetic characteristics of MF and the cascade reaction of intestinal toxins causing liver damage, particularly suitable for assessing its dynamic intervention effects on myofibroblast activation and extracellular matrix remodeling during the liver fibrosis process [119,120,121,122].
12. Conclusions
In conclusion, MF stands out as a promising natural antioxidant with significant therapeutic potential for liver diseases. Its antioxidant properties, coupled with ongoing research into its bioavailability and delivery mechanisms, will likely lead to the development of innovative therapies that can effectively address liver disease and beyond, demonstrating both scientific and translational value.
Author Contributions
J.X.: Conceptualization, Data curation, Writing—original draft, Writing—review and editing. S.S.: Resources, Supervision, Writing—review and editing. J.W.: Writing—review and editing. X.Y.: Data curation. Q.Z.: Validation. X.S.: Investigation. L.Z.: Investigation. T.W.: Data curation. N.F.: Supervision. J.S.: Writing—review and editing. Y.Z.: Funding acquisition, Resources, Writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This work was financially supported by the National Key R&D Program of China (No. 2023YFC3504400, 2023YFC3504402).
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| MF | Mangiferin |
| ALD | Alcoholic liver disease |
| MAFLD | Metabolism-associated fatty liver disease |
| Nrf2 | nuclear factor E2-related factor 2 |
| CCl4 | carbon tetrachloride |
| HO-1 | heme oxygenase-1 |
| PPI | Protein–protein interaction |
| API | active pharmaceutical ingredients |
| NDV | Newcastle disease virus |
References
- Zhao, C.; Pu, Z.; Gao, J.; Liu, C.; Xing, J.; Lang, W.; Chen, J.; Yuan, C.; Zhou, C. “Multiomics” Analyses Combined with Systems Pharmacology Reveal the Renoprotection of Mangiferin Monosodium Salt in Rats with Diabetic Nephropathy: Focus on Improvements in Renal Ferroptosis, Renal Inflammation, and Podocyte Insulin Resistance. J. Agric. Food. Chem. 2023, 71, 358–381. [Google Scholar] [CrossRef]
- Gendy, A.M.; El-Gazar, A.A.; Ragab, G.M.; Al-Mokaddem, A.K.; El-Haddad, A.E.; Selim, H.M.R.M.; Yousef, E.M.; Hamed, N.O.; Ibrahim, S.S.A. Possible Implication of Nrf2, PPAR-γ and MAPKs Signaling in the Protective Role of Mangiferin against Renal Ischemia/Reperfusion in Rats. Pharmaceuticals 2022, 16, 6. [Google Scholar] [CrossRef]
- Hu, X.; Zhao, W.; Deng, J.; Du, Z.; Zeng, X.; Zhou, B.; Hao, E. Mangiferin alleviates renal inflammatory injury in spontaneously hypertensive rats by inhibiting MCP-1/CCR2 signaling pathway. Chin. Herb. Med. 2023, 15, 556–563. [Google Scholar] [CrossRef]
- Chen, L.; Li, S.; Zhu, J.; You, A.; Huang, X.; Yi, X.; Xue, M. Mangiferin prevents myocardial infarction-induced apoptosis and heart failure in mice by activating the Sirt1/FoxO3a pathway. J. Cell. Mol. Med. 2021, 25, 2944–2955. [Google Scholar] [CrossRef] [PubMed]
- Lei, L.; Chen, C.Y.; Wang, Y.F.; Guo, Z.Y.; Zhang, Y. Mangiferin: A natural neuroprotective polyphenol with anti-inflammatory and anti-oxidant properties for depression. Prog. Neuropsychopharmacol. Biol. Psychiatry 2025, 139, 111401. [Google Scholar] [CrossRef]
- Tan, H.; Liang, D.; Lu, N.; Zhang, J.; Zhang, S.; Tan, G. Mangiferin attenuates lipopolysaccharide-induced neuronal injuries in primary cultured hippocampal neurons. Aging 2024, 16, 8645–8656. [Google Scholar] [CrossRef] [PubMed]
- Qin, F.; Zhang, M.; Wang, P.; Dai, Z.; Li, X.; Li, D.; Jing, L.; Qi, C.; Fan, H.; Qin, M.; et al. Transcriptome analysis reveals the anti-Parkinson’s activity of Mangiferin in zebrafish. Biomed. Pharmacother. 2024, 179, 117387. [Google Scholar] [CrossRef]
