Validity and Reliability of the Turkish Version of the Mindful Eating Behavior Scale
Abstract
1. Introduction
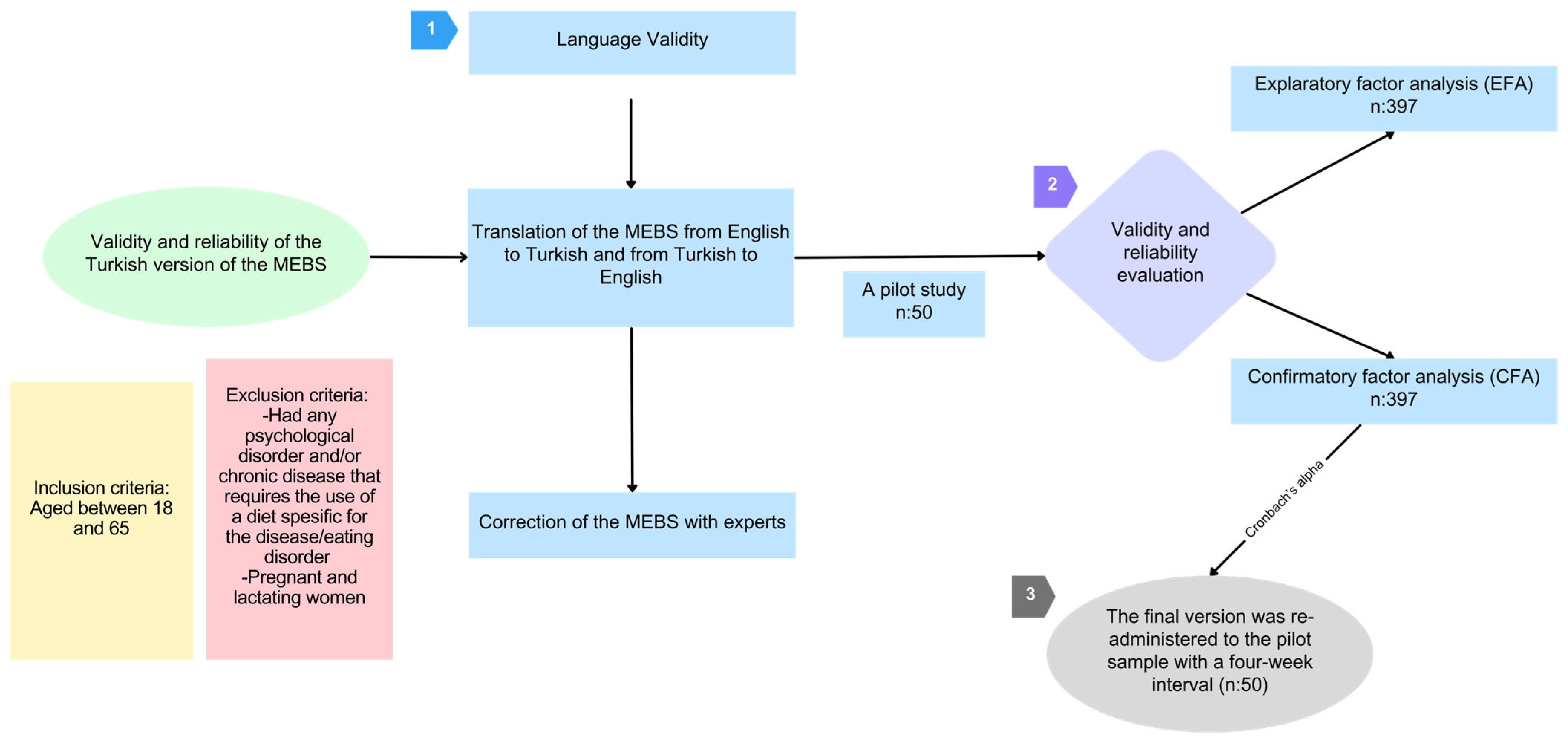
2. Materials and Methods
2.1. Study Design and Participants
2.2. Mindful Eating Behavior Scale (MEBS)
2.3. Language Validity
2.4. Reliability and Validity Evaluation
2.5. Statistical Evaluation
3. Results
3.1. Study Population
3.2. Reliability and Validity Analysis
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Warren, J.M.; Smith, N.; Ashwell, M. A structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviours: Effectiveness and associated potential mechanisms. Nutr. Res. Rev. 2017, 30, 272–283. [Google Scholar] [CrossRef] [PubMed]
- Pepe, R.B.; Coelho, G.S.M.A.; da Silva Miguel, F.; Gualassi, A.C.; Sarvas, M.M.; Cercato, C.; Mancini, M.C.; de Melo, M.E. Mindful eating for weight loss in women with obesity: A randomised controlled trial. Br. J. Nutr. 2023, 130, 911–920. [Google Scholar] [CrossRef] [PubMed]
- Mantzios, M.; Wilson, J.C. Mindfulness, eating behaviours, and obesity: A review and reflection on current findings. Curr. Obes. Rep. 2015, 4, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Papies, E.K.; Barsalou, L.W.; Custers, R. Mindful attention prevents mindless impulses. Soc. Psychol. Pers. Sci. 2012, 3, 291–299. [Google Scholar] [CrossRef]
- Mercado, D.; Robinson, L.; Gordon, G.; Werthmann, J.; Campbell, I.C.; Schmidt, U. The outcomes of mindfulness-based interventions for obesity and binge eating disorder: A meta-analysis of randomised controlled trials. Appetite 2021, 166, 105464. [Google Scholar] [CrossRef]
- Katterman, S.N.; Kleinman, B.M.; Hood, M.M.; Nackers, L.M.; Corsica, J.A. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: A systematic review. Eat. Behav. 2014, 15, 197–204. [Google Scholar] [CrossRef]
- Demirbas, N.; Kutlu, R.; Kurnaz, A. The relationship between mindful eating and body mass index and body compositions in adults. Ann. Nutr. Metab. 2021, 77, 262–270. [Google Scholar] [CrossRef]
- Allirot, X.; Miragall, M.; Perdices, I.; Baños, R.M.; Urdaneta, E.; Cebolla, A. Effects of a brief mindful eating induction on food choices and energy intake: External eating and mindfulness state as moderators. Mindfulness 2018, 9, 750–760. [Google Scholar] [CrossRef]
- Schaefer, J.T.; Magnuson, A.B. A review of interventions that promote eating by internal cues. J. Acad. Nutr. Diet. 2014, 114, 734–760. [Google Scholar] [CrossRef]
- O’Reilly, G.A.; Cook, L.; Spruijt-Metz, D.; Black, D.S. Mindfulness-based interventions for obesity-related eating behaviours: A literature review. Obes. Rev. 2014, 15, 453–461. [Google Scholar] [CrossRef]
