Abstract
Purpose: The aims of this study were to explore the differences in total body water and hydration status among Chinese children aged 6–17 years. Methods: A cross-sectional study was implemented among children aged 6–17 years in China. The total body water (TBW), intracellular water (ICW), and extracellular water (ECW) were determined by bioelectrical impedance analysis (BIA). The participants were divided according to age—age 6–8 years, age 9–11 years, age 12–14 years, age 15–17 years—and body mass index (BMI) of China—underweight, normal weight, overweight, and obese groups. The differences of variables of groups were compared using analysis of variance, Student’s t-test, and Kruskal–Wallis test. Significance levels were set at 0.05 (p < 0.05). Results: A total of 59,643 participants (30,103 males and 29,540 females) completed the study. As children became older, the TBW, ICW, ECW, ICW/TBW, and TBW/FFM (TBW to fat free mass ratio) increased simultaneously (all p < 0.05); concurrently, the ECW/TBW decreased with age (all p < 0.05). Boys had higher TBW, ICW, ECW, ICW/TBW, TBW/BW, and TBW/FFM than those of girls at each age (all p < 0.05). For all BMI groups, increases in TBW, ICW, ECW were observed from the underweight group to the obese group, both in boys and girls (all p < 0.001). For the increase in BMI in all age groups, the values of TBW made a significantly lower percentage compared to BW. The higher BMI groups showed higher levels of TBW/FFM, both in girls and boys (all p < 0.001). Conclusions: The body water contents of children aged 6–17 years varied according to their age, sex, and BMI. Overweight and obese individuals may have inferior hydration status compared to those with normal weight.
1. Background
Water is not only an essential nutrient but also a key molecule essential for keeping cellular homoeostasis, which accounts for 50–75% of the body weight (BW). The body’s water content consists of intracellular water (ICW) and extracellular water (ECW) [1]. ICW compromises 2/3 of the total body water (TBW), which is the principal element influencing the cell volume. Meanwhile, the ECW consists of plasma, interstitial fluid, and other transcellular fluids [2]. Maintaining body dynamic water balance between ICW and ECW is a matter of public health concern, especially in infants and young children [3]. It has been proved that body water compartments are impacted by water intake. Given that children have higher proportions of total water content in the body and are less sensitive to thirst sensation, children are more prone to have inadequate water intake than adults. Accordingly, children with inadequate water intake have more risk to be dehydrated than those meeting the recommendation of total water intake, which could lead to adverse effects on health [4,5]. Therefore, it is of great significance to have adequate water intake and maintain the dynamic water balance of the body in children.
More generally, the TBW and its compartments are associated with health. Currently, TBW is used to determine the hydration status [6,7,8]. Hydration statuses are divided into dehydration, optimal hydration, and middle hydration status. Dehydration, as a deficit in TBW, is associated with adverse health outcomes among children, including physical performances, cognition, intestinal mucus homeostasis, sleep duration, faster aging, and even has been linked to obesity and malnutrition [9,10,11,12]. Additionally, the proportion of ECW to TBW utilized is a signifier of the human body’s volume overload. Meanwhile, studies have revealed that the water content of the body is not only correlated with hydration status but also with health [13,14,15,16,17,18]. In the case of healthy people, in comparison with youth, the ICW compartment proved to be a more reliable predictor for muscle performance of both adults and older adults [17]. Regarding people with diseases, measuring body water content provided clinically valuable information applicable to numerous situations, such as inflammatory processes. For instance, the ECW to TBW ratio of ≥0.4 could predict treatment failure among patients with advanced lung cancer or poorer relapse-free survival in patients with correctional cancer [14,16]. In addition, TBW and ICW were correlated with cardiovascular disease [19]. Hence, monitoring the changes of body water compartments are extremely important.
Methods to measure body water in humans includes isotope dilution, air displacement plethysmography (ADP), dual-energy X-ray absorptiometry (DEXA), and bioelectrical impedance analysis (BIA) [20]. The isotope dilution is the golden method, but with highly expensive cost and difficulty in operation. While it is worth mentioning that BIA has been proved with high validity and accuracy to determine total body water content [21,22,23,24,25,26,27], even for acute water supplementation of 120 min, significant changes in ICW and ECW were observed using BIA among young adults [28]. Therefore, BIA has been able to fill the aforementioned scientific gaps in measuring body water content in a large sample of people.
In China, only a few studies have accurately assessed the changes of TBW and its compartments among adults [24,29], not to say among children or adolescents. One study reported the results of water contents of young healthy adults aged 18–23 years, mainly showing that the TBW and the compartments differed from that of adults with the same age in other countries [24]. Another research study demonstrated that TBW decreased among healthy adults after 36 h water restriction [29]. However, the characteristics of body water content have not been fully evaluated and studied among children and adolescents, and comprehensive large-sample studies are lacking. As a result, it is challenging to gauge the growth trajectory and related health perils of children but more data are needed to understand this issue.