- Deng, X.; Lin, B.; Wang, F.; Xu, P.; Wang, N. Mangiferin attenuates osteoporosis by inhibiting osteoblastic ferroptosis through Keap1/Nrf2/SLC7A11/GPX4 pathway. Phytomedicine 2024, 124, 155282. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chen, M.; Li, Y.; Guo, Y.; Yu, Y.; Zhou, Z.; Lu, H.; Yao, S.; Wu, C.; Zhang, X.; et al. Mangiferin ameliorates polycystic ovary syndrome in rats by modulating insulin resistance, gut microbiota, and ovarian cell apoptosis. Front. Pharmacol. 2024, 15, 1457467. [Google Scholar] [CrossRef]
- Wang, M.; Liang, Y.; Chen, K.; Wang, M.; Long, X.; Liu, H.; Sun, Y.; He, B. The management of diabetes mellitus by mangiferin: Advances and prospects. Nanoscale 2022, 14, 2119–2135. [Google Scholar] [CrossRef]
- Kalligeros, M.; Henry, L.; Younossi, Z.M. Metabolic dysfunction-associated steatotic liver disease and its link to cancer. Metabolism 2024, 160, 156004. [Google Scholar] [CrossRef]
- Mak, L.Y.; Liu, K.; Chirapongsathorn, S.; Yew, K.C.; Tamaki, N.; Rajaram, R.B.; Panlilio, M.T.; Lui, R.; Lee, H.W.; Lai, J.C.; et al. Liver diseases and hepatocellular carcinoma in the Asia-Pacific region: Burden, trends, challenges and future directions. Nat. Rev. Gastroenterol. Hepatol. 2024, 21, 834–851. [Google Scholar] [CrossRef]
- Oliveira, B.G.; Costa, H.B.; Ventura, J.A.; Kondratyuk, T.P.; Barroso, M.E.S.; Correia, R.M.; Pimentel, E.F.; Pinto, F.E.; Endringer, D.C.; Romão, W. Chemical profile of mango (Mangifera indica L.) using electrospray ionisation mass spectrometry (ESI-MS). Food Chem. 2016, 204, 37–45. [Google Scholar] [CrossRef]
- Alañón, M.E.; Pimentel-Moral, S.; Arráez-Román, D.; Segura-Carretero, A. HPLC-DAD-Q-ToF-MS profiling of phenolic compounds from mango (Mangifera indica L.) seed kernel of different cultivars and maturation stages as a preliminary approach to determine functional and nutraceutical value. Food Chem. 2021, 337, 127764. [Google Scholar] [CrossRef] [PubMed]
- Heo, N.Y.; Kim, H. Epidemiology and updated management for autoimmune liver disease. Clin. Mol. Hepatol. 2023, 29, 194–196. [Google Scholar] [CrossRef] [PubMed]
- Newman, K.L.; Vélez, C.; Paul, S.; Radix, A.E.; Streed, C.G.; Targownik, L.E. Research Considerations in Digestive and Liver Disease in Transgender and Gender-Diverse Populations. Clin. Gastroenterol. Hepatol. 2023, 21, 2443–2449. [Google Scholar] [CrossRef] [PubMed]
- Paternostro, R.; Sieghart, W.; Trauner, M.; Pinter, M. Cancer and hepatic steatosis. ESMO 2021, 6, 100185. [Google Scholar] [CrossRef]
- Cao, G.; Jing, W.; Liu, J.; Liu, M. Countdown on hepatitis B elimination by 2030: The global burden of liver disease related to hepatitis B and association with socioeconomic status. Hepatol. Int. 2022, 16, 1282–1296. [Google Scholar] [CrossRef]
- Saha, S.; Sadhukhan, P.; Sil, P.C. Mangiferin: A xanthonoid with multipotent anti-inflammatory potential. Biofactors 2016, 42, 459–474. [Google Scholar] [CrossRef]
- Akkewar, A.S.; Mishra, K.A.; Sethi, K.K. Mangiferin: A natural bioactive immunomodulating glucosylxanthone with potential against cancer and rheumatoid arthritis. J. Biochem. Mol. Toxic. 2024, 38, e23765. [Google Scholar] [CrossRef]
- Zivković, J.; Kumar, K.A.; Rushendran, R.; Ilango, K.; Fahmy, N.M.; El-Nashar, H.A.S.; El-Shazly, M.; Ezzat, S.M.; Melgar-Lalanne, G.; Romero-Montero, A.; et al. Pharmacological properties of mangiferin: Bioavailability, mechanisms of action and clinical perspectives. Naunyn Schmiedebergs Arch. Pharmacol. 2024, 397, 763–781. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, X.Y.; Wang, S.J.; Li, Y.B. Research progress on pharmacological effects of mangiferin. Strait Pharm. J. 2019, 31, 31–33. [Google Scholar]