- Corbally, L.; Wilkinson, M. The effect of mindfulness-based interventions on stress, depression and anxiety during the perinatal period in women without pre-existing stress, depressive or anxiety disorders: A systematic review and meta-analysis of controlled trials. Mindfulness 2021, 12, 2357–2370. [Google Scholar] [CrossRef]
- Simpson, R.; Simpson, S.; Ramparsad, N.; Lawrence, M.; Booth, J.; Mercer, S.W. Mindfulness-based interventions for mental well-being among people with multiple sclerosis: A systematic review and meta-analysis of randomised controlled trials. J. Neurol. Neurosurg. Psychiatry 2019, 90, 1051–1058. [Google Scholar] [CrossRef] [PubMed]
- Kao, T.S.A.; Ling, J.; Alanazi, M.; Atwa, A.; Suriyawong, W. Effects of mindfulness-based interventions on anthropometric outcomes: A systematic review and meta-analysis. Obes. Res. Clin. Pract. 2023, 17, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Turgon, R.; Ruffault, A.; Juneau, C.; Blatier, C.; Shankland, R. Eating disorder treatment: A systematic review and meta-analysis of the efficacy of mindfulness-based programs. Mindfulness 2019, 10, 2225–2244. [Google Scholar] [CrossRef]
- Carrière, K.; Khoury, B.; Günak, M.M.; Knäuper, B. Mindfulness-based interventions for weight loss: A systematic review and meta-analysis. Obes. Rev. 2018, 19, 164–177. [Google Scholar] [CrossRef]
- Ruffault, A.; Czernichow, S.; Hagger, M.S.; Ferrand, M.; Erichot, N.; Carette, C.; Boujut, E.; Flahault, C. The effects of mindfulness training on weight-loss and health-related behaviours in adults with overweight and obesity: A systematic review and meta-analysis. Obes. Res. Clin. Pract. 2017, 11, 90–111. [Google Scholar] [CrossRef]
- Yu, J.; Song, P.; Zhang, Y.; Wei, Z. Effects of mindfulness-based intervention on the treatment of problematic eating behaviors: A systematic review. J. Altern. Complement. Med. 2020, 26, 666–679. [Google Scholar] [CrossRef]
- Beshai, S.; Bueno, C.; Salimuddin, S. Effects of a self-guided online mindfulness and self-compassion program (Mind-OP) in reducing negative automatic thoughts about self: Randomized active controlled trial. Mindfulness 2023, 15, 259–271. [Google Scholar] [CrossRef]
- Camilleri, G.M.; Méjean, C.; Bellisle, F.; Hercberg, S.; Péneau, S. Association between mindfulness and weight status in a general population from the NutriNet-Santé study. PLoS ONE 2015, 10, e0127447. [Google Scholar] [CrossRef]
- Dunn, C.; Haubenreiser, M.; Johnson, M.; Nordby, K.; Aggarwal, S.; Myer, S.; Thomas, C. Mindfulness approaches and weight loss, weight maintenance, and weight regain. Curr. Obes. Rep. 2018, 7, 37–49. [Google Scholar] [CrossRef]
- Kömürcü Akik, B.; Yiğit, İ. Evaluating the psychometric properties of the mindful eating questionnaire: Turkish validity and reliability study. Curr. Psychol. 2023, 42, 12661–12670. [Google Scholar] [CrossRef]