To address this deficiency, we devised the present investigation to examine the water content of the body using BIA among Chinese children and adolescents aged 6–17 years in free-living conditions, including factors that affect total body water, including gender, age and, nutrition status. Our study should provide basic information of body water and its constituent compartments of children in China, and could give rise to a means of education on fluid intake that is based on science for children in order to promote their healthy development.
2. Methods
2.1. Subjects
A cross-sectional study was formulated, which consisted of 196 individuals in each age group (28 strata,14 provinces, 7 regions, 2 urban/rural samples, half males and half females). We employed a multi-stage stratified randomized cluster sampling technique to compute the sample size. In total, 65,856 children aged 6–17 years were required for the study. The inclusion criteria were as follows: age between 6 to 17 years; healthy children without diseases as diagnosed by hospital; having stayed in the survey location for longer than 6 months; and having completed a written informed consent form. Exclusion criteria were set as follows: individuals with either acute or chronic ailments, including acute respiratory tract infection, acute gastroenteritis, and congenital heart defects, were not included in the study [30].
2.2. Anthropometric Measurements
The height, weight, and body composition were assessed in the morning with participants having fasted overnight. The height of the participants was gauged with an accuracy of up to 0.1 cm, while the weight was measured with a precision of up to 0.1 kg. Furthermore, this was done when the participants were dressed in light clothing and barefoot—digital weight scales (GMCS-I electronic scale; Jianmin, Beijing, China) Body mass index (BMI) was defined as the ratio of weight (kg) to the square of height (m2).
Body water contents, including TBW, ICW and ECW, FFM were determined by a bioelectrical impedance analyzer (BIA) (Inbody 770; Inbody; Seoul, Korea) with trained investigators, in which participants were also asked to be in light clothing and barefoot. In accordance with the four-component model theory of body composition, the instrument is equipped with 8-point contact electrodes, specifically two thumb electrodes, two palm electrodes, two sole electrodes, and two heel electrodes. It functions by measuring 30 impedance values across 5 body segments, namely the left and right upper limbs, the trunk, and the lower limbs, and this is achieved at 6 distinct frequencies: 1, 5, 50, 250, 500, and 1000 kHz. By employing diverse high-frequency and low-frequency settings, it can measure the intracellular and extracellular water, respectively, thereby enabling an accurate analysis of the overall water content [31].
From the body water compartments, ratios were calculated for further analyses, namely TBW/BW (TBW to BW ratio), ICW/TBW (ICW to TBW ratio), ECW/TBW (ECW to TBW ratio), ECW/ICW (ECW to ICW ratio), and TBW/FFM (TBW to FFM ratio).
2.3. Statistics
The statistical analysis of the current study was carried out using the SAS 9.2 software (SAS Institute Inc., Cary, NC, USA). Age was categorized in four quartiles: age 6–8 years, age 9–11 years, age 12–14 years, and age 15–17 years. BMI was classified according to the health industry standards in China—Screening Standard for Malnutrition in School-age Children and Adolescents: WS/T 456-2014 [32]; Screening for overweight and obesity among school-age children and adolescents: WS/T 586-2018 [33]—into underweight, normal weight, overweight, and obesity. Data were presented in two different ways depending on their distribution. If the data were normally distributed, they were shown as the mean ± standard deviation; if not, they were presented as the median and interquartile ranges (IQR = 25th–75th percentile). Differences of variables in normal distribution including the proportions TBW/BW, ICW/TBW, ECW/TBW, ECW/ICW, and TBW/FFM among the four age groups, and three nutrition status groups were used for one-way ANOVA; the Scheffe’s method for multiple tests was employed, and the alpha level was set at 0.05, both in boys and girls. Differences of variables in skewness distribution such as the TBW, ICW, ECW, and FFM among the four age groups and three nutrition status groups were assessed by the Kruskal–Wallis H test, both in boys and girls; the alpha level was set at 0.008 (0.05/6 comparisons) and 0.017 (0.05/3 comparisons) for multiple tests. Mann–Whitney U test and Student’s t-test were used to compare differences between groups of sexes with the same age. Statistical significance was set at p < 0.05.
3. Results
The study included 59,643 participants, including 30,103 boys and 29,540 girls. About 6213 participants quitted the study. The participant characteristics are displayed in Table 1. The height, weight, and BMI differed significantly between boys and girls (all p < 0.05). The flow chart is shown in Figure 1.

Table 1.
Participant characteristics.
Figure 1.
The flow chart.
The TBW, ICW, and ECW of the participants were 24.4 kg, 15.0 kg, and 9.4 kg, respectively; the proportions of ICW/TBW, ECW/TBW, TBW/FFM, and TBW/BW were 61.6%, 38.4%, 73.1%, and 56.1%, respectively. The characteristics of body water contents of subjects with different ages are illustrated in Table 2. As the children became older, the TBW, ICW, ECW, ICW/TBW, and TBW/FFM increased year by year, while, the ECW/TBW decreased simultaneously with age. For boys, the TBW, ICW, and ECW increased with age (all p < 0.001), for which the TBW and ICW increased from 15.3 kg and 9.4 kg in age 6–7 years to 37.5 kg and 23.4 kg in age 16–17 years (p < 0.05), respectively. For girls, the same trend was observed (all p < 0.001). The values of TBW and ICW increased from 14.3 kg and 8.8 kg for subjects of age 6–7 years to 27.6 kg and 17.0 kg for subjects of age 16–17 years, respectively (all p < 0.001). Furthermore, after the age of 11 years, the TBW, ICW, and ECW increased rapidly, observed both in boys and girls.