- Sun, C.Y.; Xie, G.Y.; Qin, M.J. Research progress on distribution and pharmacological activities of mangiferin in plant kingdom. Chin. Wild Plant Resour. 2017, 36, 39–45+49. [Google Scholar]
- Fan, X.C.; Jiao, G.Y.; Zhang, F.; Han, J.; Chen, W.S. Research progress on pharmacodynamic effects of mangiferin. Acad. J. Nav. Med. Univ. 2024, 45, 219–226. [Google Scholar]
- Zhang, L.; Huang, C.; Fan, S. Mangiferin and organ fibrosis: A mini review. Biofactors 2021, 47, 59–68. [Google Scholar] [CrossRef]
- Mittal, S.; Iqubal, M.K.; Iqbal, B.; Gupta, M.M.; Ali, J.; Baboota, S. A pervasive scientific overview on mangiferin in the prevention and treatment of various diseases with preclinical and clinical updates. J. Complementary Integr. Med. 2020, 18, 9–21. [Google Scholar] [CrossRef]
- Li, L.; Dong, Y.; Liu, X.; Wang, M. Mangiferin for the Management of Liver Diseases: A Review. Foods 2023, 12, 2469. [Google Scholar] [CrossRef] [PubMed]
- Dutta, T.; Das, T.; Gopalakrishnan, A.V.; Saha, S.C.; Ghorai, M.; Nandy, S.; Kumar, M.; Radha; Ghosh, A.; Mukerjee, N.; et al. Mangiferin: The miraculous xanthone with diverse pharmacological properties. Naunyn Schmiedebergs Arch. Pharmacol. 2023, 396, 851–863. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.Q.; Zhen, H.S.; Xiong, W.N.; Ping, J.J.; Qiong, D.M. Determination of mangiferin in mango peel by RP-HPLC. Chin. Tradit. Herb. Drugs 2006, 37, 1262–1263. [Google Scholar] [CrossRef]
- Huang, H.B.; Li, X.J.; Liang, Q.Y. Determination of mangiferin in mango leaves by RP-HPLC. China J. Chin. Mater. Med. 2003, 28, 49–51. [Google Scholar]
- Zhu, F.R.; Wang, S.X.; Mao, D.Y.; Ao, W.; Qing, L.W. Optimization of ultrasound-assisted extraction process of mangiferin from mango kernel. Sci. Technol. Food Ind. 2024, 45, 161–167. [Google Scholar]
- Liu, C.K.; Yang, L.; He, L.F. Determination of total flavonoids and mangiferin content in mango pulp. Hubei Agric. Sci. 2020, 59, 138–140+144. [Google Scholar]
- Chen, M.M.; Yang, C.Y.; Wan, Y.Y.; Chen, X.; Guo, M.R.; Du, M.X. Determination of mangiferin in Anemarrhena asphodeloides by HPLC. Shandong Chem. Ind. 2022, 51, 115–119+122. [Google Scholar]
- Wu, J.Y.; Zhang, W.G.; Lang, Y.F.; Huang, Z.C.; Yang, W.L.; Yang, J.; Chen, H.F. Chemical composition analysis of mango kernel based on UPLC-Q-TOF-MS/MS. Nat. Prod. Res. Dev. 2023, 35, 949–965. [Google Scholar]
- Zou, D.F.; Gao, Y.; Zhang, K.F. Determination of mangiferin content in leaves of different mango varieties. J. Anhui Agric. Sci. 2010, 38, 2947–2948. [Google Scholar]
- Deng, J.G.; Feng, X.; Wang, Q.; Tan, J.P.; Ye, Y. Comparative study on mangiferin content in mango leaves from different origins and varieties. Chin. Tradit. Pat. Med. 2006, 28, 1755–1756. [Google Scholar] [CrossRef]
- Yang, K.S.; Zhao, H.Y.; Gu, C.Z.; Li, Z.H.; Lu, J.; Cao, J.X. Determination of mangiferin in different mango varieties from Yunnan by HPLC. Sci. Technol. Food Ind. 2014, 35, 61–63+67. [Google Scholar]
- Deng, H.M.; Chen, Y.J.; Lin, Z.H.; Zheng, L.W.; Sun, Z.F.; Guo, W.F. Separation, purification and identification of mangiferin. Agric. Prod. Process. 2018, 17, 1–4+9. [Google Scholar] [CrossRef]
- Ma, Y.L.; Li, X.N.; Qian, D.M.; Tan, J.L. Extraction of mangiferin and its antioxidant activity. Shandong Chem. Ind. 2020, 49, 24–26. [Google Scholar]
- Castro-Muñoz, R.; Cabezas, R.; Plata-Gryl, M. Mangiferin: A comprehensive review on its extraction, purification and uses in food systems. Adv. Colloid Interface Sci. 2024, 329, 103188. [Google Scholar] [CrossRef]
- Mei, S.; Perumal, M.; Battino, M.; Kitts, D.D.; Xiao, J.; Ma, H.; Chen, X. Mangiferin: A review of dietary sources, absorption, metabolism, bioavailability, and safety. Crit. Rev. Food Sci. 2023, 63, 3046–3064. [Google Scholar] [CrossRef] [PubMed]