- Framson, C.; Kristal, A.R.; Schenk, J.M.; Littman, A.J.; Zeliadt, S.; Benitez, D. Development and validation of the mindful eating questionnaire. J. Am. Diet. Assoc. 2009, 109, 1439–1444. [Google Scholar] [CrossRef] [PubMed]
- Hulbert-Williams, L.; Nicholls, W.; Joy, J.; Hulbert-Williams, N. Initial validation of the mindful eating scale. Mindfulness 2014, 5, 719–729. [Google Scholar] [CrossRef]
- Clementi, C.; Casu, G.; Gremigni, P. An abbreviated version of the mindful eating questionnaire. J. Nutr. Educ. Behav. 2017, 49, 352–356. [Google Scholar] [CrossRef] [PubMed]
- Winkens, L.H.; van Strien, T.; Barrada, J.R.; Brouwer, I.A.; Penninx, B.W.; Visser, M. The mindful eating behavior scale: Development and psychometric properties in a sample of Dutch adults aged 55 years and older. J. Acad. Nutr. Diet. 2018, 118, 1277–1290. [Google Scholar] [CrossRef]
- Brown, K.W.; Ryan, R.M. The benefits of being present: Mindfulness and its role in psychological well-being. J. Pers. Soc. Psychol. 2003, 84, 822–848. [Google Scholar] [CrossRef]
- Schuman-Olivier, Z.; Trombka, M.; Lovas, D.A.; Brewer, J.A.; Vago, D.R.; Gawande, R.; Dunne, J.P.; Lazar, S.W.; Loucks, E.B.; Fulwiler, C. Mindfulness and behavior change. Harv. Rev. Psychiatry 2020, 28, 371–394. [Google Scholar] [CrossRef]
- Büyüköztürk, Ş.; Kılıç Çakmak, E.; Akgün, Ö.E.; Karadeniz, S.; Demirel, F. Bilimsel Araştırma Yöntemleri; Pegem Akademi: Ankara, Turkey, 2013; pp. 179–250. [Google Scholar]
- Cohen, L.; Manion, L.; Morrison, K. Research Methods in Education, 5th ed.; RoutledgeFalmer: London, UK, 2002; pp. 641–907. [Google Scholar]
- Osborne, J.W.; Costello, A.B. Sample size and subject to item ratio in principal components analysis. Pract. Assess. Res. Eval. 2019, 9, 11. [Google Scholar]
- Brislin, R.W. Back-translation for cross-cultural research. J. Cross-Cult. Psychol. 1970, 1, 185–216. [Google Scholar] [CrossRef]
- Brislin, R.W. The wording and translation of research instruments. In Field Methods in Cross-Cultural Research; Lonner, W.L., Berry, J.W., Eds.; Sage Publications: Thousand Oaks, CA, USA, 1986; pp. 137–164. [Google Scholar]
- Prieto, A.J. A method for translation of instruments to other languages. Adult Educ. Q. 1992, 43, 1–14. [Google Scholar] [CrossRef]
- Bracken, B.A.; Barona, A. State of the art procedures for translating, validating and using psychoeducational tests in cross-cultural assessment. Sch. Psychol. Int. 1991, 12, 119–132. [Google Scholar] [CrossRef]
- Huck, S.W. Reading Statistics and Research, 6th ed.; Pearson: Boston, MA, USA, 2012; pp. 103–112. [Google Scholar]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef] [PubMed]