Table 2.
The body water content of participants of different age groups.
Proportions TBW/BW, ICW/TBW, ECW/TBW, and TBW/FFM were different among the age groups, for both genders of children (all p < 0.001). As for ICW/TBW, the values for boys were all higher than girls at the same age (p < 0.05), except for age 6 years. The rates of the changes in ICW/TBW surpassed those of the girls, with the girls reaching their peak at the age of 14 years; while the boys increased after reaching their peak at 8 to 12 years of age, ranging from 61.6% at age 6–7 years to 62.3% at the age 16–17 years. As for ECW/TBW, the trends of boys and girls all decreased with age, and the values of each age were all lower in boys than those of girls (all p < 0.05). Moreover, the ECW/TBW decreased after reaching peaks at 8 to 12 years of age, but that of girls did not decrease from 14 to 17 years of age. However, the trends of TBW/FFM with age differed between boys and girls, but the values of boys exceeded those of the girls (all p < 0.05). The TBW/FFM of boys did not significantly change at the ages of 8–10 years and 12–15 years, but rapidly decreased after the age of 15 years (p < 0.05). However, the peaks of TBW/FFM in girls were at the ages of 11–12 years and 15–17 years (p < 0.05), as depicted in Figure 2.
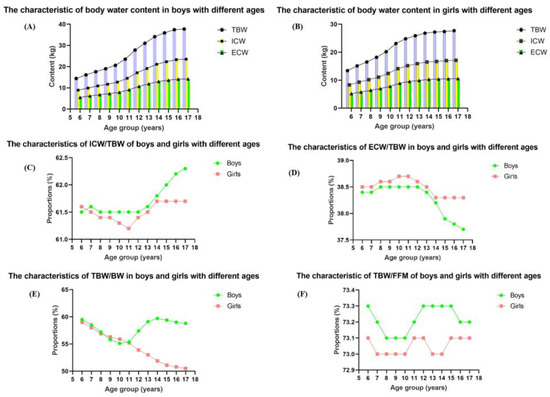
Figure 2.
The body water content of boys and girls with different age groups. (A): The characteristic of body water content in boys with different ages; (B): The characteristic of body water content in girls with different ages; (C): The characteristic of ICW/TBW of boys and girls with different ages; (D): The characteristic of ECW/TBW of boys and girls with different ages; (E): The characteristic of TBW/BW of boys and girls with different ages; (F): The characteristic of TBW/FFM of boys and girls with different ages.
The body water compartments of subjects with different BMI are given in Table 3 and Figure 3. All BMI groups showed differences in TBW, ICW, ECW, and FFM, with the highest contents of TBW, ICW, ECW, and FFM in the overweight and obese group, among both boys and girls (all p < 0.001). Additionally, the ICW/TBW, ECW/TBW, TBW/BW, ECW/ICW, and TBW/FFM differed significantly in the three BMI groups (all p < 0.001), but with different patterns. The children in the obesity group showed clearly lower levels of TBW/BW at all ages (all p < 0.001); with boys having higher proportions than those of girls with the same age (all p < 0.001). Moreover, TBW/BW demonstrated a decrease first and increased at the age of 12 years, but the decrease was marked in the overweight and obese and underweight group; the normal group showed a smaller decrease. Otherwise, the TBW/BW, ECW/TBW, and ECW/ICW showed decreases among the BMI groups, and the ICW/TBW increased among the groups (all p < 0.001). Furthermore, lower BMI groups presented lower levels of TBW/FFM, simultaneously; the higher BMI groups showed higher levels of TBW/FFM, both in girls and boys (all p < 0.001). The normal group and the overweight group showed no differences in the variance of TBW/FFM (p > 0.05), but with the highest one in the obese group and the lowest in the underweight group (all p < 0.001), as shown in Figure 3.

Table 3.
The body water content of participants in different age groups of nutrition status.
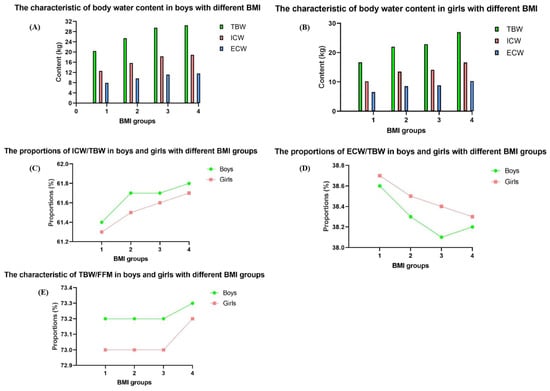
Figure 3.