- Rauf, A.; Imran, M.; Patel, S. Mangiferin: A phytochemical with panacea potential. Biomed. Pharmacother. 2017, 96, 1562–1564. [Google Scholar] [CrossRef]
- Ma, X.H.; Wei, Y.L.; Li, G.Z. Research progress of mango food products. Agric. Prod. Process. 2024, 23, 108–111. [Google Scholar] [CrossRef]
- López-Cárdenas, F.G. Advances in Mangiferin: Biosynthetic Pathways, Bioavailability and Bioactivity. In Handbook of Dietary Flavonoids; Springer International Publishing: Cham, Switzerland, 2023; pp. 1–37. [Google Scholar]
- Guan, L.; Yang, C.Q.; Li, R.J.; Zhao, H.R.; Li, W.Z. Research progress on mangiferin. Contemp. Chem. Ind. 2021, 50, 478–481+486. [Google Scholar]
- Ehianeta, T.S.; Laval, S.; Yu, B. Bio- and chemical syntheses of mangiferin and congeners. Biofactors 2016, 42, 445–458. [Google Scholar] [CrossRef]
- Quillinan, A.J.; Scheinmann, F. Studies in the xanthone series. Part XII. A general synthesis of polyoxygenated xanthones from benzophenone precursors. J. Chem. Soc. Perkin Trans. I 1973, 1, 1329–1337. [Google Scholar] [CrossRef]
- Hu, L.; Hu, H.; Wu, W.; Chai, X.; Luo, J.; Wu, Q. Discovery of novel xanthone derivatives as xanthine oxidase inhibitors. Bioorgan. Med. Chem. Lett. 2011, 21, 4013–4015. [Google Scholar] [CrossRef]
- Qin, Q.X.; Yang, J.; Yang, B. A novel and efficient synthesis of norathyriol using Pd(II) as a catalyst. Res. Chem. Intermed. 2014, 40, 1633–1636. [Google Scholar] [CrossRef]
- Wu, Z.; Wei, G.; Lian, G.; Yu, B. Synthesis of mangiferin, isomangiferin, and homomangiferin. J. Org. Chem. 2010, 7, 5725–5728. [Google Scholar] [CrossRef]
- Liao, H.L. Isolation and Structure Modification of Mangiferin from Anemarrhena asphodeloides Bge. Master’s Thesis, Naval Medical University, Shanghai, China, 2005. [Google Scholar]
- Yang, X.L.; Liu, X.; Lan, C.; Nong, J.C.Z.; Pan, L.L.; Jiao, W. Effects of mangiferin on proliferation, apoptosis and cycle of nasopharyngeal carcinoma CNE2 cells. Shandong Med. J. 2009, 49, 23–24. [Google Scholar]
- Huang, X.O.; Deng, J.G.; Chen, Z. Protective effect of mangiferin dropping pills on chronic liver injury in rats. Front. Pharm. Sci. 2009, 12, 701–704. [Google Scholar]
- Deng, J.G.; Yang, K.; Yan, L.; Guo, L.C.; Tang, H.Q. Effect of mangiferin on T lymphocyte proliferation in immunosuppressed mice. Pharmacol. Clin. Chin. Mater. Med. 2007, 23, 64–65. [Google Scholar]
- Pu, Z.J. Improving Effect of Mangiferin Sodium Salt on Alcoholic Hepatitis and Regulatory Mechanism of Metabolomics. Master’s Thesis, Hebei University, Baoding, China, 2023. [Google Scholar] [CrossRef]
- Tang, T. Inhibitory Study of Mangiferin Derivatives on 3t3-l1adipocytes. Master’s Thesis, Jiangsu University, Zhenjiang, China, 2024. [Google Scholar] [CrossRef]
- Correia-da-Silva, M.; Sousa, E.; Duarte, B.; Marques, F.; Cunha-Ribeiro, L.M.; Pinto, M.M. Polysulfated xanthones: Multipathway development of a new generation of dual anticoagulant/antiplatelet agents. J. Med. Chem. 2011, 15, 5373–5384. [Google Scholar] [CrossRef]
- Li, X.J. Chemical Synthesis and Pharmacological Activity Study of Mangiferin Esterified Derivatives. Ph.D. Thesis, Guangxi Medical University, Nanning, China, 2012. [Google Scholar] [CrossRef]
- Singh, S.K.; Sinha, S.K.; Prasad, S.K.; Kumar, R.; Bithu, B.S.; Kumar, S.S.; Singh, P. Synthesis and evaluation of novel analogues of mangiferin as potent antipyretic. Aaian Pac. J. Trop. Med. 2011, 11, 866–869. [Google Scholar] [CrossRef]
- Liu, H.; Tang, K.Y.; Sun, Z.; Jian, L.; Li, Z.; Wu, B.; Huang, C. Structure elucidation of in vivo and in vitro metabolites of mangiferin. J. Pharm. Biomed. Anal. 2011, 55, 1075–1082. [Google Scholar] [CrossRef]