- Bryman, A.; Cramer, D. Quantitative Data Analysis with SPSS for Windows: A Guide for Social Scientists; Routledge: London, UK, 1997. [Google Scholar]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; The Guilford Press: New York, NY, USA, 2016. [Google Scholar]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.; Tatham, R. Multivariate Data Analysis, 6th ed.; Pearson Prentice Hall: Upper Saddle River, NJ, USA, 2006. [Google Scholar]
- Tabachnick, B.G.; Fidell, L.S.; Ullman, J.B. Using Multivariate Statistics, 6th ed.; Pearson: Boston, MA, USA, 2013; pp. 497–516. [Google Scholar]
- Stevens, J.P. Applied Multivariate Statistics for the Social Sciences, 4th ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 2002. [Google Scholar]
- Hurley, A.E.; Scandura, T.A.; Schriesheim, C.A.; Brannick, M.T.; Seers, A.; Vandenberg, R.J.; Williams, L.J. Exploratory and confirmatory factor analysis: Guidelines, issues, and alternatives. J. Organ. Behav. 1997, 18, 667–683. [Google Scholar] [CrossRef]
- Schreiber, J.B.; Nora, A.; Stage, F.K.; Barlow, E.A.; King, J. Reporting structural equation modeling and confirmatory factor analysis results: A review. J. Educ. Res. 2006, 99, 323–338. [Google Scholar] [CrossRef]
- Tucker, L.R.; Lewis, C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika 1973, 38, 1–10. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Tapper, K. Can mindfulness influence weight management related eating behaviors? If so, how? Clin. Psychol. Rev. 2017, 53, 122–134. [Google Scholar] [CrossRef]
- Stanszus, L.S.; Frank, P.; Geiger, S.M. Healthy eating and sustainable nutrition through mindfulness? Mixed method results of a controlled intervention study. Appetite 2019, 141, 104325. [Google Scholar] [CrossRef]
- Arch, J.J.; Brown, K.W.; Goodman, R.J.; Della Porta, M.D.; Kiken, L.G.; Tillman, S. Enjoying food without caloric cost: The impact of brief mindfulness on laboratory eating outcomes. Behav. Res. Ther. 2016, 79, 23–34. [Google Scholar] [CrossRef]
- Olson, K.L.; Emery, C.F. Mindfulness and weight loss: A systematic review. Psychosom. Med. 2015, 77, 59–67. [Google Scholar] [CrossRef]
- Ouwens, M.A.; Schiffer, A.A.; Visser, L.I.; Raeijmaekers, N.; Nyklíček, I. Mindfulness and eating behaviour styles in morbidly obese males and females. Appetite 2015, 87, 62–67. [Google Scholar] [CrossRef]
- Winkens, L.H.H.; Van Strien, T.; Brouwer, I.A.; Penninx, B.W.J.H.; Visser, M. Mindful eating and change in depressive symptoms: Mediation by psychological eating styles. Appetite 2019, 133, 204–211. [Google Scholar] [CrossRef] [PubMed]