The body water content of boys and girls with different BMI groups. 1: Underweight group; 2: Normal weight group; 3: Overweight group; 4: Obese group; (A): The characteristic of body water content in boys with different BMI; (B): The characteristic of body water content in girls with different BMI; (C): The proportions of ICW/TBW in boys and girls with different BMI groups; (D): The proportions of ECW/TBW in boys and girls with different BMI groups; (E): The characteristic of TBW/FFM in boys and girls with different BMI groups.
4. Discussion
As far we know, the current study was the maiden attempt to explore the differences in body water content among children within the age range of 6–17 years in China.
As expected, in our study, the TBW, ICW, ECW increased simultaneously with age, and boys had higher indices than girls of the same age, which was consistent with other studies in Poland and Spain [34,35]. In one study, which examined ballet school aged 14 ± 2 and elementary school students aged 10 ± 2 in Poland, the results showed that the TBW increased from elementary school children to ballet high school children [35]. These results further demonstrate that as children grow older, it could bring about changes in their body water compartments. Interestingly, even among children of the same age, the numbers of TBW, ICW, and ECW of children from the United States, Spain, and Portugal were different compared to that of the present study [17,36,37]. The contents of TBW, ICW, and ECW among children aged 6–17 years in Portugal (26.7 kg, 15.1 kg, and 11.6 kg) were all higher than the results of ours (24.4 kg, 15.0 kg, and 9.4 kg), respectively [17]. Differences in the methods measuring the body water contents or race might account for the disputable findings of the research studies. The current study used BIA to determine the TBW and its compartments, whereas, in the other study in Spain, the TBW was assessed by isotope dilution. Children apart, in adults similar differences of body water compartments were found among different countries using the BIA to evaluate the body water contents [24,38,39]. Notwithstanding, the TBW differed among children of the same age with racial/ethnic groups using the same methods in evaluating body composition [40]. In this study, the TBW of Black children aged between 4 and 6 years, 7 and 9 years, 10 and 12 years, as well as 13 and 15 years, which were measured by deuterium dilution, were all higher than that of White and Hispanic children.
As previously mentioned, the values of TBW, ICW, ECW, TBW/BW, ICW/TBW, ECW/TBW, ECW/ICW, and TBW/FFM of both genders of children of different ages varied significantly. In addition, our research revealed that, in comparison to girls, boys exhibited higher values for TBW, ICW, ECW, and the ratio of TBW to fat-free mass (TBW/FFM). Moreover, these values demonstrated a steady upward trend as age advanced. The changes of TBW/BW with aging have been documented in other studies among children and adults [37,41]. Interestingly, in the current study, the percentages of TBW/BW presented a different change trend among age groups, ranging from 50.8% to 59.1%. Further on, TBW/BW decreased from 58.4% to 55.4%, reaching then the age of 9–11 years, and then a slight increase to 59.1% was observed in boys between 15 and 17 years. While girls exhibited a continuously decreasing trend in their relative values from 58.5% to 50.8%; as previously reported [42]. Moreover, we observed that compared with girls, boys had higher TBW/BW, except at the age of 9–11 years old. This may be attributed to the relatively higher increased body weight and muscle mass in boys than girls [43].
In the current research, the proportion of ECW/TBW increased with age, and in all of the age groups under consideration, girls had a higher value than boys (p < 0.001). Similar results were found in another large sample study of adults [22]. As for ECW/ICW, according to one research study, women presented a greater ECW/ICW ratio [44], which was consistent with our results that in all age group, the ECW/ICW was higher in girls and increased with age, but remained stable at 0.38. In another study conducted among 1992 healthy individuals aged ≥ 15 years in Japan, the findings indicated that as age advanced, the ratio of ECW to ICW grew because the decline in ICW content was more pronounced compared to that of ECW [45]. Nevertheless, controversial results were demonstrated in a study conducted among children aging in the United States, in that no significant differences of ECW/ICW were found in age groups, nor in boys or girls [46]. The results could be explained by differences of race. Similar trends were observed when comparing with Black, White, and Hispanic children in the United States [40]. The ratio was stable at 0.730–0.732 in our study, lower than that of adults, which may be explained by the higher proportions of water and the differences of mineral and protein when comparing children with adults [47], meaning that the children were in optimal hydration status in our study. Meanwhile, the values of TBW/FFM were lower than the results obtained from a study carried out among children within the age range of 6–16 years in the United States, in which the proportions of TBW/FFM were 74.2% [48]. The methods to assess and calculate the TBW/FFM result in the differences in the outcomes. Hence, alterations in total body water could have an impact on overall health, which confirms the importance of the balance of the body water compartments.