- Zhou, H.; Song, S.; Lan, X.; Li, Y.; Yuan, X.; Yang, J.; Li, M.; Cao, T.; Zhang, J. Comprehensive profiling of mangiferin metabolites in vivo and in vitro based on the “drug metabolite clusters” analytical strategy. ACS Omega 2023, 8, 9934–9946. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.G.; Zhao, Y.; Yang, S.Y.; Fang, L.H.; Song, J.K.; Lv, Y.; Du, G.H. Pharmacokinetics of three kinds of mangiferin polymorphs in rats. Her. Med. 2019, 38, 208–212. [Google Scholar]
- Fomenko, E.V.; Chi, Y. Mangiferin modulation of metabolism and metabolic syndrome. Biofactors 2016, 42, 492–503. [Google Scholar] [CrossRef] [PubMed]
- Tian, X.; Gao, Y.; Xu, Z.; Lian, S.; Ma, Y.; Guo, X.; Hu, P.; Li, Z.; Huang, C. Pharmacokinetics of mangiferin and its metabolite-Norathyriol, Part 1: Systemic evaluation of hepatic first-pass effect in vitro and in vivo. Biofactors 2016, 42, 533–544. [Google Scholar] [CrossRef]
- Wei, Y.; Wu, Y.W.; Zhao, D.; Xu, Y.Y.; Xu, M.J.; Hai, X.D. Hypoglycemic activity and in vivo pharmacokinetics of mangiferin. J. Chongqing Med. Univ. 2022, 47, 387–392. [Google Scholar]
- Li, J.; Liu, M.; Yu, H.; Wang, W.; Han, L.; Chen, Q.; Ruan, J.; Wen, S.; Zhang, Y.; Wang, T. Mangiferin Improves Hepatic Lipid Metabolism Mainly Through Its Metabolite-Norathyriol by Modulating SIRT-1/AMPK/SREBP-1c Signaling. Front. Pharmacol. 2018, 9, 201. [Google Scholar] [CrossRef]
- Huang, H.X.; Tan, Z.Y.; Deng, J.G.; Liang, Q.Y.; Nong, Y.M.; Song, N.M. In vitro metabolic transformation of mangiferin by human intestinal flora. China J. Chin. Mater. Med. 2011, 36, 443–445. [Google Scholar]
- Sarwar, A.R.; Iqbal, F.M.; Jamil, M.A.; Abbas, K. Nanocrystals of Mangiferin Using Design Expert: Preparation, Characterization, and Pharmacokinetic Evaluation. Molecules 2023, 28, 5918. [Google Scholar] [CrossRef]
- Sun, X.G.; Zhang, J.; Pang, X.; Liang, Q.Y.; Nong, Y.M.; Song, N.M. Research progress on metabolic pathways of natural flavonoid glycosides. Chin. Tradit. Herb. Drugs 2020, 51, 3078–3089. [Google Scholar]
- Li, M.; Wu, C.; Guo, H.; Chu, C.; Hu, M.; Zhou, C. Mangiferin improves hepatic damage-associated molecular patterns, lipid metabolic disorder and mitochondrial dysfunction in alcohol hepatitis rats. Food Funct. 2019, 10, 3514–3534. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Liu, C.; Yin, L.; Huang, C.; Fan, S. Mangiferin relieves CCl4-induced liver fibrosis in mice. Sci. Rep. 2023, 13, 4172. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Zhen, Y.; Chen, X.; Cao, L.; Song, J.; Liu, X.; Wang, M. Mangiferin Protects DNase 2 Abundance via Nrf2 Activation to Prevent Cytosolic mtDNA Accumulation during Liver Injury. Mol. Nutr. Food Res. 2023, 67, e2200885. [Google Scholar] [CrossRef]
- Zhang, X.L.; Zhang, X.Y.; Ge, X.Q.; Liu, M.X. Mangiferin prevents hepatocyte epithelial-mesenchymal transition in liver fibrosis via targeting HSP27-mediated JAK2/STAT3 and TGF-β1/Smad pathway. Phytother. Res. 2022, 36, 4167–4182. [Google Scholar] [CrossRef]
- Yang, S.; Kuang, G.; Zhang, L.; Wu, S.; Zhao, Z.; Wang, B.; Yin, X.; Gong, X.; Wan, J. Mangiferin Attenuates LPS/D-GalN-Induced Acute Liver Injury by Promoting HO-1 in Kupffer Cells. Front. Immunol. 2020, 11, 285. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Jin, S.; Chen, W.; Yu, J.; Fang, P.; Zhou, G.; Li, J.; Jin, L.; Chen, Y.; Chen, P.; et al. Mangiferin alleviates endoplasmic reticulum stress in acute liver injury by regulating the miR-20a/miR-101a-Nrf2 axis. Biochem. J. 2020, 168, 365–374. [Google Scholar] [CrossRef]