- van Meer, F.; de Vos, F.; Hermans, R.C.; Peeters, P.A.; van Dillen, L.F. Daily distracted consumption patterns and their relationship with BMI. Appetite 2022, 176, 106136. [Google Scholar] [CrossRef] [PubMed]
- Ogden, J.; Coop, N.; Cousins, C.; Crump, R.; Field, L.; Hughes, S.; Woodger, N. Distraction, the desire to eat and food intake. Towards an expanded model of mindless eating. Appetite 2013, 62, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Blass, E.M.; Anderson, D.R.; Kirkorian, H.L.; Pempek, T.; Price, I.; Koleini, M. On the road to obesity: Television viewing increases intake of high-density foods. Physiol. Behav. 2006, 88, 597–604. [Google Scholar] [CrossRef]
- Braude, L.; Stevenson, R.J. Watching television while eating increases energy intake. Examining the mechanisms in female participants. Appetite 2014, 76, 9–16. [Google Scholar] [CrossRef]
- Hinton, E.C.; Beesley, V.; Leary, S.D.; Ferriday, D. Associations between body mass index and episodic memory for recent eating, mindful eating, and cognitive distraction: A cross-sectional study. Obes. Sci. Pract. 2024, 10, e728. [Google Scholar] [CrossRef]
- Alberts, H.J.; Thewissen, R.; Raes, L. Dealing with problematic eating behaviour. The effects of a mindfulness-based intervention on eating behaviour, food cravings, dichotomous thinking and body image concern. Appetite 2012, 58, 847–851. [Google Scholar] [CrossRef]

| Items | Factor 1 | Factor 2 | Factor 3 | Factor 4 | h2 | u2 |
|---|---|---|---|---|---|---|
| 1. I notice flavors and textures when I’m eating my food | 0.78 | 0.61 | 0.39 | |||
| 2. I stay aware of my food while eating | 0.53 | 0.28 | 0.72 | |||
| 3. I notice how my food looks | 0.73 | 0.53 | 0.47 | |||
| 4. I notice the smells and aromas of food | 0.83 | 0.69 | 0.31 | |||
| 5. It is easy for me to concentrate on what I eat | 0.50 | 0.25 | 0.75 | |||
| 6. I trust my body to tell me when to eat | 0.84 | 0.71 | 0.29 | |||
| 7. I trust my body to tell me what to eat | 0.79 | 0.62 | 0.38 | |||
| 8. I trust my body to tell me how much to eat | 0.80 | 0.64 | 0.36 | |||
| 9. I rely on my hunger signals to tell me when to eat | 0.76 | 0.58 | 0.42 | |||
| 10. I rely on my fullness signals to tell me when to stop eating | 0.58 | 0.34 | 0.66 | |||
| 11. I snack without being aware that I am eating | 0.73 | 0.53 | 0.47 | |||
| 12. I eat automatically without being aware of what I eat | 0.85 | 0.72 | 0.28 | |||
| 13. I eat something without really being aware of it | 0.76 | 0.58 | 0.42 | |||
| 14. My thoughts tend to wander while I am eating | 0.70 | 0.49 | 0.51 | |||
| 15. I think about things I need to do while I am eating | 0.81 | 0.66 | 0.34 | |||
| 16. I multi-task while I am eating | 0.80 | 0.64 | 0.36 | |||
| 17. I read while I am eating | 0.76 | 0.58 | 0.42 | |||
| Eigenvalue Coefficient | 3.29 | 2.62 | 2.54 | 2.43 | ||