It demonstrated that as children increased in BMI in all age groups from underweight to obesity, the values of TBW made a significantly lower percentage to BW, both in girls and boys. This might be due to the fact that the excessive body weight (BW) stemmed from a relatively high proportion of body fat as compared to the proportions of FFM and TBW in relation to BW [49], even though the TBW and FFM increased with BMI in all age groups. Because the contributions of water to body fat and FFM were ~10% and 75% [50], overweight and obese individuals had lower TBW/BW, which has been demonstrated among adults [34]. Additionally, in our research, a gender disparity was observed in this parameter; specifically, at the same BMI, boys were found to possess more water per kilogram of body weight compared to girls, which is consistent with the results of the studies implemented among children, adolescents, and healthy adults [51,52,53]. However, previous studies revealed that participants of overweight were hypohydrated when compared with those of normal weight [54,55,56]. Unexpected slight changes of TBW/BW were found in children with normal weight, and large fluctuations were observed among those with obesity. Thereby, lower values of TBW/BW among overweight and obesity children are noteworthy, as there is a higher proportion of children with obesity around the world. More researche studies are needed to evaluate the effects of lower proportions of TBW to BW on the health of children with obesity, who were shown to have less water and a higher risk to be hypohydrated [57].
There have been few data evaluating the distribution of human body water between ECW and ICW among children. Our study showed that the ECW/TBW increased and ICW/TBW decreased with BMI, and was higher in girls than boys over the whole BMI range. Moreover, at similar BMI, girls had a higher proportion of body fat than boys, therefore, higher ECW/TBW as expected [22]. It was proved that the indicator of cellular hydration, TBW/FFM, was not only impacted by age but also impacted by nutrition status, in other words, the BMI [55]. The increasing values of TBW/FFM were obtained in girls from normal weight to overweight and obesity throughout the age range, but only among boys at the age of 6 years to 11 years, in our study, which is similar to the study implemented in a small sample of 28 obese children and 22 non-obese children [52]. The mechanism that expanded ECW may bring about the shifts in the constitution of FFM associated with obesity [58]. Furthermore, another study suggested that the higher content of water and mineral and relatively lower percentage of protein in obese children may be attributed to the higher hydration status [51]. But there may be more mechanisms leading to the alterations of TBW/FFM, which are also in need of more attention.
Our research possessed certain advantages and disadvantages. First, in China, our research was primarily to assess the influential factors including age, sex, and nutrition status of body water among adolescents including males and females in free-living conditions and it was of a substantial sample size over a wide range of age and BMI. Although our study had certain notable strengths as previously described, it was not without its limitations. The research was specifically conducted among children, which means that when extending the study’s conclusions to other age brackets, caution must be exercised. Going forward, further investigations will explore the broader applicability of our findings to a more diverse demographic, encompassing adults as well as the elderly.
5. Conclusions
The body water content and the changes of children aged 6–17 years in China varied according to their age, sex, and BMI. Overweight and obese individuals had significantly lower TBW/BW and higher TBW/FFM than those with normal weight. Hence, in order to maintain stability of the body water content, science-based education of fluid intake for children is needed in the light of the distinct traits exhibited by children, particularly those who are overweight.
Author Contributions
J.Z. was responsible for the conceptualization, formal analysis, and investigation of the study and the drafting of the paper. J.Z., W.C., H.W., and R.L. were responsible for the investigation of the study. W.C. and Q.G. were responsible for the data curation, software, and resources of the study and provided substantive revisions to the initial draft of the paper. Q.G., T.Y., and H.P. were responsible for validation of the study. J.X., Z.Y., W.Z., and Q.Z. were responsible for the funding acquisition, methodology, project administration, supervision, and review, editing, and the writing of the study. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Special Program for Science & Technology Basic Resources Investigation of China (Grant No. 2017FY101100, 2017FY101101, 2017FY101102, 2017FY101103, 2017FY101104, 2017FY101105, 2017FY101106, and 2017FY101107). The Funding source had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Institutional Review Board Statement
The project was approved by the Medical Ethical Review Committee at the National Institute for Nutrition and Health, Chinese Center for Disease Control and Prevention (No. 2019-009, 18 March 2019).
Informed Consent Statement
Parents or guardians of the study subjects signed the informed consent form, and for children > 8 years of age, both parents/guardians and the child co-signed the informed consent form.
Data Availability Statement
Data described in the manuscript will be made available upon request pending application and approval from the corresponding author.
Acknowledgments
We would like to thank investigators for participating in this project.
Conflicts of Interest
The authors declare that they have no competing interests.