- Pan, C.W.; Pan, Z.Z.; Hu, J.J.; Chen, W.L.; Zhou, G.Y.; Lin, W.; Jin, L.X.; Xu, C.L. Mangiferin alleviates lipopolysaccharide and D-galactosamine-induced acute liver injury by activating the Nrf2 pathway and inhibiting NLRP3 inflammasome activation. Eur. J. Pharmacol. 2016, 770, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Dong, M.; Li, L.; Li, G.; Song, J.; Liu, B.; Liu, X.; Wang, M. Mangiferin protects against alcoholic liver injury via suppression of inflammation-induced adipose hyperlipolysis. Food Funct. 2020, 11, 8837–8851. [Google Scholar] [CrossRef] [PubMed]
- Mi, K.; Huang, R. Mechanism of mangiferin on liver fibrosis in rats based on TGF-β/Smad signaling pathway. Sichuan Med. J. 2020, 41, 142–146. [Google Scholar]
- Shi, C.; Li, Y.; You, Z.; Tian, Y.; Zhu, X.; Xu, H.; Yang, M.; Zhang, Y.; Dong, R.; Quan, H.; et al. Mangiferin Ameliorates CCl4-Triggered Acute Liver Injury by Inhibiting Inflammatory Response and Oxidative Stress: Involving the Nrf2-ARE Pathway. J. Inflamm. Res. 2024, 17, 7081–7097. [Google Scholar] [CrossRef]
- Chu, C.; Zhao, Y.Y.; Zhou, C.Y. Protective Effect of Mangiferin on Alcoholic Hepatitis in Rats. Nat. Prod. Res. Dev. 2018, 30, 753–760. [Google Scholar]
- Chen, X.; Xia, X.D.; Tong, D.Y.; Che, D.B. Experimental Study on Mangiferin in Improving the Liver Function in Model Mice with Liver Injury. China Pharm. 2019, 28, 17–20. [Google Scholar]
- Chu, C. Experimental Study on Proteotive effects of Mangiferin on Alcoholic Liver Disease. Master’s Thesis, Hebei University, Baoding, China, 2018. [Google Scholar]
- Chowdhury, A.; Lu, J.; Zhang, R.; Nabila, J.; Gao, H.; Wan, Z.; Adelusi-Temitope, I.; Yin, X.; Sun, Y. Mangiferin ameliorates acetaminophen-induced hepatotoxicity through APAP-Cys and JNK modulation. Biomed. Pharmacother. 2019, 117, 109097. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Zhu, Y.Y.; Wang, L.; Teng, T.; Zhou, M.; Wang, S.G.; Tian, Y.Z.; Du, L.; Yin, X.X.; Sun, Y. Mangiferin ameliorates fatty liver via modulation of autophagy and inflammation in high-fat-diet induced mice. Biomed. Pharmacother. 2017, 96, 328–335. [Google Scholar] [CrossRef]
- Li, L.S. Mangiferin Protects Against Liver Injury Through Suppressing Cytosolic mtDNA Accumulation. Ph.D. Thesis, Hebei Normal University, Baoding, China, 2024. [Google Scholar]
- Xu, J.; Liu, X.J.; Lv, Q.Z.; Yu, H.; Cheng, W.G.; Ji, M.L. Protective effect of mangiferin on acute liver failure in mice. J. Xinxiang Med. Univ. 2020, 37, 327–331. [Google Scholar]
- Morozkina, S.N.; Nhung-Vu, T.H.; Generalova, Y.E.; Snetkov, P.P.; Uspenskaya, M.V. Mangiferin as New Potential Anti-Cancer Agent and Mangiferin-Integrated Polymer Systems-A Novel Research Direction. Biomolecules 2021, 11, 79. [Google Scholar] [CrossRef]
- Du, Z.C.; Deng, J.G.; Huang, H.X.; Liu, X.J.; Chen, L.; Li, H.W. Effect of Mango Leaf Extract on Acute Alcoholic Liver Injury in Mice. Chin. J. Exp. Tradit. Med. Formulae 2013, 19, 250–253. [Google Scholar]
- Toledo, R.C.L.; Brito, L.F.; Caetano, M.M.M.; Nakajima, V.M.; Da-Silva, B.P.; Soares, F.E.F.; Martino, H.S.D.; De-Queiroz, J.H. Acute treatment with Mangifera indica L. leaf extract attenuates liver inflammation in rats fed a cafeteria diet. Food Funct. 2019, 10, 4861–4867. [Google Scholar] [CrossRef]
- Yi, H.H. Preparation and Pharmacokinetics of mPEG-PLGA-Mangiferin Nanoparticles. Master’s Thesis, Northwest University, Xi’an, China, 2018. [Google Scholar]
- Han, D.D.; Chen, C.J.; Zhang, C.; Zhang, Y.; Tang, X. Determination of mangiferin in rat plasma by liquid–liquid extraction with UPLC-MS/MS. J. Pharm. Biomed. Anal. 2010, 51, 260–263. [Google Scholar] [CrossRef] [PubMed]