| Explained Variance | 19.35 | 15.43 | 14.93 | 14.30 | ||
| Explained Variance (Cumulative) | 19.35 | 34.78 | 49.71 | 64.01 |
| Fit Indices | Acceptable Fit Index Criterion | MEBS Fit Indices |
|---|---|---|
| χ2/df | 3–5 | 3.147 |
| Goodness of Fit Index (GFI) | 0.90–0.95 | 0.910 |
| Normed Fit Index (NFI) | 0.90–0.95 | 0.905 |
| Comparative Fit Index (CFI) | 0.90–0.95 | 0.918 |
| Root Mean Square Error of Approximation (RMSEA) | 0.05–0.08 | 0.074 |
| Standardized Root Mean Square Residual (SRMR) | <0.08 | 0.069 |
| Tucker–Lewis Index (TLI) | >0.90 | 0.887 |
| Subscale | Mean ± SD | α (95% CI) | ω | Item-Total r |
|---|---|---|---|---|
| Focused Eating (F1) | 4.26 ± 0.52 | 0.726 (0.67–0.78) | 0.788 | 0.382–0.617 |
| Hunger/Satiety Cues (F2) | 3.57 ± 0.89 | 0.865 (0.84–0.89) | 0.871 | 0.597–0.795 |
| Eating with Awareness (F3) | 3.80 ± 0.93 | 0.821 (0.78–0.86) | 0.834 | 0.608–0.770 |
| Eating without Distraction (F4) | 3.37 ± 0.72 | 0.723 (0.66–0.78) | 0.847 | 0.295–0.530 |
| Item | Factor | Standardized Factor Loadings (λ) | Residual | R2 |
|---|---|---|---|---|
| Item 1 | F1 | 0.742 | 0.450 | 0.551 |
| Item 2 | F1 | 0.521 | 0.729 | 0.271 |
| Item 3 | F1 | 0.695 | 0.517 | 0.483 |
| Item 4 | F1 | 0.798 | 0.363 | 0.637 |
| Item 5 | F1 | 0.485 | 0.765 | 0.235 |
| Item 6 | F2 | 0.824 | 0.321 | 0.679 |
| Item 7 | F2 | 0.798 | 0.363 | 0.637 |
| Item 8 | F2 | 0.812 | 0.341 | 0.659 |
| Item 9 | F2 | 0.743 | 0.448 | 0.552 |
| Item 10 | F2 | 0.601 | 0.639 | 0.361 |
| Item 11 | F3 | 0.756 | 0.429 | 0.571 |
| Item 12 | F3 | 0.834 | 0.304 | 0.696 |
| Item 13 | F3 | 0.782 | 0.389 | 0.611 |
| Item 14 | F4 | 0.721 | 0.480 | 0.520 |
| Item 15 | F4 | 0.798 | 0.363 | 0.637 |
| Item 16 | F4 | 0.785 | 0.384 | 0.616 |
| Item 17 | F4 | 0.743 | 0.448 | 0.552 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dinç, Ö.; Akal Yıldız, E.; Okburan, G.; Buyuktuncer, Z. Validity and Reliability of the Turkish Version of the Mindful Eating Behavior Scale. Nutrients 2025, 17, 3083. https://doi.org/10.3390/nu17193083
Dinç Ö, Akal Yıldız E, Okburan G, Buyuktuncer Z. Validity and Reliability of the Turkish Version of the Mindful Eating Behavior Scale. Nutrients. 2025; 17(19):3083. https://doi.org/10.3390/nu17193083
Chicago/Turabian StyleDinç, Özge, Emine Akal Yıldız, Gözde Okburan, and Zehra Buyuktuncer. 2025. "Validity and Reliability of the Turkish Version of the Mindful Eating Behavior Scale" Nutrients 17, no. 19: 3083. https://doi.org/10.3390/nu17193083
APA StyleDinç, Ö., Akal Yıldız, E., Okburan, G., & Buyuktuncer, Z. (2025). Validity and Reliability of the Turkish Version of the Mindful Eating Behavior Scale. Nutrients, 17(19), 3083. https://doi.org/10.3390/nu17193083