Abbreviations
| TBW | Total body water |
| ICW | Intracellular water |
| ECW | Extracellular water |
| FFM | Fat free mass |
References
- Popkin, B.M.; D’Anci, K.E.; Rosenberg, I.H. Water, hydration, and health. Nutr. Rev. 2010, 68, 439–458. [Google Scholar] [CrossRef] [PubMed]
- Kleiner, S.M. Water: An essential but overlooked nutrient. J. Am. Diet. Assoc. 1999, 99, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Jequier, E.; Constant, F. Water as an essential nutrient: The physiological basis of hydration. Eur. J. Clin. Nutr. 2010, 64, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Suh, H.; Kavouras, S.A. Water intake and hydration state in children. Eur. J. Nutr. 2018, 58, 475–496. [Google Scholar] [CrossRef] [PubMed]
- Kavouras, S.A.; Bougatsas, D.; Johnson, E.C.; Arnaoutis, G.; Tsipouridi, S.; Panagiotakos, D.B. Water intake and urinary hydration biomarkers in children. Eur. J. Clin. Nutr. 2017, 71, 530–535. [Google Scholar] [CrossRef]
- Armstrong, L.; Johnson, E. Water Intake, Water Balance, and the Elusive Daily Water Requirement. Nutrients 2018, 10, 1928. [Google Scholar] [CrossRef]
- Baron, S.; Courbebaisse, M.; Lepicard, E.M.; Friedlander, G. Assessment of hydration status in a large population. Brit J. Nutr. 2015, 113, 147–158. [Google Scholar] [CrossRef] [PubMed]
- Cheuvront, S.N.; Kenefick, R.W. Dehydration: Physiology, assessment, and performance effects. Compr. Physiol. 2014, 4, 257–285. [Google Scholar] [PubMed]
- Westfall, D.R.; Logan, N.E.; Khan, N.A.; Hillman, C.H. Cognitive Assessments in Hydration Research Involving Children: Methods and Considerations. Ann. Nutr. Metab. 2019, 74, 19–24. [Google Scholar] [CrossRef]
- Papies, E.K. The Psychology of Desire and Implications for Healthy Hydration. Ann. Nutr. Metab. 2021, 76, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Santillanes, G.; Rose, E. Evaluation and Management of Dehydration in Children. Emerg. Med. Clin. N. Am. 2018, 36, 259–273. [Google Scholar] [CrossRef] [PubMed]
- Chouraqui, J.P. Children’s water intake and hydration: A public health issue. Nutr. Rev. 2022, 5, 610–624. [Google Scholar] [CrossRef] [PubMed]
- Nishikawa, H.; Yoh, K.; Enomoto, H.; Ishii, N.; Iwata, Y.; Nakano, C.; Takata, R.; Nishimura, T.; Aizawa, N.; Sakai, Y.; et al. Extracellular Water to Total Body Water Ratio in Viral Liver Diseases: A Study Using Bioimpedance Analysis. Nutrients 2018, 10, 1072. [Google Scholar] [CrossRef] [PubMed]
- Horino, T.; Tokunaga, R.; Miyamoto, Y.; Akiyama, T.; Daitoku, N.; Sakamoto, Y.; Ohuchi, M.; Ogawa, K.; Yoshida, N.; Baba, H. Extracellular water to total body water ratio, a novel predictor of recurrence in patients with colorectal cancer. Ann. Gastroent. Surg. 2024, 8, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, H.; Hashimoto, Y.; Kaji, A.; Sakai, R.; Takahashi, F.; Yoshimura, Y.; Bamba, R.; Okamura, T.; Kitagawa, N.; Majima, S.; et al. Impact of extracellular-to-intracellular fluid volume ratio on albuminuria in patients with type 2 diabetes: A cross-sectional and longitudinal cohort study. J. Diabetes Investig. 2021, 12, 1202–1211. [Google Scholar] [CrossRef] [PubMed]
- Noda, Y.; Suzuki, H.; Kanai, T.; Samejima, Y.; Nasu, S.; Tanaka, A.; Morishita, N.; Okamoto, N.; Hirashima, T. The Association Between Extracellular Water-to-Total Body Water Ratio and Therapeutic Durability for Advanced Lung Cancer. Anticancer Res. 2020, 40, 3931–3937. [Google Scholar] [CrossRef] [PubMed]
- Hetherington-Rauth, M.; Baptista, F.; Sardinha, L.B. BIA-assessed cellular hydration and muscle performance in youth, adults, and older adults. Clin. Nutr. 2020, 39, 2624–2630. [Google Scholar] [CrossRef] [PubMed]
- Low, S.; Ng, T.P.; Lim, C.L.; Ang, S.F.; Moh, A.; Wang, J.; Yap, P.; Cheong, C.Y.; Goh, K.S.; Ang, K.; et al. Higher ratio of extracellular water to total body water was associated with reduced cognitive function in type 2 diabetes. J. Diabetes 2021, 13, 222–231. [Google Scholar] [CrossRef]
- Popiolek-Kalisz, J.; Szczygiel, K. Bioelectrical Impedance Analysis and Body Composition in Cardiovascular Diseases. Curr. Prob. Cardiol. 2023, 48, 101911. [Google Scholar] [CrossRef] [PubMed]
- Prior, E.; Uthaya, S.N.; Gale, C. Measuring body composition in children: Research and practice. Arch. Dis. Child. E 2023, 108, 285–289. [Google Scholar] [CrossRef]
- Campa, F.; Gobbo, L.A.; Stagi, S.; Cyrino, L.T.; Toselli, S.; Marini, E.; Coratella, G. Bioelectrical impedance analysis versus reference methods in the assessment of body composition in athletes. Eur. J. Appl. Physiol. 2022, 122, 561–589. [Google Scholar] [CrossRef] [PubMed]