- Kammalla, A.K.; Ramasamy, M.K.; Inampudi, J.; Dubey, G.P.; Agrawal, A.; Kaliappan, I. Comparative Pharmacokinetic Study of Mangiferin After Oral Administration of Pure Mangiferin and US Patented Polyherbal Formulation to Rats. AAPS J. 2015, 16, 250–258. [Google Scholar] [CrossRef]
- Li, X.Y.; Ye, X.Q.; Si, J.R.; Si, N.Q. Biopharmaceutics Classification System and Formulation Strategies. J. Jilin Med. Univ. 2016, 37, 60–63. [Google Scholar]
- Barakat, S.; Nasr, M.; Ahmed, R.F.; Badawy, S.; Mortada, N. Recent formulation advances of mangiferin. Rev. Bras. Farmacogn. 2022, 32, 871–882. [Google Scholar] [CrossRef]
- Baghel, M.; Baghel, I.; Kumari, P.; Bharkatiya, M.; Joshi, G.; Sakure, K.; Badwaik, H. Nano-delivery Systems and Therapeutic Applications of Phytodrug Mangiferin. Appl. Biochem. Biotechnol. 2024, 196, 7429–7463. [Google Scholar] [CrossRef]
- Mu, X.H. Preparation of Mangiferin PLGA Porous Microspheres by Pickering Emulsion Template Method. Master’s Thesis, Guangxi University of Chinese Medicine, Nanning, China, 2017. [Google Scholar]
- Huang, H.X.; Liang, Q.Y.; Deng, J.G.; Nong, Y.M.; Wei, W.; Chen, W.W. Effect of different pharmaceutical excipients on Mangiferin Absorption and Transportation in Caco-2 Cell Model. J. Guangxi Univ. Chin. Med. 2014, 17, 60–62. [Google Scholar]
- Alkholifi, F.K.; Alam, A.; Foudah, A.I.; Yusufoglu, H.S. Phospholipid-Based Topical Nano-Hydrogel of Mangiferin: Enhanced Topical Delivery and Improved Dermatokinetics. Gels 2023, 9, 178. [Google Scholar] [CrossRef]
- Lv, D.X.; Yu, R.; Qu, Z.G.; Fan, M.S. Preparation and in vivopharmacokinetics of mangiferin solid lipid nanoparticles. Chin. Trad. Pat. Med. 2020, 42, 2835–2839. [Google Scholar]
- Xuan, X.Y.; Wang, Y.J.; Tian, H.; Pi, J.X.; Sun, T.Z.; Zhang, W.L. Study on Prescription of Self-microemulsifying Drug Delivery System of Mangiferin Phospholipid Complex. J. Chin. Med. Mater. 2012, 35, 1508–1511. [Google Scholar]
- Zheng, Y.; Wang, Y.J. Physicochemical property and percutaneous permeability in vitro of mangiferin liposomes. Drugs Clin. 2014, 29, 147–150. [Google Scholar]
- Xuan, X.Y.; Wang, Y.J.; Zhang, W.L.; Pi, J.X.; Zheng, Y.; Gao, X. Preparation of self-micro emulsifying drug delivery systems of mangiferin and its pharmacokinetic study in rats. Drug Eval. Res. 2013, 36, 166–170. [Google Scholar]
- Liu, M.; Liu, Y.; Ge, Y.; Zhong, Z.; Wang, Z.; Wu, T.; Zhao, X.; Zu, Y. Solubility, Antioxidation, and Oral Bioavailability Improvement of Mangiferin Microparticles Prepared Using the Supercritical Antisolvent Method. Pharmaceutics 2020, 12, 90. [Google Scholar] [CrossRef]
- Telange, D.R.; Sohail, N.K.; Hemke, A.T.; Kharkar, P.S.; Pethe, A.M. Phospholipid complex-loaded self-assembled phytosomal soft nanoparticles: Evidence of enhanced solubility, dissolution rate, ex vivo permeability, oral bioavailability, and antioxidant potential of mangiferin. Drug. Deliv. Transl. Res. 2021, 11, 1056–1083. [Google Scholar] [CrossRef]
- Yang, L.P.; Wang, H.J.; Li, W.H.; Wang, F.Y.; Fang, X.D. Formulation optimization of mangiferin-amino-modified mesoporous silica nanoparticles and oral pharmacokinetics evaluation. Chin. Tradit. Herb. Drugs 2024, 55, 2542–2552. [Google Scholar]
- Li, Z.J.; Pu, Z.J.; Gao, Y.W.; Zhou, M.; Zhang, Z.; Xiao, P.F.; Chen, J.T.; Zhou, C.Y. Integrated serum and liver metabolomics decipher the hepatoprotective mechanisms of mangiferin sodium salt through modulating alcohol metabolism on alcoholic liver disease. Food Biosci. 2024, 61, 104631. [Google Scholar] [CrossRef]
- Xiong, W.N.; Yue, G.H.; Ye, M.L.; Liang, J.Q.; Wang, Z.P.; Tang, Z.Y.; Wu, Y.Q. Preparation and characterization of mangiferin-polyvinylpyrrolidone solid dispersons and its in vitro metabolism by human intestinal microflora. Chin. J. Hosp. Pharm. 2017, 37, 1028–1032. [Google Scholar]