- Ekingen, T.; Sob, C.; Hartmann, C.; Ruhli, F.J.; Matthes, K.L.; Staub, K.; Bender, N. Associations between hydration status, body composition, sociodemographic and lifestyle factors in the general population: A cross-sectional study. BMC Public Health 2022, 22, 900. [Google Scholar] [CrossRef] [PubMed]
- Laja García, A.; Moráis-Moreno, C.; Samaniego-Vaesken, M.; Puga, A.; Varela-Moreiras, G.; Partearroyo, T. Association between Hydration Status and Body Composition in Healthy Adolescents from Spain. Nutrients 2019, 11, 2692. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Zhang, J.; Du, S.; He, H.; Yan, X.; Ma, G. Association between the content of intracellular and extracellular fluid and the amount of water intake among Chinese college students. Nutr. Metab. 2019, 16, 67. [Google Scholar] [CrossRef] [PubMed]
- Ræder, H.; Kværner, A.S.; Henriksen, C.; Florholmen, G.; Henriksen, H.B.; Bøhn, S.K.; Paur, I.; Smeland, S.; Blomhoff, R. Validity of bioelectrical impedance analysis in estimation of fat-free mass in colorectal cancer patients. Clin. Nutr. 2018, 37, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Reale, R.; Burke, L.M.; Cox, G.R.; Slater, G. Body composition of elite Olympic combat sport athletes. Eur. J. Sport. Sci. 2020, 20, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Andreoli, A.; Garaci, F.; Cafarelli, F.P.; Guglielmi, G. Body composition in clinical practice. Eur. J. Radiol. 2016, 85, 1461–1468. [Google Scholar] [CrossRef]
- Schierbauer, J.; Gunther, S.; Haupt, S.; Zimmer, R.T.; Herz, D.; Voit, T.; Zimmermann, P.; Wachsmuth, N.B.; Aberer, F.; Moser, O. Acute Fluid Intake Impacts Assessment of Body Composition via Bioelectrical Impedance Analysis. A Randomized, Controlled Crossover Pilot Trial. Metabolites 2023, 13, 473. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhang, N.; Du, S.; Liu, S.; Ma, G. Effects of Water Restriction and Water Replenishment on the Content of Body Water with Bioelectrical Impedance among Young Adults in Baoding, China: A Randomized Controlled Trial (RCT). Nutrients 2021, 13, 553. [Google Scholar] [CrossRef]
- Yang, Z.; Zhang, Q.; Zhai, Y.; Xu, T.; Wang, Y.; Chen, B.; Tang, X.; Yuan, X.; Fang, H.; Zhu, Y.; et al. National Nutrition and Health Systematic Survey for Children 0–17 Years of Age in China. Biomed. Environ. Sci. 2021, 34, 891–899. [Google Scholar] [PubMed]
- Blue, M.; Tinsley, G.M.; Ryan, E.D.; Smith-Ryan, A.E. Validity of Body-Composition Methods across Racial and Ethnic Populations. Adv. Nutr. 2021, 12, 1854–1862. [Google Scholar] [CrossRef] [PubMed]
- WS/T 456-2014; Screening Standard for Malnutrition in School-age Children and Adolescents. National Health and Family Planning Commission of the People’s Republic of China: Beijing, China, 2014.
- WST 586-2018; Screening for Overweight and Obesity Among School-Age Children and Adolescents. National Health and Family Planning Commission of the People’s Republic of China: Beijing, China, 2018.
- Ritz, P.; Vol, S.; Berrut, G.; Tack, I.; Arnaud, M.J.; Tichet, J. Influence of gender and body composition on hydration and body water spaces. Clin. Nutr. 2008, 27, 740–746. [Google Scholar] [CrossRef] [PubMed]
- Anisko, B.; Siatkowski, I.; Wojcik, M. Body mass composition analysis as a predictor of overweight and obesity in children and adolescents. Front. Public Health 2024, 12, 1371420. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Marín, D.; Luque, V.; Ferré, N.; Fewtrell, M.S.; Williams, J.E.; Wells, J.C.K. Associations of age and body mass index with hydration and density of fat-free mass from 4 to 22 years. Eur. J. Clin. Nutr. 2019, 73, 1422–1430. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Ayers, E.; Patel, P.; Mattoo, T.K. Body water percentage from childhood to old age. Kindey Res. Clin. Prac. 2023, 42, 340–348. [Google Scholar] [CrossRef]
- Chumlea, W.C.; Guo, S.S.; Zeller, C.M.; Reo, N.V.; Baumgartner, R.N.; Garry, P.J.; Wang, J.; Pierson, R.J.; Heymsfield, S.B.; Siervogel, R.M. Total body water reference values and prediction equations for adults. Kidney Int. 2001, 59, 2250–2258. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.J.; Lee, S.W.; Song, J.H. Normal values of total body water in healthy Korean adults: Comparison with data from western populations. Yonsei Med. J. 2002, 43, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Roman, J.S.; William, W.W. Fat and fat-free mass index references in children and young adults: Assessments along racial and ethnic lines. Am. J. Clin. Nutr. 2020, 112, 566–575. [Google Scholar]