- Yang, X.; Yang, C.; Zhang, S.; Geng, H.; Zhu, A.X.; Bernards, R.; Qin, W.; Fan, J.; Wang, C.; Gao, Q. Precision treatment in advanced hepatocellular carcinoma. Cancer Cell 2024, 42, 180–197. [Google Scholar] [CrossRef]
- Terrault, N.A.; Francoz, C.; Berenguer, M.; Charlton, M.; Heimbach, J. Liver Transplantation 2023: Status Report, Current and Future Challenges. Clin. Gastroenterol. Hepatol. 2023, 21, 2150–2166. [Google Scholar] [CrossRef] [PubMed]
- Adam, R.; Piedvache, C.; Chiche, L.; Adam, J.P.; Salamé, E.; Bucur, P.; Cherqui, D.; Scatton, O.; Granger, V.; Ducreux, M.; et al. Collaborative TransMet group. Liver transplantation plus chemotherapy versus chemotherapy alone in patients with permanently unresectable colorectal liver metastases (TransMet): Results from a multicentre, open-label, prospective, randomised controlled trial. Lancet 2024, 404, 1107–1118. [Google Scholar]
- Mallapaty, S. First pig-to-human liver transplant recipient ‘doing very well’. Nature 2024, 630, 18. [Google Scholar] [CrossRef]
- Zhong, L.; Gan, L.; Wang, B.; Wu, T.; Yao, F.; Gong, W.; Peng, H.; Deng, Z.; Xiao, G.; Liu, X.; et al. Hyperacute rejection-engineered oncolytic virus for interventional clinical trial in refractory cancer patients. Cell 2025, 188, 1119–1136. [Google Scholar] [CrossRef]
- Sidik, S. How to trick the immune system into attacking tumours. Nature, 2025; online ahead of print. [Google Scholar] [CrossRef]
- Irshad, N.; Naeem, H.; Shahbaz, M.; Imran, M.; Mujtaba, A.; Hussain, M.; Al-Abdulmonem, W.; Alsagaby, S.A.; Yehuala, T.F.; Abdelgawad, M.A.; et al. Mangiferin: An effective agent against human malignancies. Food. Sci. Nutr. 2024, 12, 7137–7157. [Google Scholar] [CrossRef]
- Iqbal, H.; Inam-Ur-Raheem, M.; Munir, S.; Rabail, R.; Kafeel, S.; Shahid, A.; Mousavi Khaneghah, A.; Aadil, R.M. Therapeutic potential of mangiferin in cancer: Unveiling regulatory pathways, mechanisms of action, and bioavailability enhancements-An updated review. Food. Sci. Nutr. 2023, 12, 1413–1429. [Google Scholar] [CrossRef]
- Ji, H.W.; Wang, C.R.; Yuan, X.W.; Wang, J.; Wang, L.; Cao, Q.L.; Li, Y.H.; Xu, Y.N.; Kim, N.H. Mangiferin improves early porcine embryonic development by reducing oxidative stress. Reprod. Domest. Anim. 2024, 59, e14565. [Google Scholar] [CrossRef]
- Rao, J.; Qiu, P.; Zhang, Y.; Wang, X. Gut microbiota trigger host liver immune responses that affect drug-metabolising enzymes. Front. Immunol. 2024, 15, 1511229. [Google Scholar] [CrossRef]
- Tilg, H.; Adolph, T.E.; Trauner, M. Gut-liver axis: Pathophysiological concepts and clinical implications. Cell Metab. 2022, 34, 1700–1718. [Google Scholar] [CrossRef]
- Imparato, G.; Urciuolo, F.; Netti, P.A. Organ on Chip Technology to Model Cancer Growth and Metastasis. Bioengineering 2022, 9, 28. [Google Scholar] [CrossRef]
- Monteduro, A.G.; Rizzato, S.; Caragnano, G.; Trapani, A.; Giannelli, G.; Maruccio, G. Organs-on-chips technologies—A guide from disease models to opportunities for drug development. Biosens. Bioelectron. 2023, 231, 115271. [Google Scholar] [CrossRef]
- Alonso-Roman, R.; Mosig, A.S.; Figge, M.T.; Papenfort, K.; Eggeling, C.; Schacher, F.H.; Hube, B.; Gresnigt, M.S. Organ-on-chip models for infectious disease research. Nat. Microbiol. 2024, 9, 891–904. [Google Scholar] [CrossRef] [PubMed]
- Lucchetti, M.; Aina, K.O.; Grandmougin, L.; Jäger, C.; Pérez Escriva, P.; Letellier, E.; Mosig, A.S.; Wilmes, P. An Organ-on-Chip Platform for Simulating Drug Metabolism Along the Gut-Liver Axis. Adv. Healthc. Mater. 2024, 13, e2303943. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).