- Jonathan, C.K.W.; Nigel, J.F.; Odile, D.; Marry, S.F.; Marinos, E.; Tim, J.C. Four-component model of body composition in children: Density and hydration of fat-free mass and comparison with simpler models1,2. Am. J. Clin. Nutr. 1999, 69, 904–912. [Google Scholar]
- Novak, L.P. Changes in total body water during adolescent growth. Hum. Biol. 1989, 3, 407–414. [Google Scholar]
- Zhao, Y.; Gong, J.; Ji, Y.; Zhao, X.; He, L.; Cai, S.; Yan, X. Cross-sectional study of characteristics of body composition of 24,845 children and adolescents aged 3–17 years in Suzhou. BMC Pediatr. 2023, 23, 358. [Google Scholar] [CrossRef]
- Waki, M.A.; Kral, J.G.; Mazariegos, M.A.; Wang, J.A.; Pierson, R.N., Jr.; Heymsfield, S.B. Relative expansion of extracellular fluid in obese vs. nonobese women. Am. J. Physiol. 1991, 2, E199–E203. [Google Scholar] [CrossRef]
- Ohashi, Y.; Joki, N.; Yamazaki, K.; Kawamura, T.; Tai, R.; Oguchi, H.; Yuasa, R.; Sakai, K. Changes in the fluid volume balance between intra- and extracellular water in a sample of Japanese adults aged 15–88 yr old: A cross-sectional study. Am. J. Physiol. Renal 2018, 314, F614–F622. [Google Scholar] [CrossRef]
- Hewitt, M.J.; Going, S.B.; Williams, D.P.; Lohman, T.G. Hydration of the fat-free body mass in children and adults: Implications for body composition assessment. Am. J. Physiol. 1993, 265, E88–E95. [Google Scholar] [CrossRef] [PubMed]
- Bandyopadhyay, S.; Puttaswamy, D.; Gabriel, M.P.; Jayakumar, J.; Finkelstein, J.L.; Selvam, S.; Kurpad, A.V.; Kuriyan, R. Estimation of Hydration and Density of Fat-Free Mass in Indian Children Using a 4-Compartment Model: Implications for the Estimation of Body Composition Using 2-Compartment Models. J. Nutr. 2023, 153, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Roemmich, J.N.; Clark, P.A.; Weltman, A.; Rogol, A.D. Alterations in growth and body composition during puberty. I. Comparing multicompartment body composition models. J. Appl. Physiol. 1997, 83, 927–935. [Google Scholar] [CrossRef] [PubMed]
- Garrett, D.C.; Rae, N.; Fletcher, J.R.; Zarnke, S.; Thorson, S.; Hogan, D.B.; Fear, E.C. Engineering Approaches to Assessing Hydration Status. IEEE Rev. Biomed. Eng. 2018, 11, 233–248. [Google Scholar] [CrossRef]
- Fogelholm, M.; van Marken, L.W. Comparison of body composition methods: A literature analysis. Eur. J. Clin. Nutr. 1997, 51, 495–503. [Google Scholar] [CrossRef]
- Celik, A.; Cebeci, A.N. Evaluation of hydration status of children with obesity—A pilot study. J. Pediatr. Endocr. Met. 2021, 34, 295–300. [Google Scholar] [CrossRef]
- Maffeis, C.; Tommasi, M.; Tomasselli, F.; Spinelli, J.; Fornari, E.; Scattolo, N.; Marigliano, M.; Morandi, A. Fluid intake and hydration status in obese vs. normal weight children. Eur. J. Clin. Nutr. 2016, 70, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Harbo, T.; Brincks, J.; Andersen, H. Maximal isokinetic and isometric muscle strength of major muscle groups related to age, body mass, height, and sex in 178 healthy subjects. Eur. J. Appl. Physiol. 2012, 112, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Sagayama, H.; Yamada, Y.; Ichikawa, M.; Kondo, E.; Yasukata, J.; Tanabe, Y.; Higaki, Y.; Takahashi, H. Evaluation of fat-free mass hydration in athletes and non-athletes. Eur. J. Appl. Physiol. 2020, 120, 1179–1188. [Google Scholar] [CrossRef] [PubMed]
- Clayton, P.; Trak-Fellermeier, M.A.; Macchi, A.; Galvan, R.; Bursac, Z.; Huffman-Ercanli, F.; Liuzzi, J.; Palacios, C. The association between hydration status and body composition in healthy children and adolescents. J. Pediatr. Endocr. Met. 2023, 36, 470–477. [Google Scholar] [CrossRef]
- Stookey, J.D.; Kavouras, S.A.; Suh, H.; Lang, F. Underhydration Is Associated with Obesity, Chronic Diseases, and Death Within 3 to 6 Years in the U.S. Population Aged 51–70 Years. Nutrients 2020, 12, 905. [Google Scholar] [CrossRef] [PubMed]
- Jaremków, A.; Markiewicz-Górka, I.; Hajdusianek, W.; Gać, P. Relationships between Body Composition Parameters and Phase Angle as Related to Lifestyle among Young People. J. Clin. Med. 2022, 11, 80. [Google Scholar] [CrossRef]
- Haroun, D.; Wells, J.C.; Williams, J.E.; Fuller, N.J.; Fewtrell, M.S.; Lawson, M.S. Composition of the fat-free mass in obese and nonobese children: Matched case–control analyses. Int. J. Obesity 2005, 19, 29–36. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